Abstract
Background: Contrast-induced nephropathy (CIN) is a frequent complication in patients undergoing percutaneous coronary intervention (PCI). The degree of recovery of renal function from CIN may affect long-term prognosis. N-terminal pro B-type natriuretic peptide (NT-proBNP) is a simple but useful biomarker for predicting CIN. However, the predictive value of preprocedural NT-proBNP for CIN non-recovery and long-term outcomes in patients undergoing PCI remains unclear.
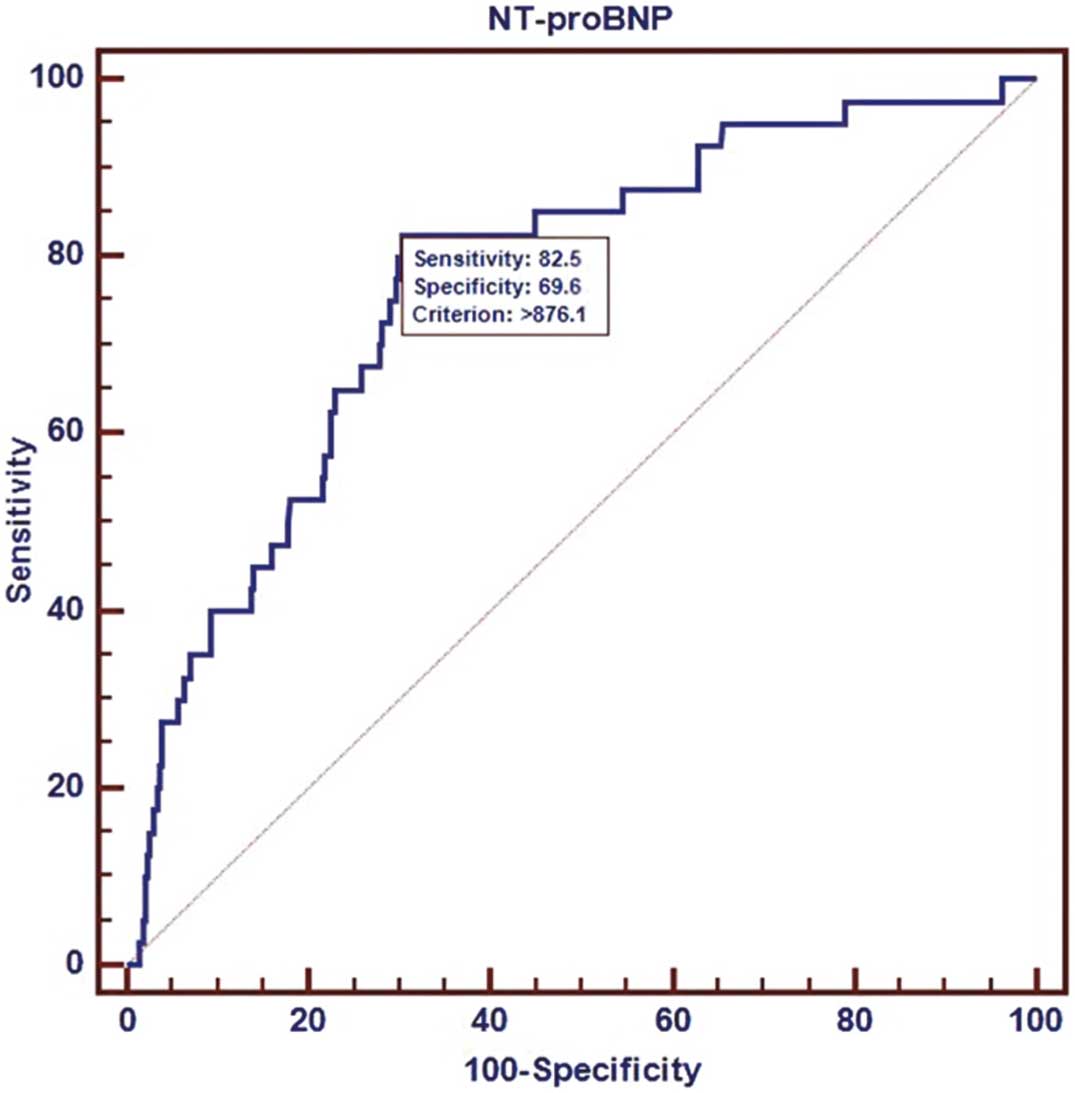
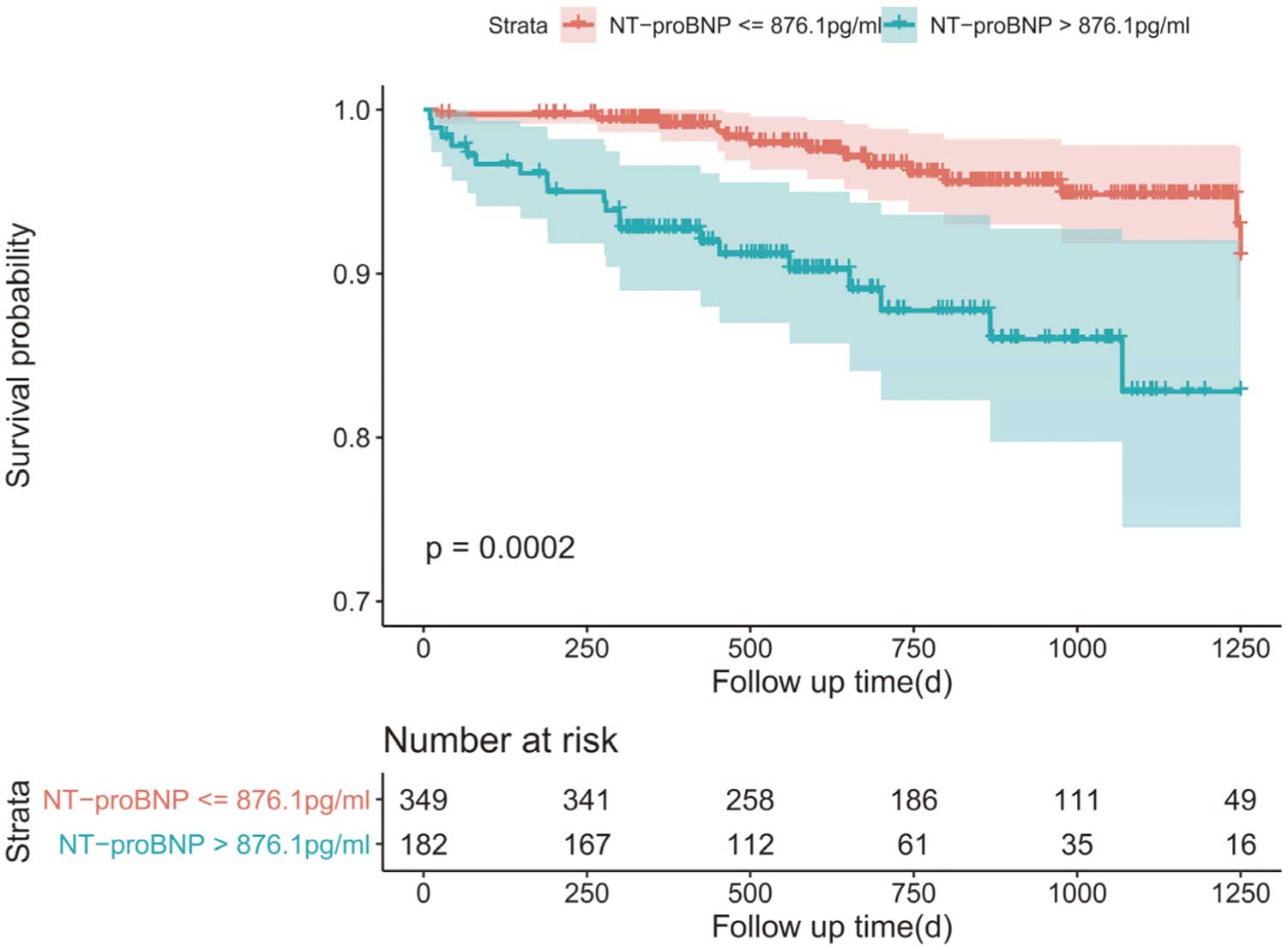
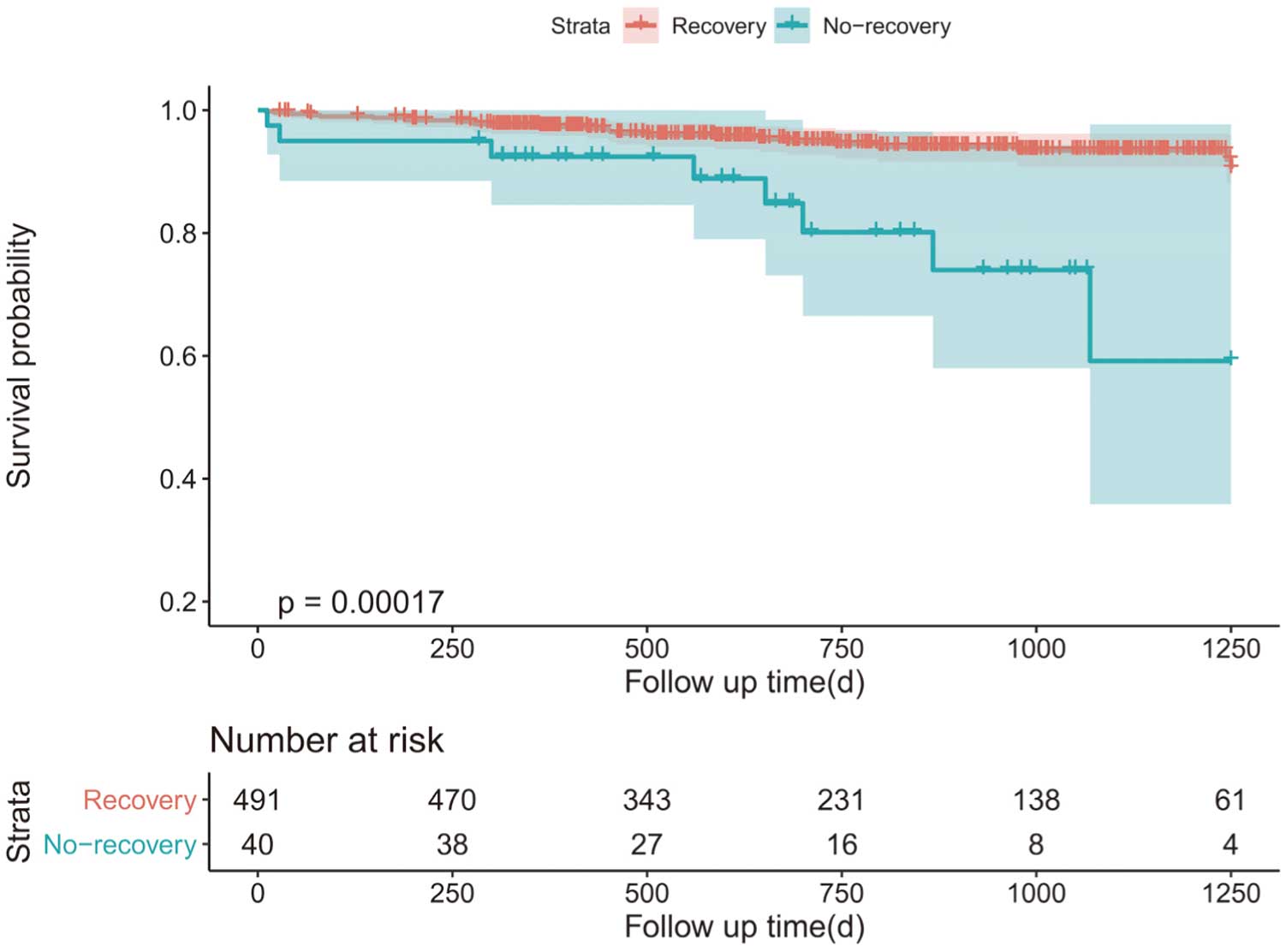
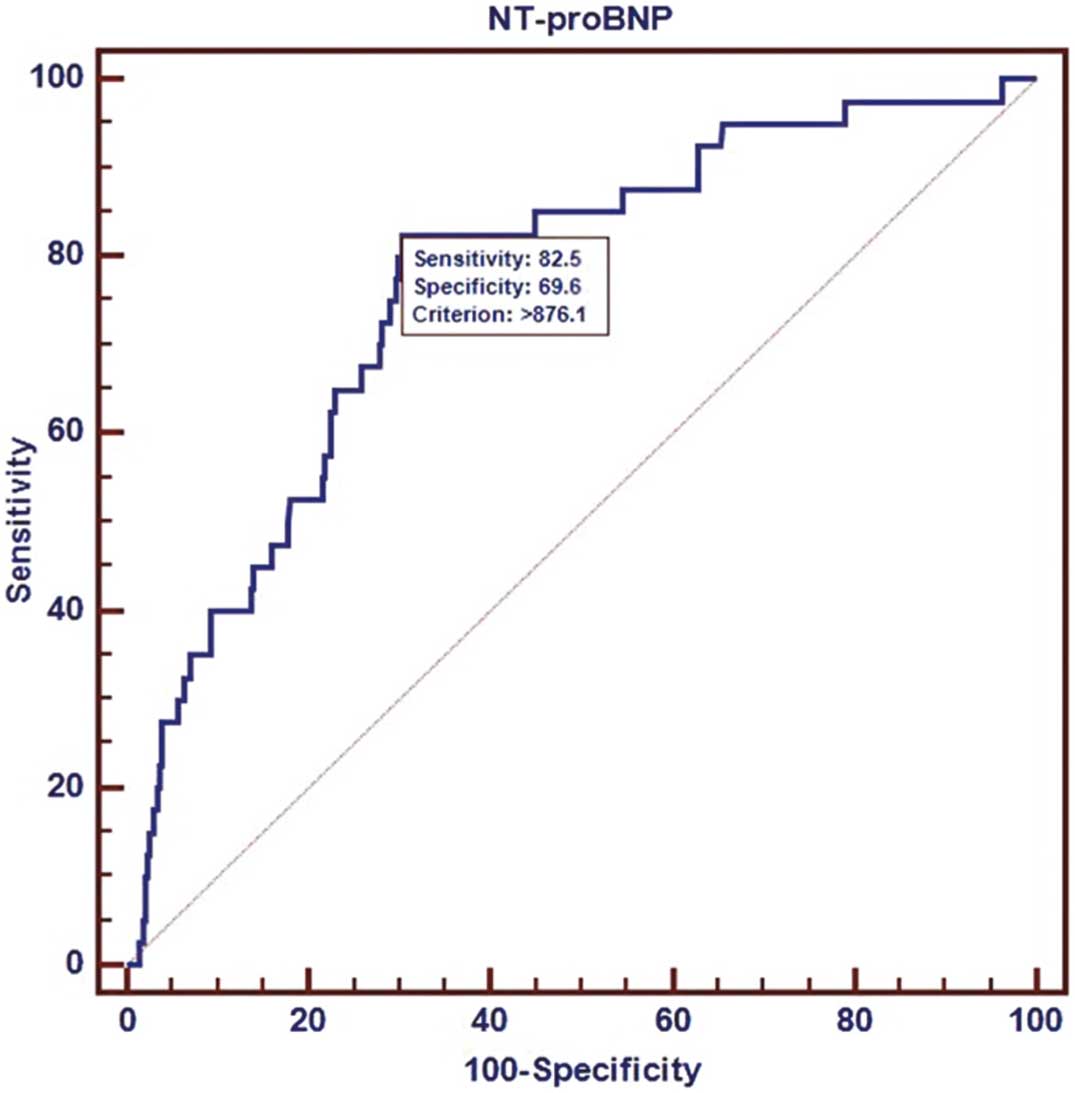
Methods and Results: This study prospectively enrolled 550 patients with CIN after PCI between January 2012 and December 2018. CIN non-recovery was defined as persistent serum creatinine >25% or 0.5 mg/dL over baseline from 1 week to 12 months after PCI in patients who developed CIN. CIN non-recovery was observed in 40 (7.3%) patients. Receiver operating characteristic analysis indicated that the best NT-proBNP cut-off value for detecting CIN non-recovery was 876.1 pg/mL (area under the curve 0.768; 95% confidence interval [CI] 0.731–0.803). After adjusting for potential confounders, multivariable analysis indicated that NT-proBNP >876.1 pg/mL was an independent predictor of CIN non-recovery (odds ratio 1.94; 95% CI 1.03–3.75; P=0.0042). Kaplan-Meier curves showed higher rates of long-term mortality among patients with CIN non-recovery than those with CIN recovery (Chi-squared=14.183, log-rank P=0.0002).
