Abstract
Parathyroid carcinoma (PC) is a rare condition with propensity to relapse. The purpose of this study was to evaluate the sonographic findings of locoregional recurrences of parathyroid carcinoma, in order to facilitate diagnosis of this condition using ultrasound (US). This was a retrospective observational study including 21 patients confirmed with pathologically confirmed locoregional recurrence of parathyroid carcinoma. All patients had undergone preoperative US examination at a tertiary center. The imaging, clinical and laboratory data of each case were collected. Sonographic appearance of the largest lesion at each recurrence was evaluated by two experienced radiologists according to a pre-agreed protocol. Overall, 29 relapses occurred in 21 patients. The median age of the patients was 45 years (range 24–71 years). The median size of the largest recurrent lesion at each relapse was 1.8 cm (range 0.8–3.8 cm). Ultrasound images showed hypoechoic solid nodules in 28 relapses (96.6%), inhomogeneous echo-texture in 28 relapses (96.6%), intralesional echogenic septa-like structures in 21 relapses (72.4%), intralesional cystic change in two relapses (6.9%), infiltrative or blurred boundary in 20 relapses (69.0%), irregular shape in 22 relapses (75.9%), marked vascularization on color Doppler imaging in 19 relapses (65.5%), multiple lesions in 26 relapses (89.7%), contralateral recurrence in 3 relapses (10.3%), and subcutaneous recurrence in 10 relapses (34.5%). None of the recurrent lesions exhibited calcification. The total size of all the recurrent lesions at each relapse fairly correlated with the serum intact parathyroid hormone levels (r = 0.450; p = 0.014).
PARATHYROID CARCINOMA (PC) is a rare endocrine entity that accounts for an estimated 0.005% of all cancers and 0.7%–2.1% of lesions causing primary hyperparathyroidism (pHPT) [1-3]. PC is associated with totally distinct morbidity and mortality compared with its benign counterparts. According to the World Health Organization 2017 criteria, unequivocal diagnosis of PC by histopathology requires at least one of the following traits: unambiguous vascular invasion, perineural invasion, gross invasion into the adjacent anatomic structures, and metastasis [4]. In clinical practice, initial histopathologic examination may fail to recognize PC, probably because of the quality of the specimen or the experience of the pathologist. Consequently, some patients with PC experience diagnosis delay until recurrent or metastatic lesions are discovered. Due to the ineffectiveness of chemotherapy and radiotherapy, palliative reoperation is often performed for the treatment of intractable hypercalcemia in these patients [5].
Accordingly, accurate identification and localization of recurrent or metastatic lesions are critical for the management of PC. Compared to Computed tomography (CT), 99mTc sestamibi (MIBI), ultrasound (US) is usually the first-line modality for the postoperative surveillance of the patients with PC because distant metastasis is believed to occur late in the progression of PC, and often secondary to local recurrences [6]. However, there is limited literature regarding the sonographic features of patients with recurrent PC. Therefore, we analyzed and summarized this information for promoting better management of patients with PC.
Materials and Methods
Patients and clinical data
Approval from the Ethics Committee of Peking Union Medical College Hospital was obtained for the study (No: S-K1518). Since this was a retrospective observational study and the identity of the patients was kept confidential, the requirement for written consent was waived. From January 2004 through December 2020, 21 patients with 29 recurrences were identified, who met the following inclusion criteria: (1) confirmed pathologic diagnosis of locoregional recurrence of parathyroid carcinoma; (2) underwent preoperative ultrasound examination at our institute; (3) with available clinical data such as serum intact parathyroid hormone (iPTH) and calcium levels at relapse, as well as the site and pathology results of the primary parathyroid lesion. The time interval between the initial onset and relapse of PC was documented. MIBI results, if available, were also reviewed for comparison with the US findings. Siemens Immulite 2000 and Beckman DxI800 platforms were used to measure the iPTH levels using the second generation assay technique.
