2017 Volume 40 Issue 6 Pages 837-843
2017 Volume 40 Issue 6 Pages 837-843
Clinical efficacy and adverse effects of the β-blocking agents, carvedilol, bisoprolol, and metoprolol were analyzed theoretically, and then compared quantitatively, for the purpose of determining their proper use for chronic heart failure. Initially, we evaluated occupancy binding to the β1 and β2 receptors (Фssβ1 and Фssβ2) by these drugs. Thereafter, we examined the relationship between Фssβ1 values and left ventricular ejection fraction (LVEF) increase rate to determine efficacy. The result showed that the efficacy with carvedilol could be attained with a lower Фssβ1 value than the others. Therefore, we constructed a model under the assumption that β-blocking agents exert both indirect action of LVEF increase through the β1 receptor and direct action on ryanodine receptor 2. Using the model, it was suggested that these drugs have no differences in regard to the efficacy, while it was clarified theoretically that only carvedilol produces an effect that directly involves ryanodine receptor 2 at clinical doses. We also investigated decreases in heart rate and forced expiratory volume in 1 s as adverse effects of β-blocking agents using a ternary complex model. It was indicated that carvedilol is less likely to induce a heart rate decrease. Meanwhile, it was also suggested that the risk of an asthmatic attack was higher for carvedilol at clinical doses. Our results are considered useful for selection of a proper β-blocking agent and its administration at a reasonable dose for successful heart failure therapy.
Chronic heart failure is a pathological condition in which sufficient cardiac output cannot be maintained due to cardiac contractile dysfunction caused by myocardial failure, which produces hemostasis in the lungs and/or systemic venous system, resulting in impairment of daily life.1,2) Cardiac contractile function regulates ejection of blood, required by peripheral organs, from the left ventricle to aorta, with left ventricular ejection fraction (LVEF) generally employed as its parameter. Cardiac contractile dysfunction is considered to be present when LVEF falls below 40–50% of that in healthy adults.2,3) Moreover, in clinical trials of drugs given to treat heart failure, LVEF increase is used as a parameter to indicate efficacy.
For chronic heart failure therapy, angiotensin-converting enzyme inhibitors, angiotensin 2-receptor antagonists, and β-blocking agents are used.2) Although β-blocking agents were previously contraindicated for conventional treatment, because they inhibit cardiac function, their usefulness for chronic heart failure caused by dilated cardiomyopathy, such as mortality decline and improvement of heart failure, was reported in large-scale clinical trials performed in the 1990s. Thus, β-blocking agents are now utilized with positive results.4,5) Treatment with one of these agents for chronic heart failure is likely to aggravate heart failure symptoms when a maintenance dose is given from the start of administration. Accordingly, the standard administration method calls for starting with a minimal dose that is one-eighth (0.125%) that of the maximum maintenance dose, with doubling of the dose every 1–2 weeks or longer and setting the final dosage for continued therapy after more than 4 weeks.6,7) In such cases, heart rate decrease and bronchoconstriction are adverse effects that should be monitored. In the present study, we performed a theoretical analysis of the efficacy and adverse effects of β-blocking agents used clinically for chronic heart failure for a quantitative comparative evaluation.
Table 1 shows the initial dose as well as minimum and maximum maintenance doses of oral β-blocking agents presented in the package inserts. Since metoprolol was not approved for treatment of chronic heart failure in Japan at present, the doses were set based on the guidelines and the clinical trial method of other two drugs.2,6,7)
| Drug | Initial dose (mg/d) | Maintenance dose (mg/d) | Dose ratio (initial/maximum) | |
|---|---|---|---|---|
| Minimum | Maximum | |||
| Carvedilol | 2.5 | 5 | 20 | 0.125 |
| Bisoprolol fumarate | 0.625 | 1.25 | 5 | 0.125 |
| Metoprolol tartrate | 15 | 30 | 120 | 0.125 |
In the present study, we compared three different β-blocking agents; carvedilol, bisoprolol, and metoprolol, and their dosages.
