Abstract
Background:
Although the aged population is increasing in developed countries, clinical evidence on super-elderly heart failure (HF) patients is scarce. This study determined the characteristics and outcomes of Japanese hospitalized super-elderly HF patients (aged ≥90 years) using a nationwide inpatient database.
Methods and Results:
A comprehensive analysis was performed of 447,818 HF patients in the Diagnosis Procedure Combination database who were hospitalized and discharged between January 2010 and March 2018. Among the study population, 243,028 patients (54.3%) were aged ≥80 years and 64,628 patients (14.4%) were aged ≥90 years. The percentage of elderly patients increased over time. Elderly patients were more likely to be female and had a higher New York Heart Association functional class at admission. Invasive and advanced procedures were rarely performed, whereas infectious complications were more common in patients with older age. Length of hospital stay and in-hospital mortality increased with age. Multivariable logistic regression analysis fitted with a generalized estimating equation showed higher in-hospital mortality in patients aged ≥80 and ≥90 years (odds ratios 1.99 and 3.23, respectively) compared with those aged <80 years.
Conclusions:
The number of hospitalized super-elderly HF patients has increased, and these patients are associated with worse clinical outcomes. The results of this study may be useful in establishing an optimal management strategy for super-elderly HF patients in the era of HF pandemic.
An aging society and the associated increases in cardiovascular diseases are common healthcare concerns in developed countries.1,2
Because aging is associated with heart failure (HF),3–5
the number of elderly patients with HF has increased in developed countries. Most previous studies on elderly HF patients defined “elderly” patients as those ≥80 years of age.6–8
However, the number of patients aged >90 years is also increasing in super-aging societies, and clinical evidence for super-elderly patients is important. Although earlier studies already showed that the percentage of elderly HF patients was increasing9
and older age was associated with adverse clinical outcomes in patients with HF,6–8,10,11
clinical data on the prevalence of super-elderly HF patients and the clinical outcomes of super-elderly HF patients are scarce. In this study we explored the outcomes of elderly patients hospitalized for worsened HF, particularly super-elderly patients aged ≥90 years, using a nationwide inpatient database. Considering the rapid increase in the proportion of the aged population in developed countries, the critical epidemiological condition so called “HF pandemic” is approaching; thus, presenting real-world data on super-elderly HF patients is critical at this time.
Methods
Study Design and Data Source
The Diagnosis Procedure Combination (DPC) database is a nationwide inpatient database in Japan.12,13
Briefly, the DPC database includes administrative claims and clinical data for approximately 7 million hospitalized patients per year from approximately 1,000 participating hospitals. The main diagnosis, comorbidities at admission, and complications during hospitalization are recorded using the International Classification of Disease and Related Health Problems 10th Revision (ICD-10) codes. In this study, we reviewed data for 466,921 patients aged ≥20 years with New York Heart Association (NYHA) Class ≥II, admitted and discharged between January 2010 and March 2018 with the main discharge diagnosis of HF defined by ICD-10 codes I50.0, I50.1, and I50.9. Patients with a length of hospital stay ≤2 days (n=15,270) and those who underwent major procedures under general anesthesia (n=3,833) were excluded from the study. Thus, the final number of patients analyzed in this study was 447,818.
Ethical Considerations
This study was approved by the Institutional Review Board of the University of Tokyo [3501-(3)]. This study was conducted in accordance with the Declaration of Helsinki. Because of the anonymous nature of the database, the requirement for informed consent was waived.
Statistical Analysis
Categorical and continuous data are presented as numbers with percentages and as the median with interquartile range (IQR). Categorical and continuous variables were compared using Chi-squared tests and 1-way analysis of variance (ANOVA). The association of age category with in-hospital mortality was evaluated using a multivariable logistic regression analysis with adjustment for other covariates, while also adjusting for within-hospital clustering using a generalized estimating equation.14
Subgroup analyses were conducted according to sex and geographic region. For analysis on geographic region, the study population was divided into 7 regions, namely the Northern, Central, Kanto, Tokyo, Kinki, Chugoku-Shikoku, and Kyushu regions, according to 47 prefectures in Japan. Two-sided P<0.05 was considered significant. Statistical analyses were performed using SPSS version 25 (IBM Corp., Armonk, NY, USA) and STATA (StataCorp, College Station, TX, USA).