Ultrasonography examinations
Neck US examinations were performed by specialists with more than 10 years of experience in the thyroid and parathyroid field. HDI 5000 7–15-MHz linear probe (Philips Medical Systems, Bothell, WA) or iU22 5–12-MHz linear probe was used for assessment. Both gray-scale and color Doppler images were reviewed by two radiologists trained in thyroid and parathyroid ultrasound. If there was any disagreement of regarding the US features of a lesion, a consensus was reached by discussion with a specialist with more than 20 years of experience in related field. The location, size, echogenicity, shape, boundary, number and vascularity of the parathyroid lesions were recorded according to a pre-agreed protocol. When multiple lesions were identified on sonography, the largest nodule was selected for assessment as the target lesion, and its size was documented. For subsequent correlation analysis, the total size was calculated as the sum of the maximal diameter of each recurrent lesion identified by ultrasound. Criteria for determining the ultrasound features of the parathyroid lesions were as follows: location was described as right or left in general, with or without additional details; the shape was divided into “oval or round” and “irregular”; boundary was classified as either “clear boundary” or “infiltrative or blurred boundary”; overall echogenicity of a specific lesion was described as hypoechogenicity or iso- or hyper-echogenicity, when compared to the echogenicity of the normal thyroid. Furthermore, echogenic septa-like structures within the hypoechoic parathyroid lesions were identified frequently during the review and taken into account. Considering the even or uneven echotexture within the lesions, each lesion was described as heterogeneous or homogeneous. The vascularity was evaluated by color Doppler imaging and categorized into, absent (grade 0), mild (grade 1), and marked (grade 2) vascularity based on the normal region of the thyroid, which was considered to have mild vascularity (grade 1).
Statistics
Statistical analyses were performed using IBM SPSS Statistics Version 25.0 (Chicago, IL, USA) and R 3.6.3 (R foundation for Statistical Computing, www.R-project.org). Continuous variables were described as means with standard deviation or medians and interquartile range depending on the results of normality testing using the Shapiro‐Wilk method, while categorical variables were described as frequencies with percentages. Correlation between the serum iPTH and size of the recurrent PC lesions (largest size and total size) were explored using the Spearman test. The Loess method was employed for delineating and fitting curves. A two-sided p < 0.05 was set as the threshold for the statistical significance of tests.
Results
Of the total 21 patients, nine were men (42.9%), and 12 were women (57.1%). The median age at relapse was 45 years (range, 24–71 years). Seven patients with more than one recurrence were included in the analysis. Of the 20 patients with histopathologic records of primary lesions, 12 patients (60.0%) had an initial diagnosis of benign disease other than malignancy, including parathyroid adenoma (n = 7) or atypical parathyroid adenoma (n = 4) or parathyroid cyst (n = 1). Of the total 21 patients, 15 (71.4%) patients had a parathyroidectomy; 6 (28.6%) underwent en bloc resection. The median disease-free interval (DFI) after the initial surgery was 36 (range 2–205) months. The median Serum iPTH and calcium levels were 345 pg/mL(range 68.8–3,304) and 3.09mmol/L (range 2.39–4.69), respectively. MIBI was performed in 26 relapses, and the negative rate was 11.5% (3/26). Concordant localization results of MIBI and US were identified in 18 out of 26 relapses (69.2%). Of the 11 relapses with records of lymphadenectomy, only one (9.1%) relapse was associated with a positive lymph node in the superior mediastinum. Additional information about the 29 relapses is displayed in Table 1.
