Abstract
Background: Although surgical approaches for infected or failing cardiac implantable electronic device (CIED) leads are more invasive than transvenous approaches, they are still required for patients considered unsuitable for transvenous procedures. In this study, surgical management with transvenous equipment for CIED complications was examined in patients unsuitable for transvenous lead extraction.
Methods and Results: We retrospectively examined 152 consecutive patients who underwent CIED extraction between April 2009 and December 2021 at the Department of Cardiovascular Surgery, Nippon Medical School. Nine patients (5.9%; mean [±SD] age 61.7±16.7 years) who underwent open heart surgery were identified as unsuitable for the isolated transvenous approach. CIED types included 5 pacemakers and 4 implantable cardioverter-defibrillators; the mean [±SD] lead age was 19.5±7.0 years. Indications for surgical management according to Heart Rhythm Society guidelines included failed prior to transvenous CIED extraction (n=6), intracardiac vegetation (n=2), and severe lead adhesion (n=1). Transvenous CIED extraction tools were used in all patients during or before surgery. Additional surgical procedures with CIED extraction included epicardial lead implantation (n=4) and tricuspid valve repair (n=3). All patients were discharged; during the follow-up period (mean 5.7±3.7 years), only 1 patient died (non-cardiac cause).
Conclusions: Surgical procedures and transvenous extraction tools were combined in the removal strategy for efficacious surgical management of CIED leads. Intensive surgical procedures were safely performed in patients unsuitable for transvenous extraction.
Recently, the incidence of cardiac implantable electronic device (CIED) implantations has increased, as has the number of CIED-related complications.1,2 Before the development of transvenous tools, open heart surgery with cardiopulmonary bypass (CPB) was performed to extract CIED leads as the first-line therapy for CIED complications.3 Surgical approaches in the 1990 s resulted in relatively higher mortality from CIED infection than recently reported.4,5 Over the past 2 decades, transvenous lead extraction tools have established a state-of-the-art strategy for infected or failing CIED leads.6,7 Nevertheless, a surgical approach is still required for some patients with CIED complications. In particular, patients at a high risk of experiencing life-threatening complications following the transvenous approach still require open heart surgery.3,6,8–10 The development of transvenous equipment and approaches has changed the surgical management of CIED lead extraction. Recent surgical management approaches for CIED lead complications incorporate advantages of both transvenous and surgical treatments. Although transvenous approaches are mainstream for CIED lead treatment, surgical procedures can guarantee safety for those at high risk of CIED complications. Few studies have reported combination management with transvenous and surgical approaches for high-risk lead extractions;7,11 however, additional evaluation of the combined procedures is needed. We believe that joint management with transvenous and surgical approaches may have the potential to safeguard patients with CIEDs.
The purpose of this study was to verify the feasibility of surgical CIED management for device extraction in high-risk patients for transvenous lead extraction.
Methods
Patient Population
In this retrospective study we reviewed the clinical records of patients who underwent CIED extraction between April 2009 and December 2021 in the Department of Cardiovascular Surgery, Nippon Medical School. All treatments were performed in accordance with the Declaration of Helsinki,12 and were approved by the Ethics Committee of Nippon Medical School, Tokyo, Japan (Reference no. B-2022-505). The requirement for informed consent was waived by the institutional review board because the researchers retrospectively accessed a deidentified database for analytical purposes.
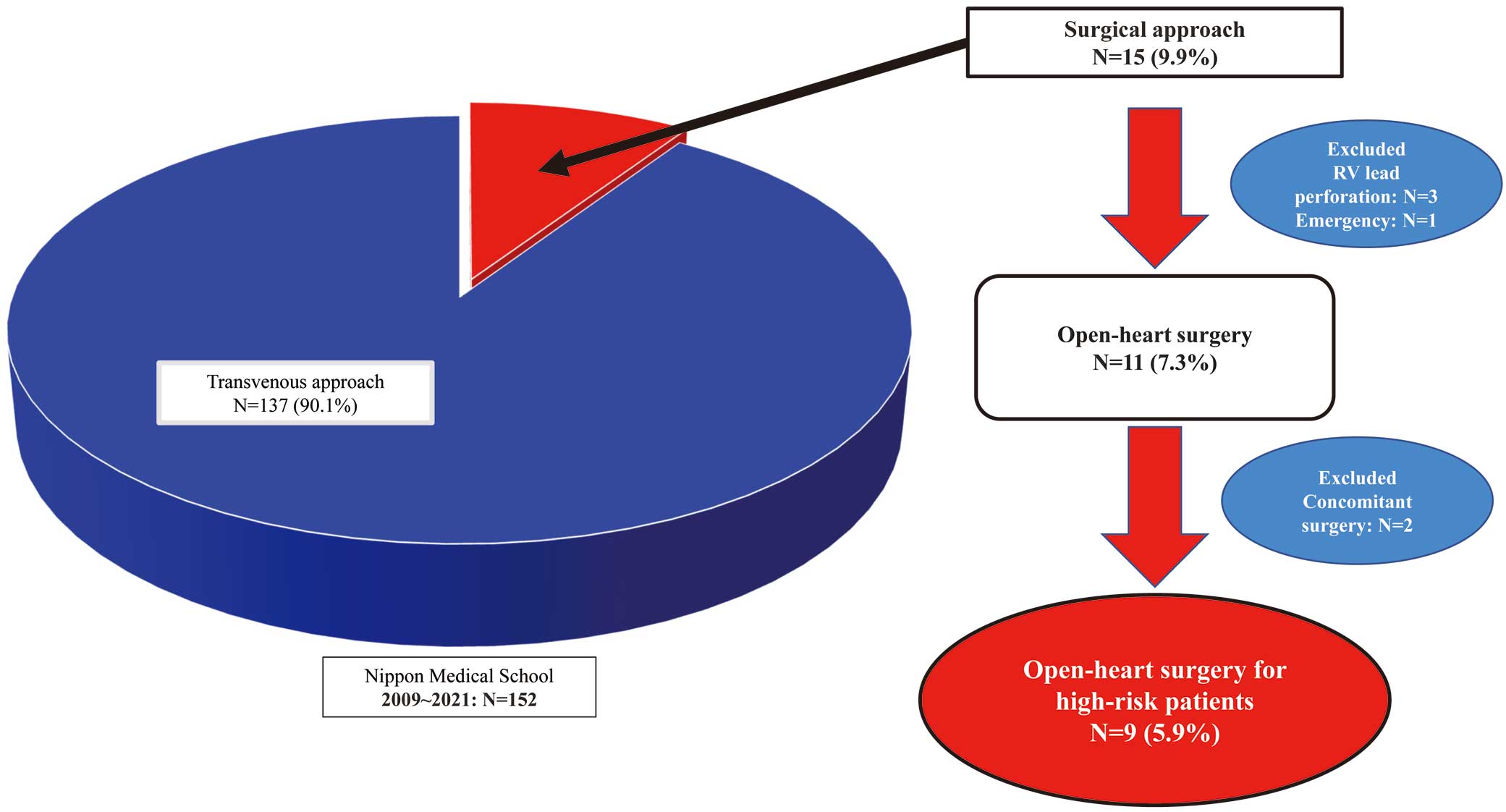
The records of all candidates were examined retrospectively; cases with clinical consensus for an infected and a failing CIED treated with any treatment modality were included in this study. Surgical approach, as such, was not an exclusion criterion, and the study included patients who underwent procedures via any surgical approach, such as sternotomy and thoracotomy. In contrast, off-pump cases (i.e., simple lead extraction for a perforated lead) and concomitant non-CIED-related surgical cases were excluded from this study (Figure 1).