Conclusions: Preprocedural NT-proBNP was associated with CIN non-recovery among patients undergoing PCI. The optimal cut-off value for NT-proBNP to predict CIN non-recovery was 876.1 pg/mL.
Contrast-induced nephropathy (CIN) is one of the most frequent complications arising after coronary angiography or coronary intervention therapy. CIN can lead to increased mortality, longer hospitalization stays, and higher treatment expenses.1–4 Many clinicians may overlook or even neglect CIN because it is transient and generally reversible renal damage;5,6 however, kidney function may continue to deteriorate after CIN,7,8 which eventually leads to unrecoverable renal function damage and higher mortality rates. Therefore, it is of great importance to identify patients who are susceptible to CIN non-recovery so that early preventive measures can be taken in this population.
Editorial p 266
N-terminal pro B-type natriuretic peptide (NT-proBNP) is the inactive 76-amino acid N-terminal fragment following cleavage of the pro-BNP, which is secreted by cardiomyocytes in response to cardiac stretch or ischemia.9 NT-proBNP is a practical and available biomarker associated with both cardiac and renal function.10 Recent studies have indicated that NT-proBNP can independently predict CIN after coronary angiography or percutaneous coronary intervention (PCI), including in patients with heart failure (HF),11 acute coronary syndrome (ACS),12 ST-elevation myocardial infarction (STEMI),13 and chronic kidney disease (CKD).14 However, the relationships between the NT-proBNP and the occurrence of CIN non-recovery and poor outcomes among patients undergoing PCI have not been well examined. Therefore, in a prospective single-center registry of patients undergoing PCI, we sought to explore the predictive value of elevated preprocedural NT-proBNP concentrations for CIN non-recovery in patients undergoing PCI.
Methods
Study Population
We conducted a prospective observational study at Fujian Provincial Hospital, Fujian Cardiovascular Institute, between January 2012 and December 2018. In all, 6,753 consecutive patients who underwent PCI for coronary artery disease were enrolled. Of these, 646 patients developed CIN after PCI, with kidney function reassessed from 1 week to 12 months after discharge. Patients were excluded from the study if they had end-stage renal disease (estimated glomerular filtration rate [eGFR] <15 mL/min/1.73 m2) or long-term dialysis treatment; n=10); died within 1 week after PCI (n=25); lacked data on serum creatinine (SCr; n=40); had cancer with a life expectancy <1 year (n=8); had been injected with contrast medium within the previous 7 days (n=7); or had used non-steroidal anti-inflammatory drugs or other nephrotoxic drugs within the 48 h prior to the procedure (n=6). Thus, 550 patients were included in the analysis.
The Ethics Committee of the Fujian Provincial Hospital approved this study, and written informed consent was obtained from all patients.
Definitions and Follow-up
CIN was defined as an absolute increase in SCr of 0.5 mg/dL or a relative increase in SCr of ≥25% within 48 h after exposure to contrast medium.15 CIN non-recovery was defined as SCr persistently >25% or 0.5 mg/dL over baseline from 1 week to 12 months after PCI in patients who developed CIN. Anemia was defined as hemoglobin <120 g/L in men or <110 g/L in women. Based on eGFR, CKD was divided into Stage 1 (eGFR ≥90 mL/min/1.73 m2) and Stages 2–4 (eGFR 15–89 mL/min/1.73 m2).
All patients included in the study were followed up by trained nurses either during outpatient clinical visits or via telephone conversations with the patients or their relatives after discharge. CIN non-recovery was assessed at 1 week and 3 and 12 months after discharge. The primary endpoint was the occurrence of CIN non-recovery. An additional endpoint was long-term mortality.
Study Protocol
NT-proBNP was measured using an electrochemiluminescence immunoassay (Roche Diagnostics, Germany) prior to PCI. SCr concentrations were measured at admission, 2 consecutive days after the procedure, at discharge, and from 1 week to 12 months after discharge. eGFR was evaluated using the level-modified Modification of Diet in Renal Disease equation:16
eGFR = 186.3 × SCr−1.154 × Age−0.203 × 1.212 (if the patient was Black) × 0.742 (if the patient was female)
Left ventricular ejection fraction (LVEF) was evaluated by echocardiography during hospitalization. All patients received 0.9% normal saline hydration at a rate of 1 mL/kg/h for 12 h during the perioperative period at the discretion of clinicians, except patients with chronic HF, who received saline hydration at a rate of 0.5 mL·kg−1·h−1. Relevant baseline, clinical, and laboratory data were recorded during the hospital stay.
PCI
PCI was performed using standard techniques, including standard guide catheters, guidewires, balloon catheters, and stents via the femoral or radial approach according to current guidelines.17 Non-ionic, low-osmolar contrast medium (either Iopamiron or Ultravist; both 370 mg I/mL) was used in all patients. The contrast dose and pharmacologic therapies were left to the discretion of cardiologists based on the patient’s condition.
Statistical Analysis
Statistical analyses were performed using R version 4.0.2. Normally distributed continuous variables are presented as the mean±SD. Categorical data are expressed as frequencies and percentages. The significance of differences among groups was determined using Student’s t-test, the Wilcoxon rank-sum test, or one way-analysis of variance. Categorical variables were compared by the Chi-squared test or Fisher’s exact test. Receiver operating characteristic (ROC) curve analysis was conducted, and the best cut-off value of NT-proBNP for predicting the occurrence of CIN non-recovery was determined using MedCalc version 11.4.2.0 (MedCalc Software). The incidence of CIN non-recovery was compared between groups with NT-proBNP concentrations higher and lower than the best cut-off value (876.1 pg/mL). Multivariable logistic analysis was used to examine independent risk factors for CIN non-recovery in adjusted models, as follows: Model 1 was adjusted for age and diabetes; Model 2 was adjusted for variables in Model 1 plus eGFR <90 mL/min/1.73 m2, LVEF, and anemia. Kaplan-Meier method with log-rank test was used to survival analysis and Kaplan-Meier curves were delineated. Two-sided P<0.05 was considered statistically significant.
Results
Baseline Characteristics
Of the 646 patients who developed CIN after PCI, 96 were excluded based on the criteria, leaving 550 for inclusion in the present study. Of all these patients, 161 (29.3%) were female and the mean patient age was 65.3±11.4 years. Baseline patient eGFR and SCr were 105±31.2 mL/min/1.73 m2
and 0.85±0.67 mg/dL, respectively. Overall, 40 (7.3%) patients developed CIN non-recovery.
Table 1 presents the baseline characteristics of patients with and without CIN non-recovery. Patients in the CIN non-recovery group were older and more frequently had anemia, diabetes, worse renal function, higher baseline NT-proBNP concentrations, and lower LVEF and hemoglobin levels. Supplementary Table 1 presents the baseline characteristics of patients with high (>876.1 pg/mL) and low (≤876.1 pg/mL) NT-proBNP concentrations. Patients with high NT-proBNP were older and more likely to have comorbidities.