Table 1
Demographic and clinical information of 21 patients with recurrent parathyroid carcinoma
| Patient ID |
Gender |
Age at each relapse |
Serum calcium level (mmol/L) |
Serum intact parathyroid hormone level (pg/mL) |
Size of the largest recurrent lesion (cm) |
Location of the recurrent lesions against the primary sites |
number of recurrent lesions |
Relapse time interval |
Pathology of primary lesion |
Type of resection |
| 1 |
M |
37 |
3.3 |
270.2 |
1.9 |
Ipsilateral |
single |
36 |
Atypical adenoma |
Parathyroidectomy + partial thyroidectomy |
| 1 |
M |
37 |
2.89 |
323.6 |
1.8 |
Ipsilateral |
multiple |
3 |
Atypical adenoma |
— |
| 2 |
F |
33 |
3.41 |
752.8 |
1.6 |
Ipsilateral, contralateral, midline |
multiple |
49 |
Atypical adenoma |
Parathyroidectomy |
| 2 |
F |
34 |
3.52 |
339.5 |
1.9 |
contralateral |
multiple |
11 |
Atypical adenoma |
— |
| 3 |
F |
64 |
3.09 |
286.8 |
2.1 |
Ipsilateral |
multiple |
42 |
Carcinoma |
En bloc + level VI dissection |
| 4 |
M |
63 |
2.92 |
318 |
1.9 |
Ipsilateral, contralateral |
multiple |
37 |
Atypical adenoma |
No definitive treatment |
| 5 |
M |
46 |
2.7 |
446 |
1.1 |
Ipsilateral |
multiple |
205 |
Adenoma |
Parathyroidectomy |
| 6 |
M |
40 |
2.39 |
726 |
1.8 |
Contralateral |
single |
2 |
Carcinoma |
Parathyroidectomy + partial thyroidectomy |
| 6 |
M |
41 |
2.85 |
215 |
2.3 |
Ipsilateral |
multiple |
31 |
Carcinoma |
— |
| 7 |
M |
56 |
3.12 |
301.1 |
2 |
Contralateral |
multiple |
144 |
Adenoma |
Parathyroidectomy |
| 8 |
M |
51 |
3.07 |
359.8 |
2 |
Ipsilateral |
multiple |
26 |
Carcinoma |
En bloc + level VI dissection |