Indications for Surgery
All patients were managed by cardiologists, cardiovascular surgeons, and infectious disease control specialists. The indications and procedures for lead and device removal were in accordance with the 2010 and 2017 Heart Rhythm Society consensus documents6,8 and Japanese Circulation Society (JCS)/Japanese Heart Rhythm Society (JHRS) guidelines.13 Indications for surgery were vegetation attached to CIED leads and cardiac tissue; leads inaccessible by any transvenous approaches; failed prior lead extraction attempts; perforated leads; and lead extraction with concomitant open heart surgery.3,6,8–10,14 The decision to perform open heart surgery was made via consensus in a meeting with the treatment team.
Surgical Procedures
In cases of a failed prior transvenous approach, a surgical approach was planned for the day after the first lead extraction procedure. All patients were operated on under general anesthesia, and median sternotomy was performed as an approach incision to the heart during open heart surgery, as described previously.15 CPB settings depended on the number of CIED leads, occlusion of the superior vena cava (SVC), and tissue adhesions. Either cardiac arrest or beating heart was selected during CPB. Cardiac arrest was used in patients who had undergone additional procedures (i.e., tricuspid repair) and had complicated leads.
Statistical Analysis
All continuous variables are presented as the mean±SD. Analyses were performed using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA).
Results
Patient Population
Between April 2009 and December 2021, 152 consecutive patients underwent CIED extraction at Nippon Medical School Hospital (Figure 1). We previously reported that over 80% of these patients underwent device removal due to CIED-related infection, which is a criterion for Class I indications at Nippon Medical School Hospital.6,8–10,13,14 In all, 137 patients underwent CIED lead extraction via the transvenous approach with powered sheaths and lead extraction equipment or simple extraction (90.8%). Fifteen patients required a surgical approach for CIED extraction (9.9%): 11 patients underwent planned open heart surgery via CPB (7.3%), 3 patients required surgical treatment for lead perforations that occurred during lead implantation and were eventually repaired by direct sutures without CPB via median sternotomy or thoracotomy, and 1 patient required open heart surgery due to vascular injury during transvenous lead extraction. Two patients underwent open heart surgery due to concomitant surgery (one for ventricular tachycardia surgery and one for atrial reduction surgery) and were excluded from the study. Therefore, we retrospectively examined the medical and surgical records of 9 consecutive high-risk patients who underwent open heart surgery (Figure 1).
Patient Baseline Characteristics and CIED-Related Data
The baseline characteristics and CIED-related data of the 9 patients (6 males, 3 females) are presented in Table 1; the mean patient age was 61.7±16.7 years (range 37–79 years). Primary diseases and diseases indicating CIED implantation are also presented in Table 1.
Table 1. High-Risk Patients’ Demographics and Basic Cardiac Implantable Electronic Device Data
| Age (years) |
61.7±16.7 |
| No. males/females |
6/3 |
| Primary disease |
| Complete AV block |
4 (44.4) |
| Brugada syndrome |
3 (33.3) |
| ARVC |
1 (11.1) |
| Giant atrium |
1 (11.1) |
| Disease indicated for CIED |
| Complete AV block |
4 (44.4) |
| Brugada syndrome |
3 (33.3) |
| ARVC |
1 (11.1) |
| Sick sinus syndrome |
1 (11.1) |
| CIED device |
| Pacemaker |
5 (55.5) |
| ICD |
4 (44.4) |
| Total target lead (n) |
19 |
| RA lead |
6 |
| RV lead |
8 |
| ICD lead |
5 |
| Lead age (years) |
19.5±7.0 |
| Comorbidity |
| Coronary artery disease |
1 (11.1) |
| Valve disease |
| TR severe |
1 (11.1) |
| Congestive heart failure |
3 (33.3) |
| Hypertension |
4 (14.4) |
| Diabetes |
1 (11.1) |
| Prior stroke |
0 (0) |
| Atrial fibrillation |
2 (22.2) |
| CRF (Cr>1/3) |
0 (0) |
| Hemodialysis |
0 (0) |
| Prior CABG |
0 (0) |
| Prior valve surgery |
0 (0) |
| Prior endocarditis |
4 (44.4) |
| COPD |
2 (22.2) |
| Steroid use |
0 (0) |
Unless indicated otherwise, data are given as the mean±SD or n (%). ARVC, arrhythmogenic right ventricular cardiomyopathy; AV, atrioventricular; CABG, coronary artery bypass grafting; CIED, cardiac implantable electronic device; COPD, chronic obstructive pulmonary disease; CRF, chronic renal failure; ICD, implantable cardioverter-defibrillator; RA, right atrium; RV, right ventricle; TR, tricuspid valve regurgitation.
Five patients initially underwent pacer implantation. Patients with complete atrioventricular block (n=4) were initially implanted with dual-chamber pacemakers, whereas 1 patient with sick sinus syndrome was implanted with a single-chamber pacer; patients with Brugada syndrome (n=3) and 1 patient with arrhythmogenic right ventricular cardiomyopathy underwent implantable cardioverter-defibrillator (ICD) implantation. CIED lead characteristics are also presented in Table 1. In all, 19 target leads were removed: 6 right atrium (RA) leads, 8 right ventricle (RV) leads, and 5 ICD leads. All ICD leads were the dual-shock coil type; the mean lead age was 19.5±7.0 years (range 3.9–37.1 years). Individual lead ages for RA, RV, and ICD leads were 19.5±5.9, 22.8±7.0, and 14.2±5.8 years, respectively. Comorbidities included valve disease (tricuspid valve regurgitation: 11.1%), congestive heart failure (33.3%), hypertension (44.4%), atrial fibrillation (22.2%), and chronic obstructive pulmonary disease (22.2%). Notably, 4 patients had a prior history of endocarditis before surgical intervention (44.4%).
