2016 年 80 巻 8 号 p. 1852-1856
2016 年 80 巻 8 号 p. 1852-1856
Background: Percutaneous stenting for branch pulmonary artery stenosis is an established interventional choice in congenital heart disease. The apparent morphologic change in the vessel diameter often differs from the hemodynamic result.
Methods and Results: We performed a subanalysis of the data from the Japanese Society of Pediatric Interventional Cardiology (JPIC) stent survey. The factors that may have contributed to morphologic effectiveness included reference vessel diameter (RVD), minimum lumen diameter (MLD) and percent diameter stenosis (%DS) and the relation between morphologic and hemodynamic effectiveness was evaluated in 206 lesions treated with stenting. We defined a “50% increase in MLD” as “morphologically effective”, while “achievement of either a reduced pressure gradient greater than 50% or an increase of perfusion ratio to the affected side to the contralateral side greater than 20%” as “hemodynamically effective”. Morphologic effectiveness was achieved in 84% of patients. Before stenting, %DS was significantly larger, while RVD was smaller in the “effective” group than in the “non-effective” group. The cutoff value for effective stenting was 51% for %DS and 14.7 mm for RVD before stenting. Hemodynamic effectiveness was obtained more often in the “morphologic effective” group.
Conclusions: RVD and %DS were the 2 main contributors to acute morphologic effectiveness. There was a significant relationship between “morphologic effectiveness” and “hemodynamic effectiveness”, judging from increased perfusion of the affected lung and/or decreased pressure gradient. (Circ J 2016; 80: 1852–1856)
Pulmonary artery stenosis (PS) commonly complicates the management of congenital heart disease. It may cause unfavorable results following surgical repair, such as right ventricular failure, arrhythmias, imbalanced lung perfusion, worsening pulmonary insufficiency, and sudden death.1–5 Stent implantation has become an established therapy for PS, and has shown good outcomes in terms of increasing vessel diameter, as well as decreasing the pressure gradient (PG) across the stenosis together with reduced right ventricular pressure and a significant increase in the perfusion of the affected lung.6 Furthermore, early aggressive stenting for PS is recognized as also beneficial in promoting lobar branch growth.7 Successful catheter intervention for PS is usually defined as ≥50% increase in the diameter of the stenotic area for morphologic change, and as either ≥50% reduction of peak systolic PG or ≥20% increase in flow to the affected lung and ≥20% reduction in ratio of systolic right ventricular to aortic pressure for hemodynamic change.8,9 However, occasionally there is disagreement between the enlargement of vessel diameter and the lack of hemodynamic improvement. Furthermore there is a paucity of evidence concerning factors that may affect morphologic effectiveness and the relationship between morphologic and hemodynamic change. This study aimed to determine the factors required for achieving morphologic effectiveness, and the association between morphologic and hemodynamic changes resulting from stenting for PS in patients with complicated congenital heart diseases.
Subanalysis was performed on data from the Japanese Society of Pediatric Interventional Cardiology (JPIC) stent survey, a retrospective questionnaire-based survey of stenting for congenital heart diseases from May 1995 to February 2009 at 14 leading hospitals in Japan.10 The decision for stent implantation was made at each hospital, and stents were deployed using standard techniques. Hemodynamic measurements as well as angiography were performed pre- and post-stent implantation. Pressures were measured directly at catheterization.
Analysis 1: Factors Contributing to Morphologic EffectivenessWe retrospectively analyzed patient profile, ventricular anatomy (1 or 2 ventricles), type of stent, stent remount on the delivery system, balloon diameter used for deployment, and morphologic and hemodynamic data of the lesions, including minimum lumen diameter (MLD), reference vessel diameter (RVD), and PG across the target lesion before and after stenting. Percent increase in MLD and percent diameter stenosis (%DS) was defined as [(MLD after–MLD before)/MLD before]×100 and [(RVD–MLD)/RVD]×100, respectively. When %DS after stenting became a negative value as a consequence of MLD exceeding RVD, we treated it as “0%” for the analysis because a negative value of %DS has no practical meaning.
Analysis 2: Relationship Between Morphologic and Hemodynamic EffectivenessWe analyzed the relationships between morphologic and hemodynamic effectiveness in patients who fulfilled either 1 or 2 of the following criteria, which are generally accepted as indications for stenting for PS: (1) %DS before stenting >50% and (2) PG before stenting >20 mmHg.
We defined “50% increase in the MLD” as “morphologically effective”,9–12 and when the lesions achieve either of the following 2 criteria, we defined it as “hemodynamically effective”: (1) reduced PG >50%, and/or (2) increased perfusion ratio of affected side to the contralateral side >20% by lung perfusion scan. We evaluated factors that may have contributed to morphologic effectiveness and the relation between morphologic and hemodynamic effectiveness. A total of 107 lesions were included in this analysis. Complete data before and after stenting of PG, the lung perfusion scan, and both were obtained in 89, 54, and 34 lesions, respectively.