Results
Trend of Age Distribution
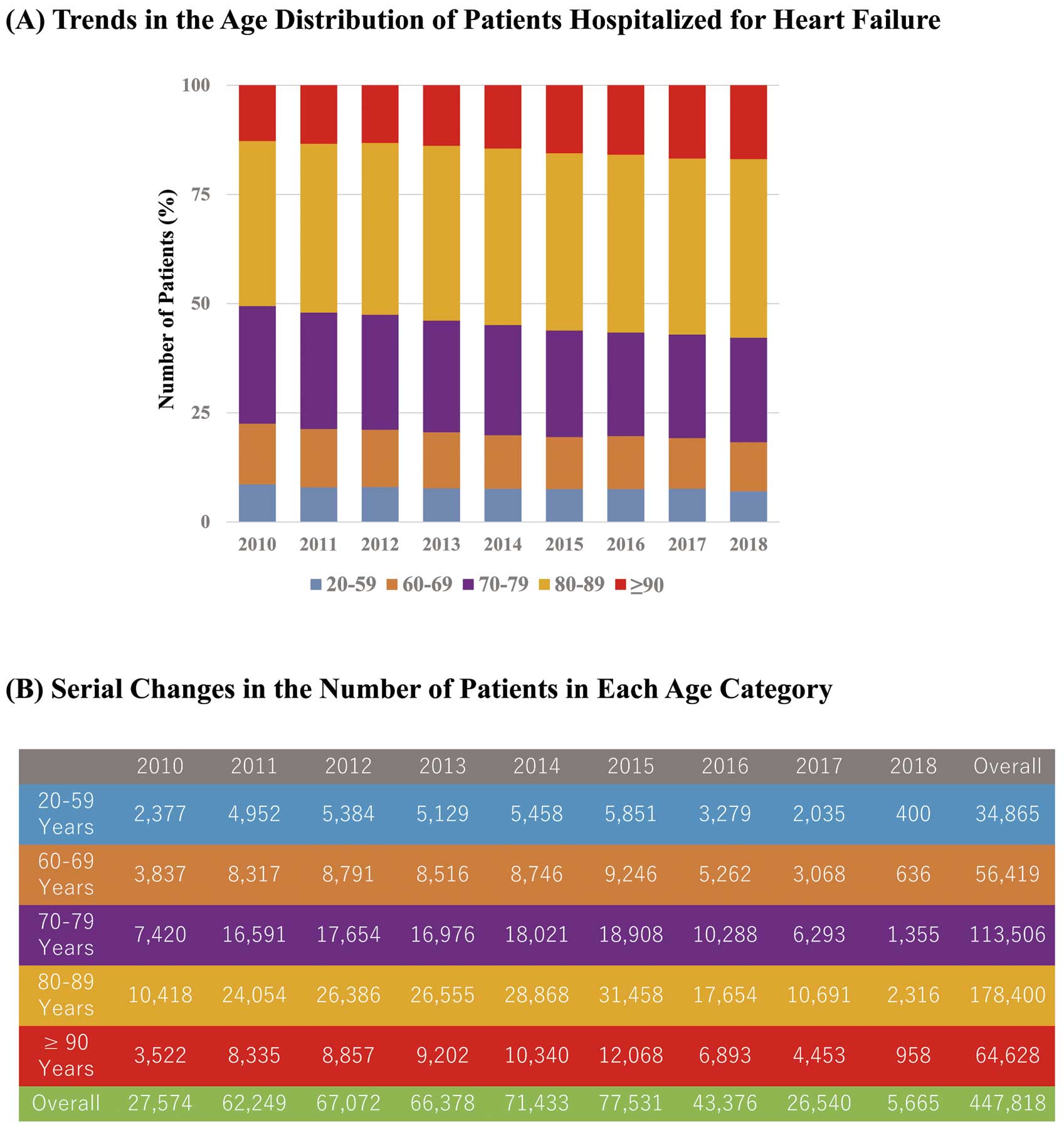
The percentage of HF patients aged ≥80 and ≥90 years increased from 50.6% and 12.8%, respectively, in 2010 to 57.8% and 16.9%, respectively, in 2018 (Figure 1).
