2020 年 43 巻 9 号 p. 1398-1406
2020 年 43 巻 9 号 p. 1398-1406
Early diagnosis of Niemann–Pick diseases (NPDs) is important for better prognosis of such diseases. N-Palmitoyl-O-phosphocholine-serine (PPCS) is a new NPD biomarker possessing high sensitivity, and with its combination with sphingosylphosphocholine (SPC) it may be possible to distinguish NPD-C from NPD-A/B. In this study, a rapid liquid chromatography-tandem mass spectrometry (LC-MS/MS) method (method 1) and a validated LC-MS/MS analysis (method 2) of PPCS and SPC were developed, and we have proposed a diagnostic screening strategy for NPDs using a combination of serum PPCS and SPC concentrations. Nexera and API 5000 were used as LC-MS/MS systems. C18 columns with lengths of 10 and 50 mm were used for method 1 and 2, respectively. 2H3-Labeled PPCS and nor-SPC were used as internal standards. Selective reaction monitoring in positive-ion mode was used for MS/MS. Run times of 1.2 and 8 min were set for methods 1 and 2, respectively. In both methods 1 and 2, two analytes showed high linearity in the range of 1–4000 ng/mL. Method 2 provided high accuracy and precision in method validation. Serum concentrations of both analytes were significantly higher in NPD-C patients than those of healthy subjects in both methods. Serum PPCS correlated between methods 1 and 2; however, it was different in the case of SPC. The serum PPCS/SPC ratio was different in healthy subjects, NPD-C, and NPD-A/B. These results suggest that using a combination of the two LC-MS/MS analytical methods for PPCS and SPC is useful for diagnostic screening of NPDs.
Niemann–Pick diseases (NPDs) is a group of diseases defined by Crocker in 1961 and is classified into types A to D.1) They are autosomal recessive disorders and have common symptoms, such as hepatosplenomegaly and central nervous system disorders, and are caused by different type of mutations. Type A (NPD-A) and B (NPD-B) are caused by a mutation of SMPD1, which codes for lysosomal acid sphingomyelinase (ASM).2–4) This enzyme catalyzes the metabolism of sphingomyelin into ceramide and phosphorylcholine. Consequently, in patients with NPD-A/B, sphingomyelin accumulates in various organs such as the liver, spleen, lungs, and central nervous system. NPD-A develops in infancy and progresses rapidly; however, patients with NPD-B exhibit late onset and milder symptoms of this disease. In terms of treatment, enzyme replacement therapy for NPD-B is currently being clinically researched.5)
Furthermore, NPD type C (NPD-C) is a mutated protein of NPC1 or NPC2 that are lysosomal cholesterol transporting proteins.6,7) The former is a membrane protein8) and the latter is a soluble protein9); the two proteins cooperate with each other for cholesterol traffic in a coordinated manner.10) As a result, such patients develop NPD-C due to the accumulation of unesterified cholesterol. NPD-C is generally classified into five types according to the age of the patients at onset: neonatal, early-infantile, late-infantile, juvenile, and adult types. As typical symptoms of NPD-C, systemic symptoms, neurological symptoms, and psychiatric symptoms are well known; clinical phenotypes of NPD-C are also very widely observed in patients. The drug, Miglustat, is used for the treatment of NPD-C,11) and cyclodextrin derivatives are under clinical study.12)
