2014 年 37 巻 4 号 p. 679-682
2014 年 37 巻 4 号 p. 679-682
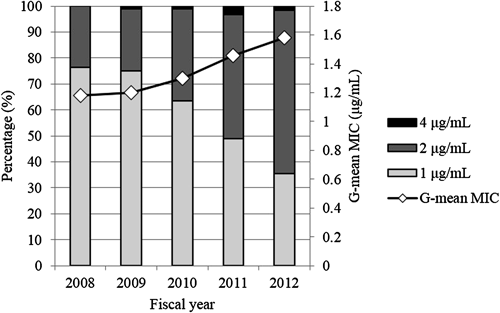
The aim of this study was to evaluate whether linezolid minimum inhibitory concentration (MIC) creep occurred in Staphylococcus aureus clinical isolates, including methicillin-resistant S. aureus (MRSA), over a recent 5-year period at a single Japanese center. A total of 453 MRSA and 195 methicillin-susceptible S. aureus (MSSA) isolates recovered from inpatients from April 1, 2008 to March 31, 2013 were analyzed. The MIC of linezolid was determined by automated Vitek-2 system. The modal MIC, MIC range, MIC50 and MIC90 (MICs required to inhibit the growth of 50% and 90% of organisms, respectively), geometric mean MIC and percentages of susceptible and resistant isolates were evaluated for each fiscal year. None of the S. aureus isolates were resistant to linezolid. Isolates with an MIC of >1 µg/mL were more common in the MSSA samples than in the MRSA samples (91.3% versus 38.2%, p<0.001). The linezolid geometric mean MIC increased by 0.403 µg/mL (from 1.178 in 2008 to 1.582 in 2012) in the MRSA isolates (p=0.006, r2=0.945 according to a linear regression analysis) over the 5-year period; however, no increase was observed in the MSSA isolates. The frequency of MRSA isolates with an MIC of 1 µg/mL decreased (from 76.3% in 2008 to 35.4% in 2012) and the isolates with MICs of >1 µg/mL increased over time (from 23.7% in 2008 to 64.6% in 2012). This report demonstrates the occurrence of linezolid MIC creep, as determined using the geometric mean MIC, in MRSA clinical isolates at a single Japanese center.
Linezolid, which was approved in 2000, is the first clinically used oxazolidinone antimicrobial agent for the treatment of infections caused by Gram-positive pathogens, including methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant S. aureus and vancomycin-resistant enterococci, in the United States as well as European and other countries.1) In 2001, immediately after the introduction of linezolid into clinical use, the emergence of a linezolid-resistant S. aureus isolate was reported in North America,2) and additional cases have recently been reported.3) However, most S. aureus isolates, including MRSA, are found to be linezolid-susceptible at a breakpoint of 4 µg/mL, according to the Clinical and Laboratory Standards Institute criteria.4)
Linezolid was approved for the treatment of MRSA infection in Japan in 2006. The first linezolid-resistant MRSA clinical isolate in Japan was reported in 2009.5) The failure of linezolid chemotherapy due to a heterogeneously resistant isolate, which represents a resistant subpopulation in a fully susceptible isolate and is indicated as a susceptible isolate according to standard susceptibility testing methods, was reported in 2011.6) However, there have been few reports of linezolid minimum inhibitory concentration (MIC) ‘creep’ (i.e., the gradual reduction in the susceptibility of S. aureus to linezolid) among clinical isolates of S. aureus.
The aim of this study was to investigate whether linezolid MIC creep occurred among S. aureus clinical isolates during the last five fiscal years (2008–2012) at a single Japanese center.
Fukuoka University Chikushi Hospital is a 345-bed university-affiliated, tertiary hospital located in the southwestern district of Japan. This study was approved by the Institutional Review Board of Fukuoka University Chikushi Hospital. S. aureus clinical isolates were recovered from inpatients at our hospital from April 1, 2008 to March 31, 2013. Only one isolate per patient was included in this study. For those patients with more than one isolate, only the first isolate for which the results of antimicrobial susceptibility testing were available was included.
