論文ID: CJ-66-0096
論文ID: CJ-66-0096
Forty-five years have passed since 1967,1 when the first case series of Kawasaki disease was reported. Currently, more than half of the patients diagnosed with Kawasaki disease are 20 years of age or older. As this timeline suggests, it is expected that more than 10,000 patients with cardiovascular sequelae in Kawasaki disease have reached adulthood. However, since Kawasaki disease develops most frequently by around 1 year of age, many internists are still not familiar with it (See Table 3). Recent issues on Kawasaki disease include the high percentage of patients who stop visiting their clinic in early adolescence or later, and the occurrence of acute coronary syndrome in adults with a history of Kawasaki disease in whom coronary artery lesions were considered regressed after the acute phase of the disease. We also have to address the problem of susceptibility to atherosclerosis in patients with a history of vasculitis due to Kawasaki disease.
Because the pathophysiology of cardiovascular sequelae in Kawasaki disease changes over time during childhood, adolescence and adulthood, guidance on the diagnosis, treatment and management of cardiovascular sequelae in different ages was required, the Japanese Circulation Society Joint Working Groups published the Guidelines for Diagnosis and Management of Cardiovascular Sequelae in Kawasaki Disease in 2003,2 and the first revision of the guidelines in 2008.3 The present second revision reflects updates over recent years.
The outline of the present revision is essentially similar to the previous versions. However, the present revision includes detailed descriptions of the pathophysiology of cardiovascular sequelae to provide important information for the diagnosis and treatment of sequelae, and describes genetic background of coronary sequelae and coronary hemodynamics. The chapters on the management and education of children with Kawasaki disease were revised and further segmented to provide more practical information suitable in the clinical setting. Because the susceptibility to atherosclerosis in adults with a history of the disease is expected to become a more important problem in the future, new findings on the pathological and clinical points of view that have been obtained by now are added in this revision.
The Joint Working Groups discussed how to classify coronary aneurysms during the acute phase. Although giant aneurysms were defined as aneurysms with an internal diameter of >8 mm in children under five years of age, and those with the internal diameter of a segment measuring >4 times that of an adjacent segment in children over five years of age, giant aneurysms in children under five years of age are defined as those with the internal diameter of ≥8 mm in a currently ongoing national epidemiological survey, recent academic presentations and literature about Kawasaki disease. We thus partly modified the classification of giant aneurysms to fit the clinical practice (See Table 4).
Although the present guidelines are based in principle on available evidence, the diagnosis and treatment of cardiovascular sequelae in Kawasaki disease are often based on case reports. Emphasis was therefore placed on case reports in the present guidelines as well. Table 1 lists the criteria for levels of recommendations on the procedure and treatment of cardiovascular sequelae in Kawasaki disease. We hope this revision will help physicians provide better treatment for their patients.
| Class I | Conditions for which there is evidence for and/or general agreement that the procedure or treatment is useful and effective. |
| Class II | Conditions for which there is conflicting evidence and/or a divergence of opinion regarding the usefulness/efficacy of a procedure or treatment. |
| Class III | Conditions for which there is evidence and/or general agreement that the procedure or treatment is not useful/effective and may in some cases be harmful. |
Table 2 lists abbreviations used in the present guidelines.
| 3D | three-dimensional | IVUS | intravascular ultrasound |
| ACC | American College of Cardiology | LDL-C | low density lipoprotein cholesterol |
| ACCP | American College of Chest Physicians | LP | late potential |
| ACE | angiotensin converting enzyme | LVEF | left ventricular ejection fraction |
| AHA | American Heart Association | MCLS | infantile acute febrile mucocutaneous lymph node syndrome |
| ALT | alanine aminotransferase | MCP-1 | monocyte chemoattractant protein-1 |
| AMI | acute myocardial infarction | MDCT | multi-detector row computed tomography |
| APTT | activated partial thromboplastin time | MLC | myosin light chain |
| APV | average peak flow velocity | MRA | magnetic resonance angiography |
| ARB | angiotensin II receptor blocker | MRCA | magnetic resonance coronary angiography |
| AST | aspartate aminotransferase | MRI | magnetic resonance imaging |
| ATP | adenosine triphosphate | NO | nitric oxide |
| BID | two times a day | NSAIDs | nonsteroidal antiinflammatory drugs |
| BNP | brain natriuretic peptide | nST | non-stress test |
| CABG | coronary artery bypass grafting | OD | once daily |
| CAG | coronary angiography | PCI | percutaneous coronary intervention |
| CASP3 | caspase 3 | PGI2 | prostacyclin |
| CFR | coronary flow reserve | POBA | plain old balloon angioplasty |
| CK | creatine kinase | pro-UK | pro-urokinase |
| CK-MB | creatine kinase-myocardial band | PTCRA | percutaneous transluminal coronary rotational atherectomy |
| CRP | C reactive protein | PVC | premature ventricular contraction |
| ECG | electrocardiography | QGS | quantitative gated SPECT |
| EF | ejection fraction | QOL | quality of life |
| FFRmyo | myocardial fractional flow reserve | sc | subcutaneous |
| FMD | flow-mediated dilatation | SCAI | Society for Cardiovascular Angiography and Interventions |
| % FS | % fractional shortening | SNP | single nucleotide polymorphism |
| HDL-C | high density lipoprotein cholesterol | SPECT | single photon emission computed tomography |
| H-FABP | heart-type fatty acid-binding protein | SSFP | steady-state free precession |
| ICAM-1 | intercellular adhesion molecule 1 | TC | total cholesterol |
| ICT | intracoronary thrombolysis | Tc | technetium |
| IgG | immunoglobulin G | TG | triglyceride |
| I map | isopotential map | TID | three times a day |
| INR | international normalized ratio | TnI | troponin I |
| ISDN | isosorbide dinitrate | TnT | troponin T |
| ITPKC | inositol 1,4,5-triphosphate 3-kinase C | t-PA | tissue plasminogen activator |
| iv | intravenous | TTP | thrombotic thrombocytopenic purpura |
| IVIG | intravenous immunoglobulin | UK | urokinase |
According to the 21st nationwide survey of Kawasaki disease (2009~2010), the number of patients newly diagnosed with Kawasaki disease was 10,975 (6,249 males and 4,726 females) in 2009, and 12,755 (7,266 males and 5,489 females) in 2010, yielding a total of 23,730 patients, consisting of 13,515 male and 10,215 female patients.4 The sex ratio (male/female) of patients was 1.32, and that of prevalence was 1.26, suggesting Kawasaki disease is more common among males. The mean prevalence during the 2-year survey period was 222.9 patients/100,000 children 0~4 years of age (247.6 in males and 196.9 in females). The total number of patients with Kawasaki disease reported in the past 20 surveys is 272,749 (157,865 males and 114,884 females).

Changes over time in the number of patients with Kawasaki disease and mortality. In the 21st nationwide survey, 1 patient (female) died in 2 years, with a mortality of 0.004%. IVIG, intravenous immunoglobulins. Adapted from Nakamura Y, et al. J Epidemiol 2012; 22: 216–221,4 with modification.
Figure 1 shows changes over time in the number of patients newly diagnosed with Kawasaki disease each year.4 In addition nationwide increases occurred in 1979, 1982 and 1986, the number of patients have tended to increase annually. There is a seasonable pattern in the number of new cases. In the recent two years the number of new cases was low in fall (September and October) while high in spring and summer. Patients under three years of age accounted for 66.8%. The incidence rate by age shows a monomodal distribution and is highest in boys 6~8 months of age and girls 9~11 months of age. Kawasaki disease was especially prevalent in Kanagawa, Nagano and Wakayama Prefectures, and there have been sporadic increases in cases in specific areas.
Patients with a family history of Kawasaki disease accounted for 1.6% of all patients. Among the reported cases, 163 patients (0.7% of the reported cases; 0.6% in males and 0.8% in females) had a parent who has suffered from Kawasaki disease (74 fathers and 69 mothers had the disease). Recurrent cases accounted for 3.6% (3.9% in males and 3.1% in females). In the latest 2 years, one patient died (mortality: 0.004%). The patient had typical Kawasaki disease that occurred at 3 months of age, and died within 2 months after the onset due to cerebral infarction.
Table 3 summarizes guidance for the diagnosis of Kawasaki disease.5
| This is a disease of unknown etiology affecting most frequently infants and young children under 5 years of age. The symptoms can be classified into two categories, principal symptoms and other significant symptoms or findings. |
| A. Principal symptoms |
| 1. Fever persisting for 5 days or more (inclusive of those cases in whom the fever has subsided before the 5th day in response to therapy) |
| 2. Bilateral conjunctival congestion |
| 3. Changes of lips and oral cavity: Redding of lips, strawberry tongue, diffuse injection of oral and pharyngeal mucosa |
| 4. Polymorphous exanthema |
| 5. Changes of peripheral extremities: |
| (Acute phase): Redding of palms and soles, indurative edema |
| (Convalescent phase): Membranous desquamation from fingertips |
| 6. Acute nonpurulent cervical lymphadenopathy |
| At least five items of 1∼6 should be satisfied for diagnosis of Kawasaki disease. However, patients with four items of the principal symptoms can be diagnosed as Kawasaki disease when coronary aneurysm or dilatation is recognized by two-dimensional (2D) echocardiography or coronary angiography. |
| B. Other significant symptoms or findings |
| The following symptoms and findings should be considered in the clinical evaluation of suspected patients. |
| 1. Cardiovascular: Auscultation (heart murmur, gallop rhythm, distant heart sounds), ECG changes (prolonged PR/QT intervals, abnormal Q wave, low-voltage QRS complexes, ST-T changes, arrhythmias), chest X-ray findings (cardiomegaly), 2D echo findings (pericardial effusion, coronary aneurysms), aneurysm of peripheral arteries other than coronary (e.g., axillary), angina pectoris or myocardial infarction |
| 2. Gastrointestinal (GI) tract: Diarrhea, vomiting, abdominal pain, hydrops of gallbladder, paralytic ileus, mild jaundice, slight increase of serum transaminase |
| 3. Blood: Leukocytosis with shift to the , thrombocytosis, increased erythrocyte sedimentation rate (ESR), positive C reactive protein (CRP), hypoalbuminemia, increased α2-globulin, slight decrease in erythrocyte and hemoglobin levels |
| 4. Urine: Proteinuria, increase of leukocytes in urine sediment |
| 5. Skin: Redness and crust at the site of BCG inoculation, small pustules, transverse furrows of the finger nails |
| 6. Respiratory: Cough, rhinorrhea, abnormal shadow on chest X-ray |
| 7. Joint: Pain, swelling |
| 8. Neurological: Cerebrospinal fluid (CSF) pleocytosis, convulsion, unconsciousness, facial palsy, paralysis of the extremities |
| Remarks |
| 1. For item 5 under principal symptoms, the convalescent phase is considered important |
| 2. Nonpurulent cervical lymphadenopathy is less frequently encountered (approximately 65%) than other principal symptoms during the acute phase |
| 3. Male: Female ratio: 1.3∼1.5:1, patients under 5 years of age: 80∼85%, mortality: 0.1% |
| 4. Recurrence rate: 2∼3%, proportion of siblings cases: 1∼2% |
| 5. Approximately 10% of the total cases do not fulfill five of the six principal symptoms, in which other diseases can be excluded and Kawasaki disease is suspected. In some of these patients coronary aneurysm or dilatation have been confirmed |
Adapted from Kawasaki Disease Study Group of the Ministry of Health, Labour and Welfare. Guidelines for the Diagnosis of Kawasaki Disease (MCLS, infantile acute febrile mucocutaneous lymph node syndrome), fifth revision. J Jpn Pediatr Soc 2002; 106: 836–837.5
Among the patients assessed in the 21st nationwide survey, 9.3% (11.0% in males and 7.1% in females) experienced acute-phase cardiovascular complications, and 3.0% (3.6% in males and 2.1% in females) experienced cardiovascular sequelae. Acute-phase complications included coronary dilatation in 7.26%, valvular lesions in 1.19%, aneurysms in 1.04%, giant aneurysms in 0.24%, coronary stenosis in 0.03%, and myocardial infarction in 0.01%, which were less prevalent as compared with the previous survey.4

Change over time in the incidence of coronary sequelae in Kawasaki disease. Source: Nakamura Y, et al. J Epidemiol 2012; 22: 216–221.4
Cardiovascular sequelae included coronary dilatation in 1.90%, aneurysms in 0.78%, valvular lesions in 0.29%, giant aneurysms in 0.22%, coronary stenosis in 0.03%, and myocardial infarction in 0.02%. The incidence rate of giant aneurysms was about three-fold higher in males than in females.4
Day 4 after onset was the most frequent day of the first visit, and 24.4% of the patients first visited the clinic for Kawasaki disease on day 4 after onset, and 65.9% of the patients visited the clinic by day 4 after onset.
1.3 Treatment4The first administration of intravenous immunoglobulin (IVIG) was given most frequently on day 5 after onset on which 37.4% of the patients received the treatment. Among patients under 2 years of age, 72.8% of them started IVIG therapy by day 5 after onset.
Patients receiving IVIG accounted for 89.5% of the patients assessed in the 21st nationwide survey, and 16.6% of the patients did not respond to the treatment. The daily dose of IVIG was 1,900~2,099 mg/kg in 84.5% of the patients receiving the drug, and 900~1,099 mg/kg in 13.7%. The duration of treatment was one day in 92.0%, and two days in 7.9%. Additional doses of IVIG were given to 19.1% of the patients. Male patients were dominant in this patient group. Among patients receiving IVIG therapy during the acute phase, 6.5%, 0.9% and 0.8% of the patients received steroids, infliximab and immunosuppressants such as cyclosporine, respectively.
Among patients not responding to IVIG therapy, 29.0%, 4.3%, and 3.7% of them were treated with steroids, infliximab and immunosuppressants, respectively. Plasmapheresis was conducted in 2.2% of the patients.
1.4 Non-Cardiovascular Complications4Non-cardiovascular complications observed in patients assessed in the 21st nationwide survey were bronchitis/pneumonia in 2.58%, severe myocarditis in 0.16%, encephalitis/encephalopathy in 0.09%, tachyarrhythmia in 0.07%, and macroscopic hematuria in 0.04%. The incidence rates of encephalitis/encephalopathy, severe myocarditis, vomiting, and diarrhea were higher in female patients than in male patients.
1.5 International ComparisonThe prevalence of Kawasaki disease differs substantially among countries. Japan is the highest prevalence of Kawasaki disease in Asia and Oceania. The prevalence of Kawasaki disease in East Asian countries is higher than any other countries, and the number of cases tends to increase in China, Hong Kong, Taiwan and Korea. The prevalences in Korea, Hong Kong, and Taiwan is half, third, and third of that in Japan, respectively. The prevalence in China ranges substantially from 1/100 to 1/7 of that in Japan.
2. Genetic Background of Kawasaki DiseaseAlthough Kawasaki disease is not a genetic disease, the possibility of a genetic predisposition toward it has been suggested by the findings that (1) the incidence of Kawasaki disease in Japan is 10~20-fold that in Western countries, (2) the incidence of Kawasaki disease among siblings of patients is about 10-fold that in the general population, and (3) the incidence in offspring of parents with a history of Kawasaki disease is about twice that in the general population. Although almost all genetic investigation on Kawasaki disease that were available during the preparation of the previous revision were case-control studies that investigated specific genes suspected to be involved in Kawasaki disease, six reports of genome-wide association studies to discover genetic polymorphisms without such hypotheses have been published thereafter.6–11
These studies have indicated that the susceptibility to Kawasaki disease may be associated with N-acetylated-α-linked acidic dipeptidase-like 2 (NAALADL2);6 zinc finger homeobox 3 (ZFHX3);6 pellino homolog 1 (PELI1);7 coatomer protein complex beta-2 subunit (COPB2);8 endoplasmic reticulum aminopeptidase 1 (ERAP1);8 immunoglobulin heavy chain variable region (IGVH); Fc fragment of immunoglobulin G (IgG), low affinity IIa, receptor (FCGR2A);9,11 inositol 1,4,5-triphosphate 3-kinase C (ITPKC);9 family with sequence similarity 167 member A (FAM167A);10,11 B lymphoid kinase (BLK);10,11 CD40 ;10,11 and human leukocyte antigen (HLA).11 Genome-wide linkage disequilibrium analyses have identified ITPKC,12 caspase 3 (CASP3),13 ATP (adenosine triphosphate)-binding cassette, sub-family C, member 4 (ABCC4),14 which were then found in case-control studies that these genetic variations are significantly more common in patients with Kawasaki disease than in healthy individuals.
