Article ID: CJ-15-0621
Article ID: CJ-15-0621
Background: To clarify the effects of warfarin therapy in very old patients with non-valvular atrial fibrillation (NVAF), a post-hoc analysis was performed using the data of the J-RHYTHM Registry.
Methods and Results: A consecutive series of AF outpatients was enrolled from 158 institutions. Of 7,937 patients, 7,406 with NVAF (men, 70.8%; 69.8±10.0 years) were followed for 2 years or until an event occurred. Patients were divided into 3 age groups (<70, 70–84, and ≥85 years) and 5 subgroups according to international normalized ratio (INR; <1.6, 1.6–1.99, 2.0–2.59, 2.6–2.99, and ≥3.0). Prevalence of female sex, permanent AF, hypertension, coronary artery disease, heart failure, and history of ischemic stroke/transient ischemic attack was higher in the older groups. In the oldest group, 79.7% of patients received warfarin and their time in therapeutic range, using the Japanese target INR of 1.6–2.6, was 67.1%. Rate of thromboembolic events was lower in the age groups <70 and 70–84 years (P=0.027 and P<0.001, respectively) for patients receiving warfarin compared with those who were not. In the oldest group, the rate of thromboembolism plus major hemorrhage was lower at INR 1.6–2.59.
Conclusions: Warfarin could have beneficial effects even in very old NVAF patients if INR is kept between 1.6 and 2.59.
Atrial fibrillation (AF) is the most common arrhythmia in subjects of advanced age and is a potent risk factor for cardiogenic embolism.1,2 The prevalence of AF in the population aged ≥80 years is approximately 7–14% in Western countries3,4 and 2–3% in Japan.5,6 The number of subjects with AF can be expected to increase further with the aging of society.4–6 According to a recent population-based study from the UK,7 the number of AF-related ischemic strokes at age ≥80 years has trebled over the last 25 years and is projected to treble again by 2050. Given that aging per se is a potent risk factor for stroke,8 prophylaxis with anticoagulation therapy is especially important for reducing AF-related ischemic stroke in elderly patients.
Editorial p ????
Although several non-vitamin K antagonist oral anticoagulants (NOAC) have been available for anticoagulation therapy in patients with non-valvular AF (NVAF), the use of NOAC in elderly patients is limited, apparently because evidence of their safety is lacking. In contrast, warfarin has been widely used in the real-world clinical setting and is more effective than aspirin in NVAF patients aged ≥75 years.9
In several guidelines for the management of AF,10,11 an international normalized ratio (INR) of prothrombin time between 2.0 and 3.0 is recommended for patients with NVAF, regardless of age. In contrast, Japanese guidelines recommend a slightly lower INR of 1.6–2.6 for elderly (≥70 years) patients with NVAF,12 based on the results of a previous study of secondary stroke prevention in NVAF patients.13 Information regarding the status and effects of anticoagulation therapy among the elderly population, however, is still limited.14 Therefore, we investigated the status of anti-thrombotic therapy, rates of ischemic and hemorrhagic events, and mortality among different age groups of NVAF patients via a post-hoc analysis of the J-RHYTHM Registry.15–17 Results of the present study should be interpreted with caution, because the data of this registry were derived from institutions that specialized in cardiology and in the management for cardiac arrhythmias. These results may not always reflect situations in a general Japanese population with NFAF.
The J-RHYTHM Registry was a prospective, observational nationwide study, the detailed design and baseline characteristics of which have been reported elsewhere.15,16 Briefly, the subjects were recruited from 158 institutions that specialized in cardiology. A consecutive series of outpatients with AF of any type was enrolled, regardless of the use of anti-thrombotic drugs. Anti-thrombotic drugs and dosages were selected at the discretion of the treating cardiologists. Patients with valvular AF18 were excluded from this subanalysis.