As diagnostic methods for NPDs, ASM activity and genetic tests are used for NPD-A/B,3,4) whereas filipin staining13) and genetic tests14) are used for NPD-C. However, these procedures are very complicated and involve a lot of time and effort; hence, they are unsuitable for multi-sample processing. In addition, more than 100 mutations of SMPD1, NPC1 and NPC2 have been reported.3,4,7,14) Considering these facts, biomarkers for NPDs are attracting attention as convenient and rapid diagnostic tests.15) As a typical biomarker for NPD-A/B, sphingosylphosphorylcholine (SPC), a deacylated metabolite of sphingomyelin, has been reported.16) It has also been reported to play a role as a biomarker for NPD-C.17) Oxysterols18,19) and cholenoic acid conjugates,20–23) which are both cholesterol metabolites, are highly accurate markers for NPD-C; they are found in NPD-A/B as well.20,21) Lysosphingomyelin-509 was also reported as a blood biomarker for NPDs and was found to be elevated in NPD-A/B and NPD-C.24) This metabolite was initially thought to be a sphingolipid metabolite; however, it was later identified as N-palmitoyl-O-phosphocholine-serine (PPCS).25,26) The metabolic relationship of PPCS with SPC has been suggested, but the pathophysiological significance is still unclear.25,27,28)
Although NPD-A/B and NPD-C have overlapping clinical manifestations, their treatment post-diagnosis is different. In addition, early treatment with medications leads to better prognosis.11) Therefore, it is clinically important to detect NPD at an early stage and distinguish NPD-C from NPD-A/B. In order to analysis a large number of suspected NPD samples, a rapid analytical method is suitable. Besides, diagnosis of such diseases requires estimating accurate concentrations based on validated analytical methods. Therefore, in this study, we aimed to develop a diagnostic screening strategy for NPDs based on simultaneous analyses of PPCS and SPC (Fig. 1). Towards this objective, we employed a rapid liquid chromatography-tandem mass spectrometry (LC-MS/MS) analytical method that could be applied to multi-sample processing (method 1) and precise quantification based on a validated LC-MS/MS method (method 2). Finally, we proposed a novel diagnostic strategy for NPDs using a combination of the two LC-MS/MS analytical methods for PPCS and SPC.

(a) N-Palmitoyl-O-phosphocholine-serine (PPCS) and (b) sphingosylphosphorylcholine (SPC).
PPCS and 2H3-labeled PPCS (PPCS-2H3) were synthesized as reported previously.25) Lysosphingomyelin (d17:1), also known as nor-SPC, and SPC were purchased from Avanti Polar Lipids, Co., Ltd. (Alabaster, AL, U.S.A.). Acetone and ethanol were procured from Nacalai Tesque (Kyoto, Japan). Formic acid and acetonitrile were purchased from FUJIFILM Wako Pure Chemical Corporation (Osaka, Japan) and Kanto Kagaku (Tokyo, Japan), respectively. Ultrapure water was prepared using an FP-α ultrapure water system (Organo Co., Ltd., Tokyo, Japan) and used in all MS analyses.
Conditions of LC-MS/MSAPI 5000 tandem mass spectrometer (SCIEX, Framingham, MA, U.S.A.) and Nexera ultra HPLC system (Shimadzu, Kyoto, Japan) were combined as an LC-MS/MS system. Selected reaction monitoring (SRM) in positive-ion mode was used for MS/MS analysis. MS parameters (ion spray voltage, turbo spray temperature, curtain gas, nebulizer gas, turbo gas, and collision gas) were optimized for each method using flow injection analysis with 1 µg/mL standard solution. The conditions are summarized in Table S1. The MS/MS parameters were optimized using infusion analysis with 1 µg/mL standard solution. Optimized SRM transitions and MS/MS parameters are shown in Table S1. Formic acid/water (0.1 : 100, v/v) and formic acid/acetone/acetonitrile (0.1 : 50 : 50, v/v/v) were used as mobile phases A and B, respectively. Temperature of the column oven was set at 40°C. Monoselect C18 for HTS (2.1 mm i.d. × 10 mm, 10 µm, GL Sciences, Tokyo, Japan) and InertSustain C18 PEEK (2.1 mm i.d. × 50 mm, 2 µm, GL Sciences) were selected as analytical columns for methods 1 and 2, respectively. Flow rates of the mobile phases for the methods 1 and 2 were set at 1.0 and 0.5 mL/min, respectively. Detailed gradient programs are shown in Table S2.