3. Severity ClassificationKawasaki disease is considered severe when coronary artery lesions develop in association with the disease (Table 4). As treatment options for Kawasaki disease have increased, different scoring systems have been proposed to predict prognosis of patients with coronary artery lesions according to the patient’s characteristics, blood test results, and clinical course. The scoring system by Asai and Kusakawa15 were used widely in the 1970 s and 1980 s when echocardiography was not common to assess whether coronary angiography (CAG) is indicated for or not. The Iwasa score16 and the Harada score17 were developed to assess the indication of IVIG.
| A. Classification of coronary aneurysms during the acute phase |
| - Small aneurysms (ANs) or dilatation (Dil): localized dilatation with ≤4 mm internal diameter |
| In children ≥5 years of age, the internal diameter of a segment measures <1.5 times that of an adjacent segment |
| - Medium aneurysms (ANm): aneurysms with an internal diameter from >4 mm to <8 mm |
| In children ≥5 years of age, the internal diameter of a segment measures 1.5∼4 times that of an adjacent segment |
| - Giant aneurysms (ANl): aneurysms with an internal diameter of ≥8 mm |
| In children ≥5 years of age, the internal diameter of a segment measures >4 times that of an adjacent segment |
| B. Severity classification |
| The severity of Kawasaki disease is classified into the following 5 grades on the basis of findings of echocardiography and selective coronary angiography or other methods: |
| I. No coronary dilatation: patients with no coronary dilatation including those in the acute phase |
| II. Transient coronary dilatation during the acute phase: patients with slight and transient coronary dilatation which typically subsides within 30 days after onset |
| III. Regression: patients who still exhibit coronary aneurysms meeting the criteria for dilatation or more severe change on day 30 after onset, despite complete disappearance of changes in the bilateral coronary artery systems during the first year after onset, and who do not meet the criteria for Group V |
| IV. Remaining coronary aneurysm: patients in whom unilateral or bilateral coronary aneurysms are detected by coronary angiography in the second year or later and who do not meet the criteria for Group V |
| V. Coronary stenotic lesions: patients with coronary stenotic lesions detectable by coronary angiography |
| (a) Patients without ischemic findings: patients without ischemic signs/symptoms detectable by laboratory tests or other examinations |
| (b) Patients with ischemic findings: patients with ischemic signs/symptoms detectable by laboratory tests or other examinations |
| Other clinical symptoms or findings: |
| When patients have moderate or severe valvular disease, heart failure, severe arrhythmia, or other cardiac disease, such conditions should be described in addition to the severity of Kawasaki disease. |
In the current situation where the benefits of initial therapy with IVIG have been established, patients at the highest risk of coronary artery lesions are those not responding to IVIG therapy. Unresponsiveness to IVIG therapy is a surrogate endpoint for the development of coronary artery lesions, and represents the severity of Kawasaki disease. In 2006, scoring systems to predict unresponsiveness to IVIG therapy were published.18–20 These scoring systems are able to predict unresponsiveness to IVIG therapy at a sensitivity of around 80%, and also predict occurrence of coronary artery lesions at a similar sensitivity. The reproducibility of these scoring systems has been demonstrated in Japan,21,22 while in North America, the sensitivity of these systems is as low as 30~40%.23 Table 5 lists commonly used scoring systems.18–20
| Threshold | Point | |
|---|---|---|
| Kobayashi score18 (≥5 points; sensitivity 76%, specificity 80%) | ||
| Na | ≤133 mmol/L | 2 |
| AST | ≥100 IU/L | 2 |
| Day of starting treatment (or diagnosis) | Day 4 after onset or earlier | 2 |
| Neutrophils | ≥80% | 2 |
| CRP | ≥10 mg/dL | 1 |
| Platelets | ≤300,000/μL | 1 |
| Age (months) | ≤12 months | 1 |
| Egami score19 (≥3 points; sensitivity 76%, specificity 80%) | ||
| ALT | ≥80 IU/L | 2 |
| Day of starting treatment (or diagnosis) | Day 4 after onset or earlier | 1 |
| CRP | ≥8 mg/dL | 1 |
| Platelets | ≤300,000/μL | 1 |
| Age (months) | ≤6 months | 1 |
| Sano score20 (≥2 points; sensitivity 77%, specificity 86%) | ||
| AST | ≥200 IU/L | 1 |
| Total bilirubin | ≥0.9 mg/dL | 1 |
| CRP | ≥7 mg/dL | 1 |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C reactive protein; IVIG, intravenous immunoglobulin; Na, sodium.
A diagnosis of Kawasaki disease is made according to “Diagnostic Guidelines of Kawasaki Disease (MCLS: Infantile Acute Febrile Mucocutaneous Lymph Node Syndrome)”5 (Table 3) that describes the following six major findings.
1. Fever persisting for 5 days or more (inclusive of those cases in whom the fever has subsided before the 5th day in response to therapy)
2. Bilateral conjunctival congestion
3. Changes of lips and oral cavity: Reddening of lips, strawberry tongue, diffuse injection of oral and pharyngeal mucosa
4. Polymorphous exanthema
5. Changes of peripheral extremities:
Acute phase: Reddening of palms and soles, indurative edema
Convalescent phase: Membranous desquamation from fingertips
6. Acute nonpurulent cervical lymphadenopathy
Patients with at least five of the above six major findings are diagnosed as typical Kawasaki disease (described as “level A certainty” in the questionnaires for the nationwide survey4). A diagnosis of atypical Kawasaki disease (“level B certainty”) is made for patients with four of the six major findings in whom two-dimensional echocardiography or cardioangiography during illness revealed coronary aneurysms or dilatation and other diseases have been excluded. A diagnosis of incomplete Kawasaki disease is made for other patients such as those who meet four of the six findings but do not have coronary aneurysms and those who have three of the six findings and have coronary aneurysms after other diagnoses are excluded.
In the 21st nationwide survey where 23,730 patients were registered during the 2-year survey period, patients with typical, atypical, and incomplete Kawasaki disease accounted for 78.7% (79.0% in males and 78.4% in females), 2.6% (2.7% and 2.5%), and 18.6% (18.3% and 19.0%), respectively.4 The percentage of incomplete Kawasaki disease has increased over time. Incomplete Kawasaki disease is more prevalent in young children <2 years of age, and older children ≥6 years of age. Patients with incomplete Kawasaki disease met four, three, two and one of the six major findings in 65.6%, 26.6%, 6.1%, 0.7%, respectively, and the number of criteria met was unknown in 0.9% of them.
A diagnosis of incomplete Kawasaki disease should not be based only on the number of findings observed, and physicians should interpret the clinical picture of individual patients. Redness of the BCG inoculation site in infants and multilocular cervical lymphadenopathy in older children are relatively specific to Kawasaki disease. Physicians should also examine laboratory results for findings typical for Kawasaki disease. Specifically, Kawasaki disease is often associated with increased direct bilirubin, increased hepatic enzyme levels, neutrophilia with left shift, thrombopenia, increased C reactive protein (CRP) and increased brain natriuretic peptide (BNP). Physicians should also observe patients for cardiac complications other than coronary artery lesions, such as cardiac dysfunction, pericardial effusion, and atrioventricular valve regurgitation.
Coronary artery lesions are prevalent in patients with incomplete Kawasaki disease.24–26 A recent meta-analysis has reported that the risk of occurrence of coronary artery lesions is higher in patients with incomplete Kawasaki disease than in those with typical disease (Odds ratio: 1.45; 95% confidence interval: 1.16~1.81).27 Physicians should consider high-dose IVIG therapy for patients with at least four major findings as those for patients with typical Kawasaki disease. Similar treatment equivalent to those for typical cases are also recommended for patients who show only three major findings or less.
Following the publication of the previous guidelines, genome-wide genetic analysis such as genome-wide SNP (single nucleotide polymorphism) analysis and linkage disequilibrium analysis have been conducted after the release of the previous revision of the guidelines, and genes associated with the susceptibility of Kawasaki disease and coronary artery lesions have been reported.11,12,28,29 Case-control studies conducted by different study groups have confirmed that ITPKC and CASP3 genes are associated with coronary artery lesions due to Kawasaki disease.11,13,30 ITPKC and CASP3 are among the genes specified in genome-wide gene analyses to be related to the susceptibility of Kawasaki disease. However, as many of these genes have no association with the development of coronary artery lesions due to Kawasaki disease, it is suspected that different genes are playing different roles in the development of Kawasaki disease and the development of coronary artery lesions. Detailed genome-wide SNP analysis should be conducted in a sufficiently large number of patients with coronary artery lesions to clarify these issues.
2. Pathology of Cardiovascular Sequelae 2.1 Coronary Artery LesionsKawasaki disease is a systemic vasculitis that often affects coronary arteries. Cardiovascular sequelae is becoming less prevalent due to the advancement in treatment, but it is estimated that in Japan more than 10,000 adults with a history of Kawasaki disease are living with cardiovascular sequelae.
2.1.1 Natural Course of Acute-Phase Coronary ArteritisCoronary arteritis due to Kawasaki disease develops on day 6~8 after onset when inflammatory cells infiltrate in the intima and adventitia of arteries. This leads to inflammation of all layers of arteries (e.g., panarteritis) around day 10 after onset, and which rapidly progresses to diffuse inflammation affecting the entire circumference of the artery. The cells lining arteries are severely attacked by monocytes, macrophages, neutrophils and other inflammatory cells, and arterial dilatation occurs on around day 12 after onset.31,32 Significant infiltration of inflammatory cells continues by around day 25 after onset, and inflammation subsides by around day 40 after onset.
2.1.2 Coronary Sequelaea. Reduction and Regression of Coronary Aneurysms
Coronary aneurysms remaining ≥30 days after the onset of Kawasaki disease typically decrease in size during the convalescent phase or later. “Regression” of coronary aneurysms, i.e., disappearance of abnormal findings on CAG, often occurs within 1~2 years after onset and typically occurs in the case of small or medium aneurysms.33 Histopathologically, the regression of coronary aneurysms due to Kawasaki disease is an apparent normalization of lumen diameter through circumferential intimal hyperplasia with the migration and proliferation of smooth muscle cells.34 It has been reported that patients may develop coronary stenosis at the site of regressed coronary aneurysms, a decrease in diastolic function.35 or abnormal vascular endothelial function36–38 after a long period of time. Patients should thus be followed up even after regression of coronary aneurysms.
b. Arteries With Remaining Aneurysms
Medium or giant aneurysms that remained during the remote phase typically show the following two different pathological features.
The first type is patent aneurysms without regression. The wall of aneurysms consists of hyalinized fibrous tissues with diffuse calcification. At the inlet and outlet of the aneurysm, intimal hyperplasia and/or luminal narrowing due to organized thrombus are noted.39,40 There have been reported cases of acute coronary syndrome due to thrombotic occlusion of an aneurysm.41
The second type is aneurysms with luminal thrombotic occlusion and partial recanalization. The recanalized lumen is surrounded by a thick layer of smooth muscle cells, and the cross-sectional view of the aneurysm shows a lotus-root appearance. Recanalized lumens may become stenotic due to the proliferation of cellular fibrous tissues, and active remodeling is present at the site of aneurysms even during the remote phase.39,42
c. Coronary Arteries Without Aneurysm Formation
Autopsy of patients with a history of Kawasaki disease who died from causes other than the disease has revealed diverse findings in arteries including clear scars of healed arteritis43 and no scars.44 There is no medical consensus about long-term prognosis of coronary artery lesions due to Kawasaki disease. Investigation should be continued to accumulate clinical data.
2.2 Myocardial DisordersSymptoms of myocarditis often develop during the acute phase of Kawasaki disease, but disappear spontaneously. In a histopathological evaluation of patients who died during the acute phase of Kawasaki disease, all patients showed inflammatory cell infiltration in the myocardium. Characteristic findings included (1) a main finding is infiltration of inflammatory cells into the cardiac interstitium, and myocyte injury is rare; (2) neutrophils are predominant cells at the early phase, but monocytes and macrophages become predominant over time; (3) inflammatory cell infiltration is observed in all regions of the heart during the acute phase, and filtration is gradually localized in the basal area; and (4) inflammatory cells infiltration into the conducting system is also common.45 Some researchers have reported that interstitial fibrosis as a sequelae of myocarditis persists during the remote phase,46 while others have pointed out that myocardial lesions in this patient population often represent myocardial fibrosis due to previous ischemia in the area perfused by the coronary artery where the aneurysm is present and reported no changes due to myocarditis.47
2.3 Non-Coronary Arterial DisordersKawasaki disease is a systemic vasculitis syndrome that causes vasculitis in a variety of blood vessels including large arteries and small muscular arteries.48–50 Inflammation occurs in blood vessels located outside the solid organs almost spontaneously.51
3. Coronary Hemodynamics in Patients With Coronary Sequelae 3.1 Methods and Criteria for Assessment of Coronary HemodynamicsIt is useful to determine average peak flow velocity (APV), coronary flow reserve (CFR), myocardial fractional flow reserve (FFRmyo), shear stress, and peripheral vascular resistance, among other measures, using a 0.014-inch guide wire equipped with an ultrasonic probe and a high-sensitivity pressure sensor (Doppler wires or pressure wires) in order to evaluate the functional severity of coronary artery lesions due to Kawasaki disease. Especially, CFR (CFR=[stress APV]/[APV at rest], where APV is the value at peak dilatation after infusion of papaverine hydrochloride injection) and FFRmyo (FFRmyo=[Mean pressure at a site distal to the coronary lesion of interest]−{[mean right atrial pressure]/[mean pressure at the coronary ostium]}−[mean right atrial pressure], where these pressures are obtained simultaneously at peak dilatation after infusion of papaverine hydrochloride injection) are suitable for the evaluation of the presence/absence and severity of myocardial ischemia and presence/absence of peripheral coronary circulatory disorder. These values are also useful in selecting appropriate treatment strategies (catheter intervention vs. coronary artery bypass grafting [CABG]) and postoperative evaluation.
The reference values in children are 2.0 for CFR and 0.75 for FFRmyo,52 and identical to those in adults.53–56 Shear stress induces a mechanical stress on vascular endothelial cells, and affects hemodynamics through endothelium-derived vasoactive substances. The reference value of shear stress in children57 that is calculated with an approximation formula using APV and lumen diameter is 40 dyn/cm2.
The APV determined with the above method represents the velocity at the center of the lumen, and the flow velocity near the wall is lower than that at the center. Therefore the shear stress near the wall is lower than the APV. As coronary blood flow fairly correlates with APV, a ratio of the mean coronary blood pressure to APV may be used to calculate total peripheral resistance. The reference values of total peripheral resistance at rest and during vascular dilatation are 4.0 and 2.0, respectively.57
Measurements obtained with pressure wires are useful in the evaluation of stenotic lesions, and those with Doppler wires in the evaluation of dilatation lesions.
3.2 Change in Coronary Hemodynamics Associated With Coronary Artery Lesions 3.2.1 Hemodynamics in Coronary Aneurysms Without Significant Stenosis and in the Distal Vesselsa. Hemodynamics in Aneurysms
Turbulent blood flow is present in coronary artery aneurysms, especially giant aneurysms. Although there is no decrease in perfusion pressure, a significant decrease in shear stress, which is known to damage vascular endothelial cells, is noted. It is considered that endothelial cells in giant aneurysms are seriously damaged by vasculitis and hemodynamic change. Vascular endothelial dysfunction promotes vasoconstriction, and increases susceptibility to thrombogenesis, inflammation, fibrosis, oxidation, and atherosclerosis. In giant aneurysms due to Kawasaki disease, thrombogenesis is the biggest problem, because thrombi may be formed readily in giant aneurysms where accelerated platelet aggregation, hypercoagulation and hypofibrinolysis are present. However, some aneurysms with an internal diameter of >8 mm have normal blood flow waveform, APV and CFR. Because giant aneurysms with normal hemodynamics may be present, functional assessment of aneurysms should be made to identify aneurysms at risk.
b. Hemodynamics in Vessels Distal to an Aneurysm
Blood flow waveform, APV, CFR and peripheral vascular resistance in vessels distal to an aneurysm are similar to those in the aneurysm. Shear stress is higher in the distal area than in the aneurysms with a significantly large luminal diameter.
On the other hand, FFRmyo in the distal area is within the normal range regardless of the size and shape of aneurysm, unless significant stenoses are present. These findings suggests that vascular endothelial dysfunction, myocardial ischemia and coronary microcirculation disorder due to decreased perfusion may be present in the area distal to a giant coronary aneurysm even when significant stenosis is not present.
3.2.2 Hemodynamics in the Area Distal to a Stenotic LesionIn the region distal to a coronary stenosis causing myocardial ischemia, CFR, FFRmyo, shear stress, and peripheral vascular resistance are significantly different from those in the control segment, and results outside the reference range are obtained in many of these items.57 The volume of blood perfusing in this region is small, which suggests the presence of endothelial dysfunction and myocardial ischemia. Perfusion pressure is also low, but peripheral vascular resistance is rather high as the effect of decreased blood perfusion volume is larger than that of decreased perfusion pressure in this region.
a. Markers of Myocardial Cytoplasm
i. CK, CK-MB
Creatine kinase (CK) and CK-myocardial band (MB) levels increase in 4~6 hours after the onset of myocardial infarction and decrease to normal levels in 2~3 days. The CK and CK-MB levels correlate well with the volume of myocardial necrosis. CK-MB is also a useful indicator of myocardial reperfusion and reinfarction.58 Increases in CK-MB2 and MB2/MB1 ratio may be detected within 4 hours after the onset of myocardial infarction.59
| Marker | Strengths | Weaknesses | Clinical use |
|---|---|---|---|
| CK-MB | - Rapid and accurate test - Reinfarction can be detected promptly |
- Low myocardial specificity (specificity for AMI is low in patients with musculoskeletal disorder) - Low detection rate within 6 hours after onset |
- CK-MB is one of the principle biochemical markers, and can be used as a standard test in almost all institutions |
| Myoglobin | - Detectable 1∼2 hours immediately a fter onset - Highly sensitive - Reperfusion can be detected |
- Poor myocardial specificity - Because the level returns to normal in 1∼2 days after onset, it cannot be detected in patients who present late after AMI |
- Due to poor myocardial specificity, AMI cannot be diagnosed with myoglobin alone |
| H-FABP | - Detectable 1∼2 hours immediately after onset - Infarct size can be estimated - Reperfusion can be detected |
- Rapid test kits are available. It is highly sensitive during the early diagnosis, but its specificity is relatively low |
- Rapid test kits are available throughout Japan and useful in early diagnosis |
| TnT | - Highly sensitive and highly specific - Diagnosis is possible 8∼12 hours a fter onset - Diagnosis is possible when testing is performed in the first 2 weeks after onset - Prompt diagnosis is possible with rapid test kits - Reperfusion can be detected |
- Sensitivity is low within 6 hours after onset (Retest 8∼12 hours after onset) - Sensitivity to late-onset small reinfarction is low |
- Rapid test kits are available throughout Japan, and TnT is a principle biochemical marker |
| MLC | - Detectable 4∼6 hours after onset - Diagnosis is possible when testing in the first 2 weeks after onset |
- Sensitivity is relatively low - MLC is excreted renally and may be abnormal in patients with renal failure |
- Rapid diagnostic tests are not available |
CK-MB, creatine kinase-myocardial band; H-FABP, heart-type fatty acid-binding protein; MLC, myosin light chain; TnT, troponin T.
ii. Myoglobin
Myoglobin levels increase in 1~2 hours after the onset of myocardial infarction, reach their peak in about 10 hours, and decrease to a normal level in 1~2 days. Myoglobin is useful in early diagnosis of myocardial infarction, and is also a good indicator of reperfusion.58 However, it is not specific to myocardium.