Table 1. Baseline Variables in Groups With and Without Contrast-Induced Nephropathy Recovery
| |
CIN recovery
(n=510) |
CIN non-recovery
(n=40) |
P value |
| Demographics |
| Age (years) |
64.9±11.3 |
70.2±11.3 |
0.006 |
| Age >75 years |
113 (22.2) |
14 (35.0) |
0.097 |
| Female sex |
146 (28.6) |
15 (37.5) |
0.314 |
| SBP (mmHg) |
135.2±22.6 |
130.4±29.5 |
0.328 |
| DBP (mmHg) |
76.7±14.0 |
74.9±15.0 |
0.474 |
| Medical history |
| Hypertension |
357 (70.0) |
33 (82.5) |
0.135 |
| Diabetes |
207 (40.6) |
26 (65.0) |
0.004 |
| Atrial fibrillation |
50 (9.8) |
7 (17.5) |
0.170 |
| Malignancy |
6 (1.2) |
2 (5.0) |
0.109 |
| Chronic heart failure |
36 (7.06) |
8 (20.0) |
0.010 |
| Medical therapy during hospitalization |
| Statin |
509 (99.8) |
40 (100) |
1.000 |
| CCB |
160 (31.4) |
13 (32.5) |
1.000 |
| Antiplatelet agents |
505 (99.0) |
38 (95.0) |
0.086 |
| β-blocker |
412 (80.8) |
35 (87.5) |
0.402 |
| Laboratory measurements |
| WBC (×109/L) |
8.7±3.6 |
9.4±3.0 |
0.193 |
| Hemoglobin (g/L) |
137.6±16.8 |
125.1±20.4 |
0.001 |
| Anemia |
124 (24.3) |
19 (47.5) |
0.002 |
| Platelets (×109/L) |
222.8±66.5 |
223.9±66.5 |
0.926 |
| Cholesterol (mmol/L) |
4.46±1.24 |
4.53±1.45 |
0.795 |
| LDL-C (mmol/L) |
2.92±1.10 |
2.91±1.23 |
0.955 |
| HDL-C (mmol/L) |
1.08±0.29 |
1.11±0.32 |
0.547 |
| NT-proBNP (ng/mL) |
1,523.3±3,980.7 |
3,932.8±4,317.5 |
0.001 |
| NT-proBNP concentration |
|
|
<0.001 |
| ≤876.1 pg/mL |
355 (69.6) |
7 (17.5) |
|
| >876.1 pg/mL |
155 (30.4) |
33 (82.5) |
|
| Serum creatinine (mg/dL) |
0.8±0.5 |
1.5±1.6 |
0.005 |
| eGFR (mL/min/1.73 m2) |
107.6±28.7 |
72.8±42.2 |
<0.001 |
| eGFR <90 mL/min/1.73 m2 |
118 (23.1) |
27 (67.5) |
<0.001 |
| Coronary artery disease type |
|
|
0.199 |
| Stable angina pectoris |
30 (5.9) |
2 (5.0) |
|
| Unstable angina pectoris |
184 (36.1) |
9 (22.5) |
|
| Acute myocardial infarction |
296 (58.0) |
29 (72.5) |
|
| Emergency PCI |
122 (23.9) |
14 (35) |
0.170 |
| LVEF (%) |
56.2±7.9 |
51.1±8.7 |
0.002 |
| Procedural characteristics |
| Contrast volume (mL) |
191.8±61.6 |
186.2±61.9 |
0.587 |
| No. stents |
1.5±0.8 |
1.7±1.1 |
0.452 |
| Stent length (mm) |
41.0±25.1 |
47.9±34.0 |
0.217 |
Unless indicated otherwise, data are given as the mean±SD or n (%). CCB, calcium channel blocker; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal pro B-type natriuretic peptide; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; WBC, white blood cell.