Preparation of the Stock and Working SolutionsEach analyte (PPCS and SPC) and internal standards (ISs, PPCS-2H3 and nor-SPC) were dissolved to prepare stock solutions of 100–200 µg/mL using water/ethanol (1 : 3, v/v). ISs were mixed and diluted with water/ethanol (1 : 1, v/v) to 1 µg/mL and used as an IS mix solution. The analytes were mixed and diluted with water/ethanol (1 : 3, v/v) to 1, 3, 10, 30, 100, 300, 1000, and 4000 ng/mL (to be used as working solutions for a calibration curve). Mixed solutions of the analytes (2, 80, and 3000 ng/mL) were used as low quality control (LQC), middle quality control (MQC), and high quality control (HQC) solutions, respectively (as working solutions for QC).
Calibration Curves Using Methods 1 and 2Water (10 µL) as a surrogate matrix, IS mix solution (10 µL), working solutions (10 µL) for the calibration curve, and acetonitrile (130 µL) were mixed thoroughly. The mixture was then centrifuged at 15000 × g at 4°C for 10 min, and 1 µL of the supernatant was injected for LC-MS/MS analysis using methods 1 or 2. Peak areas of the analytes and ISs were calculated using SCIEX OS-Q (SCIEX). Peak area ratios of each analyte to ISs were plotted against standard concentrations, and calibration curves were prepared using the least squares method with 1/x2 weighting in both the methods.
Intra-assay and Inter-assay Reproducibility for Method 2To determine intra- and inter-assay reproducibility, 10 µL of working solutions for QC [water/ethanol (1 : 3, v/v) as blank, LQC, MQC and HQC], 10 µL of IS mix, and 130 µL of acetonitrile were added to 10 µL of pooled serum (Cosmo Bio Co. Ltd., Tokyo, Japan). After the samples were mixed and centrifuged, 1 µL of the supernatants were analyzed using method 2. Every three days, these prepared serum samples were analyzed for blank, LQC, MQC, and HQC (N = 6). The recovery (%) was calculated by relative error [R.E. (%)]. In this study, because the analytes were endogenous metabolites, R.E. was calculated by adding the concentration contained in a pooled serum (Blank sample of QC).
 |
Precision (%) was calculated by relative standard deviation [R.S.D. (%)].
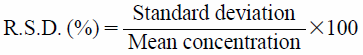 |
These experiments were performed according to the protocol approved by the Ethics Committee of the Graduate School of Medicine in Tohoku University (Approval number, 2013-1-293). Ten microliter of serum from healthy subjects (N = 17), patients with NPD-C (N = 15), and patients with NPD-B (N = 1) were analyzed using both the methods 1 and 2. Data were processed using JMP Pro version 14.0 software (SAS Institute Inc., NC, U.S.A.). Wilcoxon’s t-test was used for correlation of serum concentrations of PPCS and SPC between NPD-C patients and healthy subjects. Single regression analysis was used for correlation of the concentrations of PPCS and SPC obtained between methods 1 and 2. Receiver operating characteristic curves and area under the curve (AUC) were generated by a logistic regression model. Wilcoxon’s t-test was employed for analyzing serum PPCS/SPC ratio between NPD-C patients and healthy subjects.
First, we developed optimum conditions for the two analytical methods. By an infusion MS/MS experiment, optimum SRM transitions and MS/MS parameters were obtained (Table S1). We observed that all the metabolites provided the highest sensitivity when singly-charged positive ions were used as precursor ions and m/z 184 (m/z 187 in the case of PPCS-2H3) derived from the phosphocholine group were used as product ions. Regarding SRM parameters, similar values were obtained from optimization experiments of PPCS and PPCS-2H3. The same was true for SPC and nor-SPC. As a result of optimizing ionization parameters using flow injection analysis, different ion source conditions were obtained for each method, as shown in Table S1. The LC conditions were investigated using different columns, and the optimized chromatograms are shown in Fig. 2. In method 1, the retention times of PPCS and SPC were 0.35 min and 0.31 min, respectively (Fig. 2(a)). Well-shaped peaks were also obtained in serum (Fig. 2(b)). In method 2, the retention times of PPCS and SPC were 3.8 min and 3.1 min, respectively (Fig. 2(c)). The PPCS and SPC peaks were well separated from all other interfering peaks (Fig. 2(d)).

