Abstract
Background:
Total bilirubin (TB) concentration is inversely associated with stable coronary artery disease, but there have been few studies on initial TB in patients with ST-segment elevation myocardial infarction (STEMI).
Methods and Results:
A total of 1,111 consecutive patients with STEMI undergoing primary percutaneous coronary intervention (PCI) with drug-eluting stents (DES) were divided into a high TB group (n=295) and a low TB group (n=816) according to the optimal cut-off 0.79 mg/dl. The high TB group had a higher rate of in-hospital major adverse cardiac events (MACE), a composite of cardiac death, non-fatal MI, and definite/probable stent thrombosis (14.2% vs. 4.2%, P<0.001) and cardiac death (13.9% vs. 3.9%, P<0.001) compared with the low TB group. The 30-day MACE-free survival rate was also significantly different between the groups (P<0.001, log-rank test). On multivariate Cox regression, initial high TB was a significant predictor of in-hospital MACE (HR, 2.69; 95% CI: 1.67–4.34, P=0.010) and of cardiac death (HR 2.72, 95% CI: 1.67–4.44, P=0.012). Adding initial TB to TIMI risk score significantly improved prediction for in-hospital MACE according to net reclassification improvement (NRI=5.2%, P=0.040) and integrated discrimination improvement (IDI=0.027, P=0.006).
Conclusions:
Initial TB is a powerful prognostic marker, and inclusion of this can improve prediction of in-hospital MACE in patients with STEMI undergoing primary PCI with DES. (Circ J 2016; 80: 1437–1444)
Despite advances in understanding of the pathophysiology, and improvements in management and prevention, acute coronary syndrome (ACS) remains a major cause of mortality and morbidity in most countries. ACS may manifest as ST-segment elevation myocardial infarction (STEMI) or non-STEMI (NSTEMI). Although subjects with STEMI or NSTEMI share the same cardiovascular risk factors, patients with STEMI have worse short-term mortality compared with patients with NSTEMI.1,2
There is considerable variability in short-term mortality risk, however, in patients with STEMI, therefore, early risk stratification is crucial for successful initial management.3
Serum bilirubin, the final product of heme metabolism, is a powerful antioxidant especially at physiologic oxygen concentration.4
Several epidemiologic studies have shown that serum total bilirubin (TB) concentration is inversely associated with hypertension, diabetes mellitus, and metabolic syndrome.5–7
In addition, serum TB has been suggested to be protective against atherosclerosis and coronary artery disease (CAD) under normal conditions.8,9
In contrast, serum TB is elevated in patients with STEMI and pressure overload in the myocardium.10,11
We herein sought to investigate whether initial TB measured at the time of presentation is prognostic for in-hospital and long-term clinical outcomes in patients with STEMI undergoing primary percutaneous coronary intervention (PCI) with drug-eluting stent (DES), and, if so, to assess the increase in value of adding serum TB to the traditional Thrombolysis in Myocardial Infarction (TIMI) risk score for STEMI.
Methods
Subjects
We enrolled consecutive patients with STEMI who underwent primary PCI with DES within 12 h of symptom onset at 4 university hospitals (Inje University Busan and Haeundae Paik Hospital, Yeungnam University Hospital and Keimyung University Dongsan Hospital) between January 2009 and June 2013. STEMI was defined as cumulative ST-segment elevation ≥1 mm or new-onset left bundle branch block or new Q wave in ≥2 contiguous electrocardiogram (ECG) leads with ≥1 of the following: acute onset of typical ischemic chest pain lasting ≥30 min; elevated serum creatine kinase-MB or troponin at least twice the upper limit of normal.
Patients who did not have pre-PCI bilirubin data, who had acute or chronic infection, systemic inflammatory disease, known liver disease, end-stage renal disease (calculated creatinine clearance <15 ml/min), or malignancy were excluded from the study. Subjects with serum TB >2.0 mg/dl were also excluded due to possible Gilbert’s syndrome. Additionally, patients who had an infarct-related lesion unsuitable for stent implantation, and who were lost to follow-up were excluded from the current study. Informed consent was obtained from all patients. This study was approved by the local institutional review board.
PCI and Medication
All primary PCI were performed by experienced interventional cardiologists at each participating center. The decision to use glycoprotein IIb/IIIa antagonists or intra-aortic balloon pump/percutaneous cardiopulmonary support and selection of DES type were left to the discretion of the operators. Post-dilatation with additional balloon was selectively performed to achieve optimal stent apposition and acceptable angiographic or intravascular ultrasound results. All patients received 300 mg aspirin and individual loading dose of platelet adenosine diphosphate receptor antagonists before coronary angiography. The selection of the type of adenosine diphosphate receptor antagonist was also left to operator discretion. All patients received heparin to maintain activated clotting time ≥250 s during the procedure.