Indications for CIED Lead Extraction
The most common indication for CIED extraction was CIED infection (n=7). Other indications for CIED removal were lead malfunction and RA lead-related tricuspid valve regurgitation (n=1).
Indication for Open Heart Surgery
The indications for open heart surgery are presented in Table 2. Indication for CIED extraction with open heart surgery included failed prior transvenous lead extraction in 6 patients. Two patients had intracardiac vegetations as an indication for open heart surgery. One patient underwent perforated ICD lead with transvenous lead extraction under open chest observation. After transvenous lead extraction, a 1.5-cm oscillating vegetation persisted on the tricuspid orifice. The other case had a lead attached to 3.6-cm vegetation with CIED infection. Preoperative lead adhesion was evaluated multidirectionally based on the findings of preoperative computed tomography, lead age, lead type, and patient age. One patient with an indication of severe lead adhesion underwent open heart surgery.
Table 2. Surgical Procedure Data
| Approach (n) |
| Median sternotomy |
9 |
| Additional surgery after lead extraction (n) |
| Epicardial lead implantation |
4 |
| TVP |
3 |
| Operative plan (n) |
| One stage operation |
3 |
| Vegetation |
2 |
| Severe lead adhesion |
1 |
| Two-stage operations |
6 |
| Failed prior TV extraction |
6 |
TV, transvenous approach; TVP, tricuspid valve pasty.
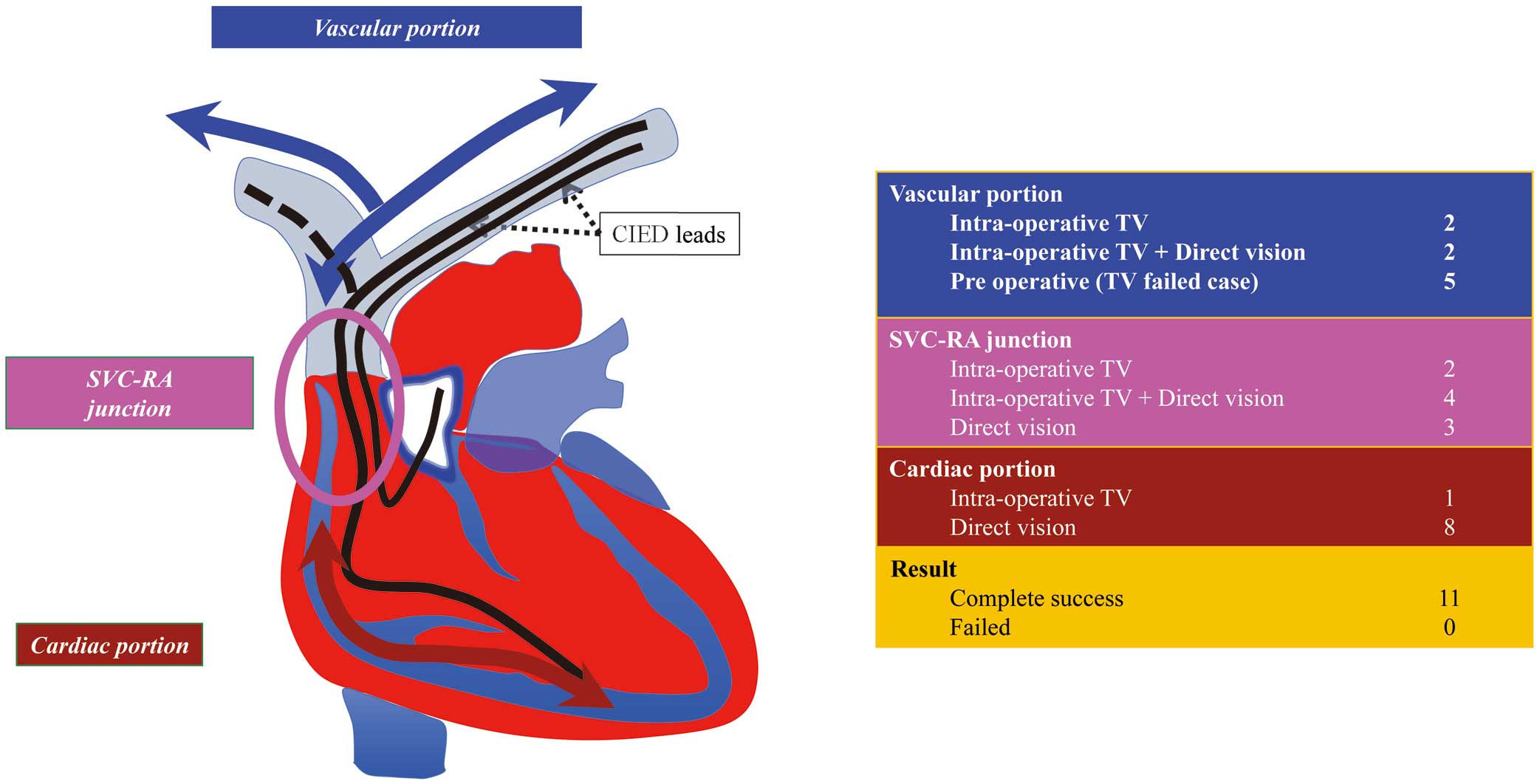
CIED lead extraction procedures and extraction results are presented in Figure 2. In all patients, transvenous lead extraction equipment was used to ablate lead adhesion before and during surgical treatment. The areas of CIED lead adhesion were divided into 3 parts according to the lead tracts (Figure 2, Left): the vascular portion was defined as the region from the lead vascular entry site to the SVC, including the subclavian vein (SCV); the SVC-RA junction was defined as the region from the SVC-SCV confluence to the RA junction; and the cardiac portion was defined as the RA and RV.
