Abstract
Background:
Low population density may be associated with high mortality in acute myocardial infarction (AMI) patients. The purpose of this study was to investigate the effect of population density and hospital primary percutaneous coronary intervention (PCI) volume on AMI in-hospital mortality in Japan.
Methods and Results:
This is a retrospective study of 64,414 AMI patients transported to hospital by ambulances. The main outcome measure was in-hospital mortality. The median population density was 1,147 (interquartile range, 342–5,210) persons/km2. There was a significant negative relationship between population density and in-hospital mortality (OR for a quartile down in population density 1.086, 95% CI 1.042–1.132, P<0.001). Patients in less densely populated areas were more often transported to hospitals with a lower primary PCI volume, and they had a longer distance to travel. By using multivariable analysis, primary PCI volume was found to be significantly associated with in-hospital mortality, but distance to hospital was not. When divided into the low- and high-volume hospitals, using the cut-off value of 115 annual primary PCI procedures, the increase in in-hospital mortality associated with low population density was observed only in patients hospitalized in the low-volume hospitals.
Conclusions:
Increased in-hospital mortality related to low population density was observed only in AMI patients who were transported to the low primary PCI volume hospitals, but not in those who were transported to high-volume hospitals.
Residents in less densely populated areas generally have limited access to healthcare resources compared to urban residents, and differences in health outcomes between urban and rural residents have been documented.1,2
For patients with acute myocardial infarction (AMI), high quality of care and early reperfusion therapy with primary angioplasty are critical to reduce mortality.3–6
However, the relationship between population density and mortality in AMI patients and the effect of distance to hospital and hospital volume on this relationship in Japan are unknown.
Editorial p 1057
The World Bank reported that the percentage of people living in rural areas has been constantly declining, from 66.4% to 45.2%, between 1960 and 2017 all over the world (https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS, accessed February 2019). The percentages of rural populations in major countries and regions are as follow: India 66.4%, China 42.0%, Europe area 23.2%, and the United States of America 17.9%. Japan, a small island country, is largely covered by mountains, and the percentage of the rural population is quite low, at 8.5%. In such a densely populated situation, the association between population density and mortality after AMI is unclear. As a result, many percutaneous coronary intervention (PCI)-capable hospitals have been created in Japan to provide prompt primary PCIs for AMI patients. A large number of hospitals providing PCI are smaller relative to other countries, and transportation time from the scene of event to a PCI-capable hospital is short. However, whether distance to a PCI-capable hospital affects the survival of AMI patients and whether hospital volume is more important for outcomes of AMI remains unknown.
In this study, we investigated the effect of population density on in-hospital mortality of patients with AMI between low- and high-hospital volumes by analyzing the database of the Japanese Registry of All Cardiac and Vascular Diseases (JROAD) and the Japanese Diagnosis Procedure Combination (DPC) nationwide administrative claims database.
Methods
Data Sources
This is a retrospective study, using the combined JROAD and DPC databases (JROAD-DPC). The JROAD was launched in 2004 by the Japanese Circulation Society to survey hospitals’ activities in clinical practice. As previously reported,7,8
almost all teaching hospitals with beds for cardiac diseases in Japan – 1,613 hospitals – were enrolled in JROAD. In contrast, the DPC is an inpatient care database used throughout Japan and is linked with a lump-sum payment system administered by the Ministry of Health, Labour, and Welfare of Japan. The DPC database includes the following individual data: unique hospital identifier; patient age and sex; main diagnoses and comorbidities; drugs and devices; diagnostic and therapeutic procedures; length of stay; and discharge status. DPC data were obtained from 806 hospitals, which were from the 1,613 hospitals in the JROAD registry. We obtained the data of patients with AMI admitted and discharged between 1 April 2012 and 31 March 2015. Patients with a diagnosis of AMI were identified by International Classification of Diseases (ICD)-10 codes I210, I211, I212, I213, I214, and I219. Patients aged <20 years were excluded, and those who were discharged alive on the same day as admission were excluded to rule out mild cases. Among patients who were hospitalized for AMI repeatedly within the study period, the first hospitalization was included in the analyses. Patients who suffered from an out-of-hospital cardiac arrest (OHCA) were also excluded; those who arrived not in an ambulance and patients who were diverted from other hospitals were excluded to investigate only those who were directly transported from the scene of the event to hospital by ambulance. We also collected hospital data from the JROAD database, including the unique hospital identifier, bed counts, annual number of primary PCI procedures, annual number of elective PCI procedures, coronary care unit (CCU), and facility of cardiac rehabilitation authorized by the Japanese Association of Cardiac Rehabilitation.