(a) Standard mixture of 100 ng/mL and (b) serum of patient with Niemann–Pick disease type C analyzed by method 1; (c) standard mixture of 100 ng/mL and (d) serum of patient with Niemann–Pick disease type C analyzed by method 2.
Next, calibration curves of the two analytes were prepared for both the analytical methods; quantitative range was set at 1–4000 ng/mL. Four calibration curves were obtained, which provided high linearity. The slopes of the calibration curves for PPCS and SPC were different between the methods 1 and 2 (Table 1).
| Method type | PPCS | SPC | ||
|---|---|---|---|---|
| Regression equation | Correlation of coefficient | Regression equation | Correlation of coefficient | |
| Method 1 | y = 0.000997x + 0.000581 | 0.9983 | y = 0.000725x + 0.000201 | 0.9966 |
| Method 2 | y = 0.000736x + 0.000114 | 0.9982 | y = 0.000527x + 0.000079 | 0.9900 |
PPCS, N-palmitoyl-O-phosphocholine-serine; SPC, sphingosylphosphocholine.
Next, analytical method validation was performed for method 2 (Table 2). In intra-day assay for reproducibility testing, the precision was in the range of 5.52 to 8.15%, and accuracy was in the range of −6.09 to 9.20%. In inter-day assay, the precision ranged between 4.81 and 10.8% and accuracy between −3.61 and 12.2%.
| (a) Intra-day assay | |||||||
|---|---|---|---|---|---|---|---|
| Compound | Precision (R.S.D., %) | Accuracy (R.E., %) | |||||
| 0 (ng/mL) | 2 (ng/mL) | 80 (ng/mL) | 3000 (ng/mL) | 2 (ng/mL) | 80 (ng/mL) | 3000 (ng/mL) | |
| SPC | 8.54 | 7.26 | 5.70 | 8.15 | -5.35 | 9.20 | 9.20 |
| PPCS | 9.54 | 7.06 | 5.52 | 8.49 | -0.580 | -3.92 | -6.09 |
| (b) Inter-day assay | |||||||
| Compound | Precision (R.S.D., %) | Accuracy (R.E., %) | |||||
| 0 (ng/mL) | 2 (ng/mL) | 80 (ng/mL) | 3000 (ng/mL) | 2 (ng/mL) | 80 (ng/mL) | 3000 (ng/mL) | |
| SPC | 8.73 | 4.81 | 10.2 | 7.46 | 0.350 | 2.39 | 9.23 |
| PPCS | 9.94 | 10.8 | 10.4 | 6.95 | 0.520 | 12.2 | -3.61 |
PPCS, N-palmitoyl-O-phosphocholine-serine; SPC, sphingosylphosphocholine; R.E, relative error: R.S.D, relative standard deviation.
Rapid screening method 1 and validated method 2 were applied to analysis of sera of patients with NPDs and healthy subjects. The results analyzed by both the methods 1 and 2 are shown in Table S3. It was observed that the serum PPCS and SPC concentrations in NPD-C patients were significantly higher than those in healthy subjects (Fig. 3).

PPCS concentration by method 1 (a) and by method 2 (b); SPC concentration by method 1 (c) and by method 2 (d).*: p < 0.0001. HC, healthy subjects; NPD-C, patients with Niemann–Pick disease type C; NPD-B, patients with Niemann–Pick disease type B.
Correlation analysis of the serum concentrations of PPCS and SPC obtained by methods 1 and 2 was performed (Fig. 4). In the case of PPCS, a high correlation was observed with y = 0.9417x + 59.00 (R2 = 0.9154) between the methods 1 and 2. A high correlation was also obtained (R2 = 0.8103) for SPC; however, the slope of the graph was low (y = 0.4467x + 2.007).

(a) PPCS and (b) SPC.