Characteristics of the Study Population
The characteristics of the study population are summarized in
Table 1. In total, 243,028 patients (54.3%) were aged ≥80 years and 64,628 patients (14.4%) were aged ≥90 years. Elderly patients were more likely to be female. Body mass index was lower in elderly patients. There were significant differences in prevalence of comorbidities, such as hypertension, diabetes, and chronic renal dysfunction among age categories. The percentage of patients categorized as NYHA Class IV at admission increased with age. Information on medications administered within 2 days after admission was also collected. Furosemide was more frequently used in patients aged ≥80 and ≥90 years than in those aged <80 years. Conversely, other medications used for the treatment of HF were less frequently administered in patients aged ≥80 and ≥90 years.
Table 1.
Characteristics of the Study Population
| |
Age (years) |
P-value |
| <80 (n=204,790) |
80–89 (n=178,400) |
≥90 (n=64,628) |
| Age (years) |
71 [13] |
84 [5] |
92 [4] |
<0.001 |
| Age group (years) |
| 20–59 |
34,865 (17.0) |
– |
– |
|
| 60–69 |
56,419 (27.5) |
– |
– |
|
| 70–79 |
113,506 (55.4) |
– |
– |
|
| 80–89 |
– |
178,400 (100.0) |
– |
|
| ≥90 |
– |
– |
64,628 (100.0) |
|
| Male sex |
135,663 (66.2) |
82,908 (46.5) |
19,621 (30.4) |
<0.001 |
| BMIA (kg/m2) |
23.2 [5.7] |
21.5 [4.9] |
20.4 [4.7] |
<0.001 |
| Hypertension |
139,459 (68.1) |
119,622 (67.1) |
41,994 (65.0) |
<0.001 |
| Diabetes mellitus |
81,184 (39.6) |
49,046 (27.5) |
10,789 (16.7) |
<0.001 |
| Chronic renal failure |
29,633 (14.5) |
27,051 (15.2) |
8,819 (13.6) |
<0.001 |
| Chronic liver disease |
10,103 (4.9) |
6,070 (3.4) |
1,344 (2.1) |
<0.001 |
| Chronic respiratory disease |
22,129 (10.8) |
21,970 (12.3) |
6,642 (10.3) |
<0.001 |
| Atrial fibrillation |
77,727 (38.0) |
74,370 (41.7) |
23,590 (36.5) |
<0.001 |
| Myocardial infarction |
6,168 (3.0) |
4,731 (2.7) |
1,618 (2.5) |
<0.001 |
| Shock |
4,418 (2.2) |
3,235 (1.8) |
1,112 (1.7) |
<0.001 |
| VT/VF |
13,908 (6.8) |
5,424 (3.0) |
957 (1.5) |
<0.001 |
| NYHA functional class |
|
|
|
<0.001 |
| Class II |
63,002 (30.8) |
50,883 (28.5) |
15,930 (24.6) |
|
| Class III |
77,383 (37.8) |
69,353 (38.9) |
24,703 (38.2) |
|
| Class IV |
64,405 (31.4) |
58,164 (32.6) |
23,995 (37.1) |
|
| Educational institute |
164,285 (80.2) |
141,991 (79.6) |
51,257 (79.3) |
<0.001 |
| Medications within 2 days after admission |
| Orally administered |
| β-blocker |
78,959 (38.6) |
54,843 (30.7) |
14,584 (22.6) |
<0.001 |
| RAS inhibitor |
83,754 (40.9) |
63,220 (35.4) |
19,384 (30.0) |
<0.001 |
| ACEI |
38,071 (18.6) |
25,622 (14.4) |
8,019 (12.4) |
<0.001 |
| ARB |
47,403 (23.1) |
38,804 (21.8) |
11,659 (18.0) |
<0.001 |
| MCR antagonist |
71,847 (35.1) |
55,015 (30.8) |
18,753 (29.0) |
<0.001 |
| Intravenously administered |
| Inotropic agent |
40,501 (19.8) |
28,807 (16.1) |
8,928 (13.8) |
<0.001 |
| Nitrate |
46,936 (22.9) |
34,723 (19.5) |