Serum Bilirubin Measurement
In all patients, antecubital venous blood samples for laboratory analysis were drawn at the time of presentation before the patients were transferred to the catheter laboratory. Serum TB was measured using autoanalyzer (Roche Diagnostic Modular Systems, Tokyo, Japan). Serum TB measurement was repeated the next morning after primary PCI in some patients. The normal range for serum TB is 0.2–1.2 mg/dl and direct bilirubin, 0–0.5 mg/dl.
Clinical Outcomes and Definitions
The primary endpoint of this study was the rate of in-hospital major adverse cardiac events (MACE), which was a composite of cardiac death, non-fatal MI, and definite/probable stent thrombosis. The secondary endpoints were the rate of 12-month MACE and the rate of each primary endpoint component during the in-hospital period and at 12-month follow-up. The academic research consortium definition of stent thrombosis was used.12
Non-fatal MI was diagnosed on recurrent chest pain and/or development of new ECG changes accompanied by an increase in serum creatine kinase-MB or troponin to more than twice the upper limit of normal during follow-up. For each patient, TIMI risk score was calculated as the arithmetic sum of the points for each risk feature (age, range 0–3; diabetes or hypertension or angina, range 0–1; systolic blood pressure [SBP] <100 mmHg, range 0–3; heart rate [HR] >100 beats/min, range 0–2; Killip classification II–IV, range 0–2; body weight <67 kg, range 0–1; anterior ST-elevation or left bundle branch block, range 0–1; symptom to balloon time >4 h, range 0–1; total score, range 0–14). All enrolled patients’ clinical and follow-up information were obtained during patient visits to the outpatient clinic or via telephone interview with the patients, their family members, or their personal physicians.
Statistical Analysis
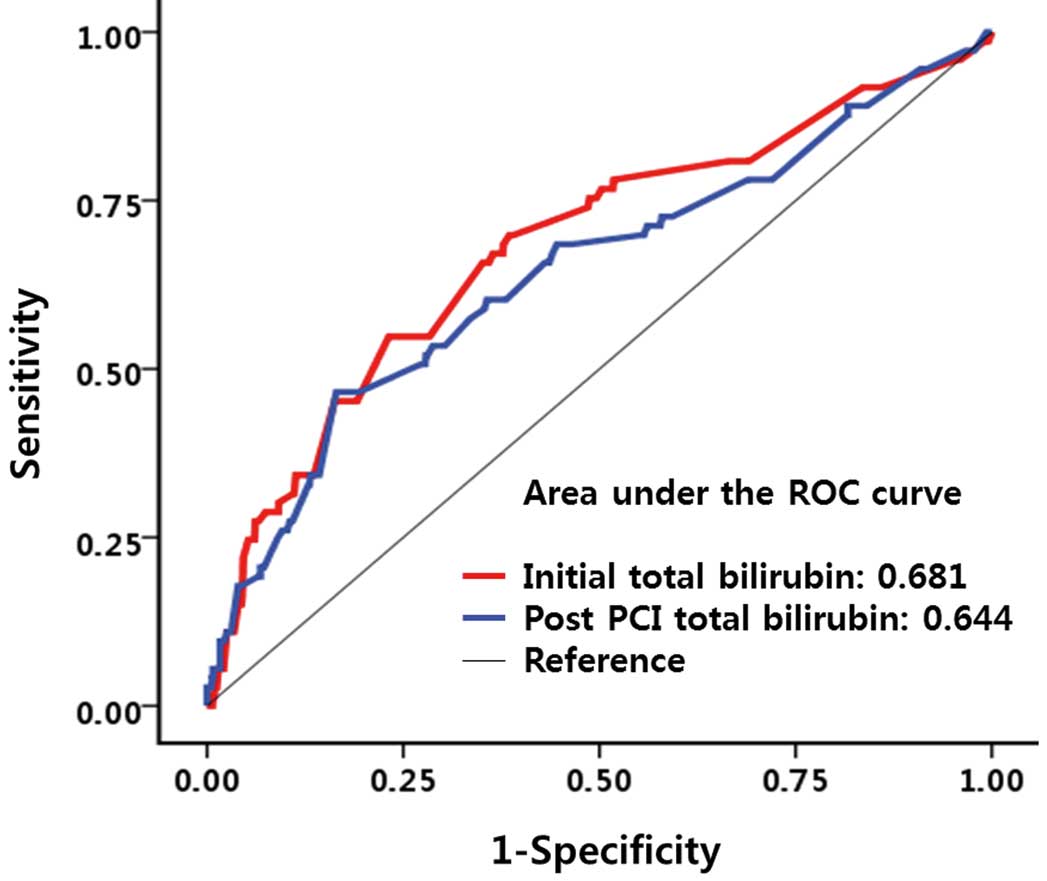
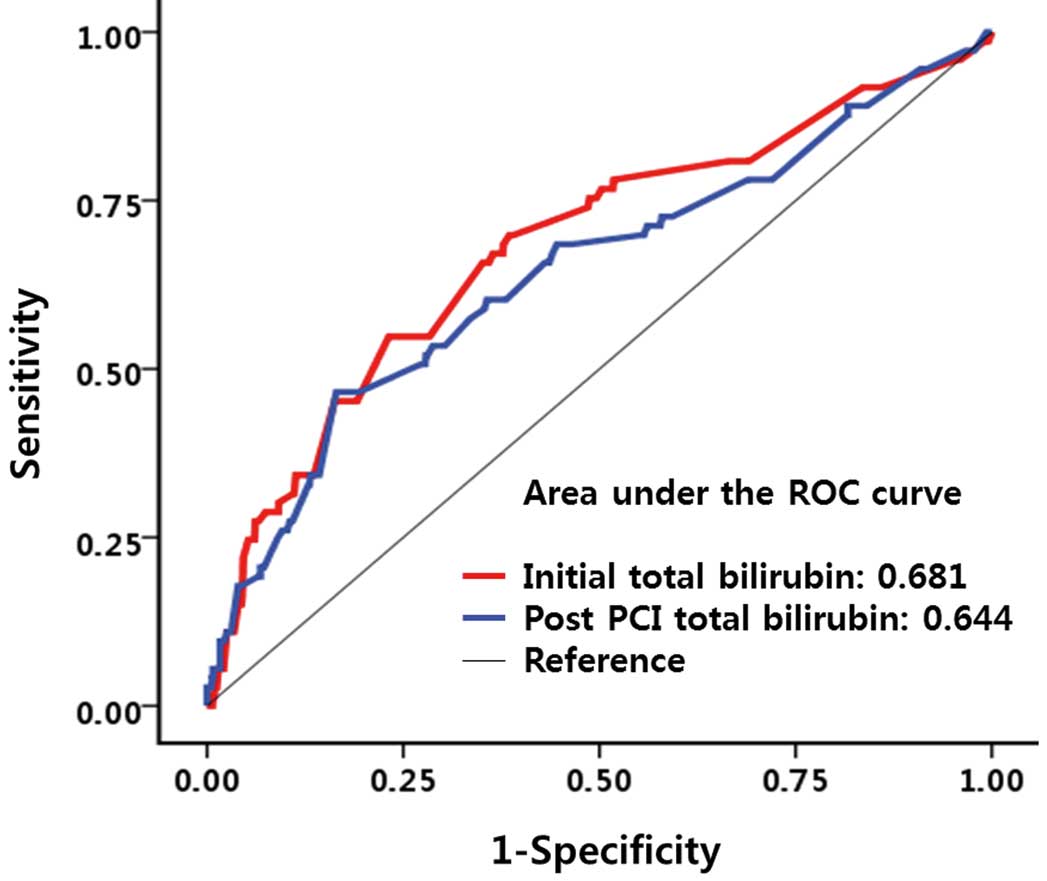
All patients were divided into a high TB group and low TB group according to the optimal cut-off serum TB to discriminate patients with or without in-hospital MACE. The cut-off (>0.79 mg/dl), defined on receiver operating characteristic curve analysis, had sensitivity 56.8%, specificity 75.6%, positive predictive value 14.2%, and negative predictive value 96.1%. Continuous