Follow-up and Definition of EndpointsThe patients were followed for 2 years or until an endpoint, whichever occurred first. The thromboembolic endpoints consisted of symptomatic ischemic stroke, transient ischemic attack (TIA), and systemic embolism. Major hemorrhage, including intracranial hemorrhage, gastrointestinal hemorrhage, and other hemorrhage requiring hospitalization, was selected as the safety endpoint. All-cause mortality and cardiovascular mortality were also determined. If any event occurred during the follow-up period, the final clinical data, including INR at the time closest to the event, were collected.15 The diagnostic criteria for each event have been described elsewhere.15,16
Age Group and INRPatients were divided into 3 different age groups (<70, 70–84, and ≥85 years). The cut-off age of 70 years was selected according to that of the age-specific target INR in the Japanese guidelines.12 Although the cut-off age of 80 years was used in some previous studies,19,20 the highest cut-off age was arbitrarily set at 85 years in the present study, given that little information was available concerning anticoagulation status and events in very old NVAF patients aged ≥85 years.14 Consequently, the oldest group consisted of 330 NVAF patients aged ≥85 years (Table 1). The cut-off ages of 65 and 75 years were also considered as the alternative age groups according to the age criteria in the CHADS2 (1 point each for the presence of congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, and 2 points for history of stroke or TIA)21 and CHA2DS2-VASc scores (2 points for age ≥75 years and additionally 1 point each for the presence of vascular disease, age 65–74 years, and female sex category).22 In addition, patients receiving warfarin were divided into 5 subgroups according to INR (<1.6, 1.6–1.99, 2.0–2.59, 2.6–2.99, and ≥3.0). Although baseline INR was used in the main analysis of the J-RHYTHM Registry,17 INR at the time of events or at the end of the follow-up period was used in the present post-hoc analysis, because INR at the time of enrollment would not always reflect the anticoagulation status at the time of events.23 The time in therapeutic range (TTR)24 was also determined, using the target INR of 1.6–2.6 for patients aged ≥70 years and 2.0–3.0 for patients aged <70 years according to the Japanese guidelines.12
| Overall | <70 years | 70–84 years | ≥85 years | P-value† | |
|---|---|---|---|---|---|
| No. patients | 7,406 | 3,365 | 3,711 | 330 | |
| Age (years) | 69.8±10.0 | 61.0±7.0 | 76.1±4.0 | 87.4±2.8 | <0.001 |
| Male | 5,241 (70.8) | 2,648 (78.7) | 2,406 (64.8) | 187 (56.7) | <0.001 |
| Type of AF | |||||
| Paroxysmal | 2,835 (38.3) | 1,414 (42.0) | 1,326 (35.7) | 95 (28.8) | <0.001 |
| Persistent | 1,081 (14.6) | 543 (16.1) | 496 (13.4) | 42 (12.7) | |
| Permanent | 3,490 (47.1) | 1,408 (41.8) | 1,889 (50.9) | 193 (58.5) | |
| Comorbidities | |||||
| CAD | 781 (10.5) | 254 (7.5) | 483 (13.0) | 44 (13.3) | <0.001 |
| Cardiomyopathy | 634 (8.6) | 361 (10.7) | 254 (6.8) | 19 (5.8) | <0.001 |
| HCM | 264 (3.6) | 133 (4.0) | 123 (3.3) | 8 (2.4) | 0.249 |
| DCM | 370 (5.0) | 228 (6.8) | 131 (3.5) | 11 (3.3) | <0.001 |
| CHD | 96 (1.3) | 66 (2.0) | 30 (0.8) | 0 (0.0) | <0.001 |
| COPD | 131 (1.8) | 30 (0.9) | 89 (2.4) | 12 (3.6) | <0.001 |
| Hyperthyroidism | 131 (1.8) | 82 (2.4) | 48 (1.3) | 1 (0.3) | <0.001 |
| CHADS2 score | |||||
| 0 | 1,157 (15.6) | 895 (26.6) | 262 (7.2) | 0 (0.0) | <0.001 |
| 1 | 2,512 (33.9) | 1,451 (43.1) | 1,023 (27.6) | 38 (11.5) | |
| 2 | 2,056 (27.8) | 676 (20.1) | 1,246 (33.6) | 134 (40.6) | |
| 3 | 1,059 (14.3) | 262 (7.8) | 717 (19.3) | 80 (24.2) | |
| 4 | 436 (5.9) | 62 (1.8) | 328 (8.8) | 46 (13.9) | |
| 5 | 161 (2.2) | 19 (0.6) | 117 (3.2) | 25 (7.6) | |
| 6 | 25 (0.3) | 0 (0.0) | 18 (0.5) | 7 (2.1) | |
| Mean | 1.7±1.2 | 1.2±1.0 | 2.0±1.2 | 2.7±1.2 | <0.001 |
| Risk factors for stroke | |||||
| Heart failure | 2,055 (27.7) | 779 (23.2) | 1,113 (30.0) | 163 (49.4) | <0.001 |
| Hypertension | 4,477 (60.5) | 1,835 (54.5) | 2,434 (65.6) | 208 (63.0) | <0.001 |
| Age (≥75 years) | 2,565 (34.6) | 0 (0.0) | 2,235 (60.2) | 330 (100) | <0.001 |
| Diabetes mellitus | 1,359 (18.3) | 584 (17.4) | 711 (19.2) | 64 (19.4) | 0.130 |
| Stroke/TIA | 1,022 (13.8) | 367 (10.9) | 589 (15.9) | 66 (20.0) | <0.001 |
| Heart rate (beats/min) | 72.5±13.2 | 72.5±13.5 | 72.3±12.9 | 74.3±13.3 | 0.031 |
| Systolic BP (mmHg) | 126.0±16.2 | 125.1±15.8 | 126.8±16.3 | 125.4±18.1 | <0.001 |
| Diastolic BP (mmHg) | 73.5±17.0 | 75.5±21.8 | 72.2±11.0 | 68.2±12.1 | <0.001 |
Data given as n (%) or mean±SD. †Comparison among 3 age groups. AF, atrial fibrillation; BP, blood pressure; CAD, coronary artery disease; CHADS2, congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, and history of stroke or TIA; CHD, congenital heart disease; COPD, chronic obstructive pulmonary disease; DCM, dilated cardiomyopathy; HCM, hypertrophic cardiomyopathy; TIA, transient ischemic attack.