Statistical AnalysisEach parameter is expressed as a mean value±SD. Logistic regression analysis was used to evaluate the factors that may have contributed to morphologic effectiveness. The cutoff value was evaluated using a receiver-operating characteristic (ROC) curve of factors that contributed to morphologic effectiveness. The optimal cutoff value was determined by Youden-Index. Student’s t-test was used to compare means between each variable. Chi-square test was used to evaluate the relationship between the “morphologic effectiveness” and “hemodynamic effectiveness”. Statistical analyses were performed using JMP® 10 (SAS Institute Inc, Cary, NC, USA). A P value <0.05 was considered statistically significant.
From May 1995 to February 2009, 199 patients (253 lesions) with PS underwent stenting. The background data of the patients, and the morphologic and hemodynamic parameters before and after stenting including MLD, PG, percent increase in MLD and PG, and complications have been previously reported.10 The median age of the patients at catheterization was 11 (0–56) years. The number of implanted original Palmaz stents was 255 (extra-large; 10, large; 199, medium; 46) and that of Palmaz Genesis stents was 23. Stents were deployed using standard techniques.
Factors Contributing to Morphologic EffectivenessWe finally enrolled 206 lesions that had complete MLD and RVD data before and after stenting (Figure 1). In 174 patients (84%) “morphologic effectiveness” was achieved. The comparisons of parameters in the 2 groups (“morphologically effective” and “non-effective”) are summarized in the Table. The RVD was significantly smaller (9.2±3.4 mm vs. 12.0±5.4 mm, P<0.001) and %DS before stenting was significantly larger in the “effective” group than in the “non-effective” group (53±14% vs. 38±12%, P<0.001), while there were no differences for age, ventricular anatomy (1 or 2 ventricles), type of stent, and stent remount on the delivery system.

Design of study of morphological and hemodynamic effectiveness of stenting for pulmonary artery stenosis. DS, diameter stenosis; MLD, minimum lumen diameter; PG, pressure gradient; RVD, reference vessel diameter.
| Effective (n=174) |
Non-effective (n=32) |
OR | 95% CI | P value | |
|---|---|---|---|---|---|
| Age (years) | 11.0±5.7 | 9.5±6.8 | 1.0 | 0.96–1.1 | NS |
| 2 ventricles/1 ventricle | 145/29 | 30/2 | 0.55 | 0.47–6.5 | NS |
| Use of Palmaz large stent | 158 | 31 | 2,067 | 0.0–7.2 | NS |
| Remount on the delivery system | 112 | 22 | 0.7 | 0.89–21.2 | NS |
| RVD (mm) | 9.2±3.4 | 12.0±5.4 | 0.64 | 0.52–0.79 | <0.001 |
| %DS | 53±14 | 38±12 | 1.2 | 1.1–1.3 | <0.001 |
CI, confidence interval; %DS, percent diameter stenosis; OR, odds ratio; RVD, reference vessel diameter.
The relationship between percent increase in MLD and %DS before stenting is shown in Figure 2, and the relationship between percent increase in MLD and RVD is shown in Figure 3. From the ROC curve (Figure 4), the cutoff value for“50% increase in MLD” was 51% for %DS and 14.7 mm for RVD (dotted line in Figures 2,3). The sensitivity and the specificity of the cutoff value for %DS was 56% and 93%, respectively (area under the curve (AUC) 0.65, P<0.01), while those for the cutoff value for RVD were 35% and 92%, respectively (AUC 0.65, P<0.01) (Figure 4). The relationship between balloon diameter and RVD is shown in Figure 5. The dotted line shows the cutoff value of 14.7 mm for RVD, and the solid line shows the value for “balloon diameter=RVD”. In lesions with RVD <14.7 mm, the RVD was smaller than the balloon diameter (8.5±2.7 mm vs. 9.8±2.3 mm, P<0.01) while for RVD >14.7 mm the RVD was larger than the balloon diameter (17.2±2.2 mm vs. 14.0±2.4 mm, P<0.01).

Relationship between percent increase in MLD and %DS. The dotted line shows a cutoff value of 51% in %DS. “50% increase in MLD” was easily achieved in the patients with >51% in %DS. DS, diameter stenosis; MLD, minimum lumen diameter.

Relation between RVD and percent increase in MLD. The dotted line shows a cutoff value of 14.7 mm in RVD. “50% increase in MLD” was easily achieved in the patients with <14.7 mm in RVD. MLD, minimum lumen diameter; RVD, reference vessel diameter.