iii. Heart-Type Fatty Acid-Binding Protein
Heart-type fatty acid-binding protein (H-FABP) increases in 1~2 hours after the onset of myocardial injury, and is useful in early diagnosis of myocardial infarction, estimating infarct size, and detecting reperfusion.58 The cut-off level for the diagnosis of myocardial infarction is 6.2 ng/mL.60
b. Markers of Myocardial Structural Proteins
i. Myocardial Troponin T and I
Myocardial troponin T and I (TnT and TnI) are specific to myocardium, and reach peak levels at 12~18 hours and 90~120 hours after the onset of myocardial infarction. These may be used as markers of reperfusion. TnT is highly sensitive and specific in detecting the onset of myocardial infarction, and is useful in the diagnosis and prognosis assessment of non-ST elevation myocardial infarction.58,61 In whole-blood rapid assay for TnT, a positive test is defined as ≥0.10 ng/mL.62 When a negative result is obtained within 6 hours after the onset of symptoms, the test should be repeated 8~12 hours after onset.
ii. Myosin Light Chain
The plasma myosin light chain (MLC) level reflects the process of myofibrillar necrosis. MLC is detected in blood in 4~6 hours after the onset of myocardial infarction, reaches a peak level in 2~5 days, and maintains high levels for 7~14 days. MLC1 and MLC2 tests are available, but only the MLC1 test is covered with the national health insurance in Japan. The cut-off level for acute myocardial infarction (AMI) is 2.5 ng/mL. The peak MLC1 level reflects infarct size, and a result of ≥20 ng/mL is defined as major infarction.63
The above-described features of individual markers indicate that myoglobin and H-FABP are useful in detecting early-phase myocardial infarction, and CK-MB and TnT are beneficial in diagnosing myocardial infarction ≥6 hours after onset. Primary markers for AMI are CK-MB and TnT (Table 6).
c. Inflammatory Proteins
i. High-Sensitive CRP
High-sensitive CRP is used as an indicator of the presence of coronary arteriosclerotic lesions,64 and it has been reported that elevation of high-sensitive CRP is observed in some patients with late-onset coronary sequelae in Kawasaki disease such as coronary artery lesions and myocardial injury.65,66 Elevation of high-sensitive CRP has been reported among patients without coronary sequelae after an average of 8 years after the onset of Kawasaki disease, suggesting that low-grade inflammation continues after healing of Kawasaki disease.67
ii. Serum Amyloid A Protein
It has been reported that serum amyloid A protein increases during the acute phase of Kawasaki disease. It has been reported that the serum amyloid A protein level remains high even during the remote phase, which suggests the presence of continued inflammation.65
1.1.2 ArteriosclerosisA diagnosis of arteriosclerosis should be made after the presence of dyslipidemia and insulin resistance is confirmed. It has been reported that coronary arteriosclerosis as part of metabolic syndrome may develop even during childhood.68 Researchers are now investigating whether a history of Kawasaki disease and/or coronary artery lesions is a risk factor for the development of arteriosclerosis in children.
i. Total Cholesterol
In adults, a total cholesterol (TC) level of <200 mg/dL is normal, 200~219 mg/dL is borderline, and ≥220 mg/dL is abnormal.70
| Total cholesterol | Normal: <190 mg/dL |
| Borderline: 190∼219 mg/dL | |
| Abnormal: ≥220 mg/dL | |
| LDL cholesterol | Normal: <110 mg/dL |
| Borderline: 110∼139 mg/dL | |
| Abnormal: ≥140 mg/dL | |
| HDL cholesterol | Cut-off value: 40 mg/dL |
| Triglycerides | Cut-off value: 140 mg/dL |
HDL, high density lipoprotein; LDL, low density lipoprotein. Source: Okada T, et al. Pediatr Int 2002; 44: 596–601.69
ii. Serum Low Density Lipoprotein Cholesterol
In adults a serum low density lipoprotein cholesterol (LDL-C) level of <120 mg/dL is normal, 120~139 mg/dL is borderline, and ≥140 mg/dL is abnormal.70
iii. Serum High Density Lipoprotein Cholesterol
High density lipoprotein cholesterol (HDL-C) prevents arteriosclerosis, and low serum HDL-C levels represent a high risk of arteriosclerosis. In adults, a serum HDL-C level of ≥40 mg/dL is normal, and <40 mg/dL is defined as hypo HDL cholesterolemia.71 Low serum HDL-C levels associated with Kawasaki disease are observed not only during the acute phase, but also among patients with coronary artery lesions in the remote phase.72
iv. Serum Triglycerides
It is known that hypertriglyceridemia promotes the progression of arteriosclerosis. In adults, a serum triglyceride (TG) level of ≥150 mg/dL is defined as hypertriglyceridemia.70
b. Homocysteine
Hyperhomocysteinemia is an independent risk factor for arteriosclerotic disorders such as cerebral infarction and myocardial infarction.73 The reference value of plasma homocysteine level is 8.2~16.9 μmol/L in men and 6.4~12.2 μmol/L in women. Plasma homocysteine levels in women increase after menopause.74
c. Criteria for Diagnosis of Metabolic Syndrome in Children
Table 8 shows the criteria for diagnosis of metabolic syndrome in children in Japan.75
| Children meeting (1) and at least 2 of items (2)~(4) should be diagnosed with metabolic syndrome. |
| (1) Abdominal girth ≥80 cm* |
| (2) Serum lipid |
| Triglyceride ≥120 mg/dL and/or HDL cholesterol <40 mg/dL |
| (3) Blood pressure |
| Systolic pressure ≥125 mmHg and/or diastolic pressure ≥70 mmHg |
| (4) Fasting blood glucose ≥100 mg/dL |
*: Children with an waist-to-height ratio of ≥0.5 fulfill item (1). In elementary school children (6∼12 years of age), those with an abdominal girth of ≥75 cm should be considered to fulfill item (1).
HDL, high density lipoprotein.
Adapted from Ohzeki T, et al. A cohort study to establish the concept, pathophysiology, and diagnostic criteria of metabolic syndrome in children and design effective interventions: A final report in 2005–2007. 2008: 89–91.75
d. Children in the Remote Phase of Kawasaki Disease
It has been reported that TC and apolipoprotein B levels are higher in individuals who had Kawasaki disease 7~20 years ago than the control group. Children in the remote phase of Kawasaki disease should be observed carefully for the progression of arteriosclerosis.71
e. Adults in the Remote Phase of Kawasaki Disease
Table 9 shows the reference values for markers of dyslipidemia in Japanese adults.70 Adults with a history of Kawasaki disease should be instructed to maintain a healthy lifestyle to keep lipid levels within normal ranges.71
| Hypercholesterolemia | Total cholesterol | ≥220 mg/dL |
| Hyper LDL cholesterolemia | LDL cholesterol | ≥140 mg/dL |
| Hypo HDL cholesterolemia | HDL cholesterol | <40 mg/dL |
| Hypertriglyceridemia | Triglyceride | ≥150 mg/dL |
HDL, high density lipoprotein; LDL, low density lipoprotein.
Adapted from Japan Atherosclerosis Society (JAS) Guidelines for Diagnosis and Treatment of Atherosclerotic Cardiovascular Diseases, 2002. 2002: 5–7.70
According to “Diagnostic Guidelines of Kawasaki Disease (MCLS: Infantile Acute Febrile Mucocutaneous Lymph Node Syndrome)” (See Table 3), during the acute phase of Kawasaki disease, the electrocardiography (ECG) may show prolonged PR interval, deep Q waves, prolonged QT interval, low voltage, ST-T changes, arrhythmias, and among other findings suggestive of myocardial injury and abnormal repolarization.5,76 ECG should be monitored continuously for these changes.77
It has been reported that QT interval during the acute phase does not clearly correlate with the development of coronary artery lesions;78 the suggestion that there are relationships between T waveforms and the presence of myocarditis, coronary arteritis, and left ventricular wall movement;79 and the suggestion that there is a relationship between QT dispersion and coronary artery lesions.80–82 Premature ventricular contractions (PVCs) are often observed, and the incidence of PVCs does not differ between patients with and without coronary artery lesions unless coronary stenosis or occlusion is present.83 When myocardial infarction occurs in patients with giant aneurysms, ST-T changes and abnormal Q waves that are consistent with the lesion of infarction are observed.84
2.2 Holter ECGHolter ECG recording is worthwhile in patients complaining of chest pain, chest discomfort, and/or palpitations. Patients with stenosis or giant aneurysms should undergo Holter ECG recording at least once even though it has been reported that the risk of serious arrhythmia and ischemic changes during remote phase is low among those with normal coronary arteries and those who experienced transient coronary artery lesions during the acute phase.83
2.3 Stress ECG 2.3.1 Exercise ECGa. Double or Triple Master’s Two-Step Test
Although benefits of exercise ECG have been reported, it cannot detect abnormal findings in patients without severe ischemia.
b. Treadmill Test and Ergometer Stress Test
Treadmill test and ergometer stress test can be administered to school-age or older children, though their sensitivity in detecting ischemic findings is less than that of myocardial scintigraphy. It has therefore been recommended that pharmacological stress be added to increase the rate of detection, or that signal-averaged ECG be used.
Treadmill test and ergometer stress test may detect coronary stenosis in some patients. A decrease in coronary reserve due to coronary microcirculation disorder is suspected in patients who have no detectable coronary stenosis but show ST depression during exercise ECG and those with perfusion defect in myocardial scintigraphy.85
2.3.2 Pharmacological Stress Test and Body Surface Potential MappingIt has been reported that dipyridamole stress tests using body surface potential mapping is highly sensitive and specific to the presence of ischemia, and is a useful method in diagnosing myocardial ischemia in patients including young children.86 Also, dobutamine stress test using body surface potential mapping is superior to treadmill test in terms of the sensitivity and specificity for myocardial ischemia, and is reported useful in children.87,88 Although magnetocardiography may detect myocardial ischemia,89 this is available only in a limited number of institutions.
2.3.3 Electrophysiological TestsLife-threatening ventricular arrhythmias may develop in a small number of patients with a history of Kawasaki disease. Studies of patients with cardiovascular sequelae in Kawasaki disease who underwent electrophysiological evaluation90 have revealed that the prevalence of abnormal sinus or atrioventricular nodal function is significantly higher in patients with cardiac sequelae than in those without them, although the findings of abnormal nodal function were not consistent with the presence of coronary stenosis/occlusion, and are believed to result from myocarditis or abnormal microcirculation in the conducting system.
2.4 Signal-Averaged ECGDuring the acute phase, filtered QRS duration changes by ≥10%.91 It has been reported that myocardial depolarization becomes inhomogeneous but this change is reversible.92 It also has been reported that RMS40 during remote phase is significantly lower in patients with coronary artery lesions than without them, and RMS40 is useful as a predictor of ventricular arrhythmias.93 Signal-averaged ECG is considered highly sensitive for myocarditis due to Kawasaki disease in any phase.94 Patients with coronary dilatation with and without stenosis during the acute phase contain a larger proportion of high frequency components, suggesting the presence of myocardial involvement.95 The presence of late ventricular potentials evaluated by criteria with an adjustment to body surface area is highly specific for ischemia and previous myocardial infarction.96 Dobutamine stress test may improve the detection of these findings in children who cannot undergo exercise stress test.97
2.5 Summary of Physiological ExaminationsTable 10 summarizes the physiological examinations commonly used for patients with Kawasaki disease and their rates of detection of cardiac complications.81,84,87,96,97
| Investigators | Examination | Target disease | Criteria | N | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| Osada M, et al81 | QT dispersion | Coronary artery lesions | QT ≥60 ms | 56 | 100% (6/6) | 92% |
| Nakanishi T, et al84 | 12-lead ECG | Inferior wall infarction | Deep Q in II, III, aVF | 7 | 86% | 97% |
| Anterior wall infarction | Deep wide Q in V1∼6 | 8 | 75% | 99% | ||
| Lateral wall infarction | Deep Q in I, aVL | 7 | 57% | 100% | ||
| Ogawa S, et al96 | Signal-averaged ECG | Myocardial ischemia | LP positive | 198 | 69.2% | 93.5% |
| Genma Y, et al97 | Dobutamine stress signal-averaged ECG |
Myocardial ischemia | LP positive | 85 | 87.5% | 94.2% |
| Takechi N, et al87 | Dobutamine stress body surface potential mapping |
Myocardial ischemia | nST >1 | 115 | 94.1% | 98.9% |
| I map ≤4 | 115 | 41.7% | 96.9% |
ECG, electrocardiography; I map, isopotential map; LP, late potential; nST, non-stress test.
Because ECG at rest is not sensitive in detecting ischemic lesions in patients in the remote phase of Kawasaki disease, exercise or pharmacological stress tests should be used. Imaging should also be performed to assess ischemic lesions more accurately. Holter ECG and signal-averaged ECG should be performed to assess for ventricular arrhythmia even in patients without ischemic lesions.
3. Diagnostic Imaging 3.1 Chest X-Ray 3.1.1 X-Ray Finding of Calcified Coronary AneurysmsPathological investigation has revealed that calcification of aneurysms occurs on day 40 after onset or later,98 but becomes detectable with a chest X-ray 1~6 years after onset.99 Observation should be made with frontal and lateral projections.
3.1.2 Cardiac Dysfunction Due to Previous Myocardial Infarction and Enlarged Heart Shadow Due to Valvular DiseasesAn enlarged heart shadow is observed in patients with cardiac dysfunction due to previous myocardial infarction, and in patients with volume overload caused by mitral or aortic insufficiency.
3.2 Echocardiography 3.2.1 Echocardiography at RestA technique proposed by Fuse et al. has been used to perform coronary echocardiography and determine the intimal diameter of coronary arteries in children.100 This technique is useful to follow up coronary dilatation101,102 and thrombi in coronary aneurysms.103 Three-dimensional (3D) echocardiography is useful in visualizing the right coronary artery and the circumflex artery, and in visualizing mural thrombi in coronary aneurysms.104 Echocardiography is the most useful method for evaluation of deterioration of cardiac function due to myocardial injury and the severity of valvular disease.105 Detailed reports have been published on evaluation of myocardial injury during the acute phase using tissue Doppler imaging.106
3.2.2 Stress EchocardiographyStress echocardiography, especially dobutamine stress echocardiography, has been established as a diagnostic method for ischemic heart diseases.107 It is also a useful noninvasive method to diagnose and follow up myocardial ischemia due to Kawasaki disease.
3.2.3 Myocardial Contrast EchocardiographyThe ability of myocardial contrast echocardiography has increased to the level comparable to that of myocardial scintigraphy due to the development and advancement of intravenous contrast agents and the advancement of echocardiography systems.108
3.3 Radionuclide ImagingIn order to ensure the lowest possible radioactive exposure to children, technetium (Tc)-labeled myocardial perfusion agents (e.g., Tc-99 m sestamibi, and Tc-99 m tetrofosmin) are commonly used.109,110 Stress myocardial single photon emission computed tomography (SPECT) is an important method of diagnosis for coronary stenotic lesions due to Kawasaki disease, and pharmacological stress SPECT is commonly performed for children who cannot undergo exercise stress SPECT.111–116 When myocardial ischemia is detected in patients without coronary stenoses and there is a false positive result of myocardial perfusion imaging, the presence of coronary microcirculation disorder is suspected.85 The availability of 3D automatic quantitative analysis of ECG-gated myocardial perfusion SPECT (quantitative gated SPECT, QGS)117 has allowed physicians to assess for post-ischemic myocardial stunning118 and the viability of infarcted myocardium in patients with severe coronary artery lesions due to Kawasaki disease.119,120
3.3.1 Tc-Labeled Myocardial Perfusion ScintigraphyTc-labeled myocardial perfusion scintigraphy is performed under stress at a dose of 10 MBq/kg (maximum 370 MBq, 10 mCi), and the second dose is administered 2~3 hours after the first administration at 2~3 times the first dose (maximum 740 MBq, 20 mCi).121 To obtain clear images, physicians should (1) exercise special caution in avoiding body movement by children during imaging and repeating the imaging when excessive body movement occurs, (2) continue the maximum stress for at least one minute after administration of perfusion agents under stress, (3) promote elimination of perfusion agents from the liver by eating egg products or cocoa, or obtaining images at least 30 minutes after administration of perfusion agents; (4) have the patient maintain the Monzen position (raising the left arm) throughout the procedure to reduce the influence of scattered rays from the liver to the heart;122 and (5) give the patient soda immediately before the imaging to expand the stomach and reduce the influence of scattered rays from the intestine.
3.3.2 Pharmacological Stress Myocardial Perfusion ScintigraphyFigure 3 illustrates the outline of pharmacological stress myocardial perfusion scintigraphy.112,116,123 In Japan, adenosine has been approved as a nuclear medicine agent, and it is expected that pharmacological stress myocardial perfusion scintigraphy using adenosine will be a common imaging method. Adenosine should not be administered with dipyridamole, which potentiates the action of adenosine. Adenosine may induce asthmatic attacks, but the half-life of adenosine is short and most of the adverse reactions disappear after discontinuation of the drug.124

Administration of drugs during myocardial perfusion scintigraphy. ATP, adenosine triphosphate; iv, intravenous.
The Guidelines for Drug Therapy in Pediatric Patients with Cardiovascular Diseases proposed by the Japanese Circulation Society recommend that the dose of nuclear medicine agents for children should be calculated using a formula of “[adult dose]×(years of age+1)/(years of age+7)”,125,126 while the Committee on Appropriate Use of Nuclear Medicine in Children of the Japanese Society of Nuclear Medicine recommends to determine appropriate doses of agents on the basis of the “dosage card” proposed by the European Association of Nuclear Medicine.127,128
3.4 Coronary CT and MRCA 3.4.1 Contrast Coronary CT Angiography (MDCT)Although usefulness of multi-detector row computed tomography (MDCT) in patients with Kawasaki disease has been reported,129 it has drawbacks such as extensive radiation exposure, use of contrast media, and use of β-blockers to control heart rate. However, these drawbacks are being overcome with measures such as decreasing radiation dose to 80 kV in infants and young children, and administering contrast media at low or intermediate doses.130
MDCT has a limitation for visualizing the coronary lumen in segments with calcification, because calcifications cause partial volume effects.131 It has been reported that the detection rate of stenotic lesions is higher in MDCT than in magnetic resonance coronary angiography (MRCA).132,133 MDCT is superior to MRCA in terms of spatial resolution, image quality, imaging time, and ease of operation. Also, MDCT is useful in visualizing collateral flows that are characteristics to Kawasaki disease.