11,906 (18.4) |
<0.001 |
| Furosemide |
132,567 (64.7) |
124,149 (69.6) |
47,956 (74.2) |
<0.001 |
Unless indicated otherwise, data are given as the median [interquartile range] or n (%). AThere were missing values for BMI (n=39,590). ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BMI, body mass index; MCR, mineralocorticoid receptor; NYHA, New York Heart Association; RAS, renin-angiotensin system; VT/VF, ventricular tachycardia/ventricular fibrillation.
Table 2
summarizes the procedures and outcomes for the study population. Invasive and advanced procedures, including implantable cardioverter defibrillator, cardiac resynchronization therapy, respiratory support, intubation, hemodialysis, intra-aortic balloon pumping, extracorporeal membrane oxygenation, and the use of inotropes, were rarely performed in patients aged ≥80 and ≥90 years. Infectious complications were frequently observed in patients aged ≥80 and ≥90 years. Patients with older age had a longer length of hospital stay and higher in-hospital mortality. Discharge disposition is also listed in
Table 2. Most patients aged <80 years were discharged to their homes. Conversely, elderly patients were more likely to be transferred to nursing homes.
Table 2.
Procedures and Outcomes for the Study Population
| |
Age (years) |
P-value |
| <80 (n=204,790) |
80–89 (n=178,400) |
≥90 (n=64,628) |
| Procedures |
| ICD |
706 (0.3) |
113 (0.1) |
2 (0.0) |
<0.001 |
| CRT |
3,610 (1.8) |
927 (0.5) |
40 (0.1) |
<0.001 |
| Respiratory support |
37,555 (18.3) |
26,010 (14.6) |
7,089 (11.0) |
<0.001 |
| Intubation |
7,764 (3.8) |
4,008 (2.2) |
592 (0.9) |
<0.001 |
| Hemodialysis |
8,298 (4.1) |
2,844 (1.6) |
243 (0.4) |
<0.001 |
| IABP |
2,295 (1.1) |
799 (0.4) |
81 (0.1) |
<0.001 |
| ECMO |
361 (0.2) |
84 (0.0) |
5 (0.0) |
<0.001 |
| Inotropic use |
80,687 (39.4) |
66,397 (37.2) |
22,625 (35.0) |
<0.001 |
| Outcomes |
| Pneumonia |
3,966 (1.9) |
5,645 (3.2) |
2,637 (4.1) |
<0.001 |
| Urinary tract infection |
1,407 (0.7) |
2,530 (1.4) |
1,346 (2.1) |
<0.001 |
| Sepsis |
994 (0.5) |
1,077 (0.6) |
440 (0.7) |
<0.001 |
| Deep vein thrombus |
596 (0.3) |
460 (0.3) |
145 (0.2) |
0.009 |
| Pulmonary embolism |
163 (0.1) |
163 (0.1) |
35 (0.1) |
0.017 |
| LOS (days) |
16 [15] |
18 [17] |
18 [18] |
<0.001 |
| In-hospital death |
8,056 (3.9) |
14,280 (8.0) |
8,486 (13.1) |
<0.001 |
Discharge disposition (excluding patients
who died in hospital) |
|
|
|
<0.001 |
| Home |
180,482 (91.7) |
134,215 (81.8) |
39,043 (69.5) |
|
| Nursing home |
2,217 (1.1) |
9,469 (5.8) |
8,000 (14.2) |
|
| Other hospital |
13,305 (6.8) |
19,703 (12.0) |
8,722 (15.5) |
|
| Other or unknown |
730 (0.4) |
733 (0.4) |
377 (0.7) |
|
Unless indicated otherwise, data are given as the median [interquartile range] or n (%). CRT, cardiac resynchronization therapy; ECMO, extracorporeal membrane oxygenation; ICD, implantable cardioverter defibrillator; IABP, intra-aortic balloon pump; LOS, length of hospital stay.