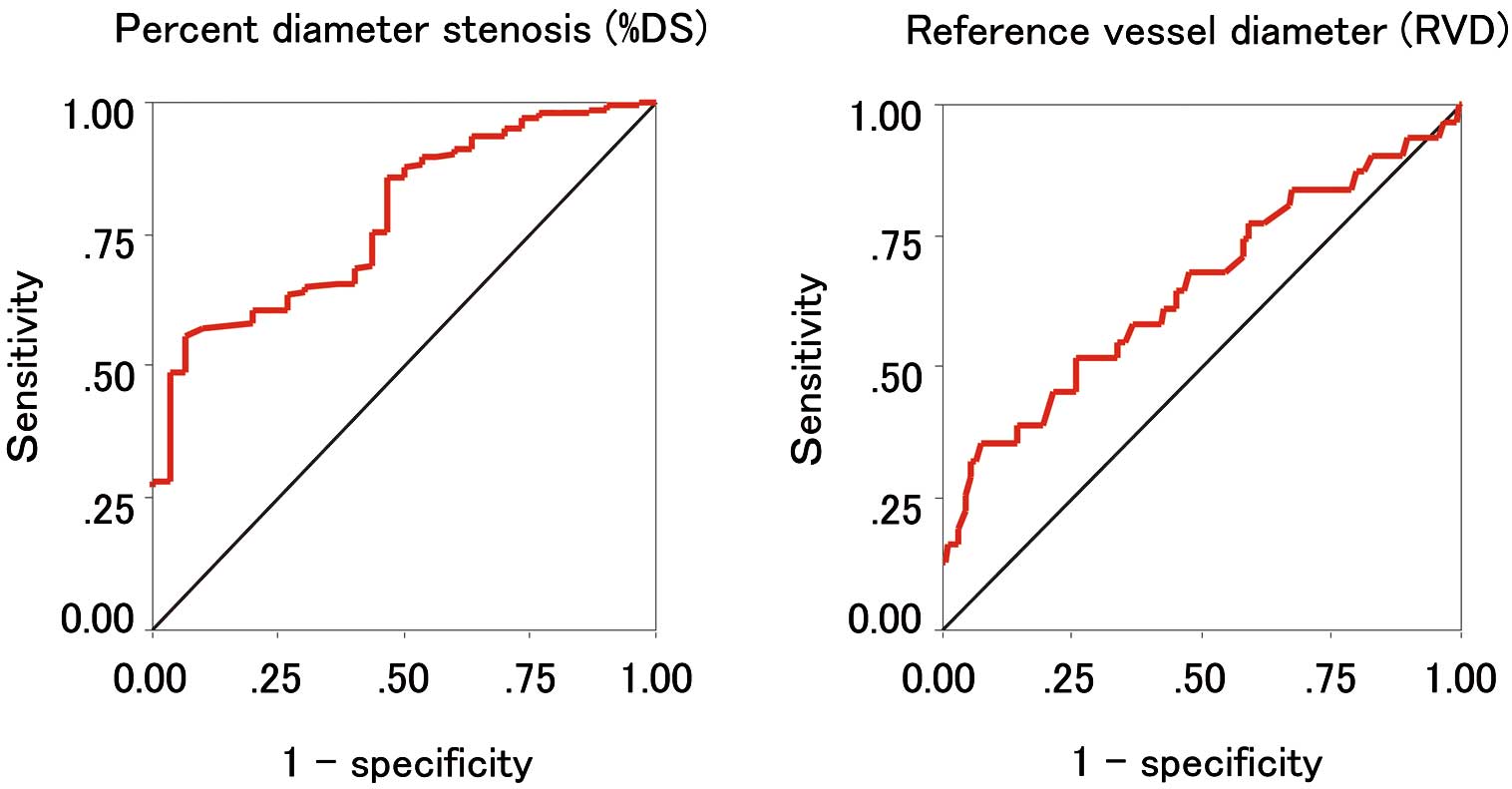
ROC curve of %DS and RVD to “morphologic effectiveness”. The cutoff value of %DS before stenting to “morphologic effectiveness” was 51%, the sensitivity was 56% and the specificity was 93% (AUC 0.65, P<0.01), while the cutoff value of RVD to “morphologic effectiveness” was 14.7 mm; the sensitivity was 35% and the specificity was 92% (AUC 0.65, P<0.01). AUC, area under the curve; DS, diameter stenosis; ROC, receiver-operating characteristic; RVD, reference vessel diameter.