Collection of Pharmacokinetic and Pharmacodynamic ParametersPharmacokinetic and pharmacodynamic parameters necessary for the present analysis were extracted from the package insert of each agent, as well as from data used for pharmaceutical product approval applications and past reports in Japanese. The parameters obtained were plasma unbound fraction (fu), area under the plasma concentration time curve (AUC0–∞), and dissociation constant for the β1 and β2 receptor (Kd).
Calculation of the Average Occupancy of Target Molecules at Time of Repeated Administration of Each AgentOn the basis of the obtained data, the steady-state average β1 and β2 receptor occupancy (Фssβ1 and Фssβ2, respectively) (%) at the time of repeated administration at the doses shown in Table 1 was calculated by using Eqs. 1 and 2.
 | (1) |
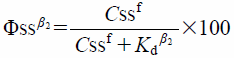 | (2) |
In clinical trials of drugs given to treat heart failure, LVEF increase is used as a parameter to indicate efficacy. Thus, the rate of LVEF increase was calculated as a parameter of clinical efficacy, in which the difference between LVEF at the time of β-blocking agent administration at the maintenance dose and the level before starting administration was divided by that before the start of administration and expressed as a percentage.9–13) For actual LVEF values, the LVEF values of patients with New York Heart Association (NYHA) Functional Classification grade II or III chronic heart failure were obtained from clinical trial results.
We initially examined the relationship between the calculated Фssβ1 value and LVEF increase rate by assuming that the LVEF-improving effect of a β-blocking agent is obtained by β1 receptor blocking on the myocardial cell membrane. When no favorable relationship was observed between them, we speculated that there might be a mechanism that functions directly act on ryanodine receptor 2 in addition to action via the β1 receptor in the LVEF-improving effect of β-blocking agents, as a study of carvedilol reported that its direct action on ryanodine receptor 2 on the sarcoplasmic reticulum membrane was partly involved in clinical efficacy.14) The rate of LVEF increase by administration of β-blocking agents was then analyzed using Eq. 3 in which an additive effect was attained by β1 receptor and ryanodine receptor 2.
 | (3) |
Based on the results of analysis obtained in “Relationship between Average β1 Receptor Occupancy and Clinical Efficacy” above, simulated clinical efficacy at the doses shown in Table 1 was examined.
Relationship between β-Blocking Agent Dose and Adverse EffectsBy using Eqs. 4 and 5 based on the ternary complex model previously reported by us, the rate of average decrease in heart rate (▲HR), which is a cardiovascular adverse effect, was predicted by using Фssβ1 and the rate of average decrease in forced expiratory volume in 1 s (▲FEV1), which is a respiratory adverse effect, was predicted by using Фssβ2. These equations show nonlinear growth graph. In addition, their relationship with dose was evaluated.15)
 | (4) |
 | (5) |
The pharmacokinetic and pharmacodynamic parameters of each agent are shown in Table 2.6–8,16–21) For Kd, the values reported by Baker, who examined the three agents simultaneously, were used.21)
| Drug | Plasma unbound fraction | Area under the plasma concentration time curve per dose (ng·h/mL/mg) | Kd (nM) | |
|---|---|---|---|---|
| β1 | β2 | |||
| Carvedilol | 0.0485a) | 4.49b) | 1.78 | 0.4 |
| Bisoprolol | 0.705a) | 82.6 | 14.8 | 199.5 |
| Metoprolol | 0.885 | 6.05 | 56.0 | 128.8 |
a) Value in serum. b) Range from 0 to 36 h.