The multivariable logistic regression analysis fitted with a generalized estimating equation for in-hospital mortality showed that in-hospital mortality was higher in patients aged 80–89 and those aged ≥90 years than in those aged <80 years (Table 3).
Table 3.
Results of the Multivariable Logistic Regression Fitted With a Generalized Estimating Equation for In-Hospital Mortality
| |
OR |
95% CI |
P-value |
| Age (years) |
| <80 |
Ref. |
|
|
| 80–89 |
1.99 |
1.92–2.05 |
<0.001 |
| ≥90 |
3.23 |
3.09–3.38 |
<0.001 |
| Sex |
| Female |
Ref. |
|
|
| Male |
1.10 |
1.07–1.13 |
<0.001 |
| BMI (kg/m2) |
0.94 |
0.94–0.95 |
<0.001 |
| Hypertension |
0.51 |
0.49–0.53 |
<0.001 |
| Diabetes |
1.03 |
1.00–1.06 |
0.027 |
| Chronic renal failure |
1.65 |
1.59–1.71 |
<0.001 |
| Chronic liver disease |
1.41 |
1.33–1.50 |
<0.001 |
| Chronic respiratory disease |
0.99 |
0.95–1.03 |
0.525 |
| Atrial fibrillation |
0.91 |
0.89–0.94 |
<0.001 |
| Myocardial infarction |
1.50 |
1.40–1.61 |
<0.001 |
| Shock |
3.24 |
2.93–3.59 |
<0.001 |
| VT/VF |
1.83 |
1.72–1.94 |
<0.001 |
| NYHA functional class |
| Class II |
Ref. |
|
|
| Class III |
1.77 |
1.67–1.87 |
<0.001 |
| Class IV |
3.89 |
3.62–4.18 |
<0.001 |
| Educational institute |
0.81 |
0.78–0.85 |
<0.001 |
| Drugs administered within 2 days |
| β-blocker |
0.92 |
0.90–0.95 |
<0.001 |
| RAS inhibitor |
0.62 |
0.59–0.64 |
<0.001 |
| MCR antagonist |
0.81 |
0.79–0.84 |
<0.001 |
| Intravenous inotropic agent |
2.27 |
2.18–2.37 |
<0.001 |
| Intravenous nitrate |
0.63 |
0.60–0.66 |
<0.001 |
| Intravenous furosemide |
1.12 |
1.08–1.16 |
<0.001 |
CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.
The results of the subgroup analyses are shown in
Figure 2. The proportion of elderly patients was higher among women than men (P<0.001;
Figure 2A). The age distribution of HF patients differed among geographic regions (P<0.001;
Figure 2B).
Discussion
The increase in the proportion of super-elderly patients with HF is associated with the rapid increase in the aging society. The percentage of the population aged ≥75 years in Japan increased from 8.6% in 2010 to 14.2% in 2018. It is estimated that there are approximately 1 million HF patients in Japan, and the number of patients with HF is predicted to increase and reach 1.3 million by 2030 in association with an aging society.15
Therefore, further increases in super-elderly patients hospitalized for HF are expected.