data are presented as mean±SD. Categorical data are presented as frequency and percentage. Student’s t-test or Mann-Whitney U-test were used for comparison of continuous data with normal or skewed distribution, when appropriate. Kolmogorov-Smirnov test was used to test normal distribution of continuous variables. Differences in categorical variables were analyzed using Pearson’s chi-squared test or Fisher’s exact test. The association between serum TB and clinical outcome was evaluated with the Cox proportional hazards model. Covariates used in the Cox model were serum TB, gender, left ventricular ejection fraction (LVEF), creatinine clearance, angiographic parameters (multi-vessel disease, left main disease) and factors included in the TIMI risk score for STEMI. The landmark analysis was performed for MACE-free survival from primary PCI to 30 days, and from 30 days to 12 months. Survival curves were generated using the Kaplan-Meier method, and the difference between the curves was assessed on log-rank test. Increase in prognostic value of the TIMI risk score by the addition of TB was assessed using the Harrell C-statistic, net reclassification improvement (NRI) and integrated discrimination improvement (IDI). NRI requires a priori meaningful risk categories (<10%, 10–50%, and >50% for risk of in-hospital MACE). P≤0.05 was considered statistically significant. Statistical analysis was performed using SPSS 18.0 (SPSS, IL, USA) and R version 3.0.2.
Results
Baseline Characteristics
Initially 1,373 patients were eligible for this study. Two hundred and sixty-two patients were excluded and finally 1,111 patients were included in the current analysis (Figure 1). The mean age was 62.5±12.4 years and 74.9% of the patients were men. Clinical and laboratory characteristics are listed in
Table 1. Overall, there was a positive relationship between clinical features associated with high risk of poor outcome, and high TB. The high TB group had lower initial SBP, lower LVEF, and higher Killip class. Mean and median serum TB were 0.63±0.30 mg/dl and 0.59 mg/dl, respectively. The high TB group had higher peak creatine kinase-MB, hemoglobin, and C-reactive protein (CRP). Angiographic and procedural characteristics are given in
Table 2. Final TIMI flow was worse in the high TB group.