The steady-state plasma concentration (Css), and average β1 and β2 receptor occupancies (Фssβ1 and Фssβ2, respectively) at the time of repeated administration at the initial dose, as well as the minimum and maximum maintenance doses were calculated, with the results shown in Table 3.
| Drug | Cssf (nM) | Φssβ1 (%) | Φssβ2 (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Initial | Minimum | Maximum | Initial | Minimum | Maximum | Initial | Minimum | Maximum | |
| Carvedilol | 0.21 | 0.41 | 1.6 | 10.4 | 18.8 | 48.1 | 34.1 | 50.8 | 80.5 |
| Bisoprolol | 4.7 | 9.3 | 37.3 | 24.0 | 38.7 | 71.6 | 2.3 | 4.5 | 15.7 |
| Metoprolol | 25.0 | 50.1 | 200.3 | 30.9 | 47.2 | 78.2 | 16.3 | 28.0 | 60.9 |
For Фssβ1, bisoprolol and metoprolol showed similar levels (initial dose: 24.0 and 30.9%, minimum maintenance dose: 38.7 and 47.2%, maximum maintenance dose: 71.6 and 78.2%, respectively), whereas carvedilol showed lower levels (10.4, 18.8, 48.1%, respectively). As for Фssβ2, the levels varied due to the differences of cardio selectivity of each agent. The level was greatest for carvedilol, followed in order by metoprolol and bisoprolol.
Relationship between Average β1 Receptor Occupancy and Clinical EfficacyThe rates of LVEF increase at a variety of doses of each agent and Фssβ1 were calculated, with their relationship shown in Fig. 1.6,9–13)

For bisoprolol and carvedilol, the same relationship was noted between Фssβ1 and LVEF increase rate. Meanwhile for carvedilol, our findings suggested that clinical efficacy was exerted with a lower Фssβ1 value as compared to the other agents, demonstrating a different aspect of this drug. Accordingly, the actual value for each agent was applied simultaneously to Eq. 3, which takes into consideration the contribution of ryanodine receptor 2 for its analysis. Those results are shown in Fig. 2.6,9–13)

The fitted lines corresponded well with the actual values. Thus, the relationship between Фssβ1 and clinical efficacy could be analyzed by taking into consideration the direct action on ryanodine receptor 2. Values for the parameters were obtained, as follows: Emaxβ1, 51.0%; EmaxRy, 20.5%; KdRy-Car, 0.0872 nM; KdRy-Bis, 301.2 nM; KdRy-Met, 3834 nM. For the increase in LVEF, based on the values for Emaxβ1 and EmaxRy, it was suggested that the ratio of contribution of the action related to the β1 receptor was 71.3%, while that of the direct action on ryanodine receptor 2 was 28.7%. Moreover, the ratio of KdRy for the ryanodine receptor to Kdβ1 for the β1 receptor of each agent (Kdβ1/KdRy) was compared. Our results showed that the affinity of carvedilol for ryanodine receptor 2 was markedly higher as compared to that of the other 2 agents (carvedilol: 20.5, bisoprolol: 0.05, metoprolol: 0.015).
Relationship between Dose and Clinical Efficacy of β-Blocking AgentsThe doses and clinical efficacy of the examined β-blocking agents were simulated on the basis of the parameters obtained, as noted above, with the results shown in Fig. 3.

Light gray area efficacy through ryanodine 2 receptor, dark gray area efficacy through β1 receptor.
The rate of LVEF increase at the maintenance dose ranged from 26.5–44.0% for carvedilol (5–20 mg), 20.3–38.8% for bisoprolol (1.25–5 mg), and 24.3–40.9% for metoprolol (30–120 mg), demonstrating that very similar levels of efficacy were obtained at the maintenance dose. That rate associated with the β1 receptor of carvedilol ranged from 9.6–24.5% and that with ryanodine receptor 2 ranged from 16.9–19.5%. The ratio of contribution was 36.2–55.7% for the β1 receptor and 63.8–44.3% for ryanodine receptor 2. For bisoprolol and metoprolol, the rate of LVEF increase rate associated with ryanodine receptor 2 was markedly lower at 0.6–2.3 and 0.3–1.0%, respectively, while the contribution ratio was 3.0–5.9 and 1.2–2.4%, respectively.