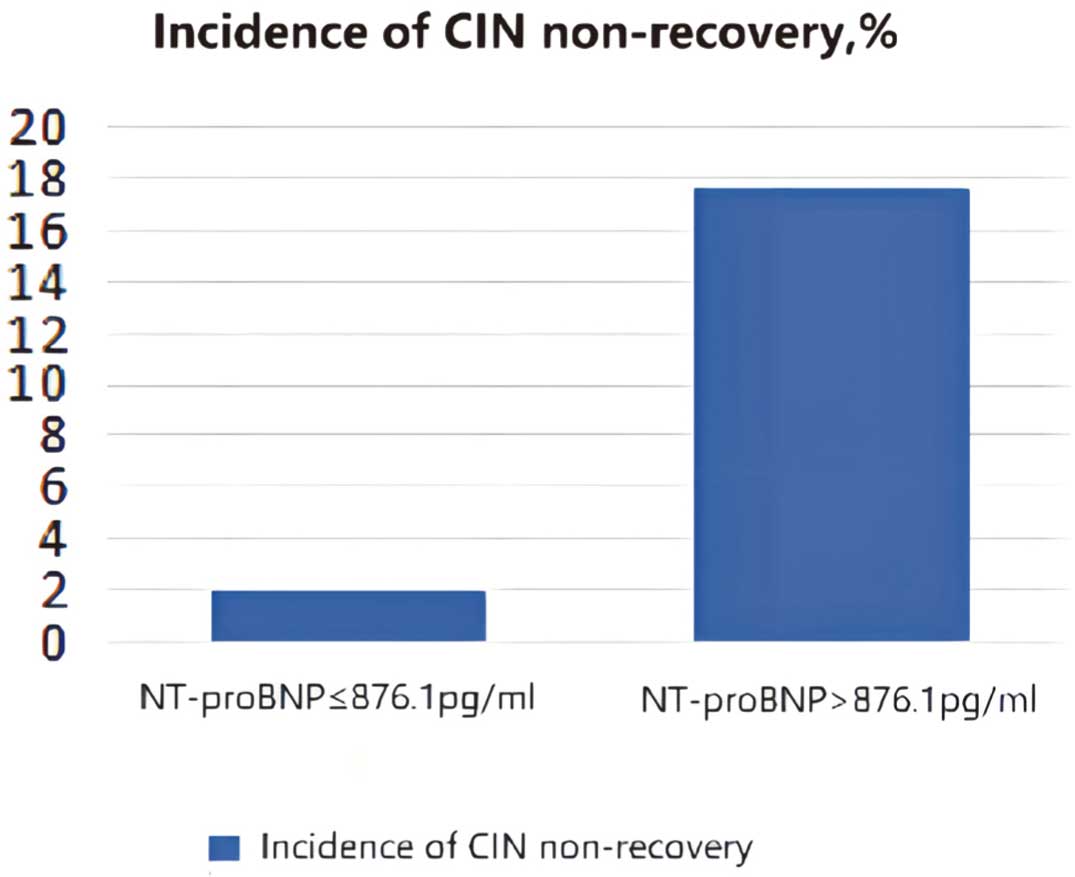
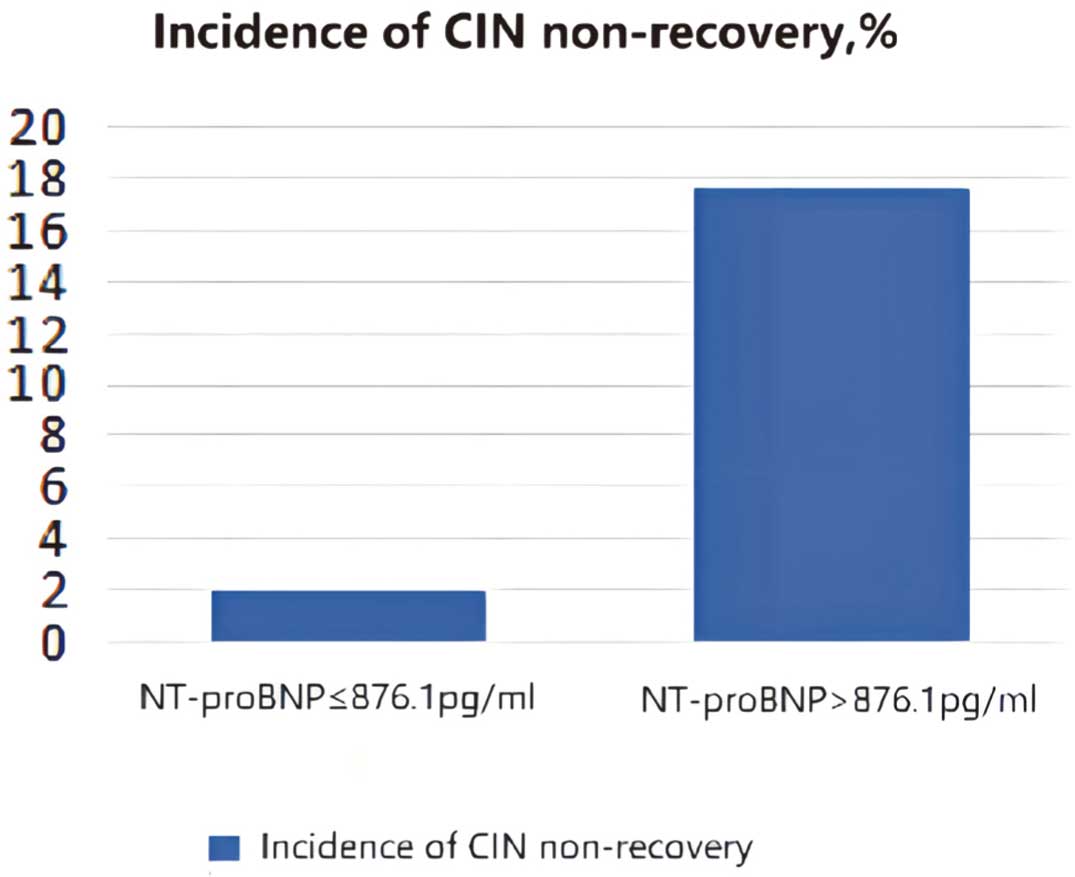
The area under the curve in ROC analysis of NT-proBNP for CIN recovery was 0.768 (95% confidence interval [CI] 0.731–0.803). Youden’s index indicated that the best cut-off value of NT-proBNP for CIN non-recovery was 876.1 pg/mL (log-transformed NT-proBNP: 2.94 pg/mL), with 82.5% sensitivity and 69.6% specificity (Figure 1). Moreover, the incidence of CIN non-recovery was significantly higher among patients with NT-proBNP >876.1 than those with NT-proBNP ≤876.1 pg/mL (17.6% vs. 1.9%, P<0.001) (Figure 2).
Univariate logistic regression analysis indicated that NT-proBNP >876.1 pg/mL, age, eGFR <90 mL/min/1.73 m2, diabetes, LVEF, and anemia were significantly associated with CIN non-recovery (all P<0.05). In multivariable logistic proportional hazard models, higher NT-proBNP concentrations were significantly associated with an increased risk of CIN non-recovery. In Model 1, after adjusting for age and diabetes, higher NT-proBNP concentrations were significantly correlated with CIN non-recovery, with an odds ratios (OR) of 3.40 (95% CI 2.09–5.76). In Model 2, after adjusting for the variables in Model 1 plus eGFR, LVEF, and anemia, the association between higher NT-proBNP concentrations and an increased risk of CIN non-recovery remained, with an OR of 4.91 (95% CI 1.81–14.84; Table 2). In addition, the association between CIN non-recovery and both CKD and diabetes remained (OR 3.53 [95% CI 1.54–8.50] and 2.35 [95% CI 1.11–5.19], respectively; Supplementary Table 2).
Table 2. Associations Between NT-proBNP Concentrations and Contrast-Induced Nephropathy Non-Recovery
NT-proBNP
(pg/mL) |
Participants
(n) |
Events
(n) |
Rate
(%) |
Model 1 |
Model 2 |
| OR (95% CI) |
P value |
OR (95% CI) |
P value |
| ≤876.1 |
362 |
7 |
1.90 |
1.00 (Reference) |
|
1.00 (Reference) |
|
| >876.1 |
188 |
33 |
17.60 |
3.40 (2.09–5.76) |
<0.001 |
4.91 (1.81–14.84) |
0.0026 |
Model 1 was adjusted for age and diabetes. Model 2 was adjusted for variables in Model 1 plus eGFR, LVEF, and anemia. CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.
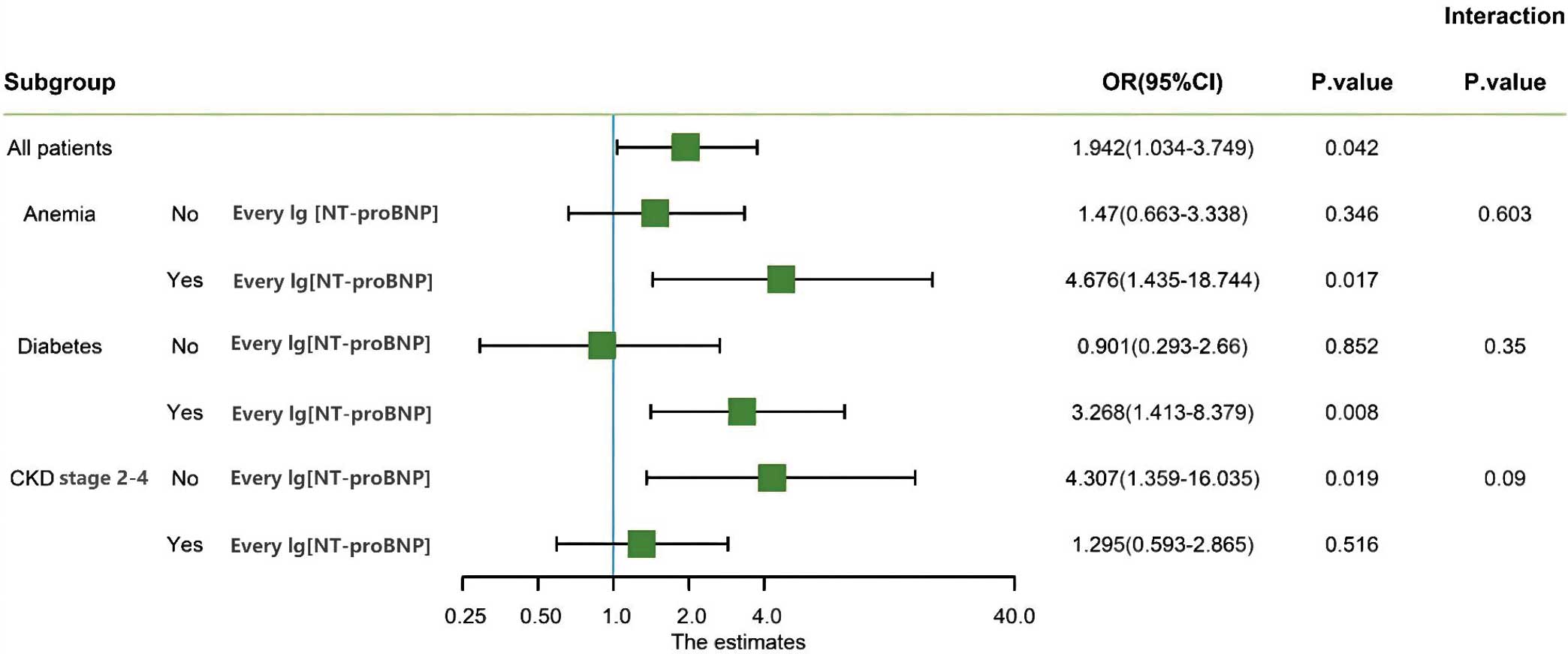
Figure 3 shows subgroup analysis stratified by CIN non-recovery risk factors. The association between plasma NT-proBNP concentrations and CIN non-recovery was consistent among these subgroups, and there was no effect modification of anemia, diabetes, and CKD Stage 2–4.