3.4.2 MRCAMRCA can be repeatedly performed from the acute phase of Kawasaki disease, because this imaging technique requires neither X-ray exposure nor contrast media, and is useful in screening for mild coronary artery lesions and intimal hyperplasia.134 Because MRCA can be performed during spontaneous breathing without controlling of the heart rate, infants and young children may undergo it during sleep.135 There are two imaging techniques of MRCA, the bright blood technique [steady-state free precession (SSFP)] which indicates blood flow as white, and the black blood technique,136,137 which indicates blood flow as black and occlusions and intimal hyperplasia as gray. MRCA is superior to MDCT as a method to observe thrombi and intimal hyperplasia. Technical expertise is needed to obtain accurate images, and it takes considerable time to create coronary images from data.
3.4.3 Magnetic Resonance Myocardial ImagingCine magnetic resonance imaging (MRI) is performed using SSFP without contrast media to acquire images from the left ventricular short axis view, long axis view, and four-chamber view to observe ventricular wall motion, and perfusion MRI is performed after infusion of gadolinium-based contrast media to evaluate the severity of myocardial ischemia by observing the first pass of contrast media in the myocardium during ATP stress and at rest from the left ventricular short axis view.138
Delayed-contrast enhanced MRI can visualize the extent and depth of subendocardial infarct lesions by obtaining images 15 minutes after the administration of contrast media with a sequence using T1-weighted gradient echo with myocardial T1 signal suppression. This technique can visualize subendocardial infarct lesions and small infarct lesions in the right ventricle. Because the prevalences of occlusions and recanalization of the right coronary artery are especially high in patients with Kawasaki disease, precise evaluation of the right ventricular myocardium is important.139
4. Cardiac Catheterization 4.1 CAG 4.1.1 Indicationsa. Evaluation of Severity of Coronary Artery Lesions and Patient Follow-up
Although in the case of adults CAG is indicated for those who exhibit findings of myocardial ischemia, it is recommended for patients with Kawasaki disease that CAG should be performed in those with medium or giant aneurysms during the convalescent phase or later to monitor for the development or progression of localized stenosis, because myocardial ischemia due to Kawasaki disease cannot be fully detected with other types of examinations and myocardial ischemia may manifest as sudden death.140,141 The severity classification of cardiovascular lesions due to Kawasaki disease (Table 4) is based on the findings of CAG.
b. CAG Before and After PCI
CAG is required before percutaneous coronary intervention (PCI) to determine whether PCI is indicated, during angioplasty to ensure safe and effective intervention, and after angioplasty to evaluate the results of PCI and follow up patients.113,142,143
c. Intracoronary Thrombolysis
Thrombi in coronary aneurysms may sometimes be observed during follow-up of medium to giant aneurysms with echocardiography. In such cases, cardiac catheterization and CAG are performed for intracoronary thrombolysis (ICT).
4.1.2 Coronary Artery Lesions Indicated for CAGa. Dilatation Lesions
The severity classification of cardiovascular lesions due to Kawasaki disease (Table 4), aneurysms with an internal diameter of ≤4 mm are defined as small aneurysms, those with from >4 mm to <8 mm as medium aneurysms, and those with ≥8 mm as giant aneurysms. In patients with aneurysms classified as medium or giant, it is desirable to perform CAG during the early part of the convalescent phase for detailed evaluation of the morphology and extent of coronary artery lesions and to specify the methods and duration of follow-up and treatment strategies. Because serious localized stenoses may develop in patients with giant aneurysms in whom examinations have not detected any findings of myocardial ischemia, such patients should undergo CAG every few years.141,144 However, as precise evaluation of coronary stenotic lesions is feasible with MRCA and MDCT, it is expected that in the future it will be possible to omit catheterization for the diagnosis of coronary stenotic lesions in some patients.135,145
Because the development of stenosis after regression of not only large aneurysms but also smaller ones146 and the development of arteriosclerotic degeneration38,147 have been observed in patients over 10 years after the onset of Kawasaki disease, patients should be followed for a long period of time using coronary imaging techniques such as MRCA and MDCT if follow-up CAG is not feasible.
b. Localized Stenosis
During the remote phase, progressive localized stenosis develop mainly in the inlet and outlet of aneurysms. Multi-directional imaging is required to evaluate stenotic lesions. A significant stenosis is defined as a ≥75% stenosis in lumen diameter in the major coronary arteries and a ≥50% stenosis in lumen diameter in the left main coronary trunk. Patients with significant stenosis should be followed with angiography141,148 or other imaging techniques such as MRCA,135 MDCT129,145 at appropriate intervals based on the speed of progression of the stenosis (from 6 months to several years), even when no signs/symptoms of myocardial ischemia are present, and should be considered for aggressive treatment such as CABG149 and PCI113 based on the results of the above-described follow-up imaging as well as the results of other studies such as myocardial scintigraphy,150 exercise ECG, and evaluation of CFR.
c. Occlusion
Complete occlusion of a coronary artery is observed in about 16% of patients with coronary artery lesions, and 78% of occlusions are visualized with imaging within 2 years after the onset of Kawasaki disease.141 It is not uncommon to find coronary occlusive lesions in asymptomatic patients for the first time on routine follow-up imaging. Collateral flows are visualized during angiography in all patients with coronary occlusion. The presence of a well-developed collateral circulation, for which the patient often shows no ischemic findings, is a characteristic feature of occlusive lesions due to Kawasaki disease. Because the extent of collateral flow and growth/development of recanalized vessels differ among individuals and depend on the time after occlusion and cause of occlusion (thrombi vs. intimal hyperplasia), follow-up angiography is required.151
4.2 Cardiac Function TestCardiac function is evaluated by determining ventricular pressure, cardiac output, ventricular volume, ejection fraction (EF), and/or other parameters.
4.3 Intravascular Ultrasound 4.3.1 Morphological Evaluation of Coronary Artery LesionsIntravascular ultrasound (IVUS) is used to evaluate the severity of intimal hyperplasia, presence/absence of thrombi or calcification, and the severity of luminal narrowing. Severe intimal hyperplasia is observed not only in lesions of localized stenosis but also in aneurysms that have regressed. Intimal narrowing and calcification not detected with angiography may be visualized with IVUS. It has been found that obvious intimal hyperplasia may develop during the remote phase in aneurysms with an internal diameter during the acute phase of >4 mm.25 Evaluation of lesions, and especially quantitative evaluation of calcified lesions with IVUS, is required when the means to be used for PCI are selected.143,152,153
4.3.2 Coronary Arterial Vasodilator FunctionIt has been reported that the absence of coronary vasodilatation in the coronary artery wall following administration of isosorbide dinitrate (ISDN) or acetylcholine suggests the presence of chronic intimal dysfunction in patients with Kawasaki disease.37,147,148 However, because evaluation of coronary arterial vasodilator function may induce coronary spasm or other adverse reactions, its potential benefits and risks should be carefully weighed before it is performed.
5. Summary of Examinations and Diagnosis (Table 11)Patients with Class III~V severity of coronary artery lesions should undergo examinations listed in Table 11 periodically to follow these lesions over time. As the most clinically significant cardiovascular sequelae in Kawasaki disease include coronary stenosis, thrombogenesis in coronary aneurysms, myocardial ischemia, myocardial infarction, vascular endothelial dysfunction, and early progression of arteriosclerosis, and these lesions may develop and progress over time in a considerable number of asymptomatic patients, patients should be followed and evaluated periodically. Recently, MRCA and MDCT have become commonly used as noninvasive methods to delineate coronary artery lesions accurately, and are expected to reduce the mental and physical burden on patients by minimizing the use of invasive catheterization. When these examinations reveal that the lesions have progressed to the point that they require interventions such as PCI and CABG, coronary hemodynamics should also be assessed using stress myocardial perfusion imaging and cardiac catheterization using Doppler flow wire and pressure wire to select appropriate treatment methods.
| Blood Test (biomarkers for myocardial ischemia, myocardial infarction, and arteriosclerosis) | |
| Severity classification IV, V | Class I |
| Severity classification I, II, III | Class II |
| None | Class III |
| Echocardiography at rest, 12-lead ECG | |
| Severity classification I, II, III, IV, V | Class I |
| None | Class II |
| None | Class III |
| Exercise ECG | |
| Severity classification III, IV, V | Class I |
| Severity classification I, II | Class II |
| None | Class III |
| Chest X-ray | |
| Severity classification III, IV, V | Class I |
| Severity classification I, II | Class II |
| None | Class III |
| Holter ECG, signal-averaged ECG | |
| Severity classification IV, V | Class I |
| Severity classification I, II, III | Class II |
| None | Class III |
| Body surface mapping, pharmacological stress ECG, magnetocardiography | |
| Severity classification IV, V | Class I |
| Severity classification I, II, III | Class II |
| None | Class III |
| Stress echocardiography, myocardial contrast echocardiography | |
| Severity classification IV, V | Class I |
| Severity classification I, II, III | Class II |
| None | Class III |
| MRCA, MDCT | |
| Severity classification IV, V | Class I |
| Severity classification I, II, III | Class II |
| None | Class III |
| Myocardial perfusion imaging, stress myocardial perfusion imaging | |
| Severity classification IV, V | Class I |
| Severity classification I, II, III | Class II |
| None | Class III |
| Cardiac catheterization | |
| Severity classification IV, V | Class I |
| Severity classification III | Class II |
| Severity classification I, II | Class III |
ECG, electrocardiography; MDCT, multi-detector row computed tomography; MRCA, magnetic resonance coronary angiography.
In assessment of cases of death during the remote phase in patients with coronary artery lesions, the major cause of death has been found to be ischemic heart disease due to stenotic lesions resulting from coronary intimal hyperplasia or thrombotic occlusion.40,154
In general, treatment of myocardial ischemia is performed to:
- Increase coronary blood flow
- Prevent or relieve coronary spasm
- Prevent the formation of thrombi
- Decrease cardiac work
- Protect myocardium
- Prevent the remodeling of vessel walls
The main purpose of treatment is to decrease the frequency and severity of chest pain attacks, prevent cardiac accidents, and improve the quality of life (QOL) of patients.155 Drugs used for this purpose include antiplatelet drugs, anticoagulant drugs, calcium channel blockers, nitrates, β-blockers, angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs) and statins (Table 12).
| Patients without anginal symptoms |
| - Patients without demonstrated ischemia: antiplatelet drugs |
| - Patients with demonstrated ischemia: antiplatelet drugs+calcium channel blockers |
| Patients with anginal symptoms |
| In addition to antiplatelet drugs; |
| - Patients with angina of effort: nitrates and/or calcium channel blockers. If treatment is ineffective, add β blockers |
| - Patients with angina at rest or during sleep: calcium channel blockers |
| - Patients with angina at night: calcium channel blockers+nitrates, or +K-channel openers (nicorandil) |
| Patients with cardiac dysfunction and those with valvular disease |
| - Assess the severity of cardiac dysfunction, and use β-blockers, ACE inhibitors, ARBs and/or statins in addition to antianginal drugs |
ACE, angiotensin converting enzyme; ARB, angiotensin II receptor blocker.
It has been reported that treatment with the ARB candesartan at a dose of 0.2~0.3 mg/kg/day starting within a few days after detecting a coronary aneurysm was effective in preventing stenosis due to intimal hyperproliferation.156 A recent study has reported that ARBs activate NAD(P)H oxidase, inhibit the expression of monocyte chemoattractant protein-1 (MCP-1) and intercellular adhesion molecule 1 (ICAM-1), and inhibit atherosclerotic changes.157 It has also been reported that ARBs exert more potent antiatherosclerotic effects when used with statins. These findings suggest that ARBs may also be effective in preventing arteriosclerosis during the remote phase.
1.3 Antiplatelet Drugs and Anticoagulant Drugs 1.3.1 Antiplatelet Drugs (Table 13)Platelet count decreases slightly immediately after the onset of Kawasaki disease (acute phase), and increases during the convalescent phase. Since platelet aggregation activity remains high during the first 3 months after onset and in some cases the first several months to 1 year after onset, it is preferable that patients with Kawasaki disease, including those without coronary sequelae, should be treated with antiplatelet drugs at low doses for about 3 months.158–160
| Drug | Dose | Adverse drug reactions (ADRs) and precautions |
|---|---|---|
| Acetylsalicylic acid (Bufferin® or Bayaspirin®) |
- 30∼50 mg/kg/day, divided into 3 doses during the acute phase - 3∼5 mg/kg/day, once daily after defervescence |
- Hepatic dysfunction, gastrointestinal ulcer, Reye syndrome (higher incidence at ≥40 mg/kg/day), bronchial asthma. - Use other drugs during varicella infection and influenza. |
| Flurbiprofen (Froben®) |
- 3∼5 mg/kg/day, divided into 3 doses | - Hepatic dysfunction, gastrointestinal ulcer. - Use when severe hepatic disorder due to aspirin develops. |
| Dipyridamole (Persantin®, Anginal®) |
- 2∼5 mg/kg/day, divided into 3 doses | - Coronary steal phenomenon, headache, dizziness, thrombocytopenia, hypersensitivity, dyspepsia. - May induce angina in patients with severe coronary stenosis. |
| Ticlopidine (Panaldine®) |
- 5∼7 mg/kg/day, divided into 2 doses | - Thrombotic thrombocytopenic purpura (TTP), leucopenia (granulocytopenia), serious hepatic dysfunction. - Blood tests must be performed every other week during the first 2 months of treatment. |
| Clopidogrel (Plavix®) |
- 1 mg/kg/day, once daily | - TTP, gastrointestinal symptoms, malaise, myalgia, headache, rash, purpura, pruritus. - Bleeding tendency may develop when used with aspirin. |
| Unfractionated heparin (iv) Low-molecular- weight heparin (sc) |
- Loading dose 50 units/kg, maintenance dose 20 units/kg to maintain an APTT of 60∼85 sec (1.5∼2.5 times baseline) - Infants <12 months of age Treatment: 3 mg/kg/day, divided into 2 doses (every 12 hours) Prevention: 1.5 mg/kg/day, as above - Children/adolescents Treatment: 2 mg/kg/day, divided into 2 doses (every 12 hours) Prevention: 1 mg/kg/day, as above |
- Major ADRs: Shock/anaphylactoid reaction, bleeding, thrombocytopenia, thrombocytopenia/thrombosis associated with heparin-induced thrombocytopenia. |
| Warfarin (Warfarin®) |
- 0.05∼0.12 mg/kg/day, once daily (0.05∼0.34 mg/kg/day in the AHA guidelines) - 3∼7 days required to obtain efficacy |
- Dose should be adjusted to an INR of 2.0∼2.5 and a thrombotest value of 10∼25%. - Sensitivity to this drug, hepatic dysfunction, and bleeding ADRs are possible. - The effect of warfarin may be reduced by barbiturates, steroids, rifampicin, bosentan hydrate, and vitamin K-rich foods such as natto, spinach, green vegetables, chlorella, and green juices. The effect of warfarin may be increased by chloral hydrate, NSAIDs, amiodarone, statins, clopidogrel, ticlopidine, antitumor drugs, antibiotics, and antifungal drugs. |
The safety and efficacy of the above drugs have not been established in children.
AHA, American Heart Association; APTT, activated partial thromboplastin time; INR, international normalized ratio; iv, intravenous; NSAIDs, nonsteroidal antiinflammatory drugs; sc, subcutaneous.
On the other hand, patients with coronary aneurysm due to Kawasaki disease should receive antiplatelet drugs continuously to prevent ischemic heart disease and prevent the formation or growth of thrombi by platelet activation. This antiplatelet therapy may decrease the incidence of angina and myocardial infarction. Patients who develop AMI should continue treatment with antiplatelet drugs at low doses in combination with anticoagulant drugs from shortly after the onset of infarction until the infarct has healed.
a. Dosage and Administration
It is recommended that children should receive aspirin, a drug inhibiting secondary platelet aggregation, at a low dose (3~5 mg/kg/day, once daily). As aspirin inhibits the production of prostacyclin (PGI2), a combination of aspirin with other antiplatelet drugs at low doses may be considered for children. Dipyridamole (2~5 mg/kg/day, divided into 3 doses) is expected to potentiate the effect of aspirin, but monotherapy of dipyridamole is not recommended. Ticlopidine is usually administered at a dose of 5~7 mg/kg/day, divided into 2 doses, and requires careful observation for major adverse reactions.
b. Adverse Drug Reactions
Aspirin may cause adverse drug reactions such as rash, bronchial asthma and hepatic dysfunction. Special care should be taken for bleeding complications. The use of aspirin should be avoided during epidemic of influenza or varicella as aspirin may cause Reye syndrome. Major adverse reactions to ticlopidine include agranulocytosis, serious hepatic dysfunction, and thrombotic thrombocytopenic purpura.
1.3.2 Anticoagulant Drugs (Table 13)Treatment with anticoagulant drugs in patients with Kawasaki disease should be limited for those with medium or giant aneurysms, those with a history of AMI, and those with abrupt dilatation of a coronary artery associated with a thrombus-like echo, among other special cases. Warfarin is often used for these patients. Intravenous heparin should be used in combination with warfarin in emergency cases, and warfarin is used for long-term anticoagulation in patients with chronic conditions. Patients with giant aneurysms should receive a combination of aspirin and warfarin to prevent thrombotic occlusion of aneurysms.162,163
a. Dosage and Administration
The maintenance dose of warfarin should be 0.05~0.12 mg/kg/day, once daily to achieve an international normalized ratio (INR) of 2.0~2.5, and should be adjusted carefully to prevent bleeding tendency due to excessive warfarin therapy. The recommended dose of unfractionated heparin ranges from 18 units/kg/day for older children to 28 units/kg/day for infants. The activated partial thromboplastin time (APTT) should be maintained at between 60 and 85 seconds.
b. Adverse Drug Reactions and Drug Interactions
As warfarin may cause a severe bleeding tendency, patients should be evaluated carefully for symptoms of bleeding tendency during warfarin therapy. The effects of warfarin are reduced by vitamin K, and are potentiated by aspirin, chloral hydrate, and ticlopidine among other drugs. Vitamin K-rich foods such as natto, green and yellow vegetables, and chlorella reduce the effect of warfarin significantly. Adverse drug reactions to unfractionated heparin include bleeding, hepatic dysfunction, alopecia, and rash.