| 9 |
M |
31 |
3.29 |
375 |
0.9 |
Contralateral, midline subcutaneously |
multiple |
26 |
Adenoma |
Parathyroidectomy |
| 9 |
M |
33 |
2.73 |
68.8 |
1.5 |
Ipsilateral |
multiple |
27 |
Adenoma |
— |
| 10 |
F |
60 |
3.34 |
194.7 |
1 |
Ipsilateral |
multiple |
16 |
Carcinoma |
Parathyroidectomy |
| 10 |
F |
60 |
3.37 |
190.1 |
1.1 |
Ipsilateral subcutaneously, contralateral |
multiple |
8 |
Carcinoma |
— |
| 11 |
F |
30 |
4.05 |
2,500 |
3.8 |
Contralateral subcutaneously, ipsilateral |
multiple |
63 |
Adenoma |
Parathyroidectomy |
| 11 |
F |
32 |
2.8 |
238 |
1.6 |
Ipsilateral subcutaneously, contralateral |
multiple |
26 |
Adenoma |
— |
| 12 |
F |
24 |
3.04 |
162.3 |
0.8 |
Contralateral |
single |
15 |
Atypical adenoma |
En bloc resection |
| 13 |
M |
68 |
3.76 |
1,611 |
1.9 |
Ipsilateral |
multiple |
52 |
Carcinoma |
Parathyroidectomy |
| 14 |
M |
58 |
3.49 |
504 |
1.1 |
Ipsilateral, midline |
multiple |
15 |
Carcinoma |
Parathyroidectomy + partial thyroidectomy |
| 14 |
M |
58 |
3.46 |
265 |
1.2 |
Ipsilateral |
multiple |
21 |
Carcinoma |
— |
| 14 |
M |
58 |
3.67 |
710 |
1.4 |
Ipsilateral |
multiple |
17 |
Carcinoma |
— |
| 15 |
M |
50 |
4.14 |
1,045.2 |
1.4 |
Ipsilateral subcutaneously, ipsilateral |
multiple |
27 |
NA |
Parathyroidectomy + partial thyroidectomy |
| 16 |
F |
36 |
4.69 |
3,304 |
2.6 |
Ipsilateral |
multiple |
26 |
Adenoma |
Parathyroidectomy |
| 17 |
F |
45 |
3.03 |
395.7 |
1.6 |
Contralateral subcutaneously, ipsilateral |
multiple |
5 |
Adenoma |
Parathyroidectomy |
| 18 |
F |
36 |
2.72 |
123.3 |
3.2 |
Ipsilateral, contralateral, midline subcutaneously |