Follow-up
Clinical outcomes were available for 531 (96.5%) over patients a median follow-up of 703 days (interquartile range 422–1,060 days). During follow-up, 36 (6.78%) deaths were reported. Figure 4 shows that higher NT-proBNP concentrations were associated with a higher mortality rate (P<0.001). In addition, as shown in Figure 5, the mortality rate was higher in the CIN non-recovery group (P<0.001).
Discussion
To the best of our knowledge, this study is the first to explore the relationship between NT-proBNP and CIN non-recovery. The main finding of this study was that preprocedural NT-proBNP is an independent risk factor for CIN non-recovery in patients undergoing PCI.
It is generally believed that CIN is transient and recoverable after coronary angiography or intervention, and that renal function returns to baseline within a few days to weeks.5,6,18 However, recent studies have shown the opposite. For example, Benini et al, who retrospectively analyzed complete clinical and biochemical data of 731 patients after PCI, found that renal dysfunction persisted in more than half the patients with CIN after PCI.19 In a retrospective observational study of 1,041 PCI-treated patients with acute myocardial infarction (AMI) from the Infarction Prognosis Study Registry, Wi et al found that renal dysfunction persisted in 45.9% of patients who developed CIN.20 Persistent renal dysfunction after CIN was associated with increased short- and long-term mortality among AMI patients treated by PCI (P<0.001).20 Similarly, Maioli et al demonstrated that mortality was significantly higher in patients with persistent renal damage than in patients with transient renal damage (P=0.015) or in those without CIN (P=0.0001).21 Another recent study found that the severity of the persistent loss of renal function is related to acute renal injury after coronary angiography, and that the probability of a future decline in renal function was higher in patients with severe acute renal injury.8 As described above, continuous deterioration of kidney function or persistent renal damage can occur after CIN. CIN is not always a transient, benign nephropathy, but rather one of the direct causes of worsening renal function. The population with CIN non-recovery should not be ignored, because CIN non-recovery can independently predict long-term mortality.
NT-proBNP is an easily available and useful biomarker that is associated not only with systolic HF and diastolic dysfunction,22 but also with acute kidney injury (AKI), CKD, diabetes, and advanced age.23–25 The findings in the present study are consistent with previous work associating NT-proBNP with the development of CIN. For example, in a retrospective observational study of 174 patients with HF undergoing elective coronary angiography or PCI, Wang et al showed that NT-proBNP ≥3,299 pg/mL is associated with CIN and long-term mortality.11 Similarly, the preprocedural NT-proBNP concentration has an independent predictive value for the development of CIN after PCI in the population with ACS.12 Another recent study found that in 1,203 patients with CKD treated by PCI, NT-proBNP remained a significant predictor of CIN (OR 3.30; 95% CI 1.57–6.93; P=0.002) after adjusting for potential confounding risk factors.14 A substudy of HORIZONS-AMI (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction), including a total of 979 patients, further confirmed the independent predictive value of BNP for CIN among patients with STEMI after PCI.26
The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines define AKI as a sudden decline in renal function within 7 days or less, and CKD as a structural or functional abnormality of the kidney lasting for more than 90 days.27,28 However, it is increasingly recognized that AKI and CKD are not always independent diseases, and they may represent a continuous process.29 When patients experience an episode of AKI, the risk of de novo CKD or worsening of underlying CKD obviously increases.29,30 In recent years, elevated plasma concentrations of either NT-proBNP or BNP have been shown to be predictive for patients with CKD: the higher the plasma concentrations, the faster the deterioration in renal function.31–33 In a prospective multicenter cohort study including 177 participants without diabetes but with mild-to-moderate renal insufficiency, Spanaus et al showed that NT-proBNP concentrations were significantly higher among the 65 CKD patients who attained the combined endpoint, defined as doubling of baseline SCr or end-stage renal disease requiring renal replacement therapy, than the 112 CKD patients who did not.34 Each 1-SD increment in log-transformed NT-proBNP and BNP increased the risk of CKD progression, with hazard ratios (HR) of 2.28 (95% CI 1.76–2.95; P<0.001) and 1.38 (95% CI 1.09–1.76; P=0.009), respectively.34 In addition, in the Cardiovascular Health Study,35 among 3,752 subjects free of HF, 685 developed CKD over a mean (±SD) follow-up period of 6.41±1.74 years. Subjects in the highest NT-proBNP quartile (>237 pg/mL) had a 38% higher adjusted risk of incident CKD than those in the lowest NT-proBNP quartile (HR 1.38; 95% CI 1.08–1.76). Similarly, another study showed that CKD developed more frequently in the population with higher than lower concentrations of natriuretic peptides, even adjusting for baseline eGFR.36 These results suggest that NT-proBNP may play an important role in the incidence and progression of CKD. Nevertheless, the role of NT-proBNP in predicting a deterioration of renal function after CIN remains uncertain. The findings of the present study fill this gap. Preprocedural NT-proBNP, an independent risk factor for CIN non-recovery in patients undergoing PCI, can identify high-risk patients who may experience persistent renal damage.
The mechanisms underlying the association between NT-proBNP concentrations and CIN non-recovery are uncertain. The first consideration is the reason why persistent renal damage may occur after CIN. The impact of numerous comorbidities (hypertension, diabetes, congestive HF, proteinuria) cannot be ignored. Our data showed that patients with higher NT-proBNP concentrations tended to be older and were more likely to have diabetes, CKD, AMI, and anemia, which is consistent with previous studies.37–39 Accumulating evidence indicates that age and chronic diseases, such as diabetes, hypertension, and cardiac disease, are risk factors for persistent renal damage of AKI.40,41 The possible mechanism is the diminished glomerular reserve associated with aging or chronic disease.41 Meanwhile, patients who develop CIN may be more susceptible to other processes that lead to progressive kidney disease, such as atheroemboli or persistent renal microvascular disease after an acute ischemic tubular injury.42,43 Animal research has indicated that chronic and permanent changes to the renal microvasculature may result from acute ischemic renal injury.44 In addition, a previous study indicated that patients with higher NT-proBNP concentrations had higher urine protein.45 Proteinuria can reflect the overexcretion of protein from the glomerulus,46 which is an important marker of underlying inflammation and oxidative stress, as well as a validated risk for the progression of cardiovascular and kidney diseases.47 Numerous studies have reported that proteinuria is an independent risk factor for CIN after cardiac catheterization and participates in the process of sustained or chronic kidney injury.48–50 This may explain, in part, the potential reason of association of NT-proBNP and CIN non recovery. The second consideration is the possible role of NT-proBNP during the pathophysiological process. Pressure and volume overload and myocardial ischemia or myocardial infarction will reduce myocardial contractility and increase NT-proBNP concentrations, respectively affecting cardiac output and hemodynamics. At the same time, renal hypoperfusion leads to activation of the renin-angiotensin-aldosterone and sympathetic nervous systems, aggravating CIN.51,52 Finally, NT-proBNP concentrations are correlated with concentrations of proinflammatory cytokines,53,54 which may be involved in the process of CIN non-recovery. Fish-Trotter et al investigated 3 independent cohorts and found that interleukin (IL)-6 was positively correlated with NT-proBNP release.55 An in vitro study revealed that IL-18 was associated with increased BNP.56 In parallel, some studies indicated that inflammatory factors, such as neutrophil gelatinase-associated lipocalin, IL-6, and IL-18, were effective biomarkers to predict AKI non-recovery.57–59 Together, these observations indicate that NT-proBNP is likely to have a strong correlation with CIN non-recovery, which leads to poor outcomes, and some factors, such as age, diabetes, proteinuria, and inflammatory factors, may contribute to this process. Therefore, patients with CIN and higher NT-proBNP concentrations should receive closer monitoring over the longer term, including monitoring of SCr and urinary protein.