1.4 Coronary Vasodilators and Antianginal Drugs (Table 14) 1.4.1 Calcium Channel BlockersIn patients with a history of Kawasaki disease, myocardial infarction may occur at rest or during sleep, which suggests the presence of coronary spasm.164,165 The addition of amlodipine, a long-acting calcium channel blocker, to the existing regimen may decrease the incidence of cardiovascular events in patients with angina or myocardial ischemia secondary to myocardial infarction. However, amlodipine should not be administered to patients with congestive heart failure and those with atrioventricular block.
| Drug | Dose | Adverse drug reactions and precautions |
|---|---|---|
| Drugs for angina | ||
| Nifedipine (Adalat®) |
- 0.2∼0.5 mg/kg/dose, TID (available as 5 and 10 mg capsules) - Adult dose: 30 mg/day, divided into 3 doses |
- Hypotension, dizziness, headache - Care is needed in patients with poor cardiac function |
| Slow-release nifedipine (Adalat-CR®, Adalat-L®) |
- 0.25∼0.5 mg/kg/day, OD or BID, maximum dose 3 mg/kg/day (Tablets of Adalat-CR® 20 mg, L® 10 mg, and L® 20 mg are available) - Adult dose: 40 mg/kg, OD (Adalat-L® should be divided into 2 doses) |
Same as above |
| Amlodipine (Norvasc®) |
- 0.1∼0.3 mg/kg/dose, OD or BID (maximum dose 0.6 mg/kg/day) (Tablets of 2.5 mg and 5 mg are available) - Adult dose: 5 mg/day, OD |
Same as above |
| Diltiazem (Herbesser®) |
- 1.5∼2 mg/kg/day, TID (maximum dose 6 mg/day) (30 mg tablets) - Adult dose: 90 mg/day divided into 3 doses |
Same as above |
| Drugs for heart failure | ||
| Metoprolol (Seloken®) |
- Start at 0.1∼0.2 mg/kg/day, divided into 3∼4 doses to titrate to 1.0 mg/kg/day (40 mg tablets) - Adult dose: 60∼120 mg/day, divided into 2∼3 doses |
- Hypotension, cardiac dysfunction, bradycardia, hypoglycemia, bronchial asthma |
| Carvedilol (Artist®) |
- Start at 0.08 mg/kg/day - Maintain at 0.46 mg/kg/day (average) - Adult dose: 10∼20 mg/day, OD |
Same as above |
| Enalapril (Renivace®) |
- 0.08 mg/kg/dose, OD (Tablets of 2.5 mg and 5 mg are available) - Adult dose: 5∼10 mg/day, OD |
- Hypotension, erythema, proteinuria, cough, hyperkalemia, hypersensitivity, edema |
| Cilazapril (Inhibace®) |
- 0.02∼0.06 mg/kg/day, divided into 1∼2 doses (1 mg tablets) - Adult dose: Start at 0.5 mg/day, OD and titrate |
Same as above |
| Nitrates | ||
| Isosorbide dinitrate (Nitorol®) |
- Sublingual: one-third∼one-half tablet/dose (5 mg tablets) - Oral: 0.5 mg/kg/day, divided into 3∼4 doses - Adult dose: 1∼2 tablets/dose (sublingual) - Frandol tape S® one-eighth∼1 sheet - Adult dose: 1 sheet (40 mg)/dose - Slow-release tablets (Nitrol-®R, Frandol® tablets) 0.5∼1 mg/kg/dose - Adult dose: 2 tablets/day (20 mg tablets) |
- Hypotension, headache, palpitations, dizziness, flushing |
| Nitroglycerin (Nitoropen®) |
- One-third∼one-half tablet/dose sublingual (0.3 mg tablets) - Adult dose: 1∼2 tablets/dose (0.3 mg tablets) |
Same as above |
The safety and efficacy of the above drugs have not been established in children. Doses should be determined according to the adult doses.
BID, two times a day; OD, once daily; TID, three times a day.
Among patients with Kawasaki disease, β-blockers may be administered to prevent reinfarction or sudden death in those with a history of myocardial infarction and to decrease long-term mortality. However, β-blockers may exacerbate already-existing coronary spasm by blocking β adrenergic receptors to thereby potentiate signaling via α adrenergic receptors.
1.4.3 NitratesIn a study of the effect of nitrates on coronary arteries in patients with a history of Kawasaki disease who received an intracoronary infusion of ISDN during CAG, the change in diameter after nitrate infusion was significantly lower in arteries with persistent aneurysms and arteries with regressed aneurysms than the control segments, which suggested the presence of endothelial dysfunction. However, the coronary vasodilative effects of nitrates are not expected to be beneficial in the treatment of acute ischemia due to severe coronary artery lesions. Sublingual or oral spray form of nitrates should be attempted in treating AMI.166,167
References
The following guidelines were referred to in the preparation of recommendations for the treatment of patients with cardiovascular sequelae in Kawasaki disease.
Guidelines proposed by the Japanese Circulation Society:
· Guidelines for diagnostic evaluation of patients with chronic ischemic heart disease (JCS 2010)168
· Guidelines for management of anticoagulant and antiplatelet therapy in cardiovascular disease (JCS 2009)169
· Guidelines for the primary prevention of ischemic heart disease revised version (JCS 2006)170
· Guidelines for management of acute coronary syndrome without persistent ST segment elevation (JCS 2007)171
· Guidelines for treatment of chronic heart failure (JCS 2010)172
· Guidelines for treatment of acute heart failure (JCS 2011)173
Guidelines proposed by the Japanese Society of Pediatric Cardiology and Cardiac Surgery:
· Guidelines for pharmacotherapy of heart failure in children174
Guidelines proposed by the American Heart Association (AHA)/American College of Cardiology (ACC):
· Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association175
· AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute176
1.5 Thrombolytic Therapy and Reperfusion Therapy (Table 15)126 1.5.1 Thrombolytic TherapyBecause AMI due to Kawasaki disease is mainly caused by thrombotic occlusion of coronary aneurysms, thrombolytic therapy is of great importance. The sooner thrombolytic therapy is initiated, the better the effect of therapy will be expected. The ACC/AHA/SCAI (Society for Cardiovascular Angiography and Interventions) guidelines recommend that thrombolytic therapy be performed within 12 hours after the onset of AMI.177a
| Mechanism of action |
| - Using an enzyme activating the fibrinolytic system to convert plasminogen on the clot into plasmin, which degrades fibrin to dissolve the clot. |
| Indications |
| - Dissolution of coronary clots in patients with acute myocardial infarction (within 12 hours after onset). |
| - Dissolution of clots in coronary aneurysms due to Kawasaki disease. |
| Drugs (drug classes) |
| - First-generation thrombolytic drugs: Urokinase (U). |
| - Second-generation thrombolytic drugs: Alteplase (A), a recombinant tissue plasminogen activator (t-PA). |
| - Third-generation thrombolytic drugs: Monteplase (M), a modified recombinant t-PA. Indicated only in Japan. |
| - Drugs indicated for children and adolescents in Japan: None. The safety and efficacy of the above drugs have not been established in this population. |
| - Use in children: The safety and efficacy of the above drugs in the treatment of acute myocardial infarction in children have not been established. |
| Method of administration |
| - Administer intravenously. Consider intracoronary thrombolysis for patients not responding to intravenous thrombolysis. |
| Doses |
| Intravenous thrombolysis |
| - Alteplase: 29.0∼43.5×104 units/kg (0.5∼0.75 mg/kg). Administer 10% of the total dose over 1∼2 minutes intravenously and infuse the remainder over 60 minutes (The recommended dose of alteplase is 0.1∼0.6 mg/kg/h for 6 hours in ACCP guidelines177). |
| - Monteplase: 2.75×104 units/kg. Administer intravenously over 2∼3 minutes. |
| - Urokinase: 1.0∼1.6×104 units/kg. Administer intravenously over 30∼60 minutes. |
| Intracoronary thrombolysis |
| - Urokinase: Administer at a dose of 0.4×104 units/kg over 10 minutes. Administration may be repeated at most four times. |
| Precautions for use during pregnancy and effects on fetuses |
| - Fetal death occurred in animal studies (U, A, M). In rabbit studies, embryos and fetuses died at high doses. It has been suggested these drug may induce premature placental separation through their fibrinolytic activity. |
| - Major adverse drug reactions: Major bleeding including cerebral hemorrhage, hemorrhagic cerebral infarction, arrhythmias, cardiac rupture, and anaphylactic reactions. |
| - Thrombolytic drugs are relatively contraindicated for patients with cerebral infarction, transient cerebral ischemia, or other neurological disorders, and those with a history of hypertension. |
ACCP, American College of Chest Physicians.
Adapted from Guidelines for Drug Therapy in Pediatric Patients with Cardiovascular Diseases (JCS 2012). Guidelines for Diagnosis and Treatment of Cardiovascular Diseases 2012: 89–301, with modification.126
There are no standard pediatric doses of the drugs used for thrombolytic therapy listed below. Thrombolytic drugs should thus be administered carefully on the basis of the condition of individual patients. It has been reported that the rate of recanalization is 70~80% after intravenous thrombolytic therapy, and may be increased by about 10% when intracoronary administration of thrombolytic drugs (urokinase [UK]) is added to intravenous therapy. Since thrombolytic therapy may be complicated by subcutaneous hemorrhage at the site of catheter insertion, cerebral hemorrhage, and reperfusion arrhythmia, patients should be carefully observed during and following thrombolytic therapy. As tissue plasminogen activators (t-PAs) and pro-urokinase (pro-UK) are proteins and may induce anaphylactic shock, repeated administrations of these drugs should be avoided whenever possible.
a. Intravenous Thrombolysis
i. UK
Infuse at a dose of 1.0~1.6×104 units/kg (maximum dose 96×104 units) over 30~60 minutes.
ii. t-PAs
- Alteplase (Activacin®, Grtpa®): 29.0~43.5×104 units/kg. Administer 10% of the total dose over 1~2 minutes intravenously and infuse the remainder over 60 minutes.
- Monteplase (Cleactor®): 2.75×104 units/kg. Administer intravenously over 2~3 minutes.
- Pamiteplase (Solinase®): 6.5×104 units/kg. Administer intravenously over 1 minute.
b. ICT
UK: Administer at a dose of 0.4×104 units/kg over 10 minutes. Administration may be repeated at most four times.
1.5.2 Antithrombotic Therapy During PCIIn general, PCI is indicated for patients within ≤12 hours after onset. Stenting is the most prevalent PCI technique, and the combination of thrombolysis and stenting is also common. Early treatment with oral antiplatelet drugs (aspirin, clopidogrel [Plavix®], and cilostazol [Pletal®]) or intravenous heparin is promptly begun after PCI to prevent the development of in-stent thrombosis.
1.6 Initial (Medical) Treatment for AMI 1.6.1 General Treatment PolicyThe main purpose of treatment of AMI in children is, as in adult patients, to decrease mortality during the acute phase and improve long-term prognosis.178–183 It has been reported in adults that reperfusion therapy shortly after the onset of AMI decreases mortality. Since AMI in children with a history of Kawasaki disease is caused by thrombotic occlusion of the coronary arteries, it is essential to initiate thrombolytic therapy or PCI as soon as possible to achieve reperfusion, as in the case of AMI in adult patients.184,185 During the initial treatment immediately after arrival at the emergency department or admission to hospital, prompt diagnosis and initial treatment should be performed to determine the treatment strategy for AMI and prepare for emergency CAG and reperfusion therapy.
1.6.2 Initial Treatmenta. General Treatment
i. Oxygen Therapy
Oxygen is administered to control myocardial injury.
ii. Establishment of Vascular Access
More than one means of vascular access should be established to ensure prompt treatment of complications possibly associated with AMI.
iii. Pain Control
Morphine hydrochloride (0.1~0.2 mg/kg) is the most effective agent, and should be slowly administered intravenously.
iv. Nitrates
Nitroglycerin should be administered intravenously or sublingually.
v. Intravenous Heparin Therapy
Use of heparin therapy prior to reperfusion therapy may increase the rate of recanalization. Heparin should be infused continuously at 10~20 units/kg/hr.
vi. Treatment of Complications
Complications of AMI such as heart failure, cardiogenic shock, and arrhythmia should be treated accordingly.
b. Reperfusion Therapy
Reperfusion therapy is performed to reopen the culprit coronary artery causing thrombotic occlusion shortly after onset in order to avoid the expansion of infarct lesion and maintain cardiac function.
i. Intravenous Thrombolytic Therapy
See Section 1.5.1.a on “Thrombolytic Therapy and Reperfusion Therapy”.
c. Anticoagulant Therapy and Antiplatelet Therapy to Prevent Recurrence of AMI
i. Heparin
Heparin should be infused intravenously at a dose of 200~400 units/kg/day, and the dose should be adjusted to maintain an APTT 1.5~2.5 times the baseline value.
ii. Warfarin
Warfarin should be administered at a dose of 0.1 mg/kg/day once daily, and the dose should be adjusted to maintain an INR of about 2.0~2.5.
iii. Aspirin
Aspirin should be administered at a dose of 3~5 mg/kg/day once daily (maximum dose of 100 mg).
2. Non-Pharmacotherapy 2.1 Catheter-Based Therapy 2.1.1 Indications for Catheter-Based TherapyThe following patients are indicated for catheter-based therapy:
1. Patients with ischemic symptoms caused by coronary stenosis in whom CAG revealed significant stenosis (≥75% luminal diameter).
2. Patients in whom CAG revealed significant stenosis (≥75% luminal diameter), and have no ischemic symptoms during activities of daily living but show ischemic findings during exercise ECG, exercise stress myocardial perfusion scintigraphy, pharmacological stress myocardial perfusion scintigraphy, or other appropriate examinations.
3. Patients with ostial lesions are contraindicated for catheter-based therapy.
4. Catheter-based therapy is contraindicated for patients with multivessel disease and those with significant stenosis (≥75% luminal diameter) or occlusion of the contralateral coronary arteries. However, the latter cases may be treated with catheter-based therapy when bypass surgery is performed for the lesions in the contralateral coronary arteries.
2.1.2 Types of PCI Techniques, Indications, and Precautionsa. PCI
i. Reperfusion Therapy
i-i. ICT
UK should be infused at a dose of 0.4×104 units/kg over 10 minutes. Administration may be repeated at most four times.
i-ii. PCI
The guidelines for the management of patients with ST-elevation acute myocardial infarction (JCS 2008) proposed by the Japanese Circulation Society recommend that primary PCI should be considered when it can be performed within 90 minutes (door-to-balloon time) of the first medical contact for patients presenting within 12 hours of symptom onset (Class I recommendation).186 The guidelines also describe that thrombosuction should be tried first during PCI in order to prevent plaque debris and clots from flowing into peripheral vessels, reduce no-reflow phenomenons, and thereby improve cardiac function after intervention. Stenting is the most prevalent PCI technique. Treatment with oral antiplatelet drugs (aspirin, clopidogrel [Plavix®], and cilostazol [Pletal®]) or intravenous heparin is promptly begun after PCI to prevent the development of in-stent thrombosis.
ii. Plain Old Balloon Angioplasty
In the treatment of coronary artery lesions due to Kawasaki disease, plain old balloon angioplasty (POBA) is effective in the treatment of stenotic lesions that developed ≤6 years previously, and becomes less effective as time increases.113,142,187–190 Coronary artery legions due to Kawasaki disease are harder than those observed in adults, a higher balloon pressure is often required, and the risk of development of new aneurysms related to balloon dilatation is higher than in adults. The recommended balloon pressure is ≤10 atm.
b. Stenting
Stenting is indicated for older children (≥13 years of age) in whom calcification of coronary lesions is relatively mild.152,153,191–198 Stenting can achieve a larger lumen than POBA can. Stenting is also effective in the treatment of coronary arteries in which aneurysms and stenosis are present in succession. The risk of the development of new aneurysms after balloon dilatation is lower in patients receiving balloon dilatation and stenting than those receiving balloon dilatation only, but the balloon pressure should not be higher than 14 atm. Lesions that might require a higher balloon pressure require lesion modification using a rotablator. Because surgical treatment of patients with a history of Kawasaki disease is often performed during adolescence, and patients may often receive surgical treatment thereafter, physicians should consider the risk of late-onset thrombosis associated with the discontinuation of antiplatelet therapy. The use of drug-eluting stents should be considered carefully.196
c. Rotablator (Percutaneous Transluminal Coronary Rotational Atherectomy, PTCRA)
The rotablator uses a rotating metal burr coated with about 2,000 microscopic diamond particles. The burr rotates at high speeds to grind the arteriosclerotic lesion into small fragments, theoretically ≤5 μm in diameter, that do not cause peripheral thromboembolism and are degraded in the reticulo-endothelial system. Some physicians do not use balloon dilatation after coronary rotational atherectomy, but many physicians perform balloon dilatation at low pressures after atherectomy.
d. IVUS
In order to ensure successful implementation of PCI, the degree and extent of calcified lesions should be accurately identified to select appropriate procedures. IVUS helps delineate the structure of the coronary artery wall, and determine the percentage of luminal circumference covered with calcification, and the extent of calcified lesions. It is desirable that physicians determine appropriate PCI procedures for children according to the body size, findings of CAG and IVUS.143,153,196,199–201
2.1.3 Institutions and Backup System RequirementsPCI for patients with coronary artery lesions due to Kawasaki disease is not possible without collaboration between cardiologists with expertise in coronary catheterization and pediatric cardiologists who understand the natural history and pathology of cardiac complications of Kawasaki disease. Support from cardiac surgeons is also essential. It is desirable that PCI for this patient population be performed in cardiovascular centers and other institutions specialized in cardiovascular diseases.