multiple |
60 |
Cyst |
Parathyroidectomy + partial thyroidectomy |
| 19 |
F |
49 |
3.57 |
286.5 |
2.3 |
Ipsilateral |
single |
37 |
Carcinoma |
En bloc resection |
| 20 |
F |
71 |
3.07 |
345 |
1.1 |
Ipsilateral |
multiple |
88 |
Adenoma |
Parathyroidectomy |
| 21 |
F |
31 |
3.51 |
1,252.6 |
3.3 |
Ipsilateral |
multiple |
25 |
Carcinoma |
En bloc resection |
M, male; F, female; —, as above; NA, not documented; Normal range of serum calcium, 2.13–2.70 mmol/L; Normal range of intact parathyroid hormone, 12–68 pg/mL; relapse time interval, the time interval between the prior surgical treatment and the relapse of PC
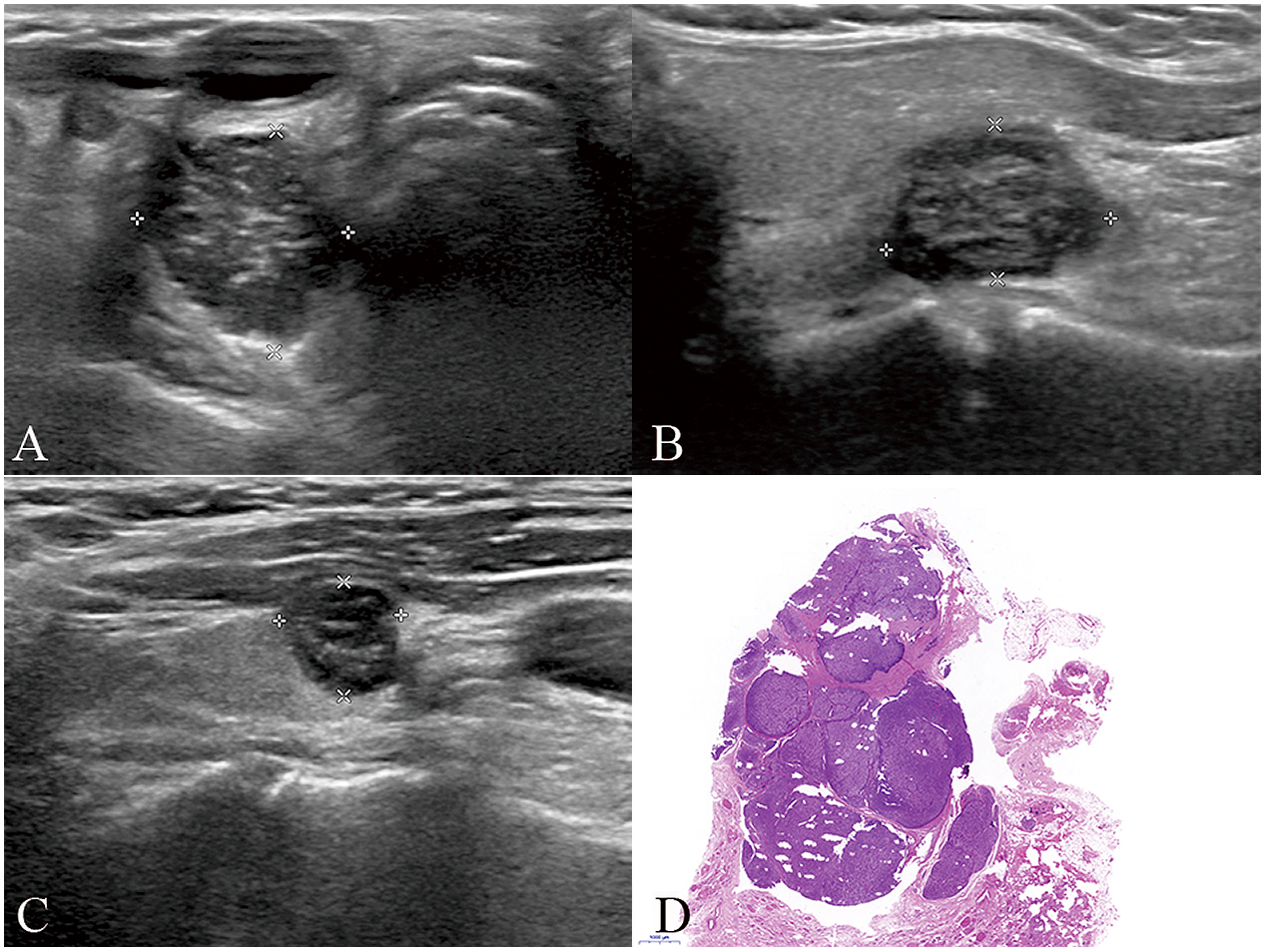
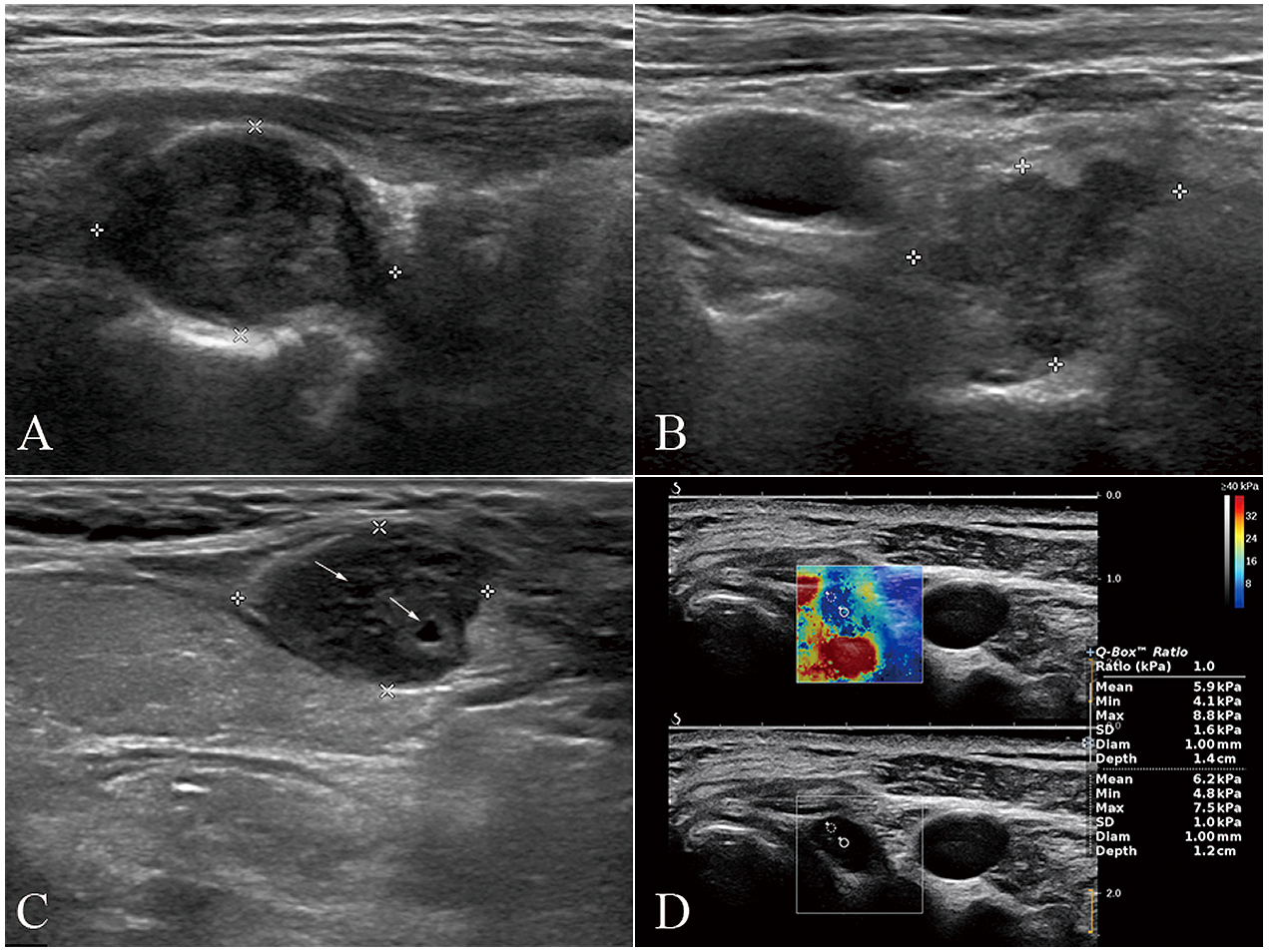
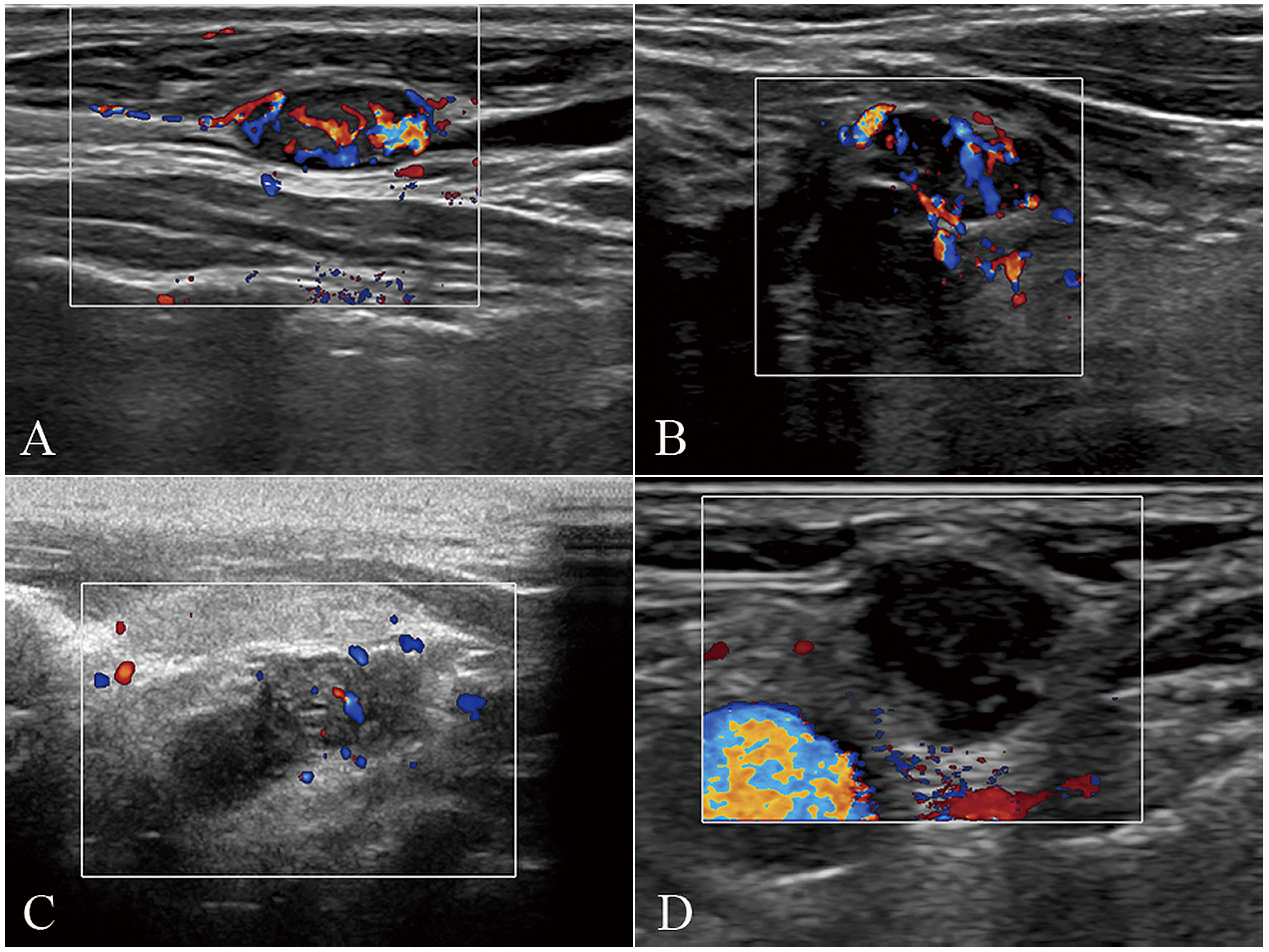
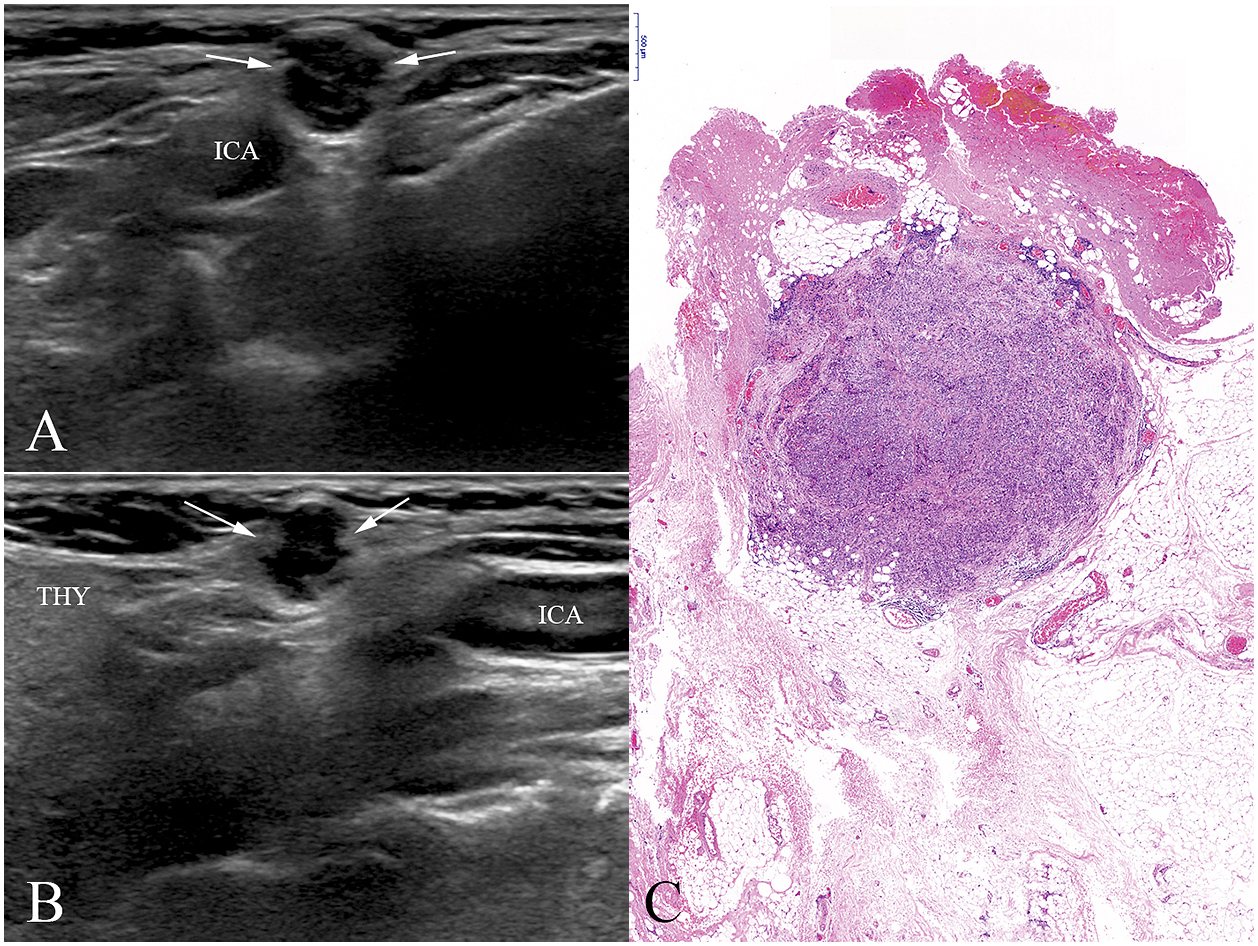