Population density at the zip code of the patient’s residence was determined according to the 2010 Population Census conducted by the Statistics Bureau, Ministry of Internal Affairs and Communications of Japan (http://www.stat.go.jp/english/data/kokusei/2010/summary.html, accessed in November 2018). Patients were divided into 4 groups based on the quartiles of population density (342, 1,147, and 5,210 persons/km2). The distance between residences and hospitals were calculated with zip code tabulation area using SAS GEODIST function.
Outcome
The primary outcome for the patient’s in this study was in-hospital mortality.
Ethics
The study protocol was approved by the ethics committees of both the Japanese Circulation Society and Yokohama City University. These ethics committees waived the requirement for individual informed consent on the basis that only anonymized data were used in this study.
Statistical Analysis
All data analyses were performed using the JMP, version 12.1.0 (12.0) (SAS Institute, Inc. Cary, NC, USA), SAS 9.2 (SAS Institute, Inc.), and Stata 14.2 (StataCorp LLC, College Station, TX, USA). Patients’ baseline characteristics were compared among the quartiles of population density. Descriptive statistics were summarized as mean±standard deviation or medians (25th to 75th percentiles) for continuous variables, and percentages for categorical variables, as appropriate. The associations between categorical variables were assessed using Fisher’s exact test, and differences in continuous variables were compared by analysis of variance (ANOVA) or the Kruskal-Wallis test. Univariable regression spline models were conducted to evaluate associations of in-hospital mortality with population density or annual PCI procedure volume. The multivariable spline model compares null, linear and lower-dimensional spline models for each continuous predictor, with the most complex spline model allowed by the specification. Knots which calculate here show the knots selected as the best-fitting subject for the testing procedure. A threshold of 115 procedures per year of primary PCI for AMI was determined by using a mixed multivariable regression model in the association with in-hospital mortality, and was used to define low- (<115) and high- (≥115) volume hospitals. Mixed logistic regression models, with institution as a random intercept, were used to estimate odds ratios (ORs) for in-hospital deaths. Two hierarchy levels (hospital and patient) were included in these models to consider the random effects of hospital variation; fixed effects included age, gender, cerebrovascular diseases, chronic kidney disease, Charlson index, and Killip class. A 2-tailed P-value of <0.05 was considered statistically significant.
Results
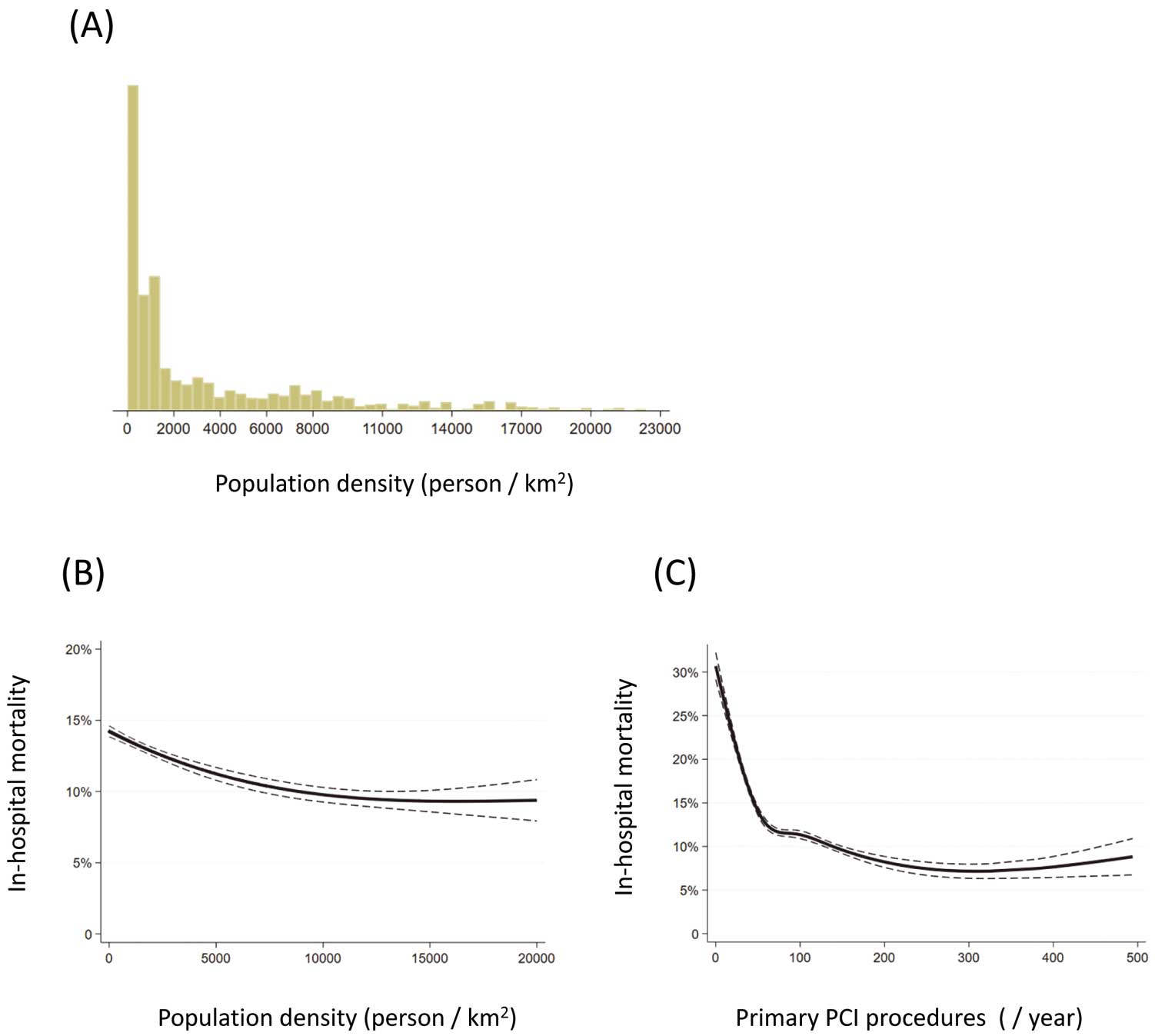