Results of receiver operating characteristic (ROC) analysis of serum PPCS concentration between NPD patients and healthy subjects indicated that both the methods 1 and 2 demonstrated AUC of 1.0 and 100% sensitivity and specificity (Fig. 5).

(a) Method 1 and (b) method 2.
Serum PPCS/SPC ratio obtained by method 2 was calculated (Fig. 6). The ratios of all the samples are shown in Table S4. The ratios in healthy subjects ranged from 3.23 to 11.9 and were significantly different (p < 0.0001) from those in NPD-C patients (87.9 to 297). Besides, a ratio of 30.8 was observed in a NPD-B patient.

The aim of this study was to develop a novel diagnostic screening method for NPDs. NPDs include types A and B, which are known as acid sphingomyelinase deficiencies, and type C, which is a deficiency of cholesterol transport protein NPC1 or NPC2.1–4,6–10) Type D is currently classified as type C. Regarding treatment of NPDs, it is necessary to diagnose them as early as possible for better prognosis in such patients.11) In addition, treatment strategies differ depending on the NPD types; hence, it is essential to distinguish among these types. Therefore, NPD biomarkers have been attracting a great deal of attention. Cholesterol metabolites are good NPD biomarkers; however, they require derivatization steps and/or time-consuming chromatographic separations.18–23,29) In addition, they have been reported as biomarkers for various metabolic diseases other than NPDs.30–33) On the other hand, PPCS and SPC are also known as biomarkers for NPDs.24–28,34) There are no reports of the increases of PPCS and SPC in diseases other than NPDs.25,26) They can be easily analyzed by LC-MS/MS. It was also suggested that the ratio of lysosphingomyelin-509 (identified as PPCS later)/SPC in serum/plasma might be useful for distinguishing NPD-C and NPD-A/B.27,28) In this study, we proposed a diagnostic screening strategy for NPDs using a combination of a rapid LC-MS/MS analysis (method 1) and a validated LC-MS/MS analysis (method 2) for serum PPCS and SPC.
Both PPCS and SPC have phosphorylcholine groups and could be detected with high sensitivity by MS/MS. All the compounds containing ISs provided product ions of m/z 184 (m/z 187 in the case of PPCS-2H3), which were similar to those reported in previous studies (Table S1(a)).24–28,34) Ion source parameters were also optimized by a flow injection method using 1 µg/mL of standard solution. The optimized ion source parameters were different in every method due to differences in flow rates (Tables S1(b), (c)).
The purpose of developing method 1 was to speed up the analytical method. However, it was necessary to remove and separate unnecessary contaminants as well. Therefore, we used a very short analytical column (10 mm length). As a type of analytical column, we used a monolith column35) that has a low back pressure. Using a short monolith column enables high-speed analysis with a high flow rate. As a result of optimization for LC conditions in method 1, flow rates of either 1 or 2 mL/min were set for analysis or washing/equilibration, respectively. The flow-through fraction was not introduced into MS Method 1 provided a relatively good peak shape (Figs. 2(a), (b)).
For method 2, C18 stationary phase column with an inner surface comprising polyether ether ketone (PEEK) was used. As a result, peak tailing was suppressed and sharp peaks were obtained (Fig. 2(c)). In this experiment, 50 mm column length column was employed. We observed that although the length of the column was short compared to that reported in a previous study (150 mm of column length),25) complete separation of both PPCS and SPC from contaminant peaks were achieved (Fig. 2(d)).
Next, when the slopes of the calibration curves plotted for methods 1 and 2, it was found that the slopes for the method 1 were larger than those observed for method 2 (Table 1 and Fig. 3). The slope ratio of method 1/method 2 was 135% for PPCS and 138% for SPC (Table 1). The cause of this phenomenon is currently not clear; however, it can be speculated that the increase in peak areas might have been affected due to the higher flow rate used in method 1 (Fig. 2).