Table 1.
Clinical and Laboratory Characteristics
| Variable |
Low TB
(n=816) |
High TB
(n=295) |
P-value |
| Age (years) |
62.9±12.2 |
61.4±12.9 |
0.063 |
| Male |
596 (73.0) |
236 (80.0) |
0.019 |
| BMI (kg/m2) |
23.5±3.1 |
23.5±2.9 |
0.696 |
| Hypertension |
331 (40.6) |
119 (40.3) |
1.000 |
| Diabetes mellitus |
252 (30.9) |
83 (28.1) |
0.416 |
| Dyslipidemia |
197 (24.1) |
64 (21.7) |
0.423 |
| Previous MI |
43 (5.3) |
13 (4.4) |
0.643 |
| Previous PTCA |
64 (7.8) |
21 (7.1) |
0.798 |
| Previous CABG |
2 (0.2) |
3 (1.0) |
0.120 |
| Current smoker |
417 (51.1) |
141 (47.8) |
0.342 |
| SBP (mmHg) |
123.3±28.1 |
118.3±24.1 |
0.006 |
| LVEF (%) |
49.0±10.7 |
46.7±10.4 |
0.001 |
| Cardiogenic shock |
96 (11.8) |
54 (18.3) |
0.007 |
| Killip class II/III/IV |
242 (43.7) |
126 (54.3) |
0.008 |
| Bilirubin (mg/dl) |
| Total, initial |
0.49±0.15 |
1.03±0.26 |
<0.001 |
| Direct, initial |
0.15±0.06 |
0.29±0.12 |
<0.001 |
| Total, after PTCA |
0.68±0.56 |
1.11±0.50 |
<0.001 |
| Direct, after PTCA |
0.21±0.17 |
0.32±0.13 |
<0.001 |
| Peak CK-MB (ng/ml) |
136.9±112.7 |
197.6±118.4 |
0.002 |
| Hemoglobin (g/dl) |
13.5±1.99 |
14.3±2.04 |
<0.001 |
| CRP (mg/dl) |
1.45±3.52 |
2.06±4.58 |
0.022 |
| CCr (ml/min)† |
68.0±29.9 |
68.4±29.2 |
0.846 |
Data given as mean±SD or n (%). †Calculated by Cockcroft and Gault method. BMI, body mass index; CABG, coronary artery bypass graft; CCr, creatinine clearance; CK-MB, creatine kinase-MB; CRP, C-reactive protein; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PTCA, percutaneous transluminal coronary angioplasty; SBP, systolic blood pressure; TB, total bilirubin.
Table 2.
Angiographic and Procedural Characteristics
| Variable |
Low TB
(n=816) |
High TB
(n=295) |
P-value |
| Culprit lesion |
|
|
0.743 |
| LAD |
411 (50.4) |
154 (52.2) |
|
| LCX |
97 (11.9) |
38 (12.9) |
|
| Right |
297 (36.4) |
98 (33.2) |
|
| Left main |
11 (1.3) |
5 (1.7) |
|
| No. diseased vessels |
|
|
0.432 |
| 1 |
368 (45.1) |
146 (49.5) |
|
| 2 |
238 (29.2) |
78 (26.4) |
|
| 3 |
210 (25.7) |
71 (21.1) |
|
| Gp IIb/IIIa inhibitor |
105 (12.9) |
50 (16.9) |
0.095 |
| IABP or ECMO |
118 (14.5) |
61 (20.7) |
0.016 |
| No. stents |
1.2±0.6 |
1.2±0.4 |
0.986 |
| Stent type |
|
|
0.573 |
| Everolimus |
407 (49.9) |
156 (52.9) |
|
| Zotarolimus |
175 (21.4) |
69 (23.4) |
|
| Biolimus |
99 (12.1) |
29 (9.8) |
|
| First-generation drug |
135 (16.5) |
41 (13.9) |
|
| Final TIMI flow |
|
|
0.019 |
| TIMI 0 |
4 (0.5) |
2 (0.7) |
|
| TIMI 1 |
22 (2.7) |
17 (5.8) |
|
| TIMI 2 |
112 (13.7) |
52 (17.6) |
|
| TIMI 3 |
678 (83.1) |
224 (75.9) |
|
Data given as mean±SD or n (%). ECMO, extracorporeal membrane oxygenation; Gp IIb/IIIa, glycoprotein IIb/IIIa; IABP, intra-aortic balloon pump; LAD, left anterior descending; LCX, left circumflex; TB, total bilirubin; TIMI, Thrombolysis in Myocardial Infarction.