Antimicrobial Susceptibility TestingThe MIC of linezolid was determined using the automated Vitek-2 system (Sysmex bioMérieux, Tokyo, Japan) according to the manufacturer’s instructions. The modal MIC, MIC range, MIC50 and MIC90 (MICs required to inhibit the growth of 50% and 90% of organisms, respectively), geometric mean MIC and percentages of susceptible (%S) and resistant (%R) isolates were evaluated for each fiscal year. The fiscal year in Japan is represented by the calendar year for the period from April 1 to March 31. S. aureus (ATCC 29213) and the Enterococcus faecalis strain (ATCC 29212) were used as reference organisms for the antimicrobial susceptibility testing.
Statistical AnalysisCategorical variables were compared using the chi-squared test or Fisher’s exact test, where appropriate. The presence of linezolid MIC creep was evaluated using a linear regression analysis for temporal trends based on the geometric mean MIC measurements. A p value of <0.05 was considered to be significant for all statistical tests.
A total of 1621 S. aureus isolates were recovered from April 1, 2008 to March 31, 2013 at our hospital. Of these isolates, 1262 (77.9%) were MRSA and 359 (22.1%) were methicillin-susceptible S. aureus (MSSA). The incidence of MRSA among the S. aureus isolates gradually decreased over the study period, with 84.1% in 2008, 77.4% in 2009, 80.0% in 2010, 69.7% in 2011 and 68.1% in 2012. Of all the isolates, 648 S. aureus isolates (453 MRSA and 195 MSSA) were analyzed in this study. The number of MRSA and MSSA isolates tested each fiscal year was as follows: n=114 and 26 in 2008; n=84 and 36 in 2009; n=96 and 34 in 2010; n=94 and 57 in 2011; and n=65 and 42 in 2012, respectively. The sources of isolation were sputum (272; 42.0%), wounds/abscesses (101; 15.6%), peritoneal fluid/abdominal drains (58; 9.0%), blood (53; 8.2%), urine (46; 7.1%), nasal cavity/pharynx secretions (30; 4.6%), intravascular catheters (20; 3.1%), pleural effusion/pleural drains (16; 2.5%), bile (16; 2.5%), bronchial lavage fluid (12; 1.9%), feces (9; 1.4%), joint fluid (6; 0.9%), spinal fluid (4; 0.6%) and others.
The modal MIC, MIC range, MIC50, MIC90, geometric mean MIC and %S/%R are shown in Table 1. None of the S. aureus isolates were resistant to linezolid, and the MIC90 values were stable over the 5-year study period. When the linezolid MIC populations were compared between the MRSA and MSSA isolates, a clear difference was observed, with better susceptibility of MRSA to linezolid (modal MIC and MIC50, 1 µg/mL) in comparison to MSSA (modal MIC and MIC50, 2 µg/mL). In fact, isolates with a higher MIC (>1 µg/mL), even within the susceptible range, were more common in the MSSA samples than in the MRSA samples (91.3% versus 38.2%, p<0.001).
