2020 年 84 巻 7 号 p. 1097-1104
2020 年 84 巻 7 号 p. 1097-1104
Background: How the time sequence of cardiopulmonary resuscitation (CPR) procedures is related to clinical outcomes in patients with out-of-hospital cardiac arrest (OHCA) remains unclear. This study examined the impact of the time interval from collapse to start of CPR (no-flow time, NF time) and the time interval from start of CPR to implementation of extracorporeal CPR (ECPR) (low-flow time, LF time) on neurological outcomes.
Methods and Results: During the period from 2010 to 2015, we enrolled 85 patients who received ECPR. Fourteen patients (16.5%) showed favorable 30-day neurological recovery. NF time was shorter in the favorable neurological recovery group than in the unfavorable recovery group (1.4±3.0 vs. 5.2±5.8 min, P<0.05), though combined NF+LF times were similar in the 2 groups (50.1±13.2 vs. 55.1±14.8 min, P=0.25). Multivariate logistic regression analysis indicated that pupil diameter at arrival and NF time were independently associated with favorable neurological recovery. The optimal cut-off value of NF time to predict favorable neurological recovery was 5 min (area under curve: 0.70, P<0.05; sensitivity, 85.7%; specificity, 52.1%).
Conclusions: The results suggest that NF time is a better predictor than NF+LF time for neurological outcomes in OHCA patients who received ECPR, and that start of CPR within 5 min after collapse is crucial for improving neurological outcomes followed by use of ECPR.
The survival rate with favorable neurological recovery from out-of-hospital cardiac arrest (OHCA) is still only 0.8–20.1%, despite international efforts to improve cardiopulmonary resuscitation (CPR) methods.1 For patients who failed to respond to conventional CPR, extracorporeal CPR (ECPR), a bridge therapy for restoration of spontaneous circulation (ROSC), has been suggested to improve survival rate and neurological outcomes.2 However, evidence for the clinical benefit of ECPR has not been provided by randomized clinical trials, and the latest 2019 American Heart Association guidelines have a Class 2b recommendation for considering ECPR for OHCA in selected patients in whom the etiology of cardiac arrest is reversible and in settings where it can be quickly implemented and supported by skilled providers.3–6 The optimal patient selection and optimal timing for implementation of ECPR have not been established.
Accumulating evidence suggests that total collapse duration; that is, the time interval from cardiac arrest to ROSC, is an independent prognostic factor in patients with OHCA,7–9 and that the same is true for the time interval from cardiac arrest to ECPR implementation in patients with refractory OHCA.10–14 The total collapse duration includes the time interval from collapse to the start of CPR (no flow time, NF time) and the time interval from CPR to ROSC (low flow time, LF time). NF time is recognized as the most crucial determinant of outcomes of CPR, and prolonged NF time is included in the exclusion criteria for advanced CPR in some of institutions.4,12 A detrimental effect of longer LF time on functional recovery has been suggested by poorer outcomes of OHCA than those of in-hospital cardiac arrest (IHCA).15–17 Furthermore, a recent meta-analysis indicated that shorter LF time is independently associated with better neurological outcomes in ECPR recipients.10 Several approaches to minimize the LF duration, including early decision for switching from conventional CPR to ECPR and a pre-hospital ECPR program with a mobile intensive care unit (MICU), have been proposed.18,19 In contrast, a recent study has suggested that NF time and LF time interact in terms of their effects on clinical outcome in OHCA patients.20 However, the relationships of NF time and LF time with clinical outcomes, particularly neurological outcomes, in OHCA patients who received ECPR have remained unclear. Thus, we addressed this issue focusing on neurological outcomes in the present study.
This study was conducted in strict adherence with the principles of the Declaration of Helsinki, and was approved by the Clinical Investigation Ethics Committee of Sapporo Medical University Hospital (Number 312-112). De-identified participant data will not be shared in public.