Of 2,369,165 patients listed in the JROAD-DPC database between 1 April 2012 and 31 March 2015, those aged <20 years, had non-AMI, had recurrent hospitalization within the study period, had an OHCA, were not transferred by ambulance from the scene of the event, and had missing data about population density were excluded (Supplementary Figure 1). Consequently, we analyzed 64,414 patients from 739 hospitals. One-hundred and forty hospitals were classified as high-volume primary PCI hospitals, and 599 were considered low-volume hospitals. In-hospital death was reported for 8,096 patients (12.6% of the study population). The distribution of population density is shown in
Figure 1A, and a median of population density (interquartile range) was 1,147 (342–5,210) persons/km2.
Characteristics of the Patients and Hospitals
Characteristics of the patients and hospitals according to the population density quartiles are shown in
Table 1. In addition, baseline characteristics by the hospital volume and the distance to hospitals are shown in
Supplementary Tables 1–4. The data about distance to hospital was missing from the records of 186 patients. Those living in the low-population density areas were older and more often female, and had more comorbidity. The median distance to hospital was 13.0 km in the lowest population density area, whereas it was 3.2 km in the highest population density area. In the lowest population density area, patients were hospitalized in smaller hospitals, which was measured by bed count, annual number of PCIs, CCUs, and rehabilitation facilities.
Table 1.
Characteristics of Patients According to Population Density
Population density
(person/km2) |
Total
1,147
(342–5,210) |
Population density quartile |
P value |
1st
≤342 |
2nd
342–1,147 |
3rd
1,147–5,210 |
4th
>5,210 |
| N |
64,414 |
16,114 |
16,150 |
16,069 |
16,081 |
|
| Age, years |
70.2 (13.3) |
71.5 (13.1) |
70.3 (13.3) |
69.6 (13.1) |
69.6 (13.5) |
<0.001 |
| Male gender |
71.1 |
69.4 |
71.6 |
72.0 |
71.3 |
<0.001 |
| Cerebrovascular disease |
5.2 |
6.6 |
4.9 |
4.9 |
4.6 |
<0.001 |
| Chronic kidney disease |
4.4 |
4.3 |
4.5 |
4.3 |
4.5 |
0.71 |
| Charlson comorbidity index |
2.0 (1.0) |
2.1 (1.1) |
2.1 (1.0) |
2.0 (1.0) |
2.0 (1.1) |
<0.001 |
| Killip class |
|
|
|
|
|
<0.001 |
| 1 |
50.2 |
49.7 |
49.6 |
49.0 |
52.8 |
|
| 2 |
27.6 |
28.0 |
28.3 |
27.6 |
26.4 |
|
| 3 |
8.5 |
8.5 |
8.1 |
8.6 |
8.6 |
|
| 4 |
13.7 |
13.8 |
14.1 |
14.8 |
12.2 |
|
| Killip class ≥2 |
49.8 |
50.3 |
50.4 |
51.0 |
47.2 |
<0.001 |
| Distance to hospital, km |
5.2 (2.6–11.1) |
13.0 (5.5–23.8) |
5.9 (3.1–10.6) |
4.5 (2.5–7.5) |
3.2 (1.8–5.3) |
<0.001 |
| PCI on the day of admission |
69.0 |
67.5 |
68.8 |
71.1 |
68.7 |
<0.001 |
| Admission to CCU |
38.7 |
27.7 |
36.4 |
43.0 |
47.5 |
<0.001 |
| Hospitals’ data |
| Bed count, n |
501 (234) |
470 (200) |
512 (233) |
505 (252) |
519 (245) |
<0.001 |
| PCI capable hospital |
99.6 |
99.4 |
99.5 |
99.6 |
99.9 |
<0.001 |
| Primary PCI, n/year |
108 (79) |