A total of 76 (6.8%) and 96 (8.6%) MACE were documented during hospitalization and at 12-month follow-up, respectively. The majority of in-hospital MACE was attributable to cardiac death (73 events, 6.6%) and the majority of 12-month MACE was also caused by cardiac death (82 events, 7.4%). The high TB group had a higher rate of in-hospital MACE (14.2% vs. 4.2%, P<0.001) and cardiac death (13.9% vs. 3.9%, P<0.001) compared with the low TB group (Table 3). The high TB group also had a higher rate of 12-month MACE (16.9% vs. 5.6%, P<0.001) and cardiac death (15.3% vs. 4.5%, P<0.001). With respect to non-fatal MI and stent thrombosis, there were no significant differences between the 2 groups during hospitalization (0.3% vs. 0.2%, P=1.000; 0.2% vs. 0.3%, P=1.000; respectively) or at 12-month follow-up (1.7% vs. 1.1%, P=0.542; 0.7% vs. 0.5%, P=0.659; respectively). On landmark analysis, 30-day MACE-free survival rate was significantly different between the high and low TB groups (P<0.001, log-rank test;
Figure 2), but this difference was not seen from 30 days up to 12 months.
Table 3.
Clinical Outcomes
| |
Low TB
(n=816) |
High TB
(n=295) |
P-value |
| In-hospital |
n=816 |
n=295 |
|
| MACE |
34 (4.2) |
42 (14.2) |
<0.001 |
| Cardiac death |
32 (3.9) |
41 (13.9) |
<0.001 |
| Non-fatal MI |
2 (0.2) |
1 (0.3) |
1.000 |
| Stent thrombosis |
2 (0.2) |
1 (0.3) |
1.000 |
| From discharge to 12 months |
n=783 |
n=253 |
|
| MACE |
12 (1.5) |
8 (3.2) |
0.115 |
| Cardiac death |
5 (0.6) |
4 (1.6) |
0.234 |
| Non-fatal MI |
7 (0.9) |
4 (1.6) |
0.478 |
| Stent thrombosis |
2 (0.3) |
1 (0.4) |
0.569 |
Data given as n (%). MACE, major adverse cardiac event. Other abbreviations as in Table 1.
On univariate analysis, in-hospital MACE rate was significantly higher in the high TB group, elderly patients (>65 years old), patients with lower body weight (<67 kg), patients with hypertension history, patients with lower initial SBP (<100 mmHg), patients with initial tachycardia (HR >100 beats/min), patients with lower LVEF (≤35%), patients with higher Killip class (II–IV), patients with lower creatinine clearance (≤66.8 ml/min; Cockcroft and Gault method), patients with left main culprit lesion, and patients with multi-vessel disease. On multivariate Cox regression analysis, initial high TB, ejection fraction ≤35%, creatinine clearance ≤66.8 ml/min, initial SBP <100 mmHg, initial HR >100 beats/min, and Killip class II–IV were found to be significant and independent predictors of in-hospital MACE and cardiac death (Table 4).
Table 4.
Indicators of In-Hospital MACE and Cardiac Death
| Variables |
Hazard ratio (95% CI) |
| No adjustment |
P-value |
Adjustment† |
P-value |
| MACE |
| Initial TB >0.79 mg/dl |
3.71 (2.35–5.86) |
<0.001 |
2.69 (1.67–4.34) |
0.010 |
| LVEF ≤35% |
13.61 (8.59–21.57) |
<0.001 |
5.63 (3.41–9.30) |
<0.001 |
| CCr ≤66.8 ml/min |
5.51 (2.97–10.21) |
<0.001 |
2.28 (1.09–4.78) |
0.030 |
| Initial SBP ≤100 mmHg |
5.85 (3.71–9.21) |
<0.001 |
2.83 (1.74–4.61) |
<0.001 |
| Initial HR >100 beats/min |
3.97 (2.43–6.48) |
<0.001 |
1.99 (1.17–3.38) |
0.011 |
| Killip class 2/3/4 |
31.46 (7.66–129.2) |
<0.001 |
5.10 (2.46–10.57) |
<0.001 |
| Cardiac death |
| Initial TB >0.79 mg/dl |
3.86 (2.42–6.15) |
<0.001 |
2.72 (1.67–4.44) |
0.012 |
| LVEF ≤35% |
14.12 (8.81–22.63) |
<0.001 |
5.72 (3.42–9.55) |
<0.001 |
| CCr ≤66.8 ml/min |
5.81 (3.06–11.04) |
<0.001 |
2.34 (1.09–5.04) |
0.030 |
| Initial SBP ≤100 mmHg |
5.94 (3.74–9.45) |
<0.001 |
2.84 (1.73–4.67) |
<0.001 |
| Initial HR >100 beats/min |
3.94 (2.39–6.51) |
<0.001 |
1.97 (1.15–3.38) |
0.013 |
| Killip class 2/3/4 |
60.46 (8.35–437.7) |
<0.001 |
5.40 (2.51–11.64) |
<0.001 |
†Adjusted for initial TB, gender, LVEF, CCr, angiographic parameters (multi-vessel disease, left main disease) and factors included in TIMI risk score for ST-segment elevation MI (age, hypertension, diabetes, previous coronary artery disease, SBP, HR, anterior ST-segment elevation or left bundle branch block, Killip classification, body weight <67 kg, and symptom to balloon time >4 h). Abbreviations as in Tables 1–3.