Similar trends have been observed in other countries. The mean (±SD) age of HF patients in The Swedish Heart Failure Registry was 76±12 years, and 37% of patients were aged ≥80 years.16
Similarly, the National Heart Failure Audit for England and Wales 2008–09 showed that median age of patients hospitalized for HF was 78 years, with more than half the patients aged ≥75 years.17
Therefore, an increase in elderly patients with HF is a critical issue not only in Japan, but also in most developed countries.
The findings of this study have clinical implications. Despite the rapid increase in the aged population in developed countries, limited information is available regarding the outcomes of super-elderly HF patients. The present study is the first to focus on super-elderly (age ≥90 years) HF patients using a nationwide large-scale database. Most previous studies defined “elderly” HF patients as those aged ≥80 years.6–8
However, considering that the median age of the present study population was 81 years, and that more than half the patients were aged ≥80 years, they could not be considered as specific subsets. In real-world clinical practice, HF patients aged ≥90 years are not rare; thus, revealing the presentations and outcomes of HF patients aged ≥90 years provides important information in the era of a super-aging society.
Subgroup analysis revealed that elderly patients were more likely to be female, and this finding is in accordance with findings from previous studies.7,8,11
Further, there was a significant geographic difference in the age distribution of HF patients. Geographic differences in the age of patients with HF among countries has been reported previously,18
and the results of the present study showed that there can also be a domestic regional difference in the age distribution of patients with HF.
Elderly patients had longer length of hospital stay than patients aged <80 years. However, the difference in length of hospital stay among the 3 groups was clinically not so large. It is assumed that the increase in elderly patients would contribute to longer hospital stays and result in an HF pandemic in acute care hospitals. However, based on the results of the present study, we cannot simply associate the longer hospital stay of HF patients with increased numbers of elderly HF patients. The length of hospital stay of patients with HF is longer in Japan than in other countries, and it is recognized as an important issue of the clinical setting in Japan.19,20
Conversely, the 30-day HF readmission rate is known to be lower in Japan (5%) than in the US (25%).21
There appears to be a trade-off between a longer hospital stay and hospital readmission. Both long hospital stays and repeated readmissions can be a significant burden for older patients. Well-balanced in-hospital management is particularly required for patients of older age.
In accordance with previous studies,6–8,10,11
in-hospital mortality in the present study was higher for patients of older age. Medications other than furosemide were less frequently used in patients of older age. Further, invasive procedures were less frequently performed in elderly HF patients. Avoiding intensive medical treatment and invasive procedures in elderly patients is sometimes reasonable. In addition, the latest guidelines indicate that several promising treatments are not indicated for patients with limited life expectancy.22,23
Therefore, we often hesitate to introduce invasive therapeutic options for patients of older age and with comorbidities in the real-world clinical setting. However, optimal indications for therapeutic options, including advanced procedures, in super-elderly patients need to be established because this subset of patients is expected to increase further. Given that infectious complications were more frequently observed in patients of older age, the importance of comprehensive management should also be noted. Simultaneously, palliative care is important for patients of older age.24,25
Although clinical evidence of palliative care for hospitalized HF patients is not yet established,26,27
Sidebottom et al reported that inpatient consultation by a palliative care team provided significant improvements in all patient-reported outcomes, including quality of life, for patients hospitalized for acute HF.26
Further, Rogers et al reported that an interdisciplinary palliative care intervention was associated with greater benefits in quality of life, anxiety, depression, and spiritual well-being than usual care alone in patients with advanced HF.28
We do believe that palliative care, including advance care planning, is required for patients of older age and with limited therapeutic options.
Regarding discharge disposition, more than 90% of patients aged <80 years were discharged to their homes, compared with <70% of patients aged ≥90 years; 14% of patients aged ≥90 years were transferred to nursing homes. These results suggest that social support and regional medical networks would be also important for elderly patients with HF.29
A multidisciplinary team approach is particularly required for super-elderly patients who have multiple comorbidities and complicated backgrounds.