Data are presented as mean±SD. The statistical significance of differences in the means was analyzed using Student’s t-test or ANOVA, as appropriate. Frequencies of parameters or events were compared using chi-squared test or Fisher’s exact test, as appropriate. P<0.05 was considere to be statistically significant. All statistical analysis was performed with SPSS version 15.0 (SPSS Inc, Chicago, IL, USA).
Of the 7,937 patients with AF who had been enrolled in the J-RHYTHM Registry,16 421 patients were excluded because they had valvular AF.18 Of the remaining 7,516 patients with NVAF, 110 (1.5%) were lost to follow-up. Therefore, a total of 7,406 patients with NVAF was eligible for the present analysis.17
Baseline Characteristics and Anti-Thrombotic Therapy StatusThe prevalence of female sex, permanent AF, hypertension, coronary artery disease, heart failure, and history of ischemic stroke/TIA, and consequently mean CHADS2 score, were higher in the older groups than in the youngest group (Table 1). The frequency of warfarin treatment was lower in the oldest group than in the other groups. Mean INR was similar among the 3 age groups receiving warfarin, but daily warfarin dosage was significantly smaller in older groups than in younger groups. The target INR of 1.6–2.612 was achieved in 57.8% of the oldest group, and the TTR for this target INR was 67.1% in this specific age group (Table 2). The frequency of antiplatelet therapy increased with age, and any antiplatelet drug was prescribed in 34.5% of patients aged ≥85 years (Table 2).
| Overall | <70 years | 70–84 years | ≥85 years | P-value† | |
|---|---|---|---|---|---|
| Warfarin | 6,404 (86.5) | 2,822 (83.9) | 3,319 (89.4) | 263 (79.7) | <0.001 |
| Dosage (mg/day) | 2.9±1.2 | 3.2±1.2 | 2.6±1.1 | 2.2±0.8 | <0.001 |
| INR | 1.91±0.49 | 1.91±0.50 | 1.90±0.49 | 1.88±0.52 | 0.512 |
| <1.6 | 1,670 (26.1) | 746 (26.4) | 838 (25.2) | 86 (32.7) | 0.027 |
| 1.6–1.99 | 2,348 (36.7) | 986 (34.9) | 1,270 (38.3) | 92 (35.0) | |
| 2.0–2.59 | 1,854 (29.0) | 850 (30.1) | 944 (28.4) | 60 (22.8) | |
| 2.6–2.99 | 363 (5.7) | 167 (5.9) | 181 (5.5) | 15 (5.7) | |
| ≥3.0 | 169 (2.6) | 73 (2.6) | 86 (2.6) | 10 (3.8) | |
| TTR (%)‡ | 59.3±29.2 (n=6,064) | 42.6±27.4 (n=2,691) | 73.0±22.9 (n=3,128) | 67.1±25.9 (n=245) | <0.001 |
| Any antiplatelet | 1,937 (26.2) | 761 (22.6) | 1,062 (28.6) | 114 (34.5) | <0.001 |
| Aspirin | 1,675 (22.6) | 687 (20.4) | 910 (24.5) | 78 (23.6) | <0.001 |
| Others | 433 (5.8) | 128 (3.8) | 261 (7.0) | 44 (13.3) | <0.001 |
| Warfarin+antiplatelet | 1,358 (18.3) | 477 (14.2) | 815 (22.0) | 66 (20.0) | <0.001 |
Data given as n (%) or mean±SD. †Comparison among 3 age groups. ‡Target INR: 2.0–3.0 (<70 years) or 1.6–2.6 (≥70 years). INR, international normalized ratio; TTR, time in therapeutic range.
During the 2-year follow-up period, thromboembolic events occurred in 126 patients (1.7%), major hemorrhage in 140 (1.9%), and all-cause death in 195 (2.6%), including cardiovascular death in 68 (0.9%).
The incidence of thromboembolism increased with age (P<0.001 for trend) and was significantly lower in patients who were taking warfarin than in those who were not, in the groups aged <70 and 70–84 years (Figure 1A). Rate of major hemorrhage in patients taking warfarin also increased in an age-dependent manner (P<0.001 for trend) and looked to be higher compared with the non-warfarin group, but the difference did not reach statistical significance in all age groups (Figure 1B). All-cause mortality showed a remarkable age-dependent trend (P<0.001 for trend), and was markedly lower in the warfarin groups than in the non-warfarin groups aged ≥70 years (Figure 2A). Cardiovascular mortality was much higher among patients in the oldest group who were not taking warfarin compared with those in the same age group who were taking warfarin (Figure 2B).