2.1.4 Postoperative Management, Assessment, and Follow-upAfter 4~6 months after PCI, selective CAG should be performed to evaluate the outcome of treatment. A survey has revealed that there is no significant difference between the CAGB and PCI groups in the composite primary endpoint of death or AMI, while the incident of repeated revascularization, a secondary endpoint, is higher in the PCI group.202 Because surgical treatment for cardiovascular sequelae in Kawasaki disease are typically performed for patients 13~18 years of age, pediatric cardiologists should communicate well with cardiologists to share information and transition the patients to ensure successful long-term management and continued patient education.203
2.2 Surgical Treatment (Table 16)Although the prevalence of coronary artery lesions due to Kawasaki disease tends to decrease, there is still a small number of children who have persistent or progressing coronary artery lesions and eventually develop ischemic heart disease during childhood. For such patients who do not respond well to medical treatment, CABG using autologous pedicle internal mammary artery grafts is the most reliable treatment option.204–208 As the leading causes of death in patients with Kawasaki disease are sudden death and myocardial infarction, the determination of surgical treatment must be made in a timely manner.
| Coronary artery bypass grafting (CABG) may be effective in patients who have severe occlusive lesions in main coronary arteries (especially in the central portions of these arteries) or rapidly progressive lesions with evidence of myocardial ischemia. It is preferable to perform CABG using autologous pedicle internal mammary artery grafts regardless of age. Treatment such as mitral valve surgery should be considered when mitral insufficiency not responding to medical treatment is present, although such cases are rare. |
| CABG |
| CABG is indicated for patients with angiographically evident severe occlusive lesions of the coronary arteries and viability of myocardium in the affected area. Viability should be evaluated comprehensively, based on the presence/absence of angina and findings of exercise ECG, thallium myocardial scintigraphy, two-dimensional echocardiography, left ventriculography (regional wall movement), and other techniques. |
| - Findings of coronary angiography: The following findings are most important. When one of the following findings is present, consider surgical treatment. |
| 1. Severe occlusive lesions in the left main coronary trunk |
| 2. Severe occlusive lesions in multiple vessels (2 or 3 vessels) |
| 3. Severe occlusive lesions in the proximal portion of the left anterior descending artery |
| 4. Jeopardized collaterals |
| In addition, the following conditions should also be considered in determining treatment strategy. |
| (1) When the event is considered a second or third infarction due to the presence of chronic infarct lesions, surgery may be indicated. For example, surgery may be considered to treat lesions limited to the right coronary artery. |
| (2) Lesions associated with recanalization of the occluded coronary artery or formation of collateral vessels should be evaluated especially carefully. Surgical treatment may be considered for patients with findings of severe myocardial ischemia. |
| (3) Whether CABG is indicated should be considered carefully in younger children based on long-term patency of grafts. In general, young children controllable with medical treatment are followed carefully with periodic coronary angiography to allow them to grow, while patients with severe findings have undergone surgery at 1∼2 years of age. It is recommended that pedicle internal mammary artery grafts be used in such cases as well. |
| - Findings of left ventricular function testing: It is desirable that patients with favorable left ventricular function be treated with surgery, though patients with regional hypokinesis may also be indicated for surgery. Patients with serious diffuse hypokinesis must be evaluated with particular care and comprehensively based on findings for the coronary arteries and other available data. Heart transplantation may be indicated in rare cases. |
| Mitral valve surgery |
| Valvuloplasty and valve replacement may be indicated for patients with severe mitral insufficiency of long duration not responding to medical treatment. |
| Other surgery |
| In rare cases, Kawasaki disease has been complicated by cardiac tamponade, left ventricular aneurysm, aneurysms of the peripheral arteries, or occlusive lesion, patients with these conditions may be indicated for surgery. |
Adapted from “Study on Kawasaki Disease”, the Ministry of Health and Welfare research project on mental and physical disorders. A research report in 1985. 1986: 39–42,209 with modification.
Table 16 lists the criteria for indications for surgical treatment of cardiovascular sequelae in Kawasaki disease.209 The nature of coronary artery lesions indicated for surgical treatment in this pediatric population is essentially identical to that in the adult population without Kawasaki disease, and includes (1) severe occlusive lesions in the left main coronary trunk; (2) severe occlusive lesions in multiple vessels (2 or 3 vessels); (3) severe occlusive lesions in the proximal portion of the left anterior descending artery; and (4) jeopardized collaterals. Surgical treatment should be considered as a priority option for patients with a history of myocardial infarction in order to ensure secondary prevention of myocardial infarction. In children, the progression of myocardial ischemia may often occur asymptomatically, and the severity of coronary angiographic findings is often inconsistent with clinical symptoms. Accordingly, candidates for CABG should be comprehensively evaluated on the basis of clinical signs and symptoms as well as findings of CAG, exercise ECG, echocardiography, stress myocardial scintigraphy, left ventriculography, and other techniques to specify the location and viability of ischemic myocardium.
2.2.2 Age at Surgical TreatmentIn a survey in Japan, patients undergoing CABG for the treatment of coronary artery lesions due to Kawasaki disease are 11 years of age on average and range between 1 month and 44 years of age at the time of surgery, with children aged 5~12 years predominant.210 It has been reported that recently CABG can be performed safely even in children younger than those for whom it was previously considered indicated.208,211,212 Surgical treatment during the early phase of the disease is beneficial in avoiding left ventricular hypokinesia, and has a lower incidence of postoperative events than that during later phases of the disease.211
2.2.3 Surgical TechniquesThe most desirable surgical technique is CABG using pedicle right or left mammary thoracic artery grafts. It has been reported that the diameter and length of such grafts increase with the somatic growth of children.208,213 Large saphenous vein grafts were frequently used in the past, but are no longer used in the present day because of its low long-term patency and the absence of growth after grafting.210,213,214 CABG using right gastroepiploic artery grafts is becoming common,215 but these grafts are not well developed in children, and can be used only in older children with a large body size.
2.2.4 Outcome of SurgeryCABG not only reduces anginal symptoms, but also prevents the occurrence of myocardial infarction and improves prognosis in patients with severe coronary artery legions.
In patients with severe coronary artery lesions due to Kawasaki disease, CABG is also effective in reducing and preventing recurrence of myocardial ischemia and angina. Studies demonstrated the efficacy of CABG, and have revealed that it improved coronary perfusion and left ventricular function during stress testing.216
a. Graft Patency
The patency of internal thoracic artery grafts, that are the only available grafts for CABG in children, is as high as 87% overall, and 91%, 100%, and 84% when grafted to the left anterior descending artery, the left circumflex artery, and the right coronary artery, respectively, at 20 years after CABG.217
b. Activities of Daily Life and Problems After Surgery
In a survey of patients with a significant limitation to activities of daily life due to cardiovascular sequelae in Kawasaki disease, 85% of them became able to participate in gym class in school with no limitation, and many patients have a favorable social outcome, including marriage and childbirth.207 According to a recent report, the 10-, 20- and 25-year survival rates are 98%, 95% and 95%, respectively.217
2.2.5 Other Surgerya. Downsizing Operation of Giant Coronary Aneurysms
Blood flow in giant aneurysms is slow and the risk of thrombogenesis is high.218,219 Recently, attempts have been made to use the combination of CABG and downsizing operation to treat giant aneurysms to improve flow rate and flow pattern in lesions by decreasing the diameter of the aneurysms, and to prevent the formation of thrombi by increasing shear stress on vessel walls. It has been reported that warfarin therapy could be terminated in some patients treated in this fashion.211,220
b. Surgical Treatment of Mitral Valve Insufficiency
Surgical treatment should be considered for patients with severe mitral valve regurgitation due to Kawasaki disease according to the severity of regurgitation, age of the patient, the severity of coronary artery lesions, left ventricular function, and other conditions.221 Valvuloplasty is the most commonly used technique. In children undergoing valve replacement, mechanical valves, which are more durable than bioprosthetic valves, are commonly used.222
c. Surgical Treatment of Aortic Aneurysms and Peripheral Aneurysms
In addition to coronary aneurysms, patients with Kawasaki disease may develop aneurysms in the ascending aorta, abdominal aorta, iliac artery, or axillary artery.216 The use of synthetic grafts has been reported in the treatment of descending aortic aneurysms. Surgical treatment of aneurysms is indicated only for large or progressive lesions.
d. Heart Transplantation
More than ten cases of heart transplantation for the treatment of Kawasaki disease have been reported in the world. It has been reported that they have severe left ventricular dysfunction with a left ventricular fractional shortening (FS) of 5~24%, 16% on average, and that all patients had coronary artery lesions, and many patients (about 40%) had ventricular arrhythmia, ventricular tachycardia, or ventricular fibrillation. Heart transplantation was performed at the age of 8.5 years on average, and two children underwent it at the age ≤4 months of age.223 Heart transplantation is beneficial in (1) patients with significant left ventricular dysfunction, and (2) patients who have life-threatening arrhythmia and significant lesions in peripheral segments of the coronary arteries.
3. Summary of Treatment Options (Table 17)Table 17 summarizes treatment options for coronary artery lesions by severity. As the major causes of death during the remote phase of Kawasaki disease are coronary stenosis due to intimal hyperplasia and ischemic heart disease due to thrombotic coronary occlusion, pharmacotherapy is important in avoiding these cardiac accidents and improving the QOL of patients. For patients not responding to pharmacotherapy who have the progression of stenotic lesions and cannot control the risk of thrombosis, non-pharmacotherapy such as PCI and CABG should be considered proactively.
| Antiplatelet drugs (aspirin, dipyridamole, ticlopidine) | |
| Severity classification IV, V | Class I |
| Severity classification III | Class II |
| Severity classification I, II | Class III |
| Anticoagulant drugs (warfarin) | |
| Severity classification IV, V | Class I |
| Severity classification III | Class II |
| Severity classification I, II | Class III |
| Coronary vasodilators (e.g., Calcium channel blockers, β-blockers, nitrates) | |
| Severity classification V | Class I |
| Severity classification IV | Class II |
| Severity classification I, II, III | Class III |
| Drugs for heart failure (ACE inhibitors, ARBs, β-blockers) | |
| Severity classification V | Class I |
| Severity classification IV | Class II |
| Severity classification I, II, III | Class III |
| PCI | |
| Severity classification V (b) | Class I |
| Severity classification V (a) | Class II |
| Severity classification I, II, III, IV | Class III |
| CABG | |
| Severity classification V (b) | Class I |
| Severity classification V (a) | Class II |
| Severity classification I, II, III, IV | Class III |
ACE, angiotensin converting enzyme; ARBs, angiotensin II receptor blockers; CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention.
Appropriate decision making is essential in the treatment of cardiovascular sequelae in Kawasaki disease according to careful consideration of the patient’s disease status, age, school life (e.g., exercise, school events, and going to university), and social life (e.g., career, job, marriage, and pregnancy/childbirth).
The guidance on activities of daily life and exercise mainly includes management of daily activities in school. The following management is desirable (See School Activity Management Table, the 2011 revision.224 Tables 18 and 19).
 |
*Basic exercise: including resistance (isometric) exercise.
Adapted from The Japanese Society of School Health. Guide for the use of the School Activity Management Table for Children with Heart Disease, the 2011 revision. 2013: 3–11.224
 |
* Basic exercise: including resistance (isometric) exercise.
Adapted from The Japanese Society of School Health. Guide for the use of the School Activity Management Table for Children with Heart Disease, the 2011 revision. 2013: 3–11.224
No restriction of activities of daily life or exercise is needed. In the School Activity Management Table, physicians may indicate “no management needed” for children ≥5 years after onset. During the 5-year period after onset, “E-allowed” (i.e., Category E [intense exercise is allowed] in terms of management, with school sport club activities “allowed”) should be selected in the table. When a patient is assigned the “no management needed” rating, the attending physician should indicate the termination of follow-up on the existing or newly created “Acute Phase Kawasaki Disease in Summary” (Figure 5) of the patient, and provide advice on how to prevent lifestyle-related diseases to the patient and parents.
1.2 Patients Not Evaluated for Coronary Artery Lesions During the Acute Phase 1.2.1 Patients in Whom Examination After the Acute Phase Revealed No Coronary Artery LesionsNo restriction of activities of daily life or exercise is needed. Follow the instructions in Section 1.1 “Children without Evidence of Coronary Artery Lesions during the Acute Phase” above.
1.2.2 Patients in Whom Examination After the Acute Phase Revealed Persistent Coronary Artery Lesions According to the Criteria for Severity of Coronary Artery Lesions in This Guidelinea. Patients in Whom Examination After the Acute Phase Revealed No Coronary Artery Lesions (or Revealed Regression of Coronary Artery Lesions)
No restriction of activities of daily life or exercise is needed. Follow the instructions in Section 1.1 “Children without Evidence of Coronary Artery Lesions during the Acute Phase” above.
b. Patients Not Evaluated With CAG
Follow the instructions on activities of daily life and exercise in Section 1.3 “Patients Who Have Been Evaluated for Coronary Artery Lesions during and after the Acute Phase” below. Patients should be categorized into the following groups, and provided with instructions accordingly.
(1) Patients in whom echocardiography detected small aneurysms or dilatation
(2) Patients in whom echocardiography detected medium aneurysms
(3) Patients in whom echocardiography detected giant aneurysms
It is desirable that patients in groups (2) and (3) undergo CAG.
c. Patients in Whom CAG Revealed Persistent Coronary Artery Lesions
Follow the instructions on activities of daily life and exercise in Section 1.3 “Patients Who Have Been Evaluated for Coronary Artery Lesions during and after the Acute Phase” below. Patients should be categorized into the following groups, and provided with instructions accordingly.
(1) Patients in whom CAG revealed small aneurysms or dilatation remaining
(2) Patients in whom CAG revealed medium aneurysms remaining
(3) Patients in whom CAG revealed giant aneurysms remaining
1.3 Patients Who Have Been Evaluated for Coronary Artery Lesions During and After the Acute Phase 1.3.1 Patients in Whom Transient Coronary Dilatation Disappeared After the Acute PhaseNo restriction of activities of daily life or exercise is needed. Follow the instructions in Section 1.1 “Children without Evidence of Coronary Artery Lesions during the Acute Phase” above.
1.3.2 Patients With Remaining Small Aneurysms or DilatationNo restriction of activities of daily life or exercise is needed. “E-allowed” should be selected in the School Activity Management Table.
(1) Follow the instructions in Section 1.1 “Children without Evidence of Coronary Artery Lesions during the Acute Phase” above when coronary artery lesions regress.
(2) Patients with remaining coronary artery lesions should be followed up at 2 months, 6 months, and 1 year after onset and annually or later.
1.3.3 Patients With Remaining Medium or Giant AneurysmsIt is desirable that patients of this type be followed by pediatric cardiologists.
a. Patients With No Findings of Stenosis or Myocardial Ischemia
No restriction of activities of daily life or exercise is needed. “E-allowed” should be selected in the School Activity Management Table not including giant aneurysms.
For patients with giant aneurysms, physicians should select “D-prohibited” (Category D [moderate exercise is allowed] in terms of management, with school sport club activities “prohibited”) in the School Activity Management Table, in principle. Patients with regressed giant aneurysms should be followed periodically because aneurysms with an internal diameter of ≥6 mm may be calcified or progress to stenotic lesions in 10 or 20 years.
b. Patients With Findings of Stenosis or Myocardial Ischemia
Intense exercise should be restricted. The level of allowable exercise should be rated at “D” or more severe category. School sport club activities should be “prohibited”.
c. Patients With a History of Myocardial Infarction
Activities of daily life and exercise should be restricted. Patients should be rated as Category “A” to “E” on the basis of their condition. School sport club activities should be “prohibited,” in principle.
1.4 Lesions Other Than Coronary Artery Lesions 1.4.1 Valvular DiseasePediatric cardiologists should evaluate patients with valvular disease due to Kawasaki disease to determine whether their activities of daily life and exercise should be restricted. Cardiac functions and indications for surgical treatment should be evaluated. Patients exhibiting improvement of echocardiographic findings may be assigned the rating of “no management needed”.
1.4.2 ArrhythmiaPediatric cardiologists should evaluate patients with arrhythmia due to Kawasaki disease to determine whether their activities of daily life and exercise should be restricted. The criteria for management of patients with arrhythmia (Guidelines for management of arrhythmia with no underling diseases, the 2002 revision, published by the School Cardiac Screening Study Committee of the Japanese Society of Pediatric Cardiology and Cardiac Surgery) should be followed when cardiac function is normal and myocardial ischemia can be ruled out.225 Arrhythmic patients with findings of abnormal cardiac function or myocardial ischemia should be collectively evaluated based on all available data.
1.4.3 Aneurysms Other Than Coronary AneurysmsPediatric cardiologists should manage these lesions individually based on their location and severity.
1.5 Management After Heart SurgeryPediatric cardiologists should follow patients undergoing heart surgery such as CABG, valvular surgery, and heart transplantation to ensure appropriate follow-up evaluation and patient education.
1.6 VaccinationsMaternal antibodies play important roles in preventing measles, rubella, mumps and varicella infections.226 Vaccinations against these diseases should be performed in order at least 6 months after high-dose IVIG therapy.
1.7 Lifestyle Changes to Prevent ArteriosclerosisSince there is concern that a history of Kawasaki disease may be a risk factor for the development of arteriosclerosis in later life, it is preferable that patients be educated on the prevention of lifestyle-related diseases when they receive their “Acute phase Kawasaki disease in summary” (Figure 5).
1.8 Cooperation With CardiologistsPatients with sequelae in Kawasaki disease should be followed by cardiologists when they grow up. Attending physicians should discuss with patients (or family) the schedule of follow-up by different departments in order to ensure lack of interruption of follow-up evaluation. Careful attention should be paid to avoid discontinuation of follow-up evaluation.
2. Follow-up EvaluationThere are no clearly defined policies on the timing and duration of non-invasive follow-up evaluation of patients with a history of Kawasaki disease in Japan. However, there is an almost complete consensus of opinion that patients with giant aneurysms and patients with regressed medium aneurysms should be followed up for life.35,146,148,227
The following guidelines are designed for patients who underwent periodic echocardiography during the acute phase of Kawasaki disease. Patients are classified by severity of coronary artery lesions on the basis of echocardiographic findings for the coronary arteries during roughly the first 30 days after onset, and guidance on how to follow up coronary artery lesions by cardiologists is provided based on the severity of echocardiographic coronary findings.
The reader should refer to the “Classification of coronary aneurysms during the acute phase” (Table 4A), and the “Severity classification” (Table 4B).