This study has several limitations. Although we performed multivariable analysis using a generalized estimating equation, there could be residual bias. The validity of the diagnoses and procedures in the database we used has been reported to be high.30
However, recorded diagnoses are generally considered less well validated because of the nature of administrative data and retrospective studies. The DPC database lacked information on several factors that were potentially associated with outcomes, including blood pressure, HF etiology, and left ventricular ejection fraction.
Conclusions
Analysis of a nationwide database showed that the number of elderly patients hospitalized for HF, particularly super-elderly patients aged ≥90 years, was increasing and that in-hospital mortality was higher for these patients. An evidence-based approach for super-elderly HF patients should be established in the era of HF pandemic.
Sources of Funding
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (19AA2007 and H30-Policy-Designated-004) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (17H04141).
Disclosures
H. Kaneko and K.F. have received research funding and scholarship funds from Medtronic Japan, Abbott Medical Japan, Boston Scientific Japan, and Fukuda Denshi, Central Tokyo. I.K. is a member of
Circulation Reports
’ Editorial Team.
IRB Information
This study was approved by the Institutional Review Board of The University of Tokyo [3501-(3)].
References
- 1.
Sidney S, Go AS, Jaffe MG, Solomon MD, Ambrosy AP, Rana JS. Association between aging of the US population and heart disease mortality from 2011 to 2017. JAMA Cardiol 2019; 4: 1280–1286.
- 2.
Kaneko H, Morita H, Komuro I. Beautiful harmony of the Japanese precious healthcare legacies for the new imperial era. Circ J 2020; 84: 371–373.
- 3.
Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev 2000; 5: 167–173.
- 4.
Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, et al. Lifetime risk for developing congestive heart failure: The Framingham Heart Study. Circulation 2002; 106: 3068–3072.
- 5.
Mosterd A, Cost B, Hoes AW, de Bruijne MC, Deckers JW, Hofman A, et al. The prognosis of heart failure in the general population: The Rotterdam Study. Eur Heart J 2001; 22: 1318–1327.
- 6.
Komajda M, Hanon O, Hochadel M, Follath F, Swedberg K, Gitt A, et al. Management of octogenarians hospitalized for heart failure in Euro Heart Failure Survey I. Eur Heart J 2007; 28: 1310–1318.
- 7.
Komajda M, Hanon O, Hochadel M, Lopez-Sendon JL, Follath F, Ponikowski P, et al. Contemporary management of octogenarians hospitalized for heart failure in Europe: Euro Heart Failure Survey II. Eur Heart J 2009; 30: 478–486.
- 8.
Hamaguchi S, Kinugawa S, Goto D, Tsuchihashi-Makaya M, Yokota T, Yamada S, et al. Predictors of long-term adverse outcomes in elderly patients over 80 years hospitalized with heart failure: A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J 2011; 75: 2403–2410.
- 9.
Shimokawa H, Miura M, Nochioka K, Sakata Y. Heart failure as a general pandemic in Asia. Eur J Heart Fail 2015; 17: 884–892.
- 10.
Mahjoub H, Rusinaru D, Souliere V, Durier C, Peltier M, Tribouilloy C. Long-term survival in patients older than 80 years hospitalised for heart failure: A 5-year prospective study. Eur J Heart Fail 2008; 10: 78–84.
- 11.
Mizuno M, Kajimoto K, Sato N, Yumino D, Minami Y, Murai K, et al. Clinical profile, management, and mortality in very-elderly patients hospitalized with acute decompensated heart failure: An analysis from the ATTEND registry. Eur J Intern Med 2016; 27: 80–85.
- 12.
Yagi M, Yasunaga H, Matsui H, Morita K, Fushimi K, Fujimoto M, et al. Impact of rehabilitation on outcomes in patients with ischemic stroke: A nationwide retrospective cohort study in Japan. Stroke 2017; 48: 740–746.