Relationship between Dose and Adverse Effects of β-Blocking AgentsThe relationship between the dose and adverse effects of the examined β-blocking agents, obtained by calculations with Eqs. 4 and 5, are shown in Fig. 4.

The average value for ▲HR at the initial dose was 0.2% for carvedilol, 0.7% for bisoprolol and 1.0% for metoprolol, demonstrating that ▲HR was suppressed at a low level. Meanwhile, the average value for ▲HR at the maximum maintenance dose was 2.2% for carvedilol, 6.0% for bisoprolol, and 8.1% for metoprolol, indicating that the heart rate decreasing effect was lower with carvedilol as compared to metoprolol and bisoprolol. In addition, the average value for ▲FEV1 at the initial dose was 5.5% for carvedilol, 0.3% for bisoprolol, and 2.1% for metoprolol, while that at the maximum maintenance dose was 25.8, 2.1, and 14.0%, respectively, suggesting that the risk of an induced asthmatic attack was higher for carvedilol, followed in order by metoprolol and bisoprolol.
In the present study, clinical efficacy and adverse effects of the β-blocking agents, carvedilol, bisoprolol, and metoprolol were analyzed theoretically, and then compared quantitatively, for the purpose of determining their proper use for chronic heart failure.
The Фssβ1 value at the usual dose was nearly the same for bisoprolol and metoprolol (24.0–71.6 and 30.9–78.2%, respectively), whereas that for carvedilol was lower (10.4–48.1%). Bisoprolol and metoprolol showed the same relationship between LVEF increase rate and Фssβ1, while our findings suggested that the LVEF increase rate with carvedilol could be attained with a lower Фssβ1 value. These findings support previous reports that noted that a targeted action other than toward the β1 receptor might be involved in the clinical efficacy of carvedilol.22–25)
The action mechanism of β-blocking agents is poorly understood. Recent reports have indicated that the major mechanism is correction of the abnormal dynamic state of Ca2+ in myocardial cells by indirectly acting on SERCA2a (Ca2+-ATPase of cardiac sarcoplasmic reticulum), based on β1 receptor blocking, to improve contractility.22,24,26–29) Moreover, findings in those studies suggested that β-blocking agents might directly act on the ryanodine receptor on the membrane of the cardiac sarcoplasmic reticulum. Another study reported that only carvedilol directly acted on ryanodine receptor 2 to selectively control arrhythmia induced by Ca2+ release from the reticulum.14) Furthermore, it has been suggested that carvedilol has no inhibitory action toward the involvement of CICR (Ca2+-induced Ca2+ release) during normal contractions, but acts on arrhythmogenic SOICR (store overload-induced Ca2+ release) on ryanodine receptor 2 to selectively inhibit it.25)
In the present study, we constructed a model under the assumption that β-blocking agents exert indirect action through the β1 receptor and direct action on ryanodine receptor 2, both of which additively exert clinical efficacy (Eq. 3). For clinical efficacy, LVEF increase rate was used as a parameter. In Fig. 2, the fitted lines corresponded well with the actual values. Thus, the relationship between Фssβ1 and clinical efficacy could be analyzed by taking into consideration the direct action on ryanodine receptor 2. Although there is only one LVEF increase rate value for bisoprolol and metoprolol respectively, Eq. 3 was simultaneously applied to the actual value for the six data of the three drugs, and the fitted lines corresponded well with the actual values. Thus, we thought that the relationship between Фssβ1 and clinical efficacy could be analyzed for these drugs. Data collected from patients with NYHA cardiac functional class II or III heart failure were used for our analyses. In analysis with our model, Emaxβ1 was 51.0% and EmaxRy was 20.5%. As for the LVEF increasing effect, the contribution ratio of the action related to the β1 receptor was 71.3% and that of the direct action on ryanodine receptor 2 was 28.7%. Moreover, the KdRy value was 0.0872 nM for carvedilol, 301.2 nM for bisoprolol, and 3.834 nM for metoprolol, thus the activity of carvedilol ranged from approximately 3500 to 44000 times greater than that of the others. Therefore, the LVEF increase rate with carvedilol was attained with a lower Фssβ1 value than the others.