2.1 Severity Classification of Coronary Artery Lesions Based on Echocardiographic FindingsTable 20 lists the severity classification of coronary artery lesions based on echocardiographic findings.
| Echocardiographic classification |
Severity classification (See Table 4B) |
Echocardiographic findings |
|---|---|---|
| A-1 | I | No dilatation of coronary arteries. The coronary arteries tend to be larger during the acute phase than in control children,228,229 but no localized dilatation is detectable with echocardiography. |
| A-2 | II | Slight and transient dilatation of coronary arteries, which subsides within 30 days after onset. |
| A-3 | Milder cases in Category III | Small aneurysms with an internal diameter of ≤4 mm are detectable on day 30 after onset. |
| A-4 | Some cases in Categories III, IV and V |
Medium aneurysms are detectable on day 30 after onset. |
| A-4-1 | Medium aneurysms with an internal diameter of >4∼<6 mm are detectable. | |
| A-4-2 | Medium aneurysms with an internal diameter of 6∼<8 mm are detectable. | |
| A-5 | IV, V | Giant aneurysms with an internal diameter of ≥8 mm are detectable on day 30 after onset. |
The severity of cardiovascular lesions evaluated according to the severity classification of cardiovascular lesions due to Kawasaki disease (Table 4B) changes over time depending on the duration after onset. Figure 4 shows typical relationships between the two classification systems.
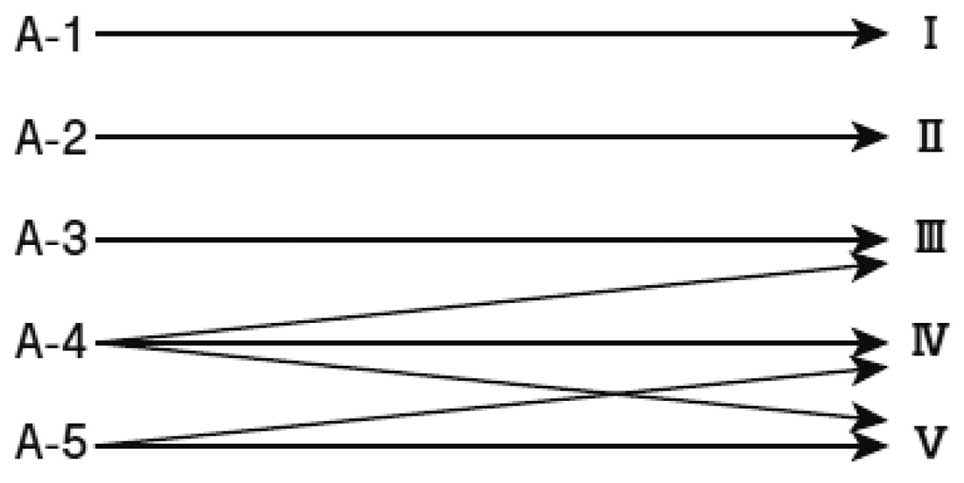
Relationship between the echocardiography-based severity classification (Left) and the severity classification of cardiovascular lesions due to Kawasaki disease (Right).
Patients in Category A-1, i.e., patients with no dilatation of coronary arteries, correspond to Category I of the severity classification of cardiovascular lesions due to Kawasaki disease.
Patients in this category should be followed for 5 years, i.e., at 1, 2, and 6 months and 1 and 5 years after the onset of Kawasaki disease. Additional annual follow-up may be scheduled from the second to fifth years through consultation between patients/family and attending physicians. Further follow-up schedules in the sixth year and thereafter should be scheduled individually.
Follow-up evaluation should include ECG, echocardiography, and, if required, chest X-ray. It is desirable that patients be evaluated with exercise ECG at the time of final evaluation.
2.3.2 Patients in Category A-2This category (patients with slight and transient dilatation of coronary arteries which subsides within 30 days after the onset of Kawasaki disease) corresponds to Category II of the severity classification of cardiovascular lesions due to Kawasaki disease.
It is believed that these patients have no significant problems in terms of coronary artery lesions.37,38,148,166,227 Follow-up examination should be performed as specified in the section on Category A-1.
2.3.3 Patients in Category A-3This category (patients who have small aneurysms at 30 days after the onset of Kawasaki disease) corresponds to relatively mild cases among those classified in Category III of the severity classification of cardiovascular lesions due to Kawasaki disease.
In principle, patients should be followed every 3 months until findings of dilatation disappear and then annually until entry into elementary school (age of 6, 7), then in 4th grade (age 9, 10), at entry into junior high school (age of 12, 13), and at entry into senior high school (age of 15, 16).
Follow-up examination should be performed as specified in the section on Category A-1, and exercise ECG should be added in children at ages when it is feasible. In patients ≥10 years after onset, coronary imaging by MDCT or MRCA (the latter is more preferable considering radioactive exposure) should be considered as the final coronary imaging at the time of final follow-up evaluation.
2.3.4 Patients in Category A-4This category (Patients who have medium aneurysms at 30 days after the onset of Kawasaki disease) corresponds to some cases among those classified in Categories III, IV, and V.
Since long-term prognosis in this category differs significantly among patients, the duration of follow-up should be determined individually according to patient condition. Typically, echocardiographically detected coronary dilatations disappear within one year after onset, and regression of coronary artery lesions detectable by CAG is observed during the two years after onset.146,230
According to findings reported by now,35–48,148,166,227 patients in category A-4 are further classified into two categories by the internal diameter of coronary aneurysms on day 30 after onset, A-4-1 (>4~<6 mm) and A-4-2 (6~<8 mm). The recommended schedules and items of follow-up evaluation are as follows.
a. Patients in Category A-4-1
In this category of patients who have medium aneurysms with an internal diameter of >4~<6 mm, thickening of the intima and media is observed, but no progression to stenotic lesions nor calcification of coronary artery lesions is observed in 20 years after onset. Patients should be evaluated once every 1~3 months with ECG, echocardiography, chest X-ray (when necessary), and exercise ECG (when feasible) until dilatation is no longer observed on echocardiography. Following the disappearance of dilatation, patients should be evaluated annually. Patients with aneurysms remaining 1 year after onset should be evaluated once every 3~6 months. Selective CAG may be considered on an individual basis. Although the prognosis of this category of patients is considered relatively good, it is desirable that they undergo MDCT or MRCA every five years to evaluate the coronary arteries until further evidence becomes available.
b. Patients in Category A-4-2
In this category of patients who have medium aneurysms with an internal diameter of 6~<8 mm, the incidence rates of stenotic and calcified lesions increase over time, and the progression to arteriosclerotic lesions is also noted. Patients should be followed in a fashion similar to those in Category A-4-1. Patients must undergo follow-up with selective CAG at least once during the early convalescent phase and at the time of disappearance of echocardiographically evident coronary dilatations. Patients with persistent aneurysms should be followed appropriately.
2.3.5 Patients in Category A-5This category (i.e., patients who have giant aneurysms at 30 days after the onset of Kawasaki disease) corresponds to Categories IV and V of the severity classification of cardiovascular lesions due to Kawasaki disease.
It is believed that aneurysms in patients in this category do not regress completely and may frequently progress to coronary occlusive lesions.146,230–232 Patients with persistent giant aneurysms must be followed for life and receive treatment continuously, and should be individually evaluated to design tailor-made treatment.
All patients in this category should undergo initial selective CAG during the early convalescent phase of Kawasaki disease to specify the extent of lesions. As aneurysms outside the coronary arteries may develop in about 2~3% of patients, careful observation should be made.146 As thrombotic occlusion in giant aneurysms in right coronary artery may often develop in the first two years after onset,232 and the incidence of stenotic lesions in giant aneurysms in the left anterior descending artery increases over time,146,232 patients should be carefully observed for clinical signs/symptoms, and followed with appropriate combinations of ECG, exercise ECG, echocardiography, stress myocardial scintigraphy, selective CAG, MRI, MRCA, MDCT or other appropriate techniques. The duration of follow-up differs among individual patients. In general, patients should be evaluated once every 1~3 months during the first year, and once every 3~6 months or later.
2.4 Acute Phase Kawasaki Disease in SummaryIn 2003, the Japan Kawasaki Disease Research Society (currently the Japanese Society of Kawasaki Disease) developed the “Acute phase Kawasaki disease in summary” (Figure 5) to encourage patients who had coronary artery lesions during the acute phase of Kawasaki disease as well as those who were treated successfully to carry summarized medical records during the acute phase of this disease (e.g., clinical signs/symptoms, treatment, and cardiac complications).233 Because long-term prognosis of this disease after reaching adulthood is still unclear, it is important for individuals with a history of this disease to keep medical information during the acute phase, and provide the information to healthcare professionals whenever necessary.

Acute phase Kawasaki disease in summary.
No consistent evidence is available on this matter. The presence of medium aneurysms with an internal diameter of ≥6 mm during the acute phase is believed a risk factor for arteriosclerosis.227,231,234 In patients with coronary aneurysms with an internal diameter of >4~<6 mm during the acute phase, thickening of the intima and media have been noted in some cases during the remote phase,227 and they are considered to be at risk for developing new stenotic or calcified lesions in 30~40 days after onset. Patients with a history of Kawasaki disease, including those who have no coronary artery lesions during the acute phase and those with transient coronary dilatation during the first 30 days after onset of the disease should use the “Acute phase Kawasaki disease in summary” (Figure 5) to provide accurate medical information during the acute phase to cardiologists who treat them.
3.2 Collaboration With Cardiologists Providing Healthcare Services to Adult PatientsPediatricians with expertise in Kawasaki disease cannot cover healthcare services to adult patients with a history of the disease who experience lifestyle-related diseases, pregnancy, childbirth or other adult-onset conditions. There is a need for special clinics for adult patients with a history of Kawasaki disease where patients are managed by cardiologists and supported by obstetricians whenever necessary.
3.3 How to Avoid DropoutsIt has been reported that dropouts, i.e., patients who stop visiting their clinic, occur in a relatively early phase of follow-up.235,236 As both patients and pediatric cardiologists should be responsible for continuing follow-up evaluations, healthcare professionals should make every effort to prevent dropout by identifying patients who stop visiting their clinic and encourage them to visit for follow-up.
Cardiovascular sequelae caused by arteritis in Kawasaki disease may be named as arteriosclerosis due to Kawasaki disease, which differs substantially from atherosclerosis in etiology, pathology and pathophysiology. However, the evidence is limited for the effect of atherosclerosis as a lifestyle-related disease during adulthood on arteriosclerosis due to Kawasaki disease.
It has been pointed out that endothelial dysfunction and chronic inflammatory reactions may continue during the remote phase in patients with medium or giant aneurysms including those in whom aneurysms have regressed.35,36,38,237 Because endothelial dysfunction is a precursor of atherosclerosis, it is highly likely that patients with persistent vascular dysfunction and perfusion abnormalities due to sequelae even after the remission of acute-phase inflammation have a high risk for the progression to atherosclerosis. In a study in patients during the remote phase of Kawasaki disease, intravascular echocardiography revealed the presence of intimal hyperplasia at the sites of regressed coronary aneurysms and severe intimal hyperplasia and calcification at the sites of localized stenotic lesions.37
Although a histopathological study has revealed the active remodeling of the coronary artery lesions due to Kawasaki disease during the remote phase,42 only a few reports have described the relationship between arteriosclerotic lesions due to Kawasaki disease and atherosclerosis. A pathological study of autopsy cases of adult patients with a history of Kawasaki disease has reported that advanced atherosclerotic lesions with microcalcification, necrotic cell debris containing cholesterin crystals, aggregation of foamy cells and hemorrhage are present in the walls of giant aneurisms, while in regressed aneurysms and recanalized aneurysms after thrombotic occlusion, small aggregations of foamy cells and penetration of plasma elements in the thickened intima composed of dense fibrotic tissues.39 When comparing these findings with autopsy findings of young Japanese patients with atherosclerosis,238 it can be concluded that coronary aneurysms due to Kawasaki disease have more severe atherosclerotic lesions than in coronary artery lesions in patients without a history of the disease. However, the findings noted in regressed aneurysms and recanalized lumen represent initial changes in atherosclerosis, and it is thus difficult to conclude that severe atherosclerosis occurs in coronary sequelae in Kawasaki disease. There is no consensus on the relationship between arteriosclerosis due to Kawasaki disease and atherosclerosis, and further investigation is required.
2. Progression of Arteriosclerosis: Clinical FeaturesRecent studies have reported findings suggestive of the presence of vascular abnormalities in patients with and without cardiovascular sequelae in Kawasaki disease during the remote phase of vasculitis due to the disease.39,42,239–241 which provoked a discussion about what kind of follow-up measures are required for adults with a history of this disease during childhood.
Vascular disorder in patients with a history of Kawasaki disease ranges widely from endothelial cell dysfunction to structural vascular dysfunction. It is believed that persistent endothelial cell dysfunction causes structural vascular dysfunction through complex interactions between inflammation, oxidant stress, different cytokines, among others.242
Morphological assessment of coronary arteries has been performed with transthoracic echocardiography and X-ray CAG. However, IVUS, a new technique enabling detailed assessment of coronary arteries, has made cardiologists understand the importance of detailed assessment of the coronary arteries as it revealed the presence of intimal hyperplasia in coronary arteries that appeared normal with the conventional procedures.243 More recently, MDCT and MRCA using the black blood method have become available as less invasive methods of morphological assessment. These new procedures can detect calcification of coronary arteries that develop frequently in the remote phase of Kawasaki disease. In general, calcification of coronary arteries is considered as a risk factor for cardiovascular events,244,245 but the mechanism of the development of calcification due to Kawasaki disease has not been clarified. Further investigation is necessary.
It is widely known that endothelial cell dysfunction occurs as a precursor of morphological changes such as intimal hyperplasia.246 Because morphological changes decrease the plasticity of arteries, assessment of vascular function is drawing attention as a procedure to facilitate early intervention. Flow-mediated dilation (FMD), a new measure of vascular function using reactive hyperemia that stimulates the release of nitric oxide (NO) from endothelium, may accurately detect vascular dysfunction. Recent studies have reported a decrease in FMD during the remote phase of Kawasaki disease,241,247 which suggest that the history of Kawasaki disease is a risk factor for endothelial cell dysfunction.
In the presence of endothelial cell dysfunction, it is likely that the process to atherosclerosis, starting with the expression of adhesion molecules and inflammatory processes, occurs over time. However, atherosclerosis is an entity different from arteriosclerosis due to Kawasaki disease occurring during the remote phase of Kawasaki disease. Although the development of atherosclerosis during the remote phase of Kawasaki disease has not been reported, it has been reported that a high-cholesterol diet induced the development of atherosclerosis developed in an animal model of vasculitis similar to Kawasaki disease.248
Further investigation is necessary to understand how atherosclerosis develops in coronary arteries affected by arteriosclerosis due to Kawasaki disease. We hope that this question will be solved when patients with a history of Kawasaki disease who have persistent endothelial cell dysfunction become middle age and have a higher risk for atherosclerosis.
Currently, there are no data on the actual status and pathological features of adult patients with a history of Kawasaki disease, and no standards are available for the diagnosis and treatment of such patients.
The most important points in the management of adult patients with cardiovascular sequelae in Kawasaki disease are (1) to clarify the accurate status of the cardiovascular sequelae; (2) to control and manage the risk factors for the progression to atherosclerosis; and (3) to administer appropriate drug and non-pharmacotherapies to ensure better prognosis.
1. DiagnosisIn adult patients, correct evaluation of coronary artery lesions is often difficult with transthoracic echocardiography as the lung overlapping the heart may reduce the quality of images. Noninvasive techniques or catheter-based methods of CAG are required for the evaluation of coronary artery lesions.
1.1 Patients Without Coronary Aneurysms During ChildhoodFamily and patients should discuss with attending physicians the need for follow-up evaluation on an individual basis, and patients may undergo noninvasive evaluation once every several years during adulthood if they request it.249
1.2 Asymptomatic Patients With Coronary Aneurysms Persisting From ChildhoodIt is desirable that patients should be evaluated with noninvasive techniques 2~3 times each year and that CAG should be performed once every several years.
1.3 Patients With Angina, Myocardial Infarction, Heart Failure, or Severe Arrhythmia in AdulthoodIt is desirable that patients should be evaluated with noninvasive techniques 3~4 times each year and CAG as appropriate.
1.4 Adult Patients With Coronary Aneurysms With Unknown History of Kawasaki DiseaseBasically, young adults with coronary aneurysms should be followed similarly to patients who had coronary aneurysms in childhood.
2. Treatment 2.1 PharmacotherapyNo evidence has been obtained on the optimal treatment period and dose of oral aspirin for adult patients with coronary aneurysms due to Kawasaki disease.
2.1.1 Patients Without Coronary Aneurysms During ChildhoodPatients without coronary aneurysms during childhood may discontinue antiplatelet treatments such as aspirin.
2.1.2 Asymptomatic Patients With Coronary Aneurysms Persisting From ChildhoodAsymptomatic patients with coronary aneurysms persisting from childhood must, in principle, continue to take aspirin and other appropriate drugs. In addition to improvements of lifestyle such as weight control and smoking cessation, prevention and appropriate treatment of coronary risk factors such as diabetes mellitus, hyperlipidemia, and hyperuricemia are necessary.
2.1.3 Patients With Angina, Myocardial Infarction, Heart Failure, or Severe Arrhythmia in AdulthoodThese patients should be treated in a fashion similar to patients with such conditions associated with etiologies other than Kawasaki disease. In addition to aspirin, antiplatelet drugs, antianginal drugs, diuretics, and other drugs for the treatment of heart failure, or antiarrhythmic drugs may be required. When ischemia is demonstrated on exercise ECG or radionuclide imaging, appropriate coronary intervention should be performed.
2.1.4 Adult Patients With Coronary Aneurysms With Unknown History of Kawasaki DiseaseBasically, young adults with coronary aneurysms should be treated as described in Sections 2.1.2 “Asymptomatic Patients with Coronary Aneurysms Persisting from Childhood” and 2.1.3 “Patients with Angina, Myocardial Infarction, Heart Failure, or Severe Arrhythmia in Adulthood” above.