Study Subjects and Definitions of Time IntervalsThis study was a single center, retrospective, and observational study. We retrieved data for 1,630 consecutive patients with OHCA of endogenous origin who were admitted during the period from January 2010 to October 2015 to the Advanced Critical Care and Emergency Center of Sapporo Medical University Hospital, which comprised 18 beds of the 938 beds in the university teaching hospital. Of those patients, we enrolled 85 patients in whom ECPR was implemented for cardiac causes of OHCA, as shown in Figure 1. ECPR was implemented according to the institutional criteria: (1) age <75 years; (2) presumed cardiac origin in accordance with the recommendation of the Utstein consensus conference; (3) collapse witnessed by a bystander or reliable report of estimated collapse time; and (4) refractory ventricular fibrillation that failed to respond to conventional CPR before arrival at the hospital. Exclusion criteria were: (1) age ≥76 years; (2) cardiac tamponade caused by aortic dissection; (3) non-cardiac origin including severe trauma, stroke, and aortic dissection; and (4) known poor prognosis or terminal malignancies. Patients who met at least one of the exclusion criteria were not included in the present analysis. We did not include the time interval from collapse to arrival at the hospital in the exclusion criteria.

Flow chart of study subject selection. OHCA, out-of-hospital cardiac arrest; ECPR, extracorporeal cardiopulmonary resuscitation; CCU, coronary care unit; ROSC, restoration of spontaneous circulation.
In accordance with earlier studies,7,9 we defined NF time as the time interval from collapse to the start of CPR, and we defined LF time as the interval from the start of CPR to ECPR implementation. In the present study, the sum of NF time and LF time was defined as total collapse duration.
Procedure for ECPRImmediately after arrival at the hospital, percutaneous cannulation of the femoral artery with a 16 French-size catheter and cannulation of the vein with a 20 French-size catheter were performed using a fluoroscope. The extracorporeal membrane oxygenation (ECMO) system consisted of a centrifugal pump (TERUMO, Tokyo, Japan) and an oxygenator module (SENKO Medical Instrument, Tokyo, Japan). Operation of the ECMO system was started immediately after cannulation had succeeded. In cases with suspected acute coronary syndrome, emergency coronary angiography (CAG) was performed and percutaneous coronary intervention (PCI) was also performed. Intra-aortic balloon counter-pulsation (IABP) was also introduced to support cardiac function in the patients if there was no contraindication to IABP. Targeted temperature management (TTM) was performed in unconscious patients with a Glasgow coma scale (GCS) score <7 after ECPR implementation. In TTM, core body temperature was lowered to 34 degrees Celsius and maintained by the ECMO heat exchanger for 24 h and then patients were gradually rewarmed for at least 12 h to discontinue hypothermia.
Clinical EndpointThirty-day neurological outcome was evaluated using Glasgow–Pittsburgh Cerebral Performance Categories (CPC): good recovery (CPC 1); moderate disability (CPC 2); severe disability (CPC 3); vegetative state (CPC 4); and death (CPC 5).21 In the present study, favorable neurological recovery was defined as CPC 1 or 2, and unfavorable recovery was defined as CPC 3, 4 or 5.
Statistical AnalysisContinuous variables are represented as means±standard deviation, and categorical variables are presented as numbers and relative frequencies. Differences between the 2 groups were tested by using the Student’s t-test for continuous variables and by the chi-squared test for categorical variables. Multivariate logistic regression models were used to assess the independent prognostic values of variables. All statistical analyses were performed using JMP (version 11 SAS Institute, Cary, NC, USA). A P-value of <0.05 was considered statistically significant.
Baseline clinical characteristics of the study subjects (age, 56.7±11.6 years; 82.4% males) are shown in Table 1. Collapse was witnessed by bystanders or by emergency medical staff in 70 (82.4%) of the 85 patients, and 43 patients (50.6%) received bystander CPR. In their first monitored rhythm, 70 patients (82.4%) showed ventricular fibrillation or ventricular tachycardia. Emergency CAG was performed in 81 patients (95.3%). According to the angiographic and echocardiographic findings, 52 patients (61.2%) were diagnosed with acute coronary syndrome, including 49 with acute myocardial infarction and 3 with unstable angina pectoris, and 9 patients (10.6%) were diagnosed with previous myocardial infarctions. Emergency PCI was performed in 47 patients (55.3%). Thirty-two patients (37.6%) survived for 30 days after the onset of OHCA, and 14 patients (16.5%) showed favorable neurological recovery.