Relationship between RVD and balloon diameter used for delivery. The dotted line shows the cutoff value of 14.7 mm for RVD, and the solid line links the value of “balloon diameter=RVD”. In the lesions with RVD <14.7 mm the RVD was smaller than the balloon diameter (8.5±2.7 mm vs. 9.8±2.3 mm, P<0.01), while with RVD >14.7 mm the RVD was larger than the balloon diameter (17.2±2.2 mm vs. 14.0±2.4 mm, P<0.01). RVD, reference vessel diameter.
We analyzed the relationships between morphologic and hemodynamic effectiveness in 107 lesions that fulfilled either 1 or 2 of the specified criteria (Figure 1). A total of 89 lesions had complete data for PG before and after stenting, while 52 had data from a lung perfusion scan. “Morphologic effectiveness” was obtained in 95 of the 107 analyzed lesions (89%). Reduction of PG greater than 50% occurred in 62/89 patients (70%), while perfusion ratio increased more than 20% in 40/52 patients (77%). As a result, “hemodynamic effectiveness” was obtained in 80/107 (75%) lesions. There was no significant difference in the frequency of achieving “reduced PG >50%”, or “improved perfusion ratio >20%” between the “morphologic effective” group and the “morphologic non-effective” group. However, if we included either achievement of “reduced PG >50%” and/or “improved perfusion ratio >20%” as hemodynamic effective, there was a significant difference in the possibility of hemodynamic effectiveness between the 2 groups (74/95; 78% vs. 6/12; 50%, P<0.05, Figure 6).

Possibility of hemodynamic effectiveness in the “morphologic effective” and “morphologic non-effective” groups.
Indications for stenting in PS are well recognized and include (1) kinking or stretch, (2) external compression, (3) intimal flaps, (4) postoperative stenosis, and (5) relatively mild stenosis and restenosis following successful balloon angioplasty.6,13 However, there is a paucity of evidence concerning factors that may determine a satisfactory achievement of acute morphological change. According to our study, “morphologic effectiveness” was likely to be achieved if the %DS before stenting is >51% and if RVD is <14.7 mm. We did not find any other significant contribution of other factors such as age, 1 or 2 ventricle physiology, and the type of stent.
Clearly, there must be some correlation between the percent increase in MLD and %DS, as each parameter is based on similar raw data. However, each cutoff value was derived from real-world clinical practice, which means that “50% increase in MLD” is easy to achieve in the patients with >51% in %DS (Figure 2). From Figure 5, it can be seen that a balloon diameter less than the RVD tended to be selected for most of the lesions with RVD >14.7 mm, in contrast to a balloon diameter larger than RVD for lesions with RVD <14.7 mm. As a consequence, “50% increase in MLD” is less likely to be achieved in cases of RVD >14.7 mm, probably because balloon size in such cases is relatively small for the RVD. Consequently, we consider that these values (>51% in %DS and <14.7 mm in RVD) are reasonable to use if the focus is on achieving acute morphological success.
Relationship Between Morphologic and Hemodynamic EffectivenessSeveral studies have demonstrated that PA stenting is effective in increasing PA diameter, reducing PG6,10,14–16 and increasing perfusion of the affected lung.4,6,11 Occasionally there is a disparity between the expected hemodynamic change and morphologic improvement. Increased flow to the affected side partially restores the PG. Cunningham et al postulated that this disagreement is likely to be attributable to the presence of diffuse, distal stenosis, and to abnormalities in the mechanical behavior of these patients’ pulmonary arteries.17 We found no significant relationship between “morphologic effectiveness” and “reduction of PG >50%”; if we took both the results of the PG and lung perfusion scan into account, “hemodynamic effectiveness” was more likely to be achieved in the “morphologic effectiveness” group. When the stenotic vessel with normal vascular resistance and decreased blood flow is dilated by stenting, the increase in blood flow may mask changes in the PG. Our result may be partly explained by such a shift in blood flow. From our data, we could not determine whether these factors might contribute to the disagreement between hemodynamic and morphological effectiveness.
Study LimitationsThis study was based on data from a questionnaire survey, and background data of the patients, morphological measurement of the target, and PG were limited. Lack of other hemodynamic data such as right ventricular pressure and definitive clinical benefits also limited the analysis. The small number of patients may limit the significance of the statistical analysis.
Factors that contributed to acute morphologic effectiveness were the morphological features of the stenotic vessel itself (>51% in %DS and <14.7 mm in RVD), while other factors such as age, ventricular anatomy, type of stent, and stent remount on the delivery system did not contribute. There was significant relationship between “morphologic effectiveness” and “hemodynamic effectiveness” when both the increase in perfusion of the affected lung as well as the PG change were taken into account.
We thank Dr Peter M. Olley, Professor Emeritus of Pediatrics, University of Alberta, and Dr. Setsuko Olley for language consultation.