96 (74) |
115 (92) |
119 (89) |
101 (54) |
<0.001 |
| Annual primary PCI ≥115 |
35.0 |
25.5 |
35.6 |
44.2 |
34.6 |
<0.001 |
| Elective PCI, n/year |
236 (193) |
193 (148) |
231 (165) |
274 (244) |
248 (193) |
<0.001 |
| Coronary care unit |
94.2 |
90.4 |
94.7 |
95.4 |
96.5 |
<0.001 |
| Rehabilitation |
70.2 |
63.2 |
71.0 |
76.0 |
70.7 |
<0.001 |
Data are shown as mean (standard deviation), median (interquartile range), or percentage. CCU, coronary care unit; PCI, percutaneous coronary intervention.
To evaluate the association between population density and in-hospital mortality among AMI patients, we conducted the regression spline model (Figure 1B) and found a negative relationship between population density and in-hospital mortality; in other words, lower population density was associated with higher in-hospital mortality as a result of AMI. This relationship was similar even after adjustment for the annual number of primary PCIs (Supplementary Figure 2). In the mixed logistic regression model (see details in the “Statistical Analysis” section), one quartile down in population density was associated with an 8.6% higher risk for in-hospital mortality (OR 1.086, 95% confidence interval [CI]: 1.042–1.132, P<0.001).
Distance to Hospital or Hospital Volume?
In all the hospitals of this study, the mean annual number of primary PCI cases was 108, and the mean annual number of elective PCI cases was 236. As mentioned before, the distance to a hospital was longer and the hospital size was smaller in the low population density areas. Furthermore, patients who were hospitalized in the high-volume hospitals were transported significantly farther (Supplementary Table 3), whereas patients who were transported farther were hospitalized more often in the high-volume hospitals (Supplementary Table 4). We conducted a mixed logistic regression model to compare distance to hospital and annual number of primary PCI procedures in association with in-hospital mortality after AMI. Although distance to hospital was not significant (OR for 1 km increase: 0.9997; 95% CI: 0.9991–1.0003, P=0.31), a lower annual number of primary PCI procedures was a significantly associated factor for higher in-hospital mortality (OR for 10 procedures decreased 1.0382; 95% CI: 1.0339–1.0424, P<0.001).
Figure 1C
shows the relationship between the annual number of primary PCI procedures and in-hospital mortality by the univariable regression spline model. In-hospital mortality was dramatically increased when the annual number of primary PCIs performed was below ∼100. We evaluated the cut-off value of the annual number of primary PCI procedures in relation to the risk of in-hospital mortality after AMI using the multivariable mixed model, and the best cut-off value was 115 in this study. With this threshold (115 primary PCIs/year), hospitals were divided into low- or high-volume hospitals.