| Overall (n=85) |
Favorable group (n=14) |
Unfavorable group (n=71) |
P value | |
|---|---|---|---|---|
| Age (years) | 56.7±11.6 | 51.1±8.2 | 57.8±11.9 | 0.0478 |
| Male | 70 (82.4) | 10 (71.4) | 60 (84.5) | 0.24 |
| Location of cardiac arrest | ||||
| At home | 35 (41.2) | 6 (42.9) | 29 (40.9) | 0.89 |
| In ambulance | 9 (10.6) | 4 (28.6) | 5 (7.0) | 0.0167 |
| Others | 41 (48.2) | 4 (28.6) | 37 (52.1) | 0.11 |
| AED | 8 (9.4) | 0 (0.0) | 8 (11.3) | 0.19 |
| Bystander witness | 70 (82.4) | 13 (92.9) | 57 (80.3) | 0.26 |
| Bystander CPR | 43 (50.6) | 11 (78.6) | 32 (45.1) | 0.0219 |
| Initial shockable rhythm (VF or VT) | 70 (82.4) | 12 (85.7) | 58 (81.7) | 0.72 |
| Number of defibrillations before arrival | 2.6±1.8 | 2.6±1.9 | 2.6±1.8 | 0.88 |
| GCS >3 at arrival | 5 (5.9) | 3 (21.4) | 2 (2.8) | 0.0068 |
| Pupil diameter at arrival (mm) | 5±1.8 | 4.1±1.1 | 5.2±1.2 | 0.0023 |
| Pupillary reflex at arrival | 7 (8.2) | 3 (21.4) | 4 (5.6) | 0.0494 |
| Laboratory data at arrival | ||||
| pH | 6.92±0.17 | 6.96±0.15 | 6.91±0.17 | 0.36 |
| Lactic acid | 120.4±44.1 | 126.8±42.2 | 119.1±44.7 | 0.57 |
| eGFR | 54.6±18.6 | 53.4±19.1 | 54.9±18.6 | 0.79 |
| Cause of cardiac arrest | ||||
| Acute coronary syndrome | 52 (61.2) | 10 (71.4) | 42 (59.2) | 0.39 |
| Previous myocardial infarction | 9 (10.6) | 0 (0.0) | 9 (12.7) | 0.16 |
| Others | 24 (28.2) | 4 (28.6) | 20 (28.2) | 0.98 |
| Emergency CAG | 81 (95.3) | 13 (92.9) | 68 (95.8) | 0.64 |
| Emergency PCI | 47 (55.3) | 7 (50.0) | 40 (56.3) | 0.66 |
| IABP | 80 (94.1) | 13 (92.9) | 67 (94.4) | 0.83 |
| TTM | 81 (95.3) | 13 (92.9) | 68 (95.8) | 0.64 |
| Collapse-to-hospital arrival (min) | 35.8±11.4 | 32.3±13.9 | 36.5±10.8 | 0.21 |
| Arrival-to-ECPR implementation (min) | 19.3±8.4 | 20.1±7.5 | 19.2±8.6 | 0.7 |
| Total collapse duration (min) | 54.2±14.6 | 50.1±13.2 | 55.1±14.8 | 0.25 |
| NF time (min) | 4.6±5.6 | 1.4±3.0 | 5.2±5.8 | 0.0194 |
| LF time (min) | 49.6±13.4 | 48.7±13.7 | 49.8±13.5 | 0.78 |
Data are presented as mean value±standard deviation or number (percentage) of patients. AED, automated external defibrillator; CPR, cardiopulmonary resuscitation; CAG, coronary angiography; ECPR, extracorporeal CPR; eGFR, estimated glomerular filtration rate; GCS, Glasgow coma scale; IABP, intra-aortic balloon counter-pulsation; LF time, low-flow time; NF time, no-flow time; PCI, percutaneous coronary intervention; TTM, targeted temperature management; VF, ventricular fibrillation; VT, ventricular tachycardia.