To compare two methods, it is necessary to obtain accurate quantitative concentrations. Therefore, we also performed an analytical method validation for method 2. In this experiment, stability tests for PPCS and SPC were omitted because they had proved to be very stable in our previous study.25) Because analytes of this study are endogenous substances,22,23,25,29) the analytical method validation was performed using calibration curves prepared by surrogate matrix (water) and standard spiked serum as QC samples.17,22,23,29) The results satisfied the all criteria laid down by the U.S. Food and Drug Administration (FDA) guidelines36) (Table 2).
Further, serum samples of 17 healthy subjects, 15 NPD-C patients, and 1 NPD-B patient were analyzed by both the methods 1 and 2. Significant differences were observed in both PPCS and SPC between NPD-C patients and healthy subjects in both these methods (Figs. 4(a), (c)). These results were similar to those obtained in previous studies.27,28,32) Regarding NPD-A/B patients, we could analyze only one serum sample from an adult patient. The serum PPCS concentration in this patient was about 3 times higher than the mean serum concentration of NPD-C patients (Figs. 4(a), (c)). This difference was similar to that described in previous reports.24,27,28) Although the metabolic pathway of PPCS is still unclear, we believe that the pathology of NPD-A/B might affect this pathway more than that of NPD-C. In NPD-B patients, serum SPC level increased remarkably because of a lack of functional ASM (Table S3). The concentration was 16.56 times higher than that of the mean concentration in NPD-C patients as observed in method 2.
Next, to investigate the quantitative performance of method 1, we compared the concentrations of PPCS to those observed in method 2. In the correlation analysis of PPCS, the regression equation of y = 0.9417x + 59.00 was obtained (Fig. 4(a)). It was found that the methods 1 and 2 were highly correlated (R2 = 0.9154, Fig. 4(a)). However, although the slope was slightly smaller than 1.0, it was found that the PPCS analysis could provide sufficiently accurate concentrations even by using method 1. The accuracy may not have been compromised even in the rapid analysis, probably because an isotope-labeled compound (PPCS-2H3) was used for IS. On the contrary, the regression equation of SPC showed a slope <0.5 (y = 0.4467x + 2.007) (Fig. 4(b)). The coefficient of determination was R2 = 0.8103. However, this result may not have been due to a variation between individual samples but due to a problem of method 1 itself. Regarding method 1, we did not investigate the matrix effect and reproducibility. It was observed that the calculated SPC concentration in serum samples was reduced due to ion suppression against SPC. In the analysis of SPC, nor-SPC, a structural analog of SPC, was used as IS. Unlike the isotope-labeled compound, nor-SPC could not correct the matrix effect. However, this phenomenon could be ameliorated by the use of isotope-labeled SPC based on previous reports.27,28)
These results indicated that method 1 is useful for PPCS analysis but is inaccurate for SPC analysis. The rapid analysis of PPCS by method 1 is considered to be useful for detecting different types of NPDs. Next, ROC analysis was performed using serum PPCS concentrations, and the results demonstrated that the PPCS concentrations by method 1 discriminated between healthy subjects and NPD patients, including types B and C; AUC was 1.0 and both sensitivity and specificity were 100%. The cut-off concentration was calculated to be about 900 ng/mL as observed from the result of NPD-C patient No. 7, who had the smallest PPCS concentration in this study. By method 2, the cut-off concentration was calculated to be about 1000 ng/mL. The highest PPCS concentration in healthy subjects was 97.2 ng/mL by method 1 and 44.5 ng/mL by method 2 (healthy subject No. 4, Table S3). Therefore, a large difference of serum PPCS concentrations was observed between healthy subjects and NPDs patients. Accordingly, screening of NPDs using method 1 may be considered sufficient, and rapid screening of PPCS using method 1 may enable rapid screening of NPDs. It was thought that a cut-off concentration should be ideally set between the lowest concentration in NPD patients and the highest concentration in healthy subjects. Therefore, the cut-off concentration of PPCS was considered to be 500–900 ng/mL, which was midway between NPD patients and healthy subjects but was slightly lower than the lowest concentration in NPD patients.