The area under the curve (AUC) for initial TB (AUC, 0.681; 95% CI: 0.611–0.751; P<0.001) was numerically greater than that for post-PCI TB (AUC, 0.644; 95% CI: 0.571–0.717, P<0.001) and CRP (AUC, 0.638; 95% CI: 0.566–0.710, P<0.001;
Figure 3). Initial TB AUC was also numerically greater than that for initial direct bilirubin (AUC, 0.648; 95% CI: 0.576–0.720. P<0.001) and initial indirect bilirubin (AUC, 0.630; 95% CI: 0.559–0.700, P<0.001). Harrell’s C-statistic for in-hospital MACE numerically increased (0.882 vs. 0.872, P=0.187) when initial TB was incorporated into the multivariate model as a covariate with the risk factors in the TIMI risk score. On NRI analysis, net reclassification after adding TB to TIMI risk score in the multivariate model classified 3 patients (3.9%) in the MACE group as having higher risk, while 13 patients (1.3%) in the non-MACE group were reclassified into the lower risk categories. Overall NRI was 5.2% (P=0.040) and IDI was 0.027 (P=0.006). The combination of initial TB with TIMI risk score further stratified the risk of in-hospital MACE, especially in the case of high TIMI risk score (Figure 4).
Discussion
In this consecutive series of patients recruited from real-world clinical practice, serum TB measured at the time of presentation was able to predict in-hospital MACE in patients with STEMI who underwent primary PCI with DES. The important findings were as follows. First, the initial high TB group had a higher rate of in-hospital MACE and cardiac death compared with the low TB group. Second, an initial high TB was an independent predictor of in-hospital MACE and cardiac death after adjusting for multiple cardiovascular risk factors. Third, the availability of TIMI risk score to predict in-hospital adverse clinical events was improved by incorporating initial TB.
Heme is highly reactive in its unbound form. Under homeostasis, the reactivity of heme is controlled by its insertion into the heme pockets of hemoproteins, for example hemoglobin. Under oxidative stress, however, hemoglobin can release the heme prosthetic groups. The non-protein-bound heme becomes highly cytotoxic and related to the production of free radicals. Heme oxygenase (HO) cleaves the pro-oxidant heme at the α-methene bridge to form biliverdin, carbon monoxide, and ferrous iron. Biliverdin is subsequently reduced to bilirubin by biliverdin reductase. Therefore, HO has anti-oxidant and anti-inflammatory properties. HO activity is induced by its substrate heme and by various non-heme substances. There are 2 isoforms of HO.13
HO-1 is an inducible isoform in response to diverse cellular stress such as oxidative stress, hypoxia, heavy metals, cytokines, but is not expressed under normal conditions. HO-2 is a constitutive isoform that is expressed under homeostatic conditions and is not influenced by stress. Although bilirubin was believed to be only a final product of the heme catabolic metabolism, recent data have shown that serum bilirubin has potent anti-oxidant and cytoprotective properties.4,14
In addition, serum bilirubin has been proven to have anti-inflammatory properties.15
Accordingly, it may seem natural that serum TB is negatively associated with stable cardiovascular disease. Higher serum TB is associated with decreased risk for early familial CAD.8
Serum TB is an inverse and independent risk factor for CAD, with an association equivalent in degree to that of SBP.9
Similar inverse association was shown between serum TB and peripheral vascular disease.16
Serum TB concentration was found to be negatively related to coronary artery calcification17
and ischemic stroke.18
These findings were also noted in a Taiwanese prospective study on cardiac X syndrome patients followed for 5 years, in which patients with the lowest serum TB had a higher incidence of non-fatal MI, ischemic stroke, re-hospitalization for unstable angina, and coronary revascularization.19
In contrast, the serum TB levels show different associations in stressful conditions. TB level is an independent predictor of no-reflow and in-hospital adverse outcome in STEMI patients undergoing primary PCI.10
Another study also noted a significant association between higher TB and adjusted risk of in-hospital cardiovascular mortality in patients with STEMI who underwent primary PCI. No association was found, however, with long-term mortality.20
Increased serum TB was independently associated with severity of CAD on SYNTAX score in patients with NSTEMI.21
Such an association between higher serum TB and higher SYNTAX score was also found in patients with STEMI.22
Increasing TB was significantly associated with the risk of pump failure death but not for sudden death in patients with severe systolic heart failure.11
HO-1 protein and HO activity are markedly upregulated in the myocardium in response to infarction and pressure overload in animals.23
Okuhara et al found the first human evidence for HO-1 activation following acute MI, which was at least partly mediated by the upregulation of HO-1.24