In a comparison between a group of patients with favorable neurological recovery (CPC 1–2) and a group of patients with unfavorable recovery (CPC 3–5), patients in the favorable recovery group were younger than those in the unfavorable recovery group (51.1±8.2 vs. 57.8±11.9 years, P=0.0478) and had a higher prevalence of cardiac arrest in an ambulance (28.6% vs. 7.0%, P=0.0167) and bystander CPR (78.6% vs. 45.1%, P=0.0219) than those in the unfavorable recovery group (Table 1). GCS was more frequently >3, pupil reflex was more frequently positive, and pupil diameter was smaller at admission in the favorable recovery group than in the unfavorable recovery group. In contrast, there were no significant differences between the 2 groups in the frequency of bystander witness, usage of automated external defibrillator (AED), initial shockable cardiac rhythm, number of defibrillation attempts before arrival, time interval from collapse to hospital arrival, time interval from hospital arrival to ECPR, prevalence of acute coronary syndrome (ACS), indices of tissue hypoxia (arterial pH and blood lactate level) and indices of renal function (estimated glomerular filtration rate (eGFR)). The proportions of patients who received TTM, CAG, PCI, and IABP were similar in the 2 groups.
The mean total collapse duration, NF time and LF time in patients were 54.2±14.6 min, 4.6±5.6 min and 49.6±13.4 min, respectively. NF time was significantly shorter in the favorable recovery group than in the unfavorable recovery group (1.4±3.0 vs. 5.2±5.8 min, P=0.0194). However, there was no significant difference between the 2 groups in terms of LF time (48.7±13.7 vs. 49.8±13.5 min, P=0.78) or total collapse duration (50.1±13.2 vs. 55.1±14.8 min, P=0.25; Table 1).
Predictors of 30-Day Favorable Neurological RecoveryResults of univariate and multivariate logistic regression analyses are shown in Table 2. Univariate analysis indicated significant increases in the odds ratio of favorable recovery from cardiac arrest in an ambulance, bystander CPR, GCS >3, reduced pupil diameter at arrival and shorter NF time. In multivariate analysis, GCS >3, pupil diameter at arrival and NF time (OR: 0.84, 95% CI: 0.67–0.99, P=0.022) were selected as variables having independent associations with change in the odds ratio for favorable neurological recovery (Table 2). In contrast to NF time, LF time and total collapse duration were not significantly associated with change in the odds ratio for favorable recovery. In receiver operating characteristic curve (ROC) analysis, the optimal cut-off value of NF time to predict a favorable neurological outcome was 5 min (area under the curve: 0.70, P=0.0065), of which sensitivity and specificity were 85.7% and 52.1%, respectively (Figure 2A). Considering this NF cut-off value, we divided the patients into a group with NF time ≤5 min (n=46), a group with NF time of 5–10 min (n=26) and a group with NF time ≥11 min (n=13), and we compared the rates of favorable recovery at 30 days (Figure 2B). The rate of favorable neurological recovery (CPC1–2) in the group with NF time <5 min (26.1%, 12/46) was higher than the rates in the group with NF time of 5–10 min (7.7%, 2/26) and the group with NF time ≥11 min NF (0%, 0/13).
| Predictors | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age | 0.95 | 0.9–1 | 0.0503 | |||
| Male | 0.46 | 0.13–1.9 | 0.26 | |||
| Cardiac arrest at home | 1.09 | 0.33–3.45 | 0.89 | |||
| Cardiac arrest in ambulance | 5.28 | 1.15–23.5 | 0.0338 | |||
| Bystander witness | 3.19 | 0.56–60.4 | 0.22 | |||
| Bystander CPR | 4.47 | 1.27–21 | 0.0186 | |||
| Initial shockable rhythm | 1.34 | 0.31–9.3 | 0.71 | |||
| Number of defibrillations before arrival | 1.02 | 0.74–1.39 | 0.88 | |||
| GCS >3 at arrival | 9.41 | 1.41–77.9 | 0.0218 | 8.49 | 0.85–141.3 | 0.07 |
| Pupil diameter at arrival | 0.48 | 0.28–0.78 | 0.0026 | 0.48 | 0.27–0.81 | 0.0052 |
| Pupillary reflex at arrival | 4.57 | 0.81–23.62 | 0.08 | |||
| Serum pH at arrival | 5.37 | 0.15–218.65 | 0.35 | |||
| Serum lactic acid at arrival | 1 | 0.99–1.02 | 0.57 | |||
| eGFR at arrival | 0.99 | 0.96–1.03 | 0.78 | |||
| Total collapse duration | 0.97 | 0.93–1.02 | 0.23 | |||
| NF time | 0.81 | 0.65–0.95 | 0.0065 | 0.84 | 0.67–0.98 | 0.022 |
| LF time | 0.99 | 0.95–1.04 | 0.78 | |||
CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.