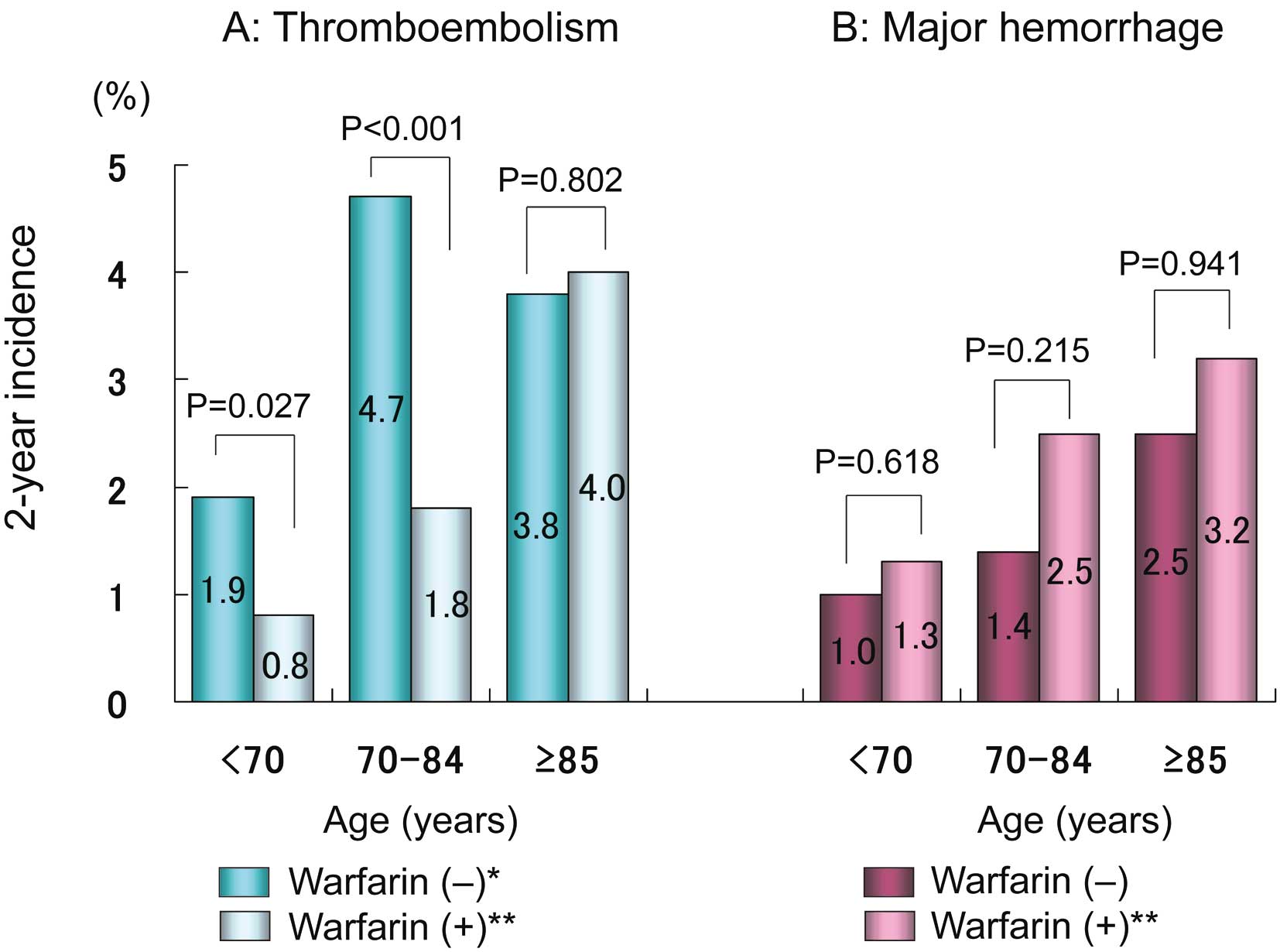
Two-year incidence of (A) thromboembolism and (B) major hemorrhage vs. age. *P=0.032 for trend, **P<0.001 for trend.