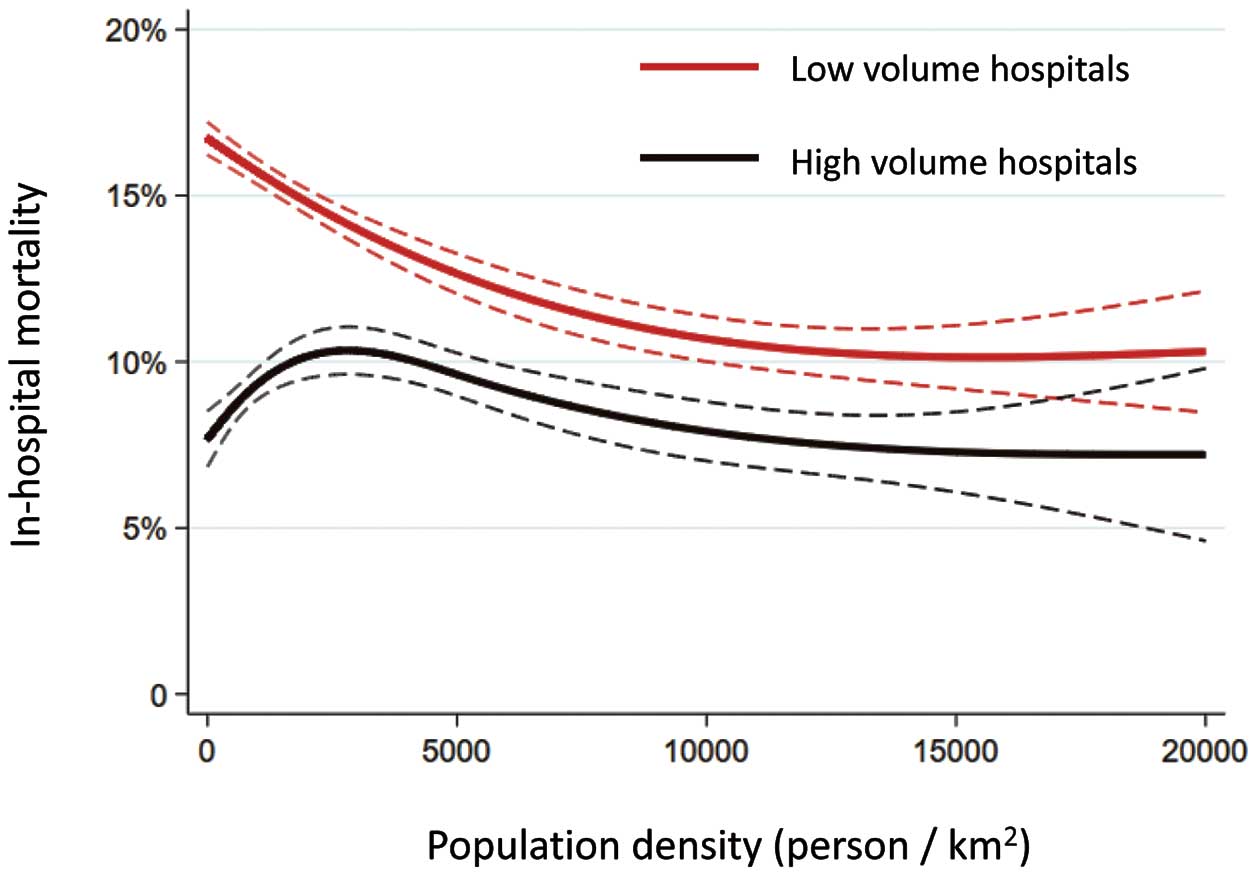
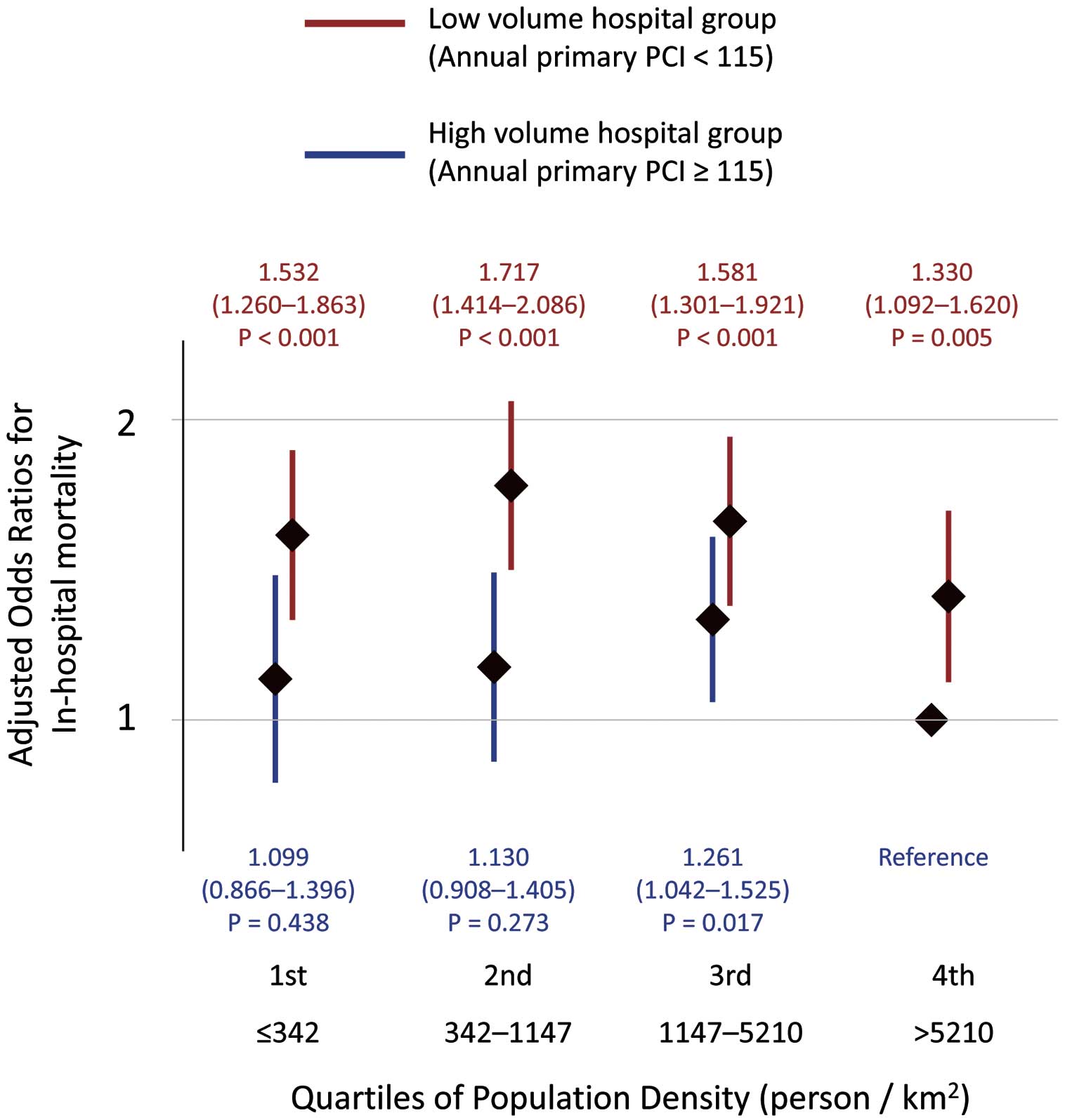
Association Between Population Density and In-Hospital Mortality According to the Primary PCI Procedure Volume
In total, 41,898 (65.0%) out of 64,414 patients were transported to the low-volume hospitals. When patients were divided into the low- and high-volume hospitals according to their hospitals, different associations between population density and in-hospital mortality were observed (Table 2, Figure 2, and
Figure 3).
Figure 2
shows crude spline curves of the relationship between population density and in-hospital mortality according to the hospital volume. Among patients who were hospitalized in the low-volume hospitals, decreasing population density was associated with high in-hospital mortality. Throughout the population density, in-hospital mortality of patients who were hospitalized in the high-volume hospitals was lower than that for low-volume hospitals, and the risk associated with the low-volume hospitals compared to high-volume hospitals increased according to decreasing population density (Table 2, Figure 3). In contrast, the risk associated with low population density was not significant in patients who were hospitalized in the high-volume hospitals (Figure 3).
Table 2.
Relative Risk of the Low Volume Hospital Compared to the High-Volume Hospital in Each Population Density Quartile
| |
Population density quartile |
| 1st |
2nd |
3rd |
4th |
OR for the low- vs. high-volume
hospitals |
1.428
(1.110–1.836)
P=0.005 |
1.405
(1.118–1.767)
P=0.004 |
1.293
(1.078–1.552)
P=0.006 |
1.415
(1.181–1.695)
P<0.001 |
Data are shown as odds ratios (ORs) and 95% confidence interval. ORs were adjusted for age, gender, cerebrovascular diseases, chronic kidney disease, Charlson index, Killip class, percutaneous coronary intervention on the day of admission, and admission to coronary care unit.
Discussion
This study found that AMI patients in the less densely populated areas had higher in-hospital mortality risk than those in the higher population density areas. In the low population density areas, distance to hospital was longer and hospital volume was smaller. By using multivariable analysis, it was found that the annual number of primary PCI procedures was significantly associated with in-hospital mortality, but distance to hospital was not. Although the cut-off of the annual number of primary PCI procedures should be discussed according to the circumstances, our results showed that 115 was the best cut-off level in association with in-hospital mortality. When the hospitals were divided into low- and high-volume and the cut-off value of 115 annual primary PCI procedures was used, the increase in in-hospital mortality associated with low population density was observed only among patients who were hospitalized in the low-volume hospitals. In contrast, among those who were hospitalized in the high-volume hospitals, in-hospital mortality did not significantly increase with a population density decrease. Our results suggest that the centralization of cardiologists and healthcare resources to increase high-volume hospitals and that patients with AMI should be triaged directly to these hospitals for high-quality primary PCI and post-reperfusion care, regardless of the distance.