Relationship between no-flow time (NF) and favorable neurological recovery. (A) Receiver operating curve (ROC) analysis for cut-off value of NF time to predict favorable neurological recovery (area under curve, 0.70, P<0.05; sensitivity, 85.7%; specificity, 52.1%). (B) Relationship between NF and cerebral performance category (CPC) rate on day 30. The rate of favorable neurological recovery rate (CPC1–2) was 26.1% (12/46) in a group with NF time ≤5 min, 7.7% (2/26) in a group with NF time from 6 to 10 min, and 0% (0/13) in a group with NF time ≥11 min.
As logistic regression analysis did not indicate a significant association between total collapse duration and neurological recovery, we examined whether the rate of favorable neurological recovery differs between tertiles of total collapse duration. As shown in Figure 3, there was a trend for a lower rate of favorable recovery in the upper tertile group, but differences between the 3 tertile groups were not statistically significant.
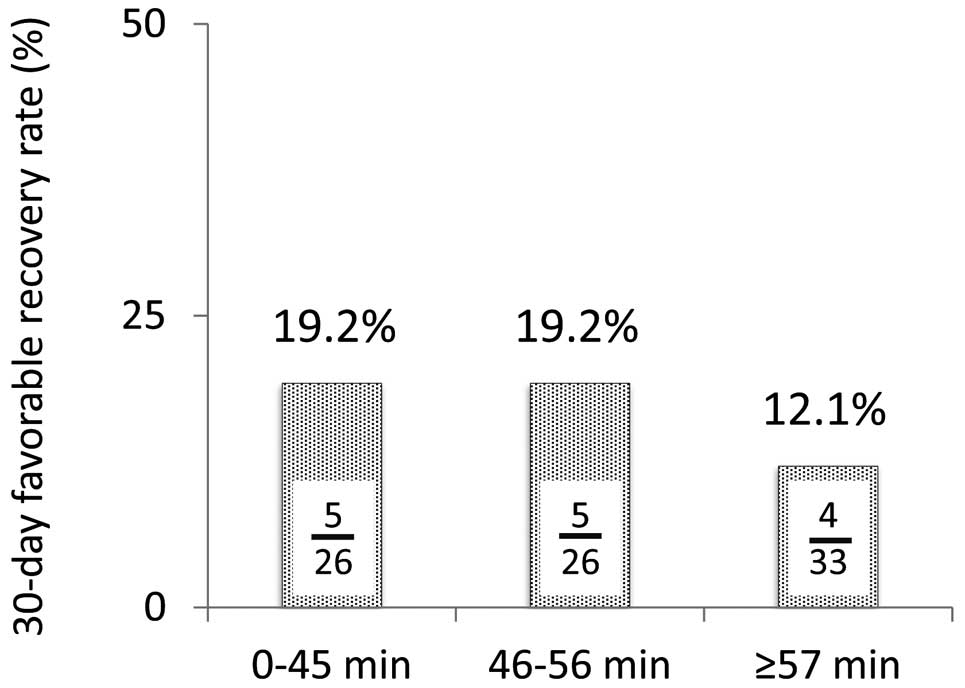
Relationship between favorable neurological recovery and total collapse duration. Rates of favorable neurological recovery are shown for tertiles of total collapse duration.