- 13.
Shigemi D, Isogai S, Uda K, Aso S, Matsui H, Fushimi K, et al. Association between rehabilitation during hospitalization and perinatal outcomes among pregnant women with threatened preterm birth. J Matern Fetal Neonatal Med, doi:10.1080/14767058.2019.1623197.
- 14.
Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: An orientation. Am J Epidemiol 2003; 157: 364–375.
- 15.
Okura Y, Ramadan MM, Ohno Y, Mitsuma W, Tanaka K, Ito M, et al. Impending epidemic: Future projection of heart failure in Japan to the year 2055. Circ J 2008; 72: 489–491.
- 16.
Chen X, Savarese G, Dahlstrom U, Lund LH, Fu M. Age-dependent differences in clinical phenotype and prognosis in heart failure with mid-range ejection compared with heart failure with reduced or preserved ejection fraction. Clin Res Cardiol 2019; 108: 1394–1405.
- 17.
Cleland JG, McDonagh T, Rigby AS, Yassin A, Whittaker T, Dargie HJ, et al. The National Heart Failure Audit for England and Wales 2008–2009. Heart 2011; 97: 876–886.
- 18.
Sani MU, Cotter G, Davison BA, Mayosi BM, Damasceno A, Edwards C, et al. Symptoms and signs of heart failure at admission and discharge and outcomes in the Sub-Saharan Acute Heart Failure (THESUS-HF) Registry. J Card Fail 2017; 23: 739–742.
- 19.
Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, et al. The global health and economic burden of hospitalizations for heart failure: Lessons learned from hospitalized heart failure registries. J Am Coll Cardiol 2014; 63: 1123–1133.
- 20.
Shiraishi Y, Kohsaka S, Sato N, Takano T, Kitai T, Yoshikawa T, et al. 9-year trend in the management of acute heart failure in Japan: A report from the National Consortium of Acute Heart Failure Registries. J Am Heart Assoc 2018; 7: e008687.
- 21.
Krumholz HM, Hsieh A, Dreyer RP, Welsh J, Desai NR, Dharmarajan K. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS One 2016; 11: e0160492.
- 22.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200.
- 23.
Otto CM, Kumbhani DJ, Alexander KP, Calhoon JH, Desai MY, Kaul S, et al. 2017 ACC expert consensus decision pathway for transcatheter aortic valve replacement in the management of adults with aortic stenosis: A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2017; 69: 1313–1346.
- 24.
Kavalieratos D, Gelfman LP, Tycon LE, Riegel B, Bekelman DB, Ikejiani DZ, et al. Palliative care in heart failure: Rationale, evidence, and future priorities. J Am Coll Cardiol 2017; 70: 1919–1930.
- 25.
Hauser J. Communication in heart failure and palliative care. Heart Fail Rev 2017; 22: 535–542.
- 26.
Sidebottom AC, Jorgenson A, Richards H, Kirven J, Sillah A. Inpatient palliative care for patients with acute heart failure: Outcomes from a randomized trial. J Palliat Med 2015; 18: 134–142.
- 27.
Hopp FP, Zalenski RJ, Waselewsky D, Burn J, Camp J, Welch RD, et al. Results of a hospital-based palliative care intervention for patients with an acute exacerbation of chronic heart failure. J Card Fail 2016; 22: 1033–1036.
- 28.
Rogers JG, Patel CB, Mentz RJ, Granger BB, Steinhauser KE, Fiuzat M, et al. Palliative care in heart failure: The PAL-HF randomized, controlled clinical trial. J Am Coll Cardiol 2017; 70: 331–341.
- 29.
Komuro I, Kaneko H, Morita H, Isobe M, Nakayama H, Minematsu K, et al. Nationwide actions against heart failure pandemic in Japan: What should we do from academia? Circ J 2019; 83: 1819–1821.
- 30.
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol 2017; 27: 476–482.