Finally, serum PPCS/SPC ratio analyzed by method 2 is shown in Fig. 6 and Table S4. The serum PPCS/SPC ratio in NPD-C patients was significantly higher than that in healthy subjects (p < 0.0001). This result indicates that the increase in PPCS was higher than that in SPC in NPD-C patients than in healthy subjects (Fig. 3, Table S3). Serum PPCS/SPC ratios did not overlap between healthy subjects and NPD-C patients, suggesting that this parameter itself might be useful for distinguishing NPD-C patients from healthy subjects. The mean ratio of PPCS/SPC in NPD-C patients was 5.65 times higher than that in an NPD-B patient. Serum PPCS/SPC ratio was lower in NPD-B patients than in NPD-C patients because of the difference of SPC concentrations between these two groups of patients. SPC increased remarkably in NPD-B patients but only increased several-fold in NPD-C patients than in healthy subjects. Therefore, it was found that the PPCS/SPC ratio showed higher values in the order of healthy subjects < NPD-B patient < NPD-C patients. The cut-off concentration that discriminates between NPD-C and NPD-A/B patients was also investigated. The lowest PPCS/SPC ratio in patients with NPD-C was 87.9, the median was 161, and the highest was 297. Regarding NPD-A/B patients, the number of cases was too small and the variation in the PPCS/ SPC ratio of NPD-A/B patients was not considered; however, we set it just under the minimum value of NPD-C patients and set the cut-off concentration to 75.
In this study, the performance of method 1, whose run time was as short as 1.2 min, was evaluated. It is useful for PPCS analysis for NPDs screening. From the result of ROC analyses, the cut-off concentration between healthy subjects and NPD patients was considered to be about 900–1000 ng/mL. A validated analytical method (method 2) could accurately quantify PPCS and SPC and the run time was 8 min. The cut-off of PPCS/SPC ratio of NPD-C and NPD-A/B was considered to be about 75.
In summary, we propose a diagnostic screening strategy for NPDs (Fig. 7). Following diagnosis of NPDs based on characteristic clinical symptoms of NPDs, such as hepatosplenomegaly and neurological symptoms, a rapid LC-MS/MS test for serum of patients using method 1 should be performed as a first-tier test. At this time, only serum PPCS concentration is used as a screening parameter to detect NPDs. If the concentration of serum PPCS is found to be above 500–900 ng/mL, method 2 should be applied as a second-tier test. Method 2 could be applied to the same sample as method 1 by only changing the analytical column and LC-MS/MS method. Method 2 provides accurate PPCS and SPC concentrations and serum PPCS/SPC ratio. When the PPCS/SPC ratio is found to be lower than 75, NPD-A/B, which is called as ASM deficiency, should be suspected. However, if the PPCS/SPC ratio is higher than 75, NPD-C should be suspected. Later, the diagnosis of NPDs can be confirmed by applying specific diagnostic tests such as genetic tests. However, in this study, we could not collect adequate NPD-A/B patient samples compared to NPD-C patients or healthy subjects because NPD-A/B patients are more difficult to diagnosis and more serious than NPD-C patients. The range of PPCS/SPC ratios in NPD-A/B patients can be expanded a little more if we refer to previous reports related to semi-quantification of PPCS (as lysosphingomyelin-509).24,27,28,32) Accordingly, in the future, the cut-off of the serum PPCS/SPC ratio might change as the number of samples analyzed increase. Hence, for the purpose of verification, method 2 is useful for analyzing PPCS/SPC ratios in patient samples. PPCS and SPC are easier to analyze than cholesterol metabolites that previously required derivatization and long-term LC separations. Furthermore, at present, it is considered to be superior in terms of disease specificity. It has been reported that PPCS could also be analyzed in dried blood spots26); consequently, our proposal can possibly be developed to be used for mass screening of newborns in the further. In addition, the results of this study can be applied to early medical treatments based on early diagnosis and will assist in better prognosis of NPD patients.

We are grateful to all the donors who provided us their valuable serum samples and to doctors who collected the serum samples. This work was supported in part by JSPS KAKENHI 18K15699.
The authors declare no conflict of interest.
The online version of this article contains supplementary materials.