OHCA patients with total collapse duration exceeding 60 min were often excluded from the total number of study subjects in earlier investigations because the duration was thought to be too long for CPR to be successful.22 However, we did not exclude study subjects by such a criterion for total collapse duration. In fact, 24 patients (28.2%) had a total collapse duration of >60 min (mean duration: 73.8±9.7 min, 70.8% males), and 21 and 10 patients in this subgroup of patients were OHCA-witnessed and afforded bystander CPR, respectively. Of the 24 patients with a total collapse duration of >60 min, 7 patients (29.2%) survived and 3 patients (12.5%) showed favorable neurological recovery at 30 days. Notably, the 3 patients had NF time ≤5 min (Figure 4), suggesting the importance of short NF time for favorable recovery in patients with longer total collapse duration.

Favorable recovery rates in subgroups of patients with total collapse duration exceeding 60 min; patients with NF time ≤5 min vs. patients with NF time ≥6 min.
Although a criterion for NF time (up to 15 min) is commonly included in the indication for ECPR,4,7 the relationship between NF time and clinical outcome in ECPR recipients has not been fully characterized. To address this issue, we enrolled only patients in whom reliable data for NF time and LF time were obtained as study subjects. Results of multivariate logistic regression analysis suggested that NF time is a better predictor than total collapse duration or LF time of neurological outcomes in OHCA patients who received ECPR. To the best of our knowledge, this is the first report showing the impact of NF time on neurological recovery in ECPR-treated OHCA patients.
Associations of NF time and LF time with clinical outcomes in patients with OHCA have been characterized in recent studies.23,24 Hasselqvist-Ax et al analyzed data for 30,381 OHCA patients in the Swedish Cardiac Arrest Registry and showed an inverse correlation between NF time and 30-day survival rate.25 Using data from 27,301 OHCA patients, Adnet et al recently reported that 30-day survival with CPC 1–2 is predicted by combining data for NF time and LF time, and that the incidence of ROSC is dependent not only on LF time but also on NF time.20 However, the effect of ECPR therapy on the associations of NF time and LF time with clinical outcomes in OHCA patients has not been clarified. Interestingly, ECPR appears to shift the inverse relationship between LF time and survival rate toward the right (i.e., longer LF time),9,26 possibly by reduction in the incidence of “post-cardiac arrest syndrome”.27 In the present study, the optimal cut-off value of NF time to predict a favorable neurological outcome was calculated to be 5 min, and 26.1% of the patients with NF time of <5 min achieved neurological recovery to the CPC 1–2 level (Figure 2). Furthermore, a benefit was found also in subgroup analysis of patients with total collapse duration of >60 min (Figure 4). In contrast, LF time, per se, was not an independent predictor of neurological recovery (Table 2). Taken together, the findings support the notion that ECPR attenuates the detrimental effect of long LF time, and consequently, makes NF time a predominant determinant of neurological recovery in OHCA patients.
A recently published international multi-center consensus recommends implementation of ECPR within 60 min of collapse.12 This recommendation is supported by several reports, including a report showing that the rate of favorable neurological recovery sharply decreased after 16 min of conventional CPR,7 and a report showing that the best discriminative duration of conventional CPR for favorable recovery was 21 min, whereas ECPR afforded better recovery than conventional CPR for a CPR duration of 21–80 min.28 In contrast, the influence of total collapse time on the clinical benefit of ECPR remains unclear, though long total collapse time is frequently used as a criterion for exclusion of ECPR from alternative therapeutic options or for discontinuation of CPR. Prolonged collapse duration causes post-cardiac arrest syndrome, potentially leading to mortality via multiple organ failure in OHCA patients. In fact, Le Guen et al reported that favorable neurological recovery was found in only 4% of OHCA patients in whom LF time exceeded 75 min, despite NF time being <5 min.29 A study by Wang et al also showed that there was a trend for patients with longer LF time to have a lower rate of favorable outcomes.30 However, favorable neurological recovery was observed in 27.3% of a subgroup of patients with total collapse duration of ≥60 min and NF time of <5 min in the present study (Figure 4). This finding is consistent with case reports showing that immediate start of conventional CPR followed by ECPR saved patients with prolonged cardiac arrest.31,32 The level of organ perfusion during LF in OHCA patients is likely to depend on multiple factors, including the quality of CPR, cause of cardiac arrest and pre-existing organ damage. Thus, the present study findings suggest that a total collapse duration of 60 min does not preclude the benefit of ECPR in OHCA patients if NF time is <5 min.