2.2 Non-PharmacotherapyAdult patients with a history of Kawasaki disease include those who were diagnosed with Kawasaki disease during childhood and underwent elective PCI during school age for the treatment of angina (coronary aneurysm due to Kawasaki disease, stenosis distal or proximal to a coronary aneurysm), and those who were not diagnosed during childhood but need the treatment for coronary artery disease that developed for the first time during adulthood.
Kokura Memorial Hospital in Kyushu, Japan, has conducted a long-term follow-up survey in 39 patients who underwent the first elective PCI for the treatment of a total of 44 cardiovascular lesions due to Kawasaki disease at the median age of 16 years, and were followed for 13 years. During 5 years after treatment, 35% of the patients underwent repeated PCI for restenosis. Most of these patients underwent repeated PCI in the first year after the initial PCI. No patients received repeated PCI from 5~15 years after the initial PCI. No patients experienced the progression or rupture of coronary aneurysms. The long-term outcome of giant aneurysms was favorable as Suda et al reported.250 However, 2 patients (5.6%) had cardiovascular events during adulthood ≥10 years after the initial PCI. These findings indicate that restenosis may occur in some children undergoing PCI at school age during the first year after PCI, but the outcome of repeated PCI is favorable as the lesions are stable with no progression of coronary aneurysms during adulthood. However, these findings also indicate that patients must continue antiplatelet drugs and, for patients with coronary aneurysms, antiplatelet drugs with anticoagulant drugs, and that they tend to develop new coronary artery lesions at an earlier age as compared with people without a history of Kawasaki disease. Patients with a history of Kawasaki disease require more strict medical treatment to prevent arteriosclerosis as compared with people without it.251
It is not rare that patients in whom Kawasaki disease had been overlooked during childhood present with acute coronary syndrome, which causes more severe symptoms than those observed in children with Kawasaki disease, during adulthood due to coronary artery lesions in Kawasaki disease. Among 3,300 patients who were hospitalized in Kokura Memorial Hospital due to AMI during the period from 2000~2011, 55 patients (1.6%) were hospitalized at the age of less than 40 years, and five of the 55 patients (9.1%) had coronary aneurysms specific to coronary sequelae in Kawasaki disease. None of the five patients had been diagnosed with Kawasaki disease. The prevalence of cardiovascular sequelae in Kawasaki disease is consistent with the findings of Daniels et al who reported that coronary sequelae in Kawasaki disease are present in 5% of 261 adults less than 40 years of age who were evaluated by angiography for myocardial ischemia.252 The prevalences of obesity and smokers were significantly lower in these five patients than patients without a history of Kawasaki disease. Many of these five patients did not have known risk factors for arteriosclerosis. PCI was successful in all five patients with a history of Kawasaki disease, but in-hospital mortality was 40%, which was significantly higher than 6% among patients without a history of Kawasaki disease.
3. Guidance on Lifestyle and ExerciseNo evidence has been obtained about coronary risk factors that affect the progression and prognosis of coronary artery lesions in adults with a history of Kawasaki disease. However, because they may have additional risk factors for arteriosclerosis during adulthood, patients with a history of Kawasaki disease should be controlled for known coronary risk factors for arteriosclerosis in adults.
Exercise training may favorably affect body weight, sense of well-being, and the use of drugs for the treatment of coronary artery lesions. Exercise therapy should be prescribed according to the results of risk assessment using exercise testing or other appropriate methods.
4. Pregnancy, Labor and Childbirth 4.1 Pregnancy and LaborPhysicians should assess female patients with a history of Kawasaki disease for whether they may maintain normal cardiac function during pregnancy and labor, the risk of drugs during pregnancy including antithrombotic drugs, optimal methods of delivery, and measures for cardiac accidents that may develop during pregnancy or perinatal period.253 When they reach childbearing age, physicians should assess them for coronary artery lesions, myocardial ischemia or myocardial injury, treat such disorders if present before pregnancy to reduce the risk during delivery, and explain appropriate measures during pregnancy and the risk of childbirth to patients. Pregnant women may undergo cardiac and coronary MRI at week 12 of pregnancy or later.254 Although the number of women who have a history of Kawasaki disease and had given birth is small and evidence is limited, there have been no serious cardiac accidents reported in this population.255,256
4.2 ChildbirthPatients in NYHA Class I without myocardial ischemia may give birth as normal. Women with cardiac dysfunction with a left ventricular ejection fraction (LVEF) of 40~<50% should be monitored carefully during childbirth for the aggravation of cardiac dysfunction due to change in hemodynamics.257 Patients with normal cardiac function without myocardial ischemia should be assessed using the standard obstetric criteria to determine the method of delivery. When patients with cardiac dysfunction undergo vaginal delivery, the use of forceps or vacuum extractor and epidural anesthesia are beneficial as measures to avoid the risk of cardiac overload due to pain during the second stage of labor.258 Caesarian section should be considered for women with signs and symptoms of cardiac ischemia.
4.3 Drugs During Pregnancy and Perinatal PeriodPhysicians should carefully consider the benefits and potential risks of the use of drugs during pregnancy and perinatal period. Drugs used during this period may induce anomaly in the fetus or excessive bleeding during delivery, and may be excreted into the mother’s milk.258
4.3.1 Anticoagulant Drugs and Antiplatelet Drugsa. Aspirin
When women with coronary artery lesions become pregnant and need the treatment with antiplatelet drugs and anticoagulant drugs during pregnancy, they should be treated with aspirin at a small dose (60~81 mg/day) and should be carefully observed. At 34~36 weeks of pregnancy, aspirin should be replaced with continuous intravenous heparin infusion, which should be discontinued 4~6 hours before delivery.258 When aspirin therapy is continued, patients should be hospitalized and discontinue aspirin therapy one week before delivery.256
b. Warfarin
It has been reported that the incidence of warfarin fetal complications is dose-dependent, and that the risk of fetal complications is high in patients receiving warfarin at ≥5 mg/day.259,260 Warfarin should be discontinued during the first 12 weeks of pregnancy, when the major organs systems are developing, and weeks 34~36 of pregnancy and thereafter. For patients in whom discontinuation of warfarin increases the risk of thrombogenesis, physicians should consider subcutaneous administration of heparin.258,261
4.3.2 Other DrugsACE inhibitors should be discontinued during pregnancy, as they are teratogenic. Other drugs should be used only when the benefits overweigh the risk.262,263
4.4 Cardiac AccidentsFor patients with a risk of cardiac accidents during pregnancy, cardiologists and obstetricians should collaborate closely to prepare for emergency measures according to the individual patient conditions.
4.4.1 AMIThe presence of a giant aneurysm is among the biggest factors that influence the development of AMI.251 The outcome of myocardial infarction during pregnancy depends on whether the cardiac accident is managed successfully.264,265 Women at 20 weeks of pregnancy or thereafter may undergo catheter intervention via the radial artery approach. As the supine position may cause inferior vena cava syndrome, physicians should be careful about the body position of the patient.258
4.4.2 ArrhythmiasPatients with myocardial injury, cardiac dysfunction or myocardial ischemia may develop ventricular arrhythmias during pregnancy. Physicians should conduct Holter ECG monitoring in such women, and consider treatment when ventricular tachycardia occurs.258
5. Healthcare System for Adult PatientsAs patients with a history of Kawasaki disease are often examined by general internists whose knowledge on this disease is limited. The following problems exist: (1) internists have only limited knowledge and experience in the management of adults with cardiovascular sequelae in Kawasaki disease, and there is only limited information on this matter that is available for physicians and non-physician healthcare professionals; (2) there is only a limited number of specialists who understand the unique pathology and pathophysiology of cardiovascular sequelae in Kawasaki disease during adulthood; and (3) collaborative activities and institutions to ensure effective management through cardiac rehabilitation or other measures have not been fully developed.
5.1 Understanding of Kawasaki Disease by InternistsGeneral internists are not sufficiently aware of the pathophysiology of Kawasaki disease during the acute phase. It is important to foster specialists in this area. Non-physician healthcare professionals should also be educated on cardiovascular sequelae in Kawasaki disease.
5.2 Collaboration Between Pediatricians and CardiologistsPediatricians and internists must share data on clinical course and laboratory findings obtained from adult patients who had a history of Kawasaki disease. Collaboration between pediatricians and internists especially cardiologists is essential to diagnose, treat and follow patients with cardiovascular sequelae in Kawasaki disease.
5.3 Coronary Aneurysms and Myocardial Infarction in Young Patients and Kawasaki DiseaseAsymptomatic patients with coronary aneurysms due to Kawasaki disease may have ischemic heart disease during adolescence or adulthood. Myocardial infarction is more prevalent than angina among patients with cardiovascular sequelae in Kawasaki disease.266 There is a need for a nationwide archive to register and disclose childhood medical records of patients with a history of Kawasaki disease.
5.4 Comparison With Adult-Type Myocardial InfarctionIn the pathologic evaluation of patients with Kawasaki disease, no severe atherosclerotic lesions are observed although substantial arteriosclerosis is present.267 Remodeling of coronary artery lesions in patients with sequelae in Kawasaki disease may persist for years after onset, and is associated with intimal hyperplasia and neovascularization.42 These findings differ from those in juvenile patients with arteriosclerosis not associated with Kawasaki disease.
Because patients with cardiovascular sequelae in Kawasaki disease may have atherosclerosis and may present with more complex lesions in the future, specialists who are fully aware of such condition must be available.
5.5 Cardiac RehabilitationFew medical institutions are providing cardiac rehabilitation programs for adults with cardiovascular sequelae in Kawasaki disease. This patient population needs appropriate cardiac rehabilitation programs and facilities where physicians and rehabilitation specialists work together.
Table 21 summarizes the pathophysiology, diagnosis, clinical course, treatment, lifestyle management and exercise management for patients with a history of Kawasaki disease by severity.
| Severity | Pathophysiology | Diagnosis/clinical course |
Treatment | Daily life/exercise management* |
|---|---|---|---|---|
| I No dilatation | There is no evidence whether or not a history of Kawasaki disease is a factor associated with arteriosclerotic lesion. |
Follow up patients for 5 years. Evaluate at 30 days, 60 days, 6 months, 1 year, and 5 year after onset with ECG, echocardiography, and, if necessary, chest X-ray. It is desirable that patients be evaluated with exercise ECG at the final examination. |
Basically, no treatment is required during the remote phase. Patients with no coronary aneurysms after the acute phase may discontinue antiplatelet drugs such as aspirin. |
No restriction is placed on daily life or exercise. Management Table: “No management needed” for children ≥5 years after onset. Consult with parents (or patients) to determine further management. Lifetime prevention of lifestyle-related diseases is important. Junior and senior high school students should be educated on lifestyle-related diseases (e.g., blood lipid measurement, education on smoking cessation, and prevention of obesity). |
| II Transient dilatation during the acute phase |
During the acute phase, histopathologically vasculitis develops in the outer layer of the tunica media and then expands to the intima in coronary arteries. Echocardiography reveals diffuse dilatation of coronary arteries, but these changes subside within 30 days after onset. |
|||
| III Regression | In many cases regression may occur 1∼2 years after onset, particularly in small or medium aneurysms. In the segment with regression, decrease in coronary diastolic function, abnormal function of vascular endothelium, and substantial intimal hyperplasia have been reported. Also, it is reported that the occurrence of acute coronary syndrome in adults with a history of Kawasaki disease in whom coronary artery lesions were considered regressed after the acute phase of the disease. |
Basically, follow patients annually with ECG, echocardiography, and chest X-ray up to entry into elementary school (age of 6, 7), and then with the same methods and exercise ECG in 4th grade (age 9, 10), at entry into junior high school (age 12, 13), and entry into senior high school (age 15, 16). Follow patients who had coronary aneurysms with a large internal diameter during the acute phase with an appropriate combination of imaging techniques.** |
Continue antiplatelet drugs such as aspirin whenever necessary. |
No restriction is placed on daily life or exercise. Follow the recommendations for Categories I and II. |
| IV Remaining coronary aneurysms |
Aneurysms remaining during the convalescent phase or later are considered sequelae. Histopathologically, progression of inflammation leads to rupture of the internal elastic band, causing panangiitis. The internal and external elastic bands are broken into fragments and ruptured by arterial pressure to form aneurysms. Patients with giant aneurysms must be observed carefully for myocardial ischemia, because in such patients myocardial ischemia may develop even if no significant stenotic lesions are present. |
Patients must be followed with exercise ECG and an appropriate combination of imaging techniques.** It is desirable that patients who had coronary aneurysms with a large internal diameter during the acute phase be evaluated with stress myocardial scintigraphy every 2∼5 years, since they may have myocardial ischemia. |
Continue treatment with antiplatelet drugs such as aspirin. Anticoagulant therapy may be needed in patients with giant aneurysms or thrombi in coronary aneurysms. CABG may be indicated for patients with giant aneurysms not accompanied by signifcant stenotic lesions when myocardial ischemia has occurred. |
No restriction is placed on daily life or exercise. Management Table: “Eallowed”. Patients with giant aneurysms: Instruct as “D-prohibited” in the Management Table. In the second year after onset or later, “E-prohibited” is possible when no changes are noted. |
| V-a Coronary stenotic lesions (no findings of ischemia) |
Thrombotic occlusion of medium or giant aneurysms may develop during the relatively early stage after onset. Sudden death may occur, though two-thirds patients with occlusion are asymptomatic. Patients often show improvement of myocardial ischemia due to the development of recanalized vessels and collateral flow after occlusion. Development/ progression of regional stenosis during the remote phase is more prevalent in the left coronary artery than in the right coronary artery. The segments with greatest prevalence are the proximal segment or the main trunk of the left anterior descending artery. The risk of progression to stenosis/occlusion is higher in larger aneurysms. Stenosis may develop during long-term follow up. |
Patients must be followed for life, and physicians must design the tailor-made management plan for individual patients. Follow-up examination must include exercise ECG and an appropriate combination of imaging techniques.** Although schedule may differ among individuals, patients are generally evaluated every 3∼6 months. |
Continue treatment with antiplatelet drugs such as aspirin. Use calcium channel blockers, nitrates, β-blockers, ACE inhibitors, and/or angiotensin receptor II blockers to prevent ischemic attacks and treat heart failure. |
No restriction is placed on daily life or exercise. School Activity Management Table: “E-allowed” for patients other than those with giant aneurysms. Explain the importance of pharmacotherapy and ensure adherence, as well as symptoms which may occur and actions to be taken when ischemia develops. Patients must be followed at least annually until the stenotic lesions have improved. |
| V-b Coronary stenotic lesions (with findings of ischemia) |
Follow the instructions for pharmacotherapy in Category V-a. Consider CABG or appropriate PCI technique when exercise ECG or stress myocardial scintigraphy reveals ischemia. |
Exercise shuld be restricted. Categorize in “D” or higher category based on patient condition. School sport club activities should be “prohibited”. Select the most appropriate category from “A” to “D” on the basis of findings of exercise testing and evaluation of severity of myocardial ischemia. Educate patients well about the importance of pharmacotherapy. |
**Imaging techniques include echocardiography (including stress echocardiography), stress myocardial scintigraphy, selective CAG, IVUS, MRI, MRA, and MDCT.
ACE, angiotensin converting enzyme; CABG, coronary artery bypass grafting; CAG, coronary angiography; ECG, electrocardiography; IVUS, intravascular ultrasound; MDCT, multi- detector row computed tomography; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; PCI, percutaneous coronary intervention.
Chair:
• Shunichi Ogawa, Department of Pediatrics, Nippon Medical School
Members:
• Mamoru Ayusawa, Department of Pediatrics, Nihon University School of Medicine
• Ryuji Fukazawa, Department of Pediatrics, Nippon Medical School
• Kenji Hamaoka, Department of Pediatric Cardiology and Nephrology, Graduate School of Medical Science, Kyoto Prefectural University of Medicine
• Masahiro Ishii, Department of Pediatrics, Kitasato University
• Kazuhiko Nishigaki, Second Department of Internal Medicine, Gifu University
• Hirotarou Ogino, Department of Pediatrics, Kansai Medical University
• Tsutomu Saji, Department of Pediatrics, Toho University Omori Medical Center
Collaborators:
• Hiroshi Kamiyama, Department of Pediatrics, Nihon University School of Medicine
• Masami Ochi, Department of Cardiovascular Surgery, Nippon Medical School, Graduate School of Medicine
• Kei Takahashi, Department of Pathology, Toho University School of Medicine, Ohashi Hospital
• Etsuko Tsuda, Departments of Pediatric Cardiology, National Cerebral and Cardiovascular Center
• Hiroyoshi Yokoi, Department of Cardiology, Kokura Memorial Hospital
Independent Assessment Committee:
• Takashi Akasaka, Department of Cardiovascular Medicine, Wakayama Medical University
• Soichiro Kitamura, Sakai City Hospital
• Yoshikazu Nakamura, Department of Public Health, Jichi Medical University
• Toshio Nakanishi, Department of Pediatric Cardiology, Tokyo Women’s Medical University
• Tomoyoshi Sonobe, Department of Pediatrics, Japanese Red Cross Medical Center
(The affiliations of the members are as of August 2013)
| Author | Employer/ leadership position (private company) |
Stakeholder | Patent royalty |
Honorarium | Payment for manuscripts |
Research grant |
Scholarship (educational) grant/endowed chair |
Other rewards |
Potential COI of the marital partner, first-degree family members, or those who share income and property. |
|---|---|---|---|---|---|---|---|---|---|
| Members: Kazuhiko Nishigaki |
Shionogi Boehringer Ingelheim Japan Mochida Pharmaceutical |
||||||||
| Members: Masami Ochi |
St. Jude Medical Japan Senko Medical Instrument Manufacturing Edwards Lifesciences Corporation |
Companies are listed only by name. The following members have no COI to disclose.
Members with no COI to disclose.
Chair: Shunichi Ogawa, None
Members: Mamoru Ayusawa, None
Members: Masahiro Ishii, None
Members: Hirotarou Ogino, None
Members: Tsutomu Saji, None
Members: Kenji Hamaoka, None
Members: Ryuji Fukazawa, None
Collaborators: Hiroshi Kamiyama, None
Collaborators: Kei Takahashi, None
Collaborators: Etsuko Tsuda, None
Collaborators: Hiroyoshi Yokoi, None