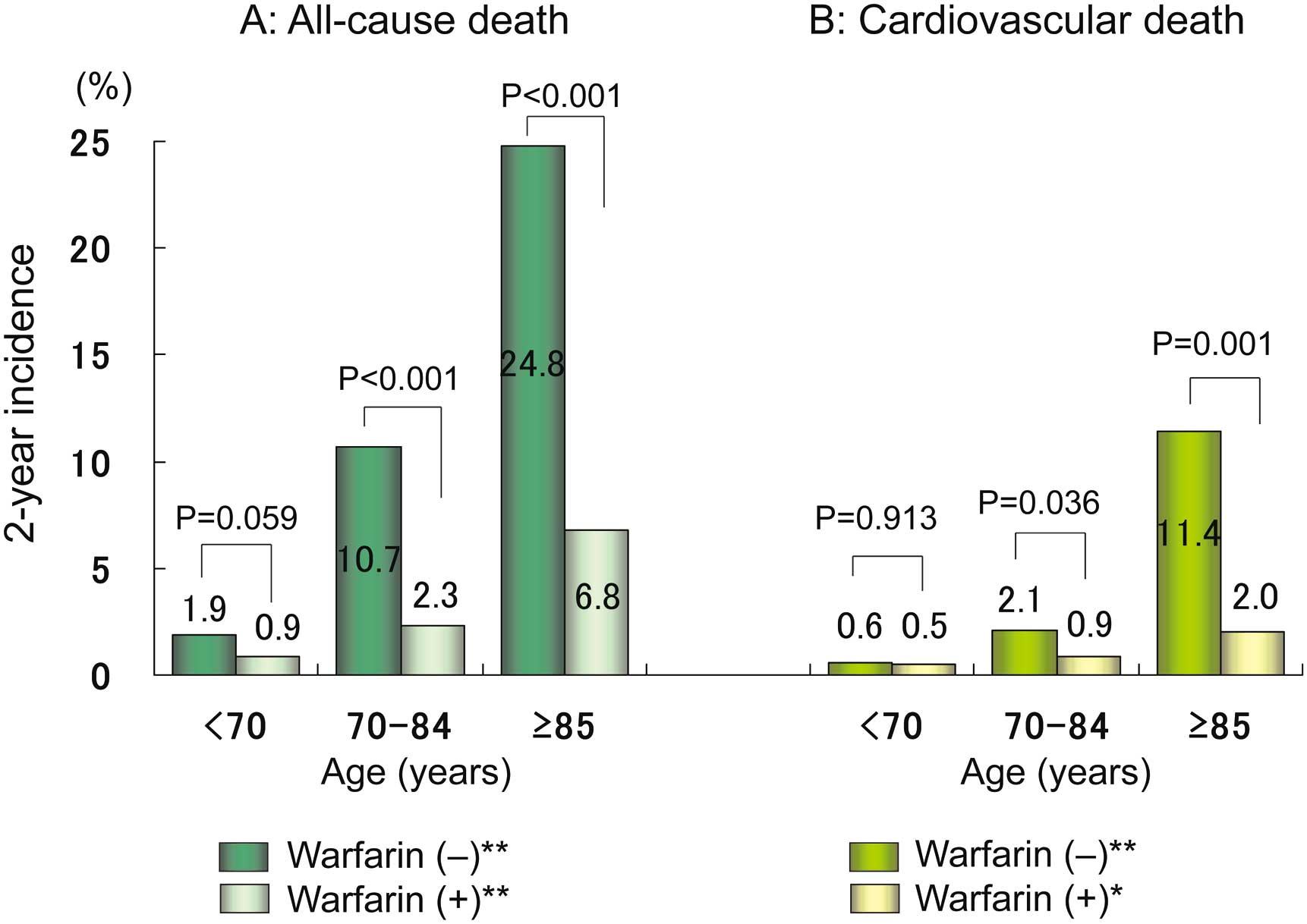
Two-year incidence of (A) all-cause death and (B) cardiovascular death vs. age. *P=0.010 for trend, **P<0.001 for trend.
Event rates in the alternative age groups are shown in Figures S1,S2. Rate of thromboembolism was not significantly lower in patients who were taking warfarin than in those who were not, in the group aged <65 years (P=0.089; Figure S1A).
Incidence Rates and INRRate of thromboembolic events decreased with an increase in INR in the groups aged <70 and 70–84 years, whereas it was higher at INR ≥2.6 in the oldest group aged ≥85 years (Table 3). Rate of major hemorrhage also showed a clear relationship with INR in all 3 age groups, and was much higher at INR ≥2.6 in the oldest patient group (Table 3). Consequently, the combined rates of thromboembolic and major hemorrhagic events were the lowest at INR 1.6–1.99 in groups aged 70–84 and ≥85 years (Table 3; Figure 3). All-cause mortality was notably higher among patients in the groups aged 70–84 and ≥85 years who were not taking warfarin as well as among those in the warfarin group who had INR ≥3.0 (Table 3). Cardiovascular mortality showed a similar trend, especially in the oldest group (Table 3).