The present study has some limitations. First, this was a single-center observational study and the sample size was relatively limited with the subsequent disadvantages secondary to its nature. Thus, larger multicenter studies are needed in the future to validate our findings. Second, some detailed data, including the frequency of periprocedural saline hydration and more specific follow-up information about cardiovascular outcomes, were not recorded. Third, there are no experimental data to support our conclusion, which will be the subject of our next studies.
Conclusions
Preprocedural NT-proBNP is an easily available and useful biomarker that should be routinely measured before PCI to assess the risk of CIN non-recovery and long-term mortality after the procedure. The cut-off value of preprocedural NT-proBNP of 876.1 pg/mL in the present study may provide guidance for carrying out prevention of CIN non-recovery.
Sources of Funding
This study was funded by a grant from the National Natural Science Foundation of China General Program (Grant no. 81873495, 82171569), Heart Failure Center Research Foundation of Fujian Provincial Hospital (supported by the Fujian Provincial Department of Finance), and National Key Clinical Specialty Construction Project of China (Cardiovascular Medicine 2021). The funders had no role in study design, data collection, follow-up of patients, data interpretation, and writing the manuscript.
Disclosures
The authors declare that they have no conflict of interests.
IRB Information
The study protocol fulfilled the requirements of the Declaration of Helsinki and was approved by the Ethics Committee of the Fujian Provincial Hospital, China (Ethics Approval no. K2019-07-011). Written informed consent was obtained from all patients included in the study.
Data Availability
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
Supplementary Files
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-22-0399
References
- 1.
Almendarez M, Gurm HS, Mariani J Jr, Montorfano M, Brilakis ES, Mehran R, et al. Procedural strategies to reduce the incidence of contrast-induced acute kidney injury during percutaneous coronary intervention. JACC Cardiovasc Interv 2019; 12: 1877–1888.
- 2.
Aubry P, Brillet G, Catella L, Schmidt A, Benard S. Outcomes, risk factors and health burden of contrast-induced acute kidney injury: An observational study of one million hospitalizations with image-guided cardiovascular procedures. BMC Nephrol 2016; 17: 167.
- 3.
Silvain J, Nguyen LS, Spagnoli V, Kerneis M, Guedeney P, Vignolles N, et al. Contrast-induced acute kidney injury and mortality in ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Heart 2018; 104: 767–772.
- 4.
Scharnweber T, Alhilali L, Fakhran S. Contrast-induced acute kidney injury: Pathophysiology, manifestations, prevention, and management. Magn Reson Imaging Clin N Am 2017; 25: 743–753.
- 5.
Pannu N, Wiebe N, Tonelli M, Alberta Kidney Disease Network. Prophylaxis strategies for contrast-induced nephropathy. JAMA 2006; 295: 2765–2779.
- 6.
Gross JL, Friedman R, Silveiro SP. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354: 1853–1855.
- 7.
Nemoto N, Iwasaki M, Nakanishi M, Araki T, Utsunomiya M, Hori M, et al. Impact of continuous deterioration of kidney function 6 to 8 months after percutaneous coronary intervention for acute coronary syndrome. Am J Cardiol 2014; 113: 1647–1651.
- 8.
James MT, Ghali WA, Tonelli M, Faris P, Knudtson ML, Pannu N, et al. Acute kidney injury following coronary angiography is associated with a long-term decline in kidney function. Kidney Int 2010; 78: 803–809.
- 9.
Nishikimi T, Kuwahara K, Nakao K. Current biochemistry, molecular biology, and clinical relevance of natriuretic peptides. J Cardiol 2011; 57: 131–140.
- 10.
Volpe M. Natriuretic peptides and cardio-renal disease. Int J Cardiol 2014; 176: 630–639.
- 11.
Wang K, Li HL, Chen LL, Bei WJ, Lin KY, Smyth B, et al. Association of N-terminal pro-brain natriuretic peptide with contrast-induced acute kidney injury and long-term mortality in patients with heart failure and mid-range ejection fraction: An observation study. Medicine (Baltimore) 2017; 96: e6259, doi:10.1097/MD.0000000000006259.
- 12.
Kurtul A, Duran M, Yarlioglues M, Murat SN, Demircelik MB, Ergun G, et al. Association between N-terminal pro-brain natriuretic peptide levels and contrast-induced nephropathy in patients undergoing percutaneous coronary intervention for acute coronary syndrome. Clin Cardiol 2014; 37: 485–492.
- 13.
Goussot S, Mousson C, Guenancia C, Stamboul K, Brunel P, Brunet D, et al. N-terminal fragment of pro-B-type natriuretic peptide as a marker of contrast-induced nephropathy after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol 2015; 116: 865–871.
- 14.
Liu YH, Liu Y, Zhou YL, Yu DQ, He PC, Xie NJ, et al. Association of N-terminal pro-B-type natriuretic peptide with contrast-induced nephropathy and long-term outcomes in patients with chronic kidney disease and relative preserved left ventricular function. Medicine (Baltimore) 2015; 94: e358, doi:10.1097/MD.0000000000000358.
- 15.
JSN, JRS and JCS Joint Working Group. Guidelines on the use of iodinated contrast media in patients with kidney disease 2012: Digest version. Circ J 2013; 77: 1883–1914.
- 16.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis 2002; 39(Suppl 1): S1–S266.
- 17.
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines and the society for cardiovascular angiography and interventions. Catheter Cardiovasc Interv 2012; 79: 453–495.
- 18.
Guitterez NV, Diaz A, Timmis GC, O’Neill WW, Stevens MA, Sandberg KR, et al. Determinants of serum creatinine trajectory in acute contrast nephropathy. J Interv Cardiol 2002; 15: 349–354.
- 19.
Benini A, Scarsini R, Pesarini G, Pighi M, Ferrero V, Gambaro A, et al. Early small creatinine shift predicts contrast-induced acute kidney injury and persistent renal damage after percutaneous coronary procedures. Cardiovasc Revasc Med 2020; 21: 305–311.
- 20.
Wi J, Ko YG, Kim JS, Kim BK, Choi D, Ha JW, et al. Impact of contrast-induced acute kidney injury with transient or persistent renal dysfunction on long-term outcomes of patients with acute myocardial infarction undergoing percutaneous coronary intervention. Heart 2011; 97: 1753–1757.
- 21.
Maioli M, Toso A, Leoncini M, Gallopin M, Musilli N, Bellandi F. Persistent renal damage after contrast-induced acute kidney injury: Incidence, evolution, risk factors, and prognosis. Circulation 2012; 125: 3099–3107.
- 22.
Nishikimi T. Do plasma levels of brain natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP) increase in diastolic dysfunction as well as in systolic dysfunction? Circ J 2012; 76: 2540–2541.
- 23.
Patel UD, Garg AX, Krumholz HM, Shlipak MG, Coca SG, Sint K, et al. Preoperative serum brain natriuretic peptide and risk of acute kidney injury after cardiac surgery. Circulation 2012; 125: 1347–1355.
- 24.
Schaub JA, Coca SG, Moledina DG, Gentry M, Testani JM, Parikh CR. Amino-terminal pro-B-type natriuretic peptide for diagnosis and prognosis in patients with renal dysfunction: A systematic review and meta-analysis. JACC Heart Fail 2015; 3: 977–989.
- 25.
Peng Q, Hu W, Su H, Yang Q, Cheng X. Levels of B-type natriuretic peptide in chronic heart failure patients with and without diabetes mellitus. Exp Ther Med 2013; 5: 229–232.
- 26.
Jarai R, Dangas G, Huber K, Xu K, Brodie BR, Witzenbichler B, et al. B-type natriuretic peptide and risk of contrast-induced acute kidney injury in acute ST-segment-elevation myocardial infarction: A substudy from the HORIZONS-AMI trial. Circ Cardiovasc Interv 2012; 5: 813–820.
- 27.