In analysis of the inhibitory effect of Ca2+ released from the cardiac sarcoplasmic reticulum by HEK293 cells in mice, which express ryanodine receptor 2, it was found that the IC50 of carvedilol was 15.9 µM and that of metoprolol was >1000 µM.25) Although these results cannot be directly compared with the KdRy values obtained in our study, they suggest the validity of our analysis, as nearly the same response was obtained in regard to proportion by the agents. On the basis of the parameters obtained and analyzed, LVEF increase rate could be predicted from the dose.
For the maintenance dose range, nearly the same levels were obtained for the β-blocking agents (carvedilol 26.5–44.0%, bisoprolol 20.3–38.8%, metoprolol 24.3–40.9%), suggesting the same level of clinical efficacy. For patients with NYHA functional classification class II and III, average LVEF was reported to be 42.8 and 36.3%, respectively, thus it was considered that the percentage increase in LVEF necessary for attaining the target of 50% might be 16.8 and 37.7%, respectively.30) Those levels agree with the levels obtained in our analysis, indicating that clinical efficacy could be evaluated by using the model constructed in the present study. The LVEF increase rate for carvedilol attained through the β1 receptor was shown to be 9.6–24.5%, while that attained by direct involvement with ryanodine receptor 2 was 6.9–19.5%. On the other hand, the LVEF increase rate attained by involvement with ryanodine receptor 2 for bisoprolol and metoprolol was remarkably low at 0.6–2.3 and 0.3–1.0%, respectively. Our results clarified, at least theoretically, that only carvedilol produces an effect that directly involves ryanodine receptor 2 at clinical doses.
We also investigated decreases in heart rate and FEV1 as adverse effects of β-blocking agents using a ternary complex model. Although it was reported that β-blocking agents could improve delayed afterdepolarization and prevent arrhythmia via ryanodine receptor 2, the mechanism of decreasing heart rate via the receptor is not reported.31) Thus, we assumed that the ▲HR could be predicted by using Фssβ1. The average ▲HR value from administration of the initial dose to that of the maximum maintenance dose ranged from 0.2–2.2% for carvedilol, 0.7–6.0% for bisoprolol, and 1.0–8.1% for metoprolol, indicating that carvedilol is less likely to induce a heart rate decrease. The relationship between Фssβ1 and ▲HR value is nonlinear growth.15) Thus, if there was a little difference in high Фssβ1 value (maximum dose of bisoprolol: 71.6% and metoprolol: 78.2%), ▲HR value is affected (maximum dose of bisoprolol: 6.0% and metoprolol: 8.1%). These findings were in line with past studies that found carvedilol good for chronic heart failure, as it did not decrease heart rate, and stated that bisoprolol should be used with care in patients with a lower heart rate.13,32) Moreover, average ▲HR at the initial dose was lower by one-eighth to one-eleventh of that at the maximum maintenance dose, demonstrating quantitatively the importance of starting administration at one-eight of the maximum maintenance dose to prevent aggravation of heart failure. Meanwhile, average ▲FEV1 from the initial to maximum maintenance dose ranged from 5.5–25.8% for carvedilol, 0.3–2.1% for bisoprolol, and 2.1–14.0% for metoprolol, providing evidence that carvedilol is contraindicated for patients with asthma, as they have a high risk of adverse effects on the respiratory system. These results were considered to support previous reports of the patients with pulmonary disease.33,34)
The present theoretical findings suggest that carvedilol, bisoprolol, and metoprolol have no differences in regard to clinical efficacy, while their action mechanisms for producing effects vary. Moreover, evidence of adverse effects previously reported for these agents was theoretically confirmed, suggesting predictable risk. Thus, our results are considered useful for selection of a proper β-blocking agent and its administration at a reasonable dose for successful heart failure therapy.
The authors declare no conflict of interest.