Comparison of Population Density Between Japan and Other Countries
In this study, the median population density (interquartile range) was 1,147 (342–5,210) persons/km2. The population density of Japan as a whole was 337 persons/km2
in 2018. The three countries with the highest populations – China, India, and the United States of America – have population densities of 146 persons/km2, 412 persons/km2, and 35 persons/km2, respectively, and European countries such as the United Kingdom, Germany, and Italy have population densities of 274 persons/km2, 230 persons/km2, and 197 persons/km2, respectively (http://worldpopulationreview.com/countries/countries-by-density/, accessed in February 2019). Thus, the results of the current study were derived from very densely populated areas, and consistently, distances between patients’ residences and hospitals were short (the median was 5.2 km [interquartile range 2.6–11.1]). The difference in distance to hospitals was 0.9 km (Supplementary Table 3) between the low- and high-volume hospitals, which results in a difference in system delay of only a few minutes. This system delay could be negligible.
Importance of the High-Volume PCI Center for AMI
The novelty of our study is that transportation of patients with AMI to the low-volume hospitals was the major factor associated with high in-hospital mortality, especially among patients living in low population density areas in Japan, and long transportation distance was not associated with high in-hospital mortality.
The rural–urban disparity has been observed in terms of emergent diseases, including AMI. A recent study of AMI patients in Japan (1,695 patients in rural areas and 2,075 patients in urban areas) by Masuda et al9
demonstrated that AMI patients in rural areas were less likely to be transported directly to PCI-capable facilities, resulting in a time delay to primary PCI compared with those in urban areas. Numerous previous studies have reported on the relationship between the volume of PCI procedures and the outcome in patients with AMI.6,10,11
Multiple factors may contribute to the association between higher primary PCI procedure volume and lower in-hospital mortality, such as shorter door-to-balloon time; greater physician skill and judgment, derived from greater experience with these cases; and a well-coordinated, high-quality healthcare team. The current Japanese densely populated circumstances might be one reason distance to hospital was not associated with the in-hospital mortality in this study. In considering the results of the current study, it is speculated that the clinical benefit from the healthcare system in the high-volume hospitals outweighs the disadvantage caused by the small increase in distance to hospitals. Although medical conditions were different from the current study, because we excluded OHCA patients, immediate cardiopulmonary resuscitation and post-resuscitation care in emergent hospitals are crucial to the survival of patients who experience OHCA. Survival of patients who experience OHCA is much more dependent on time-to-treatment than it is for those with AMI. Our results are similar to a recent study from Denmark that included 41,186 OHCA patients.12
They reported that distance from the site of the event of OHCA to an invasive heart center was not associated with survival, whereas admission to an invasive heart center was associated with better outcomes in comparison to admission to a local hospital.
Future Perspectives
This is not a study that promotes the shift towards a concentration of the population into big cities; however, our data supports the establishment of high-volume centers and suggests that patients should field triage directly to these centers for high-quality primary PCI and post-reperfusion care, regardless of the distance, by doing pre-hospital diagnosis of AMI. A pre-hospital electrocardiogram is recommended for early diagnosis of AMI, based on the current clinical guidelines of Europe, Japan, and the USA.13–15
Under current Japanese circumstances, we propose the annual primary PCI number of 115 for the cut-off level to define high-volume hospitals. However, the annual PCI volumes, including primary and elective procedures conducted in this Japanese study, were lower than that for other countries.11
In order to achieve the best outcomes for AMI patients in each country or region, a cut-off level for the annual primary PCI number reflecting hospital volume should be assessed according to each circumstance. The pre-hospital diagnosis can be completed using the pre-hospital electrocardiogram recorded by paramedics. Interestingly, a study of ST-elevation myocardial infarction (STEMI) patients in Denmark reported that, by performing a pre-hospital electrocardiogram diagnosis of AMI, the system delay for patients living far from a PCI center was comparable to that observed in patients who lived near a PCI center, and a pre-hospital electrocardiogram diagnosis may be associated with lower mortality.16
Study Limitations
First, this is a retrospective observational study. This study can identify only associations rather than causality. The data should be interpreted with caution because of the possibility of residual confounding such as ambulance team triage, although its strengths include a large sample and the use of a wide array of clinical variables in adjusting for differences in clinical characteristics and potential confounders. Second, we are also limited because the hospitals included in this study were limited to approximately 50% of Japanese Circulation Society-certified hospitals and 29% of all hospital beds in Japan; this may introduce potential selection bias. Third, although driving time, taking into consideration traffic network issues from locations of AMI events and hospitals, should have been used, we used the Euclidean distance between residences and hospitals, and the data about location of the AMI events was not available. Fourth, reliability of the Killip classification based on DPC data might be low. Finally, these results may not be generalizable to other countries and regions. Further studies in other regions are needed.