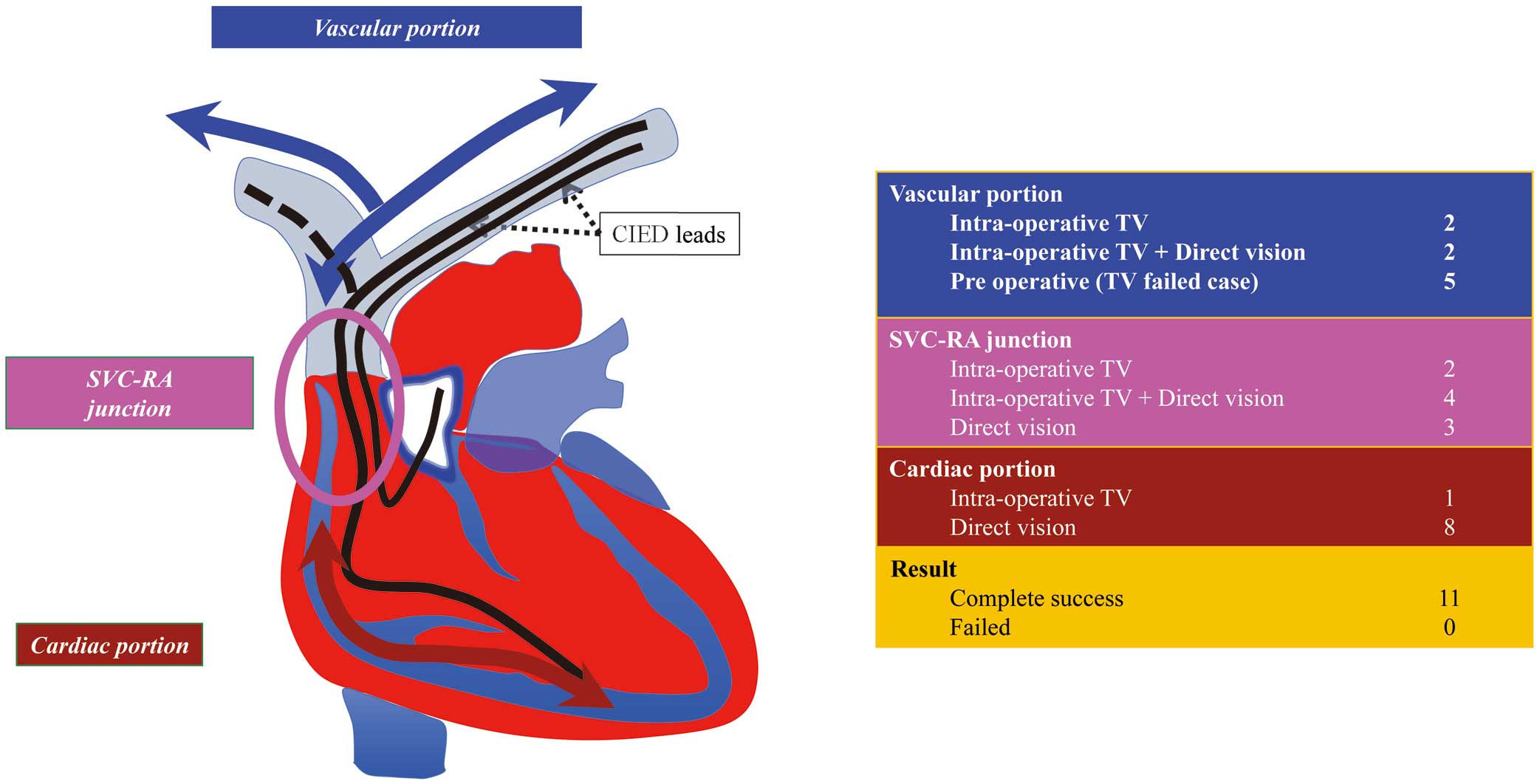
For the vascular portion, intraoperative transvenous tools were used to release the lead adhesions in 4 patients; in the other 2 patients, both intraoperative transvenous and direct visual elimination were used to release lead adhesions. Even in the 5 patients who experienced failed prior transvenous approaches, remaining CIED leads were released from the vasculature in their vascular portions (Figure 2, Right). For the SVC-RA junction, intraoperative transvenous equipment was used in 2 patients, and direct visual eliminations were applied in 3 patients. Both transvenous and direct visual methods were used in the SVC of 4 patients (Figure 2, Right). For the cardiac portion, the intraoperative transvenous approach was applied in 1 patient; in the remaining 8 patients, direct visual approaches were used to release lead adhesions to the SVC (Figure 2, Right). All leads were completely removed in these patients (Figure 2, Right).
Surgical Data and Additional Surgical Procedures
Surgical procedural data are presented in Table 2. In all cases, surgical treatments were instituted through a median sternotomy; epicardial lead implantation (n=4) and tricuspid valve repair (n=3) were performed as additional surgical procedures after lead extraction. In 3 patients, lead extraction procedures were performed in 1 stage (vegetation: 2; severe lead adhesion: 1). In the other 6 patients, planned lead extraction with open heart surgery was conducted on a different day after the failed prior transvenous approach.