In their study, change in serum TB concentration after PCI was significantly correlated with changes in serum HO-1 level after PCI for culprit lesions, suggesting that elevation of serum TB reflects HO-1 activation. The degree of HO-1 (stress-induced catalytically active enzyme) activation reflects the intensity of the inflammatory reaction to myocardial damage following acute MI. Therefore, serum TB (the end product of heme metabolism) may be a good surrogate marker for the degree of myocardial damage at the acute stage. In the current study, high TB was a significant predictor of in-hospital cardiac adverse events, but prognostic value was not realized at 1 year, suggesting that prognostic value is limited to the early phase. The activation of HO-1 may have lasted only for a short time after the onset of STEMI, resulting in the loss of prognostic value of TB after the acute period. Activation of HO-1 is reported to reach its maximum within 1 h, and return to normal by 6 h after acute stress.25
The present findings are in agreement with previously published data showing that serum high TB is independently associated with in-hospital adverse events in patients with STEMI who underwent primary PCI, although serum TB was taken on the morning after primary PCI in that study.20
To our knowledge, this is the first study to demonstrate an association between initial TB and in-hospital adverse clinical outcomes in patients with STEMI undergoing primary PCI with DES. Bleeding complications at the access site or other focus and other complications related to the primary PCI may have an effect on serum TB level. In the present study, post-PCI TB was higher than initial TB (0.79±0.42 mg/dl vs. 0.63±0.30 mg/dl, P<0.001). Patients with peri-procedural major bleeding requiring blood transfusion (n=8, 0.7%) had a greater increase of TB after PCI compared with patients without major bleeding (0.88±1.20 vs. 0.13±0.30; P=0.123). In addition, the AUC for post-PCI TB for predicting in-hospital adverse events was numerically smaller than that for initial TB. Moreover, we can presume that TB taken at the time of presentation may be more valuable than TB after primary PCI for early risk stratification in patients with STEMI.
Study Limitations
This study has a few limitations. First, this was a retrospective and non-randomized study, therefore, the possibility of selection bias and/or residual confounding from unknown or unmeasured covariates cannot be excluded. All consecutive patients undergoing primary PCI, however, were included, and the present subjects comprised a large real-world cohort. Second, serum TB concentration is affected by many factors including cigarette smoking, fasting, gender, medication and/or diet, and age; we could not evaluate all such factors. Third, the present cut-off (>0.79 mg/dl) is not an absolute value that can be used universally in all STEMI cohorts. Fourth, peri-procedural bleeding may have an effect on post-PCI TB level. Although post-PCI TB was higher than initial TB, and peri-procedural major bleeding requiring blood transfusion raised post-PCI TB more, there was no evidence of a definite relationship between peri-procedural bleeding and post-PCI TB elevation, and post-PCI TB elevation and in-hospital MACE. Fifth, we had no information on changes in TB level during the course of the hospital stay and follow-up. Finally, the clinical availability of serum TB was not compared with that of other inflammatory markers, such as myeloperoxidase or fibrinogen.
Conclusions
Serum TB measured at the time of presentation, an inexpensive and immediately obtainable blood test, is a useful and powerful marker to predict in-hospital MACE and cardiac death. Initial serum TB increases accuracy of prediction of in-hospital adverse clinical events when it is added to TIMI risk score. This study may provide the rationale for the use of initial TB as an early phase prognostic marker in patients with STEMI undergoing primary PCI with DES.
Disclosures
The authors declare no conflicts of interest.
References
- 1.
Fox KA, Dabbous OH, Goldber RJ, Pieper KS, Eagle KA, Van de Werf F, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: Prospective multinational observational study (GRACE). BMJ 2006; 333: 1091–1094.
- 2.
Ishihara M, Fujino M, Ogawa H, Yasuda S, Noguchi T, Nakao K, et al. Clinical presentation, management and outcome of Japanese patients with acute myocardial infarction in the troponin era. Circ J 2015; 79: 1255–1262.
- 3.
Fujii T, Suzuki T, Torii S, Murakami T, Nakano M, Nakazawa G, et al. Diagnostic accuracy of global registry of acute coronary events (GRACE) risk score in ST-elevation myocardial infarction for in-hospital and 360-day mortality in Japanese patients. Circ J 2014; 78: 2950–2954.
- 4.
Stocker R, Yamamoto Y, McDonagh AF, Glazer AN, Ames BN. Bilirubin is an antioxidant of possible physiological importance. Science 1987; 235: 1043–1046.
- 5.
Chin HJ, Song YR, Kim HS, Park M, Yoon HJ, Na KY, et al. The bilirubin level is negatively correlated with the incidence of hypertension in normotensive Korean population. J Korean Med Sci 2009; 24(Suppl): S50–S56.