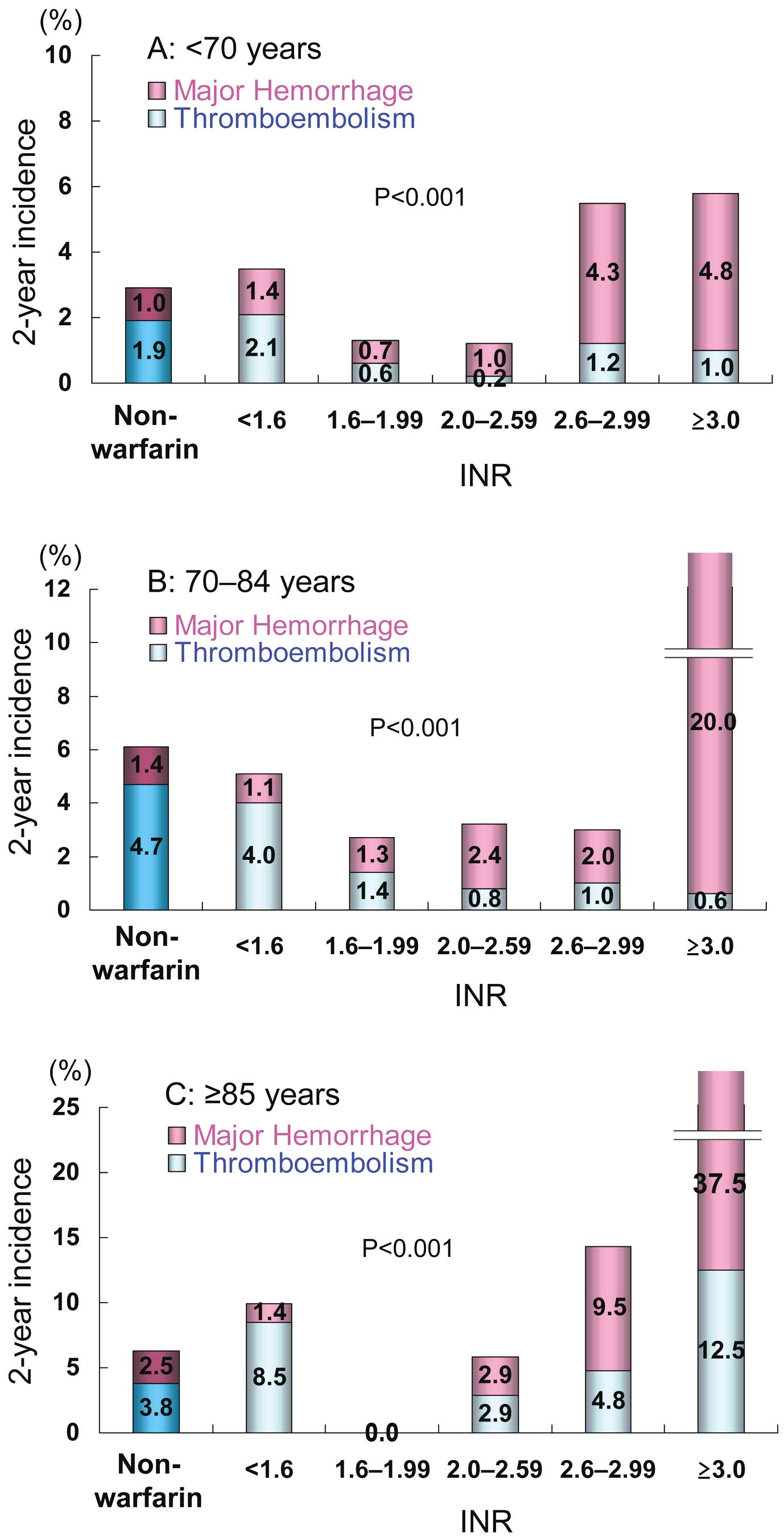
Two-year incidence of thromboembolism and major hemorrhage vs. INR in patients aged (A) <70 years, (B) 70–84 years, and (C) ≥85 years. P-values: comparison among 6 groups (non-warfarin group and 5 INR subgroups). INR, international normalized ratio.
| Non-warfarin | Warfarin | ||||||
|---|---|---|---|---|---|---|---|
| INR† | |||||||
| No. patients | <1.6 | 1.6–1.99 | 2.0–2.59 | 2.6–2.99 | ≥3.0 | ||
| <70 years | 619 | 571 | 974 | 926 | 161 | 105 | |
| 70–84 years | 428 | 747 | 1,176 | 992 | 203 | 155 | |
| ≥85 years | 79 | 71 | 81 | 69 | 21 | 8 | |
| Thromboembolism | P-value§ | ||||||
| <70 years | 12 (1.9) | 12 (2.1) | 6 (0.6) | 2 (0.2) | 2 (1.2) | 1 (1.0) | 0.001 |
| 70–84 years | 20 (4.7) | 30 (4.0) | 17 (1.4) | 8 (0.8) | 2 (1.0) | 1 (0.6) | <0.001 |
| ≥85 years | 3 (3.8) | 6 (8.5) | 0 (0.0) | 2 (2.9) | 1 (4.8) | 1 (12.5) | 0.785 |
| P-value‡ | 0.032 | 0.004 | 0.229 | 0.008 | 0.530 | 0.242 | |
| Major hemorrhage | P-value§ | ||||||
| <70 years | 6 (1.0) | 8 (1.4) | 7 (0.7) | 9 (1.0) | 7 (4.3) | 5 (4.8) | 0.010 |
| 70–84 years | 6 (1.4) | 8 (1.1) | 15 (1.3) | 24 (2.4) | 4 (2.0) | 31 (20.0) | <0.001 |
| ≥85 years | 2 (2.5) | 1 (1.4) | 0 (0.0) | 2 (2.9) | 2 (9.5) | 3 (37.5) | 0.002 |
| P-value‡ | 0.242 | 0.709 | 0.489 | 0.014 | 0.895 | <0.001 | |
| Thromboembolism+major hemorrhage | P-value | ||||||
| <70 years | 18 (2.9) | 20 (3.5) | 15 (1.3) | 11 (1.2) | 9 (5.6) | 6 (5.7) | <0.001 |
| 70–84 years | 26 (6.1) | 38 (5.1) | 32 (2.7) | 32 (3.2) | 6 (3.0) | 32 (20.6) | <0.001 |
| ≥85 years | 5 (6.3) | 7 (9.9) | 0 (0.0) | 4 (5.8) | 3 (14.3) | 4 (50.0) | <0.001 |
| P-value‡ | 0.014 | 0.022 | 0.177 | <0.001 | 0.821 | <0.001 | |
| All-cause death | P-value | ||||||
| <70 years | 12 (1.9) | 7 (1.2) | 6 (0.6) | 8 (0.9) | 3 (1.9) | 2 (1.9) | 0.163 |
| 70–84 years | 46 (10.7) | 19 (2.5) | 23 (2.0) | 13 (1.3) | 5 (2.5) | 14 (9.0) | <0.001 |
| ≥85 years | 19 (24.1) | 3 (4.2) | 8 (9.9) | 5 (7.2) | 0 (0.0) | 1 (12.5) | <0.001 |
| P-value‡ | <0.001 | 0.036 | <0.001 | 0.004 | 0.956 | 0.017 | |
| Cardiovascular death | P-value | ||||||
| <70 years | 4 (0.6) | 2 (0.4) | 3 (0.3) | 5 (0.5) | 2 (1.2) | 0 (0.0) | 0.240 |
| 70–84 years | 9 (2.1) | 9 (1.2) | 11 (0.9) | 4 (0.4) | 0 (0.0) | 5 (3.2) | 0.002 |
| ≥85 years | 9 (11.4) | 0 (0.0) | 2 (2.5) | 2 (2.9) | 0 (0.0) | 1 (12.5) | 0.006 |
| P-value‡ | <0.001 | 0.307 | 0.015 | 0.347 | 0.122 | 0.207 | |
Data given as n (%). †At the time of events or at the end of follow-up. ‡Comparison among the 3 age groups (χ2 test for trend). §Comparison among 6 groups (non-warfarin group and 5 INR subgroups) (χ2 test for trend). INR, international normalized ratio.
Event rates according to INR in the alternative age groups are listed in Table S1. Similar trends were observed even in the alternative age groups.