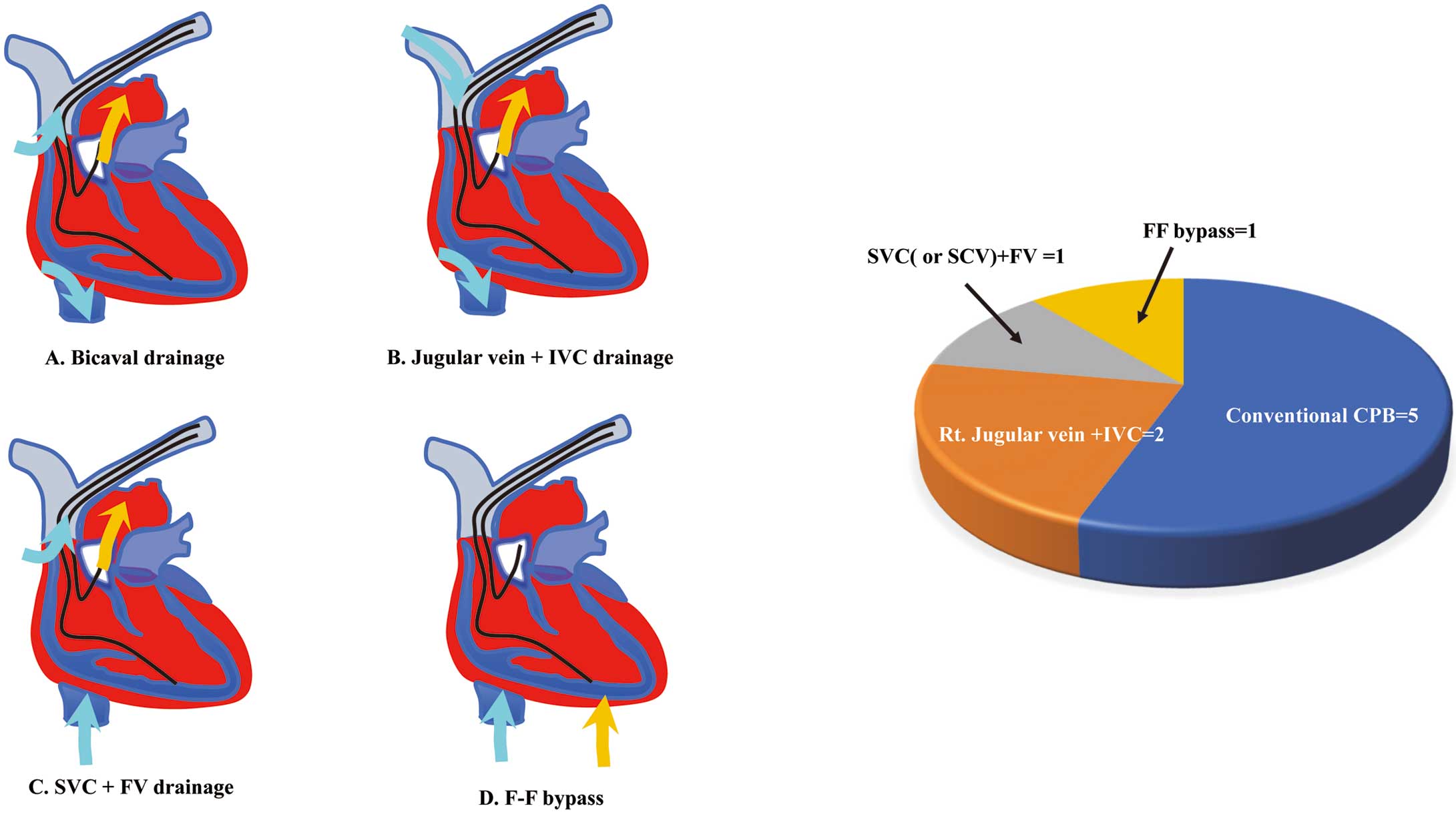
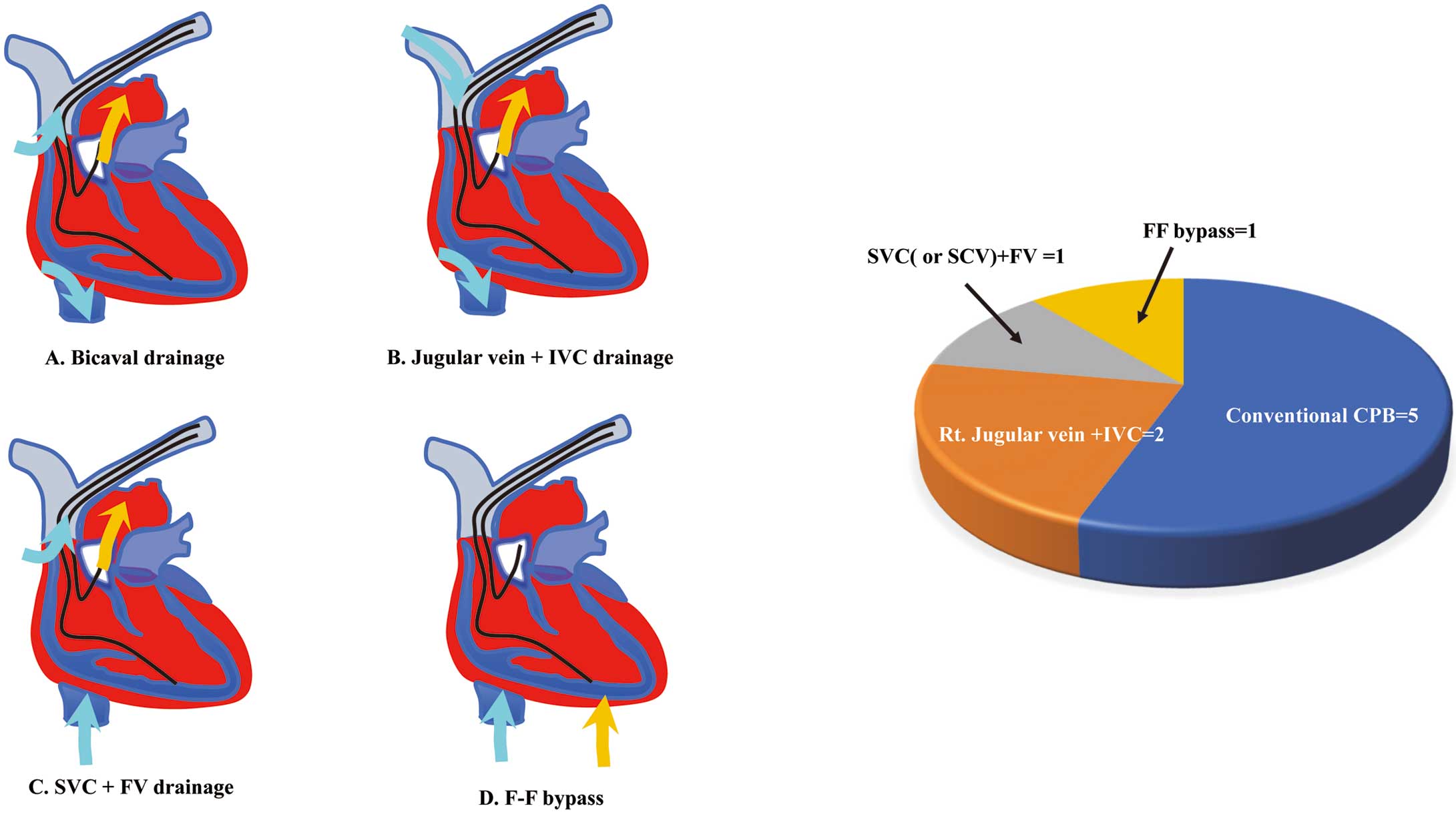
CPB pump settings and data are presented in Figure 3. Essentially, conventional bicaval venous cannulations were used during the open heart procedures (Figure 3A); however, when CIED leads and their adhesions encumbered the CPB pump settings, pump settings were changed based on lead positions, venous occlusions, and lead adhesions. Conventional CPB, established by ascending aorta perfusion and bicaval venting was used in 5 patients (Figure 3A). CPB established via ascending aorta perfusion with right jugular vein and inferior vena cava venting was used in 2 patients with severe lead adhesion at the SVC (Figure 3B). CPB established via ascending aorta perfusion with SVC (or SCV) and femoral vein venting was used in a patient with many leads in the RA or repeat median sternotomy after prior cardiac surgery (Figure 3C). Femoral-femoral bypass was used in 1 patient with severe adhesion at the pericardium due to CIED-related pericarditis (Figure 3D). The cardiac arrest technique with aortic cross-clamping was performed in 3 patients, with a mean cross-clamping time of 62.0±54.8 min (range 20–124 min). The remaining 6 patients underwent surgical procedures, including on-pump beating; overall, the mean pump time was 115.2±57.8 min (range 20–194 min).