| Organism | Fiscal year | Number of isolates | Modal MIC | MIC range | MIC50 | MIC90 | G-Mean MIC | %S/%R |
|---|---|---|---|---|---|---|---|---|
| MRSA | 2008 | 114 | 1 | 1–2 | 1 | 2 | 1.178 | 100/0 |
| 2009 | 84 | 1 | 1–4 | 1 | 2 | 1.199 | 100/0 | |
| 2010 | 96 | 1 | 1–4 | 1 | 2 | 1.297 | 100/0 | |
| 2011 | 94 | 1 | 1–4 | 2 | 2 | 1.457 | 100/0 | |
| 2012 | 65 | 2 | 1–4 | 2 | 2 | 1.582 | 100/0 | |
| MSSA | 2008 | 26 | 2 | 1–2 | 2 | 2 | 1.947 | 100/0 |
| 2009 | 36 | 2 | 1–4 | 2 | 2 | 1.924 | 100/0 | |
| 2010 | 34 | 2 | 2–4 | 2 | 2 | 2.041 | 100/0 | |
| 2011 | 57 | 2 | 1–2 | 2 | 2 | 1.793 | 100/0 | |
| 2012 | 42 | 2 | 1–2 | 2 | 2 | 1.872 | 100/0 |
MIC50/90, MIC for 50% and 90% of the isolates, respectively; G-mean, geometric mean; %S/%R, percentage susceptible and resistant, respectively. The fiscal year in Japan is represented by the calendar year from April 1 to March 31.
Interestingly, the linezolid geometric mean MIC increased over time in the MRSA isolates only, from 1.178 in 2008 to 1.582 in 2012 (Fig. 1). When we evaluated whether linezolid MIC creep was observed using a linear regression analysis, the linezolid geometric mean MIC of the MRSA isolates increased significantly over the study period (p=0.006, r2=0.945); however, this trend did not occur in the MSSA isolates (p=0.408, r2=0.235). The shifts in the linezolid MIC distribution of MRSA clinical isolates occurred primarily as a result of a decrease in the percentage of isolates with an MIC of 1 µg/mL (from 76.3% in 2008 to 35.4% in 2012) and an increase in the percentage of isolates with an MIC of 2 µg/mL (from 23.7% in 2008 to 63.1% in 2012). Furthermore, MRSA isolates with a linezolid MIC of 4 µg/mL first emerged in 2009 and continued to constantly emerge until 2012.
The fiscal year in Japan is represented by the calendar year from April 1 to March 31.
In addition, we evaluated the use of anti-MRSA agents, including linezolid, at our hospital, as assessed according to the antimicrobial use density (AUD), days of therapy (DOT) and the percentage of linezolid in the total AUD (%LZDAUD) or DOT (%LZDDOT) of whole anti-MRSA agents.7) The AUD and DOT of linezolid calculated each fiscal year was as follows: 2.09 and 2.03 in 2008; 2.49 and 2.71 in 2009; 3.13 and 3.30 in 2010; 1.50 and 1.72 in 2011; and 2.22 and 2.39 in 2012, respectively. The %LZDAUD and %LZDDOT ranged from 18.5% and 15.7% to 30.2% and 25.9%, respectively. There were no correlations between AUD, DOT, %LZDAUD or %LZDDOT and geometric mean MIC (p=0.614, p=0.723, p=0.845 and p=0.911 by Pearson’s correlation coefficient, respectively).
S. aureus, including MRSA, continues to be a major pathogen responsible for hospital-acquired infections. At our hospital, the incidence of MRSA among all cases of S. aureus was 77.9% over the study period, which is higher than the rate of 59.8% recently reported in a Japanese nationwide surveillance study,8) although it has been decreasing every year for the past five years at our institution.
Linezolid has been available as a drug for the treatment of infections caused by Gram-positive pathogens in the United States as well as European and other countries since 2000.1) Since 2001, reports have emerged describing linezolid-resistant or heterogeneously resistant S. aureus clinical isolates worldwide, including Japan.3–6) The primary pharmacodynamic parameter predicting the efficacy of linezolid is the area under the concentration–time curve over 24 h divided by the MIC.9) Therefore, since even a subtle shift in an MIC population within the susceptible range has the potential to affect the pharmacodynamic efficacy, and thus the outcomes of patients with MRSA infections, clinical microbiologists and experts in infectious diseases must pay considerable attention to the clinical occurrence of this phenomenon.