- 6.
Han SS, Na KY, Chae D, Kim YS, Kim S, Chin HJ. High serum bilirubin is associated with the reduced risk of diabetes mellitus and diabetic nephropathy. Tohoku J Exp Med 2010; 221: 133–140.
- 7.
Giral P, Ratziu V, Couvert P, Carrié A, Kontush A, Girerd X, et al. Plasma bilirubin and gamma-glutamyltransferase activity are inversely related in dyslipidemic patients with metabolic syndrome: Relevance to oxidative stress. Atherosclerosis 2010; 210: 607–613.
- 8.
Hopkins PN, Wu LL, Hunt SC, James BC, Vincent GM, Williams RR. Higher serum bilirubin is associated with decreased risk for early familial coronary artery disease. Arterioscler Thromb Vasc Biol 1996; 16: 250–255.
- 9.
Schwertner HA, Jackson WG, Tolan G. Association of low serum concentration of bilirubin with increased risk of coronary artery disease. Clin Chem 1994; 40: 18–23.
- 10.
Celik T, Kaya MG, Akpek M, Yarlioglues M, Sarli B, Topsakal R, et al. Does serum bilirubin level on admission predict TIMI flow grade and in-hospital MACE in patients with STEMI undergoing primary PCI. Angiology 2014; 65: 198–204.
- 11.
Wu AH, Levy WC, Welch KB, Neuberg GW, O’Connor CM, Carson PE, et al. Association between bilirubin and mode of death in severe systolic heart failure. Am J Cardiol 2013; 111: 1192–1197.
- 12.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Academic Research Consortium: Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007; 115: 2344–2351.
- 13.
Maines MD, Trakshel GM, Kutty RK. Characterization of two constitutive forms of rat liver microsomal heme oxygenase: Only one molecular species of the enzyme is inducible. J Biol Chem 1986; 261: 411–419.
- 14.
Wu TW, Fung KP, Yang CC. Unconjugated bilirubin inhibits the oxidation of human low density lipoprotein better than Trolox. Life Sci 1994; 54: P477–P481.
- 15.
Vitek L, Schwertner HA. The heme catabolic pathway and its protective effects on oxidative stress-mediated diseases. Adv Clin Chem 2007; 43: 1–57.
- 16.
Schwertner HA, Vitek L. Gilbert syndrome, UGT1A1*28 allele, and cardiovascular disease risk: Possible protective effects and therapeutic applications of bilirubin. Atherosclerosis 2008; 198: 1–11.
- 17.
Tanaka M, Fukui M, Tomiyasu K, Akabame S, Nakano K, Hasegawa G, et al. Low serum bilirubin concentration is associated with coronary artery calcification (CAC). Atherosclerosis 2009; 206: 287–291.
- 18.
Kimm H, Yun JE, Jo J, Jee SH. Low serum bilirubin level as an independent predictor of stroke incidence: A prospective study in Korean men and women. Stroke 2009; 40: 3422–3427.
- 19.
Huang SS, Huang PH, Leu HB, Wu TC, Lin SJ, Chen JW. Serum bilirubin predicts long-term clinical outcomes in patients with cardiac syndrome X. Heart 2010; 96: 1227–1232.
- 20.
Gul M, Uyarel H, Ergelen M, Akgul O, Karaca G, Turen S, et al. Prognostic value of total bilirubin in patients with ST-segment elevation acute myocardial infarction undergoing primary coronary intervention. Am J Cardiol 2013; 111: 166–171.
- 21.
Kaya MG, Sahin O, Akpek M, Duran M, Uysal OK, Karadavut S, et al. Relation between serum total bilirubin levels and severity of coronary artery disease in patients with non-ST-segment elevation myocardial infarction. Angiology 2014; 65: 245–249.
- 22.
Sahin O, Akpek M, Elcik D, Karadavut S, Simsek V, Tulmac M, et al. Bilirubin levels and the burden of coronary atherosclerosis in patients with STEMI. Angiology 2014; 65: 198–204.
- 23.
Mito S, Ozono R, Oshima T, Yano Y, Watari Y, Yamamoto Y, et al. Myocardial protection against pressure overload in mice lacking Bach1, a transcriptional repressor of heme oxygenase-1. Hypertension 2008; 51: 1570–1577.
- 24.
Okuhara K, Kisaka T, Ozono R, Kurisu S, Inoue I, Soga J, et al. Change in bilirubin level following acute myocardial infarction is an index for heme oxygenase activation. South Med J 2010; 103: 876–881.
- 25.
Yano Y, Ozono R, Kambe M, Omura S, Yoshizumi M, Ooshima T. Genetic ablation of bach1, a critical transcriptional repressor of heme oxygenase-1, prevents left ventricular remodeling after myocardial infarction in mice. Circ J 2005; 69: 422–423.