Postoperative complications were examined in all patients (Table 3). Major morbidities were defined as prolonged ventilation (>72 h), acute renal failure, permanent stroke, deep sternal wound infection, and all-cause reoperation.16 One patient was on mechanical respirator management for >72 h; this patient had congestive heart failure before the surgical procedures. Minor complications included upper gastrointestinal bleeding (n=1) and phrenic nerve palsy (n=1).
Table 3. Preoperative Complications and Outcomes
| Follow-up period (years) |
5.7±3.7 |
| Perioperative complications |
| Major |
| Prolonged ventilator (>48 h) |
1 |
| Minor |
| Upper gastrointestinal bleeding |
1 |
| Phrenic nerve palsy |
1 |
| Outcome |
| Death at 30 days |
0 |
| Death in hospital |
0 |
| Alive (discharge) |
9 |
| Follow-up findings |
| Death |
1A |
| Alive |
8 |
| Events |
| Pericarditis |
1 |
| Additional operation |
2 |
| TVR |
1 |
| Leadless PM implantation |
1 |
Data are given as the mean±SD or n. ANon-cardiac cause. PM, pacemaker; TVR, tricuspid valve replacement.
Outcomes are presented in Table 3; the mean follow-up period was 5.7±3.7 years (range 1.5–12.1 years), and all 9 patients were discharged. Throughout the follow-up period, 1 patient died of non-cardiac disease (pneumonia); the remaining 8 patients survived. One patient underwent tricuspid valve replacement due to severe tricuspid valve regurgitation, occurring 3.8 years after the initial operation; 1 patient experienced pericarditis a few months after discharge and another patient underwent leadless pacemaker implantation due to pacing failure of the epicardial pacing lead, occurring 2.8 years after the operation. In 7 patients with CIED infection, there was no recurrence of infection during the follow-up period.
Discussion
Approximately 10% of our cohort required a surgical approach for CIED-related complications. Nine patients who underwent open heart surgery during the study period were considered unsuitable for transvenous lead extraction. Open heart surgeries were performed for failed prior transvenous approaches (n=6), intracardiac vegetation (n=2), and severe lead adhesion (n=1). For open heart surgery, extracorporeal circulation settings were decided on a case-by-case basis due to complicated CIED lead positions. We used both surgical and transvenous CIED lead extraction procedures without intraoperative procedural complications. Over 80% of candidates survived throughout long-term follow-up. Surgical management for CIED lead extraction was therefore safely achieved for patients who were unsuitable for the transvenous approach.
Surgical Approach for Unsuitable Isolated CIED Lead Extraction
In most CIED lead extraction cases, transvenous approaches are preferred because they are less invasive.9 The success rate of transvenous lead extraction is reported to be >90%;7 according to a Japanese study, 96.7% of target leads were completely removed.17 Despite the high success rate of the transvenous approach, there are still some patients who require open heart surgery for CIED lead extraction.6 Open heart lead extractions are preferred in high-risk patients to prevent potentially life-threatening complications, such as vascular injury and cardiac perforation.6,8–10 Expert statements and previous studies have defined high-risk patients for transvenous lead extraction.6,8–10,18 Indications for open heart surgery are failed transvenous lead extraction and leads attached to large vegetations.17 In ICD and pacing leads, transvenous lead extraction can fail due to long-dwelling leads (≥10 years).3 In addition, large vegetations have the potential to cause pulmonary embolization. In cases of vegetation-attached leads, open heart surgery is indicated for patients with a patent foramen ovale and atrial septal defect.3 Surgical lead removal is the preferred approach for patients with leads attached to vegetations with diameters >2 cm.6 The impacts of the size and shape of the vegetations remain undetermined. With regard to right-sided endocarditis, surgical procedures with a pump are warranted in some cases, such as those with persistent tricuspid valve vegetations (>2 cm), right heart failure secondary to severe tricuspid regurgitation, recurrent pulmonary emboli, or right heart failure secondary to severe tricuspid regurgitation.19 In addition, the transvenous approach is a high-risk procedure for patients with potential extracardiac or extravascular leads on preoperative computed tomography or echocardiography.11
In our cohort, 9 of the 152 patients who underwent CIED lead extractions were considered high risk (5.9%); these patients included 6 with prior failed transvenous lead extractions, 2 with vegetation, and 1 with severe lead adhesion on preoperative evaluation. Mean lead age was very high (19.5±7.0 years; range 3.9–37.1 years). Long-dwelling leads cause the transvenous lead extraction procedure to fail due to hard lead adhesion.20
Advantages of Combining Open Heart Surgery and Transvenous Tools
In most previous reports regarding open heart CIED extraction, direct surgical procedures were used to release all parts of lead adhesion.4,5,18,21–23 These procedures enabled exfoliation of adhered tissue from the leads under direct visualization; however, the surgical approach cannot always to access all parts of the CIED lead. For example, the SCV is covered by the clavicle and anatomically difficult to expose directly; here, transvenous tools have the potential to access and release lead adhesion. Transvenous extraction tools are used globally, with endovascular equipment used during and/or before open heart surgical procedures.
Surgical management for CIED complications should include seamless coalescence of transvenous and surgical treatments. In this study, transvenous tools were used in all patients during and/or before open heart surgery. Combined procedures may provide some advantages as therapeutic strategies in high-risk patients.