In this study, none of the S. aureus isolates were resistant to linezolid, and almost all of the MRSA isolates had an MIC of <4 µg/mL. These results are consistent with those reported by Jones et al. in the ZAAPS Program.3) These authors also demonstrated that MRSA isolates exhibit better susceptibility to linezolid compared with MSSA, which is in agreement with our results. In contrast to their results, however, we found that the trend in decreased susceptibility to linezolid (i.e., linezolid MIC creep) occurred only for MRSA (p=0.006), and not for MSSA (p=0.408), over the study period. In a frequency analysis, the rate of MRSA isolates with a higher linezolid MIC (>1 µg/mL), even when the MIC was within the susceptible range, was found to have been increasing over time (23.7% in 2008 versus 64.6% in 2012, p<0.001). Of note, linezolid MIC creep was observed based on the geometric mean MIC using a linear regression analysis, and this trend was not found based on analyses of changes in the MIC50 and MIC90. This confirms that the geometric mean MIC is a more sensitive marker and have more statistical power to detect changes in the MIC distribution than traditional percentile calculations, such as the %S, %R, MIC50 and MIC90.10)
In Japan, linezolid has been available as a drug for the treatment of MRSA infection since 2006. With the expanded use of linezolid, more exposure of pathogens to this agent has occurred, which may lead to the emergence of clinical isolates with resistance or decreased susceptibility to linezolid. In fact, resistance was not seen in staphylococci during the initial clinical trials prior to the introduction of the drug in the clinical setting.11) Although it is well known that susceptibility to antibiotics is influenced by the use of antibiotics,7) no correlations were found between the trend in decreased susceptibility to linezolid and the AUD, DOT, %LZDAUD or %LZDDOT in this study. It has been reported, however, that a long duration of linezolid therapy is a risk factor for the development of resistance or heterogeneous resistance in S. aureus clinical isolates.5,6) Meka et al. demonstrated that, in the absence of antibiotic pressure, linezolid resistance is unstable in S. aureus clinical isolates.12) In the future, the proper use of linezolid may help to stop MIC creep and return the bacterial population to one that is more susceptible to linezolid.
This study is associated with some limitations. First, this was a retrospective study conducted at a single center. The susceptibility of MRSA to linezolid at our hospital may have been affected by the use of linezolid at medical facilities in the surrounding area. Further analysis of multicenter study is required to investigate the relationship between the linezolid susceptibility trend and the use of linezolid. Second, we determined the linezolid MIC using the automated Vitek-2 system, which is based on the two-fold dilution method. Further studies using the gradient method, such as Etest, which includes an assessment of an intermediate concentration between doubling dilutions are warranted to determine the more precise MIC values. Third, approximately 40% of sample origins were from sputum and therefore our results may not reflect the whole picture of MRSA infection. In addition, the MRSA isolates in this study were not evaluated according to molecular typing methods, and thus the increase in the proportion of strains for which the linezolid MIC is >1 µg/mL may have been caused by the dissemination of limited numbers of clones with less susceptibility to linezolid. However, in our sub-analysis focused on the only MRSA samples from sputum (n=197), the similar linezolid MIC creep phenomenon was observed based on the geometric mean MIC using a linear regression analysis (p=0.012, r2=0.907). Further studies are warranted to distinguish linezolid MIC creep from the increased occurrence of specific clones for which the linezolid MIC is elevated, and more attention should be paid to studying the linezolid MIC shifts of MRSA isolates obtained from blood or other specimens.
In summary, we documented the occurrence of linezolid MIC creep in MRSA clinical isolates using geometric mean MIC measurements. This trend was not observed in MSSA isolates and was not reliably detected using percentile susceptibility markers, such as the MIC50 and MIC90. The clinical significance of the observed trend toward decreased susceptibility of MRSA isolates to linezolid is currently unclear. However, this shift of the linezolid MIC, while it remains within the susceptible range, may portend the future development of either resistance or heterogeneous resistance. Closer scrutiny of linezolid susceptibility trends should include not only measurements of percentile susceptibility markers, but also assessments of the geometric mean statistic and results of MIC frequency analyses.