The major findings of the present study are as follows. First, very old patients aged ≥85 were characterized as a high-risk population, with a CHADS2 score of 2.7±1.2. Second, warfarin was prescribed in approximately 80% of patients aged ≥85 years, and the TTR, based on the Japanese target INR of 1.6–2.6,12 was 67.1% in these patients. This indicated that anticoagulation therapy was performed frequently in Japan, even in very old patients, and that the quality of warfarin therapy was high25 in these elderly patients. Third, the rates of thromboembolism, major hemorrhage, and mortality clearly increased with age. The efficacy of warfarin for preventing thromboembolism was evident in patients aged 65–84 years. Even in very old patients aged ≥85 years, the combined event rate of thromboembolism plus major hemorrhage remained lower at INR 1.6–2.59 than in those in the non-warfarin group. In addition, all-cause mortality was markedly lower in elderly patients receiving warfarin than in those without warfarin treatment.
Thromboembolic and Hemorrhagic Events in Elderly PatientsIn the present study, the rates of thromboembolic events increased with age in both the warfarin group and the non-warfarin group. The incidence of thromboembolism was markedly reduced at INR ≥1.6, especially in the group aged 70–84 years. Although the rate of thromboembolism was similar between very old patients aged ≥85 years with and without warfarin, it remained lower at INR 1.6–2.59 as compared with the non-warfarin group. This indicates that warfarin could be effective at preventing thromboembolism at INR between 1.6 and 2.59, even in very old patients aged ≥85 years.
The Incidence of major hemorrhage also increased with age in both the warfarin and the non-warfarin group. The rate of major hemorrhage increased markedly, depending on INR, and was higher at INR ≥2.6, especially in patients aged ≥85 years. Therefore, INR needs to be controlled below 2.6 for preventing hemorrhagic complication in elderly patients, a finding that is consistent with a previous study.13 Another previous study in elderly Japanese patients with NVAF also reported similar results: the rate of major hemorrhage was not high (1.1%/patient-year) in elderly patients aged ≥80 years with INR 1.5–2.5 and TTR of 73.9%.26
Mortality and WarfarinThe present study also found that all-cause mortality clearly increased with age, as indicated by previous studies.27,28 The warfarin group had lower all-cause mortality in patients aged ≥70 years, as well as lower cardiovascular mortality in very old patients aged ≥85 years. All-cause mortality, however, was markedly higher at INR ≥3.0, especially in groups aged ≥70 years; therefore, INR should be controlled below 3.0 when warfarin is given to elderly patients aged ≥70 years. Optimal intensity of warfarin therapy could be beneficial for all-cause mortality even in very old patients with NVAF, although it should be kept in mind that elderly patients may have any comorbidity to avoid warfarin, such as malignant neoplasm, resulting in a higher mortality in elderly patients in the non-warfarin group.