The first advantage of the surgical approach is safety in high-risk patients due to direct visualization. Although transvenous approaches are less invasive for CIED extraction, surgical approaches are safer. This is because a surgical approach with a median sternotomy provides direct access to the SVC and the RV free wall, which are sites where life-threatening complications frequently occur in the transvenous approach.24 The SVC is at a high risk of vascular tear due to severe adhesion between the lead and vessel tissue, especially in the case of ICD leads with an SVC coil,19,24–27 whereas the RV free wall is at high risk of RV perforation due to long-dwelling leads with tinned tips.25
The second advantage is that both direct and transvenous procedures can be used for lead extraction in the current era of widespread transvenous equipment. We divided the CIED lead pathway into 3 portions: the vascular portion, the SVC-RA junction, and the cardiac portion. The vascular portion included the vascular entry site and SCV, and transvenous tools were suitable for releasing lead adhesion. Because the SCV beneath the clavicle is anatomically difficult to expose directly, the SVC-RA junction posed the most frequent life-threatening complications and most severe lead adhesion.24–27 In this section, direct surgical dissection of the lead adhesion is safe in high-risk patients who are expected to experience severe lead adhesion. Rather than surgical procedures, transvenous equipment can be used at the SVC-RA junction under direct visualization with sternotomy. In the cardiac portion, surgical treatment is suitable for releasing lead tip adhesion; lead tips, especially the tinned type, can adhere to cardiac tissue. In the surgical approach, direct repair is possible without RV free wall perforation.25
Some studies have reported the use of transvenous sheaths in the retrograde approach.28 The transvenous retrograde approach is an advanced surgical approach that may be a less invasive surgical procedure than cutting and sawing the vascular portion. However, surgical and transvenous treatments do not need to be performed at the same time. Of note, failed transvenous approach attempts can prolong the operative time.29 Moreover, prolonged transvenous sessions may result in increased anesthesia duration during open heart surgery, which may induce further complications. In this series, all patients underwent both approaches during and/or before open heart surgery, and all CIED systems were completely removed without procedural complications.
The third advantage of the surgical approach is that additional CIED operations can be performed during the procedure. Epicardial lead implantations are useful for both pacing-dependent and infection cases. Some patients exhibit tricuspid valve regurgitation after the transvenous approach.30 The surgical approach has the potential to repair the tricuspid valve (i.e., leaflet repair, orifice repair) after lead extraction; in the present sample, 4 epicardial lead implantations and 3 tricuspid valve repairs were performed during the surgical approach.
Establishing Extracorporeal Circulation Settings for Patients With a CIED
Establishing CPB is an important procedure for safe open heart surgery; however, in patients with CIED, extracorporeal circulation settings needed to be decided on a case-by-case basis due to complicated CIED lead positions. Appropriate extracorporeal circulation can ensure good surgical visualization without blood in the RA, RV, and SVC. The most popular CPB setting is the ascending aorta with bicaval drainage cannulation,5,21,22 which is conventional for open heart surgery and may provide stable flow during surgery. In cases in which there are many leads in the SVC and RA, the leads prevent cannulation from these portions. In particular, SVC cannulation below innominate veins can help set up circulation in patients with many leads in the SVC; CPB with inferior vena cava cannulation only is another solution.21 CPB with femoral-femoral bypass is useful for the thoracotomy approach.11
Long-Term Follow-up and Outcomes
In the present study, 7 patients exhibited CIED infection; there were no incidences of death or recurrent CIED infection throughout the follow-up period. In addition, other open heart surgery patients were discharged without life-threatening complications.
The favorable outcomes in our study can be attributed to 2 factors. First, technological advances have made it possible to combine different techniques for CIED lead removal. In the 1990s, only surgical and invasive procedures were available for the extraction of all CIED components.3–5 Using combined procedures in high-risk patients provides not only safe, but also less invasive lead extraction. Second, our strategy for the management of CIED complications was based on modern guidelines. According to these guidelines, timely treatment could effectively address CIED complications, particularly CIED infection.14 This factor was important in reducing the mortality rate of surgical treatment.4
Thus, although transvenous lead extractions are less invasive, open heart surgery combined with transvenous techniques may be safer for high-risk patients who require CIED lead removal.
Study Limitations
This retrospective study has some limitations. Most importantly, the small size of our cohort may have reduced the power of the study. This study included a small number of high-risk patients with CIED who underwent open heart surgery. Among the 152 patients who underwent CIED removal, only 9 (5.9%) qualified as patients unsuitable for transvenous lead extraction. The high success rate (>90%) of transvenous lead extraction implies that life-threatening complications rarely occur with this technique. Therefore, only a few cases qualify as high-risk for transvenous lead removal.6,7 Future studies with larger cohorts are needed to confirm our findings.
Conclusions
Open heart surgery is still required for patients who are at a high risk of developing life-threatening complications from transvenous lead extraction. For the surgical management of CIED leads, surgical procedures and transvenous extraction tools can be combined in the CIED removal strategy. Intensive surgical procedures can therefore be performed safely in high-risk patients for transvenous lead extractions.
Sources of Funding
This study did not receive any specific funding.
Disclosures
The authors declare that there are no conflicts of interest.
IRB Information
The study protocol was approved by the Ethics Committee of the Nippon Medical School, Tokyo, Japan (Reference no. B-2022-505).
Data Availability
The deidentified participant data will be shared upon reasonable request. Data will become available immediately following publication. The data will be shared as Excel or csv files via email.
References
- 1.
Cabell CH, Heidenreich PA, Chu VH, Moore CM, Stryjewski ME, Corey GR, et al. Increasing rates of cardiac device infections among Medicare beneficiaries: 1990–1999. Am Heart J 2004; 147: 582–586.
- 2.
Voigt A, Shalaby A, Saba S. Continued rise in rates of cardiovascular implantable electronic device infections in the United States: Temporal trends and causative insights. Pacing Clin Electrophysiol 2010; 33: 414–419.
- 3.
Koneru JN, Ellenbogen KA. High-risk lead extraction using a hybrid approach: The blade and the lightsaber. J Cardiovasc Electrophysiol 2014; 25: 622–623.
- 4.
Frame R, Brodman RF, Furman S, Andrews CA, Gross JN. Surgical removal of infected transvenous pacemaker leads. Pacing Clin Electrophysiol 1993; 16: 2343–2348.
- 5.
Abad C, Manzano JJ, Quintana J, Bolaños J, Manzano JL. Removal of infected dual chambered transvenous pacemaker and implantation of a new epicardial dual chambered device with cardiopulmonary bypass: Experience with seven cases. Pacing Clin Electrophysiol 1995; 18: 1272–1275.
- 6.
Wilkoff BL, Love CJ, Byrd CL, Bongiorni MG, Carrillo RG, Crossley GH 3rd, et al. Transvenous lead extraction: Heart Rhythm Society expert consensus on facilities, training, indications, and patient management: This document was endorsed by the American Heart Association (AHA). Heart Rhythm 2009; 6: 1085–1104.