Thomas ME, Blaine C, Dawnay A, Devonald MA, Ftouh S, Laing C, et al. The definition of acute kidney injury and its use in practice. Kidney Int 2015; 87: 62–73.
- 28.
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 2005; 67: 2089–2100.
- 29.
Chawla LS, Eggers PW, Star RA, Kimmel PL. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med 2014; 371: 58–66.
- 30.
Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, et al. Acute kidney disease and renal recovery: Consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 2017; 13: 241–257.
- 31.
Vickery S, Price CP, John RI, Abbas NA, Webb MC, Kempson ME, et al. B-type natriuretic peptide (BNP) and amino-terminal proBNP in patients with CKD: Relationship to renal function and left ventricular hypertrophy. Am J Kidney Dis 2005; 46: 610–620.
- 32.
Desai AS, Toto R, Jarolim P, Uno H, Eckardt KU, Kewalramani R, et al. Association between cardiac biomarkers and the development of ESRD in patients with type 2 diabetes mellitus, anemia, and CKD. Am J Kidney Dis 2011; 58: 717–728.
- 33.
Khalifeh N, Haider D, Horl WH. Natriuretic peptides in chronic kidney disease and during renal replacement therapy: An update. J Investig Med 2009; 57: 33–39.
- 34.
Spanaus KS, Kronenberg F, Ritz E, Schlapbach R, Fliser D, Hersberger M, et al. B-type natriuretic peptide concentrations predict the progression of nondiabetic chronic kidney disease: The mild-to-moderate kidney disease study. Clin Chem 2007; 53: 1264–1272.
- 35.
Bansal N, Katz R, Dalrymple L, de Boer I, DeFilippi C, Kestenbaum B, et al. NT-proBNP and troponin T and risk of rapid kidney function decline and incident CKD in elderly adults. Clin J Am Soc Nephrol 2015; 10: 205–214.
- 36.
Ogawa N, Komura H, Kuwasako K, Kitamura K, Kato J. Plasma levels of natriuretic peptides and development of chronic kidney disease. BMC Nephrol 2015; 16: 171.
- 37.
Seki S, Tsurusaki T, Kasai T, Taniguchi I, Mochizuki S, Yoshimura M. Clinical significance of B-type natriuretic peptide in the assessment of untreated hypertension. Circ J 2008; 72: 770–777.
- 38.
Kanda H, Kita Y, Okamura T, Kadowaki T, Yoshida Y, Nakamura Y, et al. What factors are associated with high plasma B-type natriuretic peptide levels in a general Japanese population? J Hum Hypertens 2005; 19: 165–172.
- 39.
Nakagawa K, Umetani K, Fujioka D, Sano K, Nakamura T, Kodama Y, et al. Correlation of plasma concentrations of B-type natriuretic peptide with infarct size quantified by tomographic thallium-201 myocardial scintigraphy in asymptomatic patients with previous myocardial infarction. Circ J 2004; 68: 923–927.
- 40.
Schmitt R, Coca S, Kanbay M, Tinetti ME, Cantley LG, Parikh CR. Recovery of kidney function after acute kidney injury in the elderly: A systematic review and meta-analysis. Am J Kidney Dis 2008; 52: 262–271.
- 41.
Kellum JA, Sileanu FE, Bihorac A, Hoste EA, Chawla LS. Recovery after acute kidney injury. Am J Respir Crit Care Med 2017; 195: 784–791.
- 42.
Thadhani RI, Camargo CA Jr, Xavier RJ, Fang LS, Bazari H. Atheroembolic renal failure after invasive procedures. Natural history based on 52 histologically proven cases. Medicine (Baltimore) 1995; 74: 350–358.
- 43.
Basile DP. The endothelial cell in ischemic acute kidney injury: Implications for acute and chronic function. Kidney Int 2007; 72: 151–156.
- 44.
Basile DP, Donohoe D, Roethe K, Osborn JL. Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am J Physiol Renal Physiol 2001; 281: F887–F899.
- 45.
Nakayama S, Satoh M, Metoki H, Murakami T, Asayama K, Hara A, et al. N-terminal pro-B-type natriuretic peptide is a predictor of chronic kidney disease in an Asian general population: The Ohasama Study. Circ Rep 2019; 2: 24–32.
- 46.
Guo JK, Marlier A, Shi H, Shan A, Ardito TA, Du ZP, et al. Increased tubular proliferation as an adaptive response to glomerular albuminuria. J Am Soc Nephrol 2012; 23: 429–437.
- 47.
Huang JC, Chen SC, Tsai YC, Kuo IC, Chiu YW, Chang JM, et al. Prognostic significance of left ventricular mass index and renal function decline rate in chronic kidney disease G3 and G4. Sci Rep 2017; 7: 42578.
- 48.
Saito Y, Watanabe M, Aonuma K, Hirayama A, Tamaki N, Tsutsui H, et al. Proteinuria and reduced estimated glomerular filtration rate are independent risk factors for contrast-induced nephropathy after cardiac catheterization. Circ J 2015; 79: 1624–1630.
- 49.
Tao Y, Dong W, Li Z, Chen Y, Liang H, Li R, et al. Proteinuria as an independent risk factor for contrast-induced acute kidney injury and mortality in patients with stroke undergoing cerebral angiography. J Neurointerv Surg 2017; 9: 445–448.
- 50.
Gorriz JL, Martinez-Castelao A. Proteinuria: Detection and role in native renal disease progression. Transplant Rev (Orlando) 2012; 26: 3–13.
- 51.
Weber M, Dill T, Arnold R, Rau M, Ekinci O, Muller KD, et al. N-terminal B-type natriuretic peptide predicts extent of coronary artery disease and ischemia in patients with stable angina pectoris. Am Heart J 2004; 148: 612–620.
- 52.
Azzalini L, Spagnoli V, Ly HQ. Contrast-induced nephropathy: From pathophysiology to preventive strategies. Can J Cardiol 2016; 32: 247–255.
- 53.
Dinh W, Futh R, Nickl W, Krahn T, Ellinghaus P, Scheffold T, et al. Elevated plasma levels of TNF-alpha and interleukin-6 in patients with diastolic dysfunction and glucose metabolism disorders. Cardiovasc Diabetol 2009; 8: 58.
- 54.
Li X, Peng H, Wu J, Xu Y. Brain natriuretic peptide-regulated expression of inflammatory cytokines in lipopolysaccharide (LPS)-activated macrophages via NF-kappaB and mitogen activated protein kinase (MAPK) pathways. Med Sci Monit 2018; 24: 3119–3126.
- 55.
Fish-Trotter H, Ferguson JF, Patel N, Arora P, Allen NB, Bachmann KN, et al. Inflammation and circulating natriuretic peptide levels. Circ Heart Fail 2020; 13: e006570, doi:10.1161/CIRCHEARTFAILURE.119.006570.
- 56.
Di Somma S, Pittoni V, Raffa S, Magrini L, Gagliano G, Marino R, et al. IL-18 stimulates B-type natriuretic peptide synthesis by cardiomyocytes in vitro and its plasma levels correlate with B-type natriuretic peptide in non-overloaded acute heart failure patients. Eur Heart J Acute Cardiovasc Care 2017; 6: 450–461.
- 57.
Forni LG, Darmon M, Ostermann M, Oudemans-van Straaten HM, Pettilä V, Prowle JR, et al. Renal recovery after acute kidney injury. Intensive Care Med 2017; 43: 855–866.
- 58.
Dewitte A, Joannès-Boyau O, Sidobre C, Fleureau C, Bats ML, Derache P, et al. Kinetic eGFR and novel AKI biomarkers to predict renal recovery. Clin J Am Soc Nephrol 2015; 10: 1900–1910.
- 59.
Verbrugge FH, Dupont M, Shao Z, Shrestha K, Singh D, Finucan M, et al. Novel urinary biomarkers in detecting acute kidney injury, persistent renal impairment, and all-cause mortality following decongestive therapy in acute decompensated heart failure. J Card Fail 2013; 19: 621–628.