Conclusions
Patients with AMI in less densely populated areas had higher in-hospital mortality risk than those in more densely populated areas. Distance from the patient’s residence to the hospital was not associated with in-hospital mortality in the current study, whereas transportation of patients with AMI to low-volume hospitals was associated with a high in-hospital mortality among patients living in the low population density areas in Japan. Our results support the establishment of high-volume hospitals, and suggest that patients with AMI should field triage directly to these hospitals for high-quality primary PCI and post-reperfusion care, regardless of the distance.
Funding
This study did not receive any funding.
Disclosures
The authors declare no conflicts of interest.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0869
References
- 1.
Amoah PA, Edusei J, Amuzu D. Social networks and health: Understanding the nuances of healthcare access between urban and rural populations. Int J Environ Res Public Health 2018; 15: 973–988.
- 2.
Gamble JM, Eurich DT, Ezekowitz JA, Kaul P, Quan H, McAlister FA. Patterns of care and outcomes differ for urban versus rural patients with newly diagnosed heart failure, even in a universal healthcare system. Circ Heart Fail 2011; 4: 317–323.
- 3.
Gibbons RJ, Holmes DR, Reeder GS, Bailey KR, Hopfenspirger MR, Gersh BJ. Immediate angioplasty compared with the administration of a thrombolytic agent followed by conservative treatment for myocardial infarction: The Mayo Coronary Care Unit and Catheterization Laboratory Groups. N Engl J Med 1993; 328: 685–691.
- 4.
Grines CL, Browne KF, Marco J, Rothbaum D, Stone GW, O’Keefe J, et al. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med 1993; 328: 673–679.
- 5.
Zijlstra F, de Boer MJ, Hoorntje JC, Reiffers S, Reiber JH, Suryapranata H. A comparison of immediate coronary angioplasty with intravenous streptokinase in acute myocardial infarction. N Engl J Med 1993; 328: 680–684.
- 6.
Vakili BA, Kaplan R, Brown DL. Volume-outcome relation for physicians and hospitals performing angioplasty for acute myocardial infarction in New York state. Circulation 2001; 104: 2171–2176.
- 7.
Yasuda S, Nakao K, Nishimura K, Miyamoto Y, Sumita Y, Shishido T, et al. The current status of cardiovascular medicine in Japan: Analysis of a large number of health records from a nationwide claim-based database, JROAD-DPC. Circ J 2016; 80: 2327–2335.
- 8.
Yasuda S, Miyamoto Y, Ogawa H. Current status of cardiovascular medicine in the aging society of Japan. Circulation 2018; 138: 965–967.
- 9.
Masuda J, Kishi M, Kumagai N, Yamazaki T, Sakata K, Higuma T, et al. Rural-urban disparity in emergency care for acute myocardial infarction in Japan. Circ J 2018; 82: 1666–1674.
- 10.
Canto JG, Every NR, Magid DJ, Rogers WJ, Malmgren JA, Frederick PD, et al. The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. N Engl J Med 2000; 342: 1573–1580.
- 11.
Spaulding C, Morice MC, Lancelin B, El Haddad S, Lepage E, Bataille S, et al. Is the volume-outcome relation still an issue in the era of PCI with systematic stenting? Results of the greater Paris area PCI registry. Eur Heart J 2006; 27: 1054–1060.
- 12.
Tranberg T, Lippert FK, Christensen EF, Stengaard C, Hjort J, Lassen JF, et al. Distance to invasive heart centre, performance of acute coronary angiography, and angioplasty and associated outcome in out-of-hospital cardiac arrest: A nationwide study. Eur Heart J 2017; 38: 1645–1652.
- 13.
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 61: e78–e140.
- 14.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39: 119–177.
- 15.
Kimura K, Kimura T, Ishihara M, Nakagawa Y, Nakao K, Miyauchi K, et al; on behalf of the Japanese Circulation Society Joint Working Group. JCS 2018 Guideline on diagnosis and treatment of acute coronary syndrome. Circ J 2019; 83: 1085–1196.
- 16.
Sorensen JT, Terkelsen CJ, Norgaard BL, Trautner S, Hansen TM, Botker HE, et al. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur Heart J 2011; 32: 430–436.