Optimal Anticoagulation Intensity in Elderly NVAF PatientsThe Birmingham Atrial Fibrillation Treatment of the Aged (BAFTA) study included 190 patients aged ≥85 years and compared the rates of thromboembolic and hemorrhagic events in NVAF patients aged ≥75 years between 488 patients treated with warfarin and 485 receiving aspirin.9 The annual risk of ischemic stroke was significantly lower in the warfarin group than in the aspirin group (0.8% vs. 2.5%, P=0.0004), whereas the risk of hemorrhagic events was similar between the groups.9 This finding supports the use of anticoagulants in NVAF patients aged ≥75 years, unless there are contraindications. Other studies have demonstrated that the bleeding risk of warfarin in elderly NVAF patients aged ≥80 years is acceptably low.20,26 These findings suggest that age itself should not be regarded as a contraindication to anticoagulation therapy. The present findings also indicate that warfarin therapy could reduce thromboembolism and all-cause death even in very old patients aged ≥85 years, without an increase in major hemorrhage, when INR is controlled within the age-specific target values of 1.6–2.59.
Anticoagulation Therapy in Younger NVAF PatientsThe present study also provides information on anticoagulation therapy with warfarin in younger NVAF patients. Rate of thromboembolism was low even in patients not taking warfarin in the youngest age group. Although significant reduction in rate of thromboembolism was observed in the youngest group when patients were divided at 70 years, it was not significant when the cut-off age was set at 65 years. Anticoagulation therapy might be unnecessary for patients aged <65 years who have no other risk factor for ischemic stroke. In patients receiving warfarin, the combined rates of thromboembolism and major hemorrhage at INR 1.6–2.59 tended to be lower even in patients aged <65 years, but this was not statistically significant. Therefore, it would be difficult to conclude that INR 1.6–2.6 is optimal in patients aged <65 years from the present data.
Study LimitationsThe present study had several limitations. First, it was performed in a single country and the registry was established only in 158 selected institutions in Japan. Given that most of the participating physicians specialized in cardiology, patient clinical background may not be able to be extrapolated to a general Japanese patient population with NVAF.29 Second, although this registry was large, analyzing a total of 7,406 patients with NVAF, the numbers of patients and those having events in each age group and in the INR subgroups were small. This might have reduced the statistical power of the present study. In particular, the number in the oldest group with INR ≥2.6 was small. Therefore, generalizing from the results of this specific subgroup to daily clinical practice should be done with great caution. Third, given that the study design was prospective but observational, the selection of anti-thrombotic drugs was not randomized. Warfarin and INR levels for individual patients were selected at the discretion of the participating physicians. Fourth, 1.5% of patients were lost to follow-up in the present study, which could have led to the underreporting of endpoints.
Anticoagulation therapy with warfarin was performed frequently even in very old Japanese patients with NVAF. Warfarin therapy could reduce thromboembolism and all-cause mortality without an increase in major hemorrhage, even in very old patients aged ≥85 years, if INR is kept between 1.6 and 2.59.
The current study was presented in part at ESC Congress 2014 (Barcelona, Spain, 30 August 2014). Investigators in the J-RHYTHM Registry are listed in references 15, 16, and 30. The J-RHYTHM registry was supported by a grant from the Japan Heart Foundation.
Co-authors have a potential conflict of interest: H.A. has received research funding from Boehringer Ingelheim, and remuneration from Bayer Healthcare, Boehringer Ingelheim, and Daiichi-Sankyo; H.I. has received research funding from Boehringer Ingelheim and Daiichi-Sankyo, and remuneration from Daiichi-Sankyo, Bayer Healthcare, and Boehringer Ingelheim; K.O. has received research funding from Boehringer Ingelheim and Daiichi-Sankyo, and remuneration from Boehringer Ingelheim, Bayer Healthcare, Daiichi-Sankyo, and Pfizer; T.Y. has received research funding from Boehringer Ingelheim and Daiichi-Sankyo, and remuneration from Boehringer Ingelheim, Daiichi-Sankyo, Bayer Healthcare, Pfizer, Bristol-Myers Squibb, and Eisai; H.O. has received lecture fees from Daiichi-Sankyo.
Supplementary File 1
Figure S1. Two-year incidence of (A) thromboembolism and (B) major hemorrhage in alternative age groups.
Figure S2. Two-year incidence of (A) all-cause death and (B) cardiovascular death in alternative age groups.
Table S1. Two-year event rates, age, and anticoagulation intensity in alternative age groups
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-15-0621