- 7.
Wazni O, Epstein LM, Carrillo RG, Love C, Adler SW, Riggio DW, et al. Lead extraction in the contemporary setting: The LExICon study: An observational retrospective study of consecutive laser lead extractions. J Am Coll Cardiol 2010; 55: 579–586.
- 8.
Kusumoto FM, Schoenfeld MH, Wilkoff BL, Berul CI, Birgersdotter-Green UM, Carrillo R, et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm 2017; 14: e503–e551, doi:10.1016/j.hrthm.2017.09.001.
- 9.
Bongiorni MG, Burri H, Deharo JC, Starck C, Kennergren C, Saghy L, et al. 2018 EHRA expert consensus statement on lead extraction: Recommendations on definitions, endpoints, research trial design, and data collection requirements for clinical scientific studies and registries: Endorsed by APHRS/HRS/LAHRS. Europace 2018; 20: 1217.
- 10.
Blomström-Lundqvist C, Traykov V, Erba PA, Burri H, Nielsen JC, Bongiorni MG, et al. European Heart Rhythm Association (EHRA) international consensus document on how to prevent, diagnose, and treat cardiac implantable electronic device infections-endorsed by the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS), the Latin American Heart Rhythm Society (LAHRS), International Society for Cardiovascular Infectious Diseases (ISCVID) and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Europace 2020; 22: 515–549.
- 11.
Goyal SK, Ellis CR, Ball SK, Ahmad R, Hoff SJ, Whalen SP, et al. High-risk lead removal by planned sequential transvenous laser extraction and minimally invasive right thoracotomy. J Cardiovasc Electrophysiol 2014; 25: 617–621.
- 12.
Stockhausen K. The Declaration of Helsinki: Revising ethical research guidelines for the 21st century. Med J Aust 2000; 172: 252–253.
- 13.
Nogami A, Kurita T, Abe H, Ando K, Ishikawa T, Imai K, et al. JCS/JHRS 2019 guideline on non-pharmacotherapy of cardiac arrhythmias. Circ J 2021; 85: 1104–1244.
- 14.
Miyagi Y, Sakamoto SI, Kawase Y, Oomori H, Watanabe Y, Kurita J, et al. Temporal and microbiological analysis of cardiac implantable electrical device infections: A retrospective study. Circ Rep 2021; 3: 488–496.
- 15.
Miyagi Y, Kawase Y, Kunugi S, Oomori H, Sasaki T, Sakamoto SI, et al. Histological properties of oscillating intracardiac masses associated with cardiac implantable electric devices. J Arrhythm 2020; 36: 478–484.
- 16.
Seese L, Sultan I, Gleason TG, Navid F, Wang Y, Thoma F, et al. The impact of major postoperative complications on long-term survival after cardiac surgery. Ann Thorac Surg 2020; 110: 128–135.
- 17.
Shoda M, Kusano K, Goya M, Nishii N, Imai K, Okamoto Y, et al. Lead EXtraction (J-LEX) registry: Annual report 2019. J Arrhythm 2022; 38: 187–191.
- 18.
Chaudhry UA, Harling L, Ashrafian H, Athanasiou C, Tsipas P, Kokotsakis J, et al. Surgical management of infected cardiac implantable electronic devices. Int J Cardiol 2016; 203: 714–721.
- 19.
Shmueli H, Thomas F, Flint N, Setia G, Janjic A, Siegel RJ. Right-sided infective endocarditis 2020: Challenges and updates in diagnosis and treatment. J Am Heart Assoc 2020; 9: e017293, doi:10.1161/JAHA.120.017293.
- 20.
Epstein LM, Love CJ, Wilkoff BL, Chung MK, Hackler JW, Bongiorni MG, et al. Superior vena cava defibrillator coils make transvenous lead extraction more challenging and riskier. J Am Coll Cardiol 2013; 61: 987–989.
- 21.
Camboni D, Wollmann CG, Löher A, Gradaus R, Scheld HH, Schmid C. Explantation of implantable defibrillator leads using open heart surgery or percutaneous techniques. Ann Thorac Surg 2008; 85: 50–55.
- 22.
Okada M, Narita Y, Araki Y, Oshima H, Usui A, Ueda Y. Long-term outcome of complete cardiovascular implantable electronic device removal with cardiopulmonary bypass. J Artif Organs 2013; 16: 164–169.
- 23.
Chang JP, Chen MC, Guo GB, Kao CL. Less-invasive surgical extraction of problematic or infected permanent transvenous pacemaker system. Ann Thorac Surg 2005; 79: 1250–1254.
- 24.
Brunner MP, Cronin EM, Wazni O, Baranowski B, Saliba WI, Sabik JF, et al. Outcomes of patients requiring emergent surgical or endovascular intervention for catastrophic complications during transvenous lead extraction. Heart Rhythm 2014; 11: 419–425.
- 25.
Hauser RG, Katsiyiannis WT, Gornick CC, Almquist AK, Kallinen LM. Deaths and cardiovascular injuries due to device-assisted implantable cardioverter-defibrillator and pacemaker lead extraction. Europace 2010; 12: 395–401.
- 26.
Cronin EM, Brunner MP, Tan CD, Rodriguez ER, Rickard J, Martin DO, et al. Incidence, management, and outcomes of the arteriovenous fistula complicating transvenous lead extraction. Heart Rhythm 2014; 11: 404–411.
- 27.
Epstein AE, Kay GN, Plumb VJ, Dailey SM, Anderson PG. Gross and microscopic pathological changes associated with nonthoracotomy implantable defibrillator leads. Circulation 1998; 98: 1517–1524.
- 28.
Rodriguez Y, Garisto JD, Carrillo RG. A novel retrograde laser extraction technique using a transatrial approach: An alternative for complex lead extractions. Circ Arrhythm Electrophysiol 2011; 4: 501–505.
- 29.
Bontempi L, Vassanelli F, Cerini M, Inama L, Salghetti F, Giacopelli D, et al. Predicting the difficulty of a transvenous lead extraction procedure: Validation of the LED index. J Cardiovasc Electrophysiol 2017; 28: 811–818.
- 30.
Park SJ, Gentry JL 3rd, Varma N, Wazni O, Tarakji KG, Mehta A, et al. Transvenous extraction of pacemaker and defibrillator leads and the risk of tricuspid valve regurgitation. JACC Clin Electrophysiol 2018; 4: 1421–1428.