A NF time >5 min is adopted as a contraindication for ECPR in some guidelines and studies.33–35 In contrast, there are also studies in which patients with NF time up to 15 min were enrolled for ECPR.4,7 In the focused update to the American Heart Association–Advanced Life Support (AHA–ACLS) guideline,3 ECPR for OHCA is a class 2b recommendation with evidence level of C with Limited Data, and its specific contraindication is not described. In the present study, we focused on the cut-off value of NF time for prediction of the favorable neurological recovery and showed that the ideal cut-off value is 5 min.
Although NF time is an established determinant of clinical outcomes in OHCA patients who received CPR, it is not always possible in an emergency room to know the precise time of collapse in OHCA patients. A witness of the collapse has been reported to be present in approximately 50–70% of OHCA cases.1,14,36 Recently, Tanguay-Rioux et al proposed that initial rhythm in electrocardiogram is useful as a surrogate marker of short NF time.37 They retrieved data for 2,532 OHCA patients in a prospective registry in British Colombia and found that 94% (95% confidence interval: 92–96%) of the patients with initial shockable rhythms (ventricular fibrillation or pulseless ventricular tachycardia) had NF time of <10 min. In the present study, NF time was significantly shorter in the favorable neurological recovery group than in the unfavorable neurological recovery group (1.4±3.0 vs. 5.2±5.8 min), but there was no significant difference in the prevalence of initial shockable rhythm between the 2 groups (85.7% vs. 81.7%). Together with the results reported by Tanguay-Rioux et al,37 the present study findings support the notion that initial shockable rhythm is a surrogate maker of NF time of <10 min, and also suggest that functional prognosis differs depending on NF time even at a range within 10 min. Nevertheless, the validity of initial rhythm as a surrogate marker of NF time needs to be confirmed in different populations because causes of OHCA are not the same in populations with different backgrounds for genetics, lifestyle and environment.
There are several limitations in the present study. First, because of the retrospective observational design in a single tertiary center, possible influences of selection bias in study subjects and lack of randomization of therapeutic interventions on the results cannot be excluded. Second, in 18% of the study subjects, direct witnesses were lacking and reports of estimated collapse times, which attending physicians judged as reliable, were used for the calculation of NF time. Third, because we did not include a specific duration of pre-hospital CPR in the inclusion or exclusion criteria, patients with a relatively long pre-hospital CPR might have been excluded from ECPR implementation and thus from the study subjects. Finally, data for the quality of pre-hospital CPR were not available. The time interval from collapse to hospital arrival was only 35.8±11.4 min and the number of defibrillation attempts before hospital arrival was 2.6±1.8 times. Those parameters were not significantly different between the favorable neurological recovery group and the unfavorable recovery group (Table 1). However, we cannot totally exclude the possibility that different qualities of pre-hospital CPR in the study subjects confounded the results of multivariate analysis.
The results of the present study suggest that NF time is a better predictor than LF time and total collapse duration for neurological outcomes in OHCA patients who received ECPR. Commencement of conventional CPR within 5 min after collapse may be crucial for improving neurological outcomes followed by use of ECPR, and such ECPR combined with short NF time may afford a clinical benefit, even in cases with total collapse duration of >60 min.
The authors thank all medical personnel at the Advanced Critical Care and Emergency Center, Sapporo Medical University Hospital for their help in this project. This study was supported by an Education and Research Grant 2017–2018 (to T.M.) from Sapporo Medical University and a grant (to J. Nishida) from Hokkaido Heart Association, Sapporo, Japan.
T.M. is a Circulation Journal Associate Editor. All other authors declare that they have no conflicts of interest.
This study was approved by the Clinical Investigation Ethics Committee of Sapporo Medical University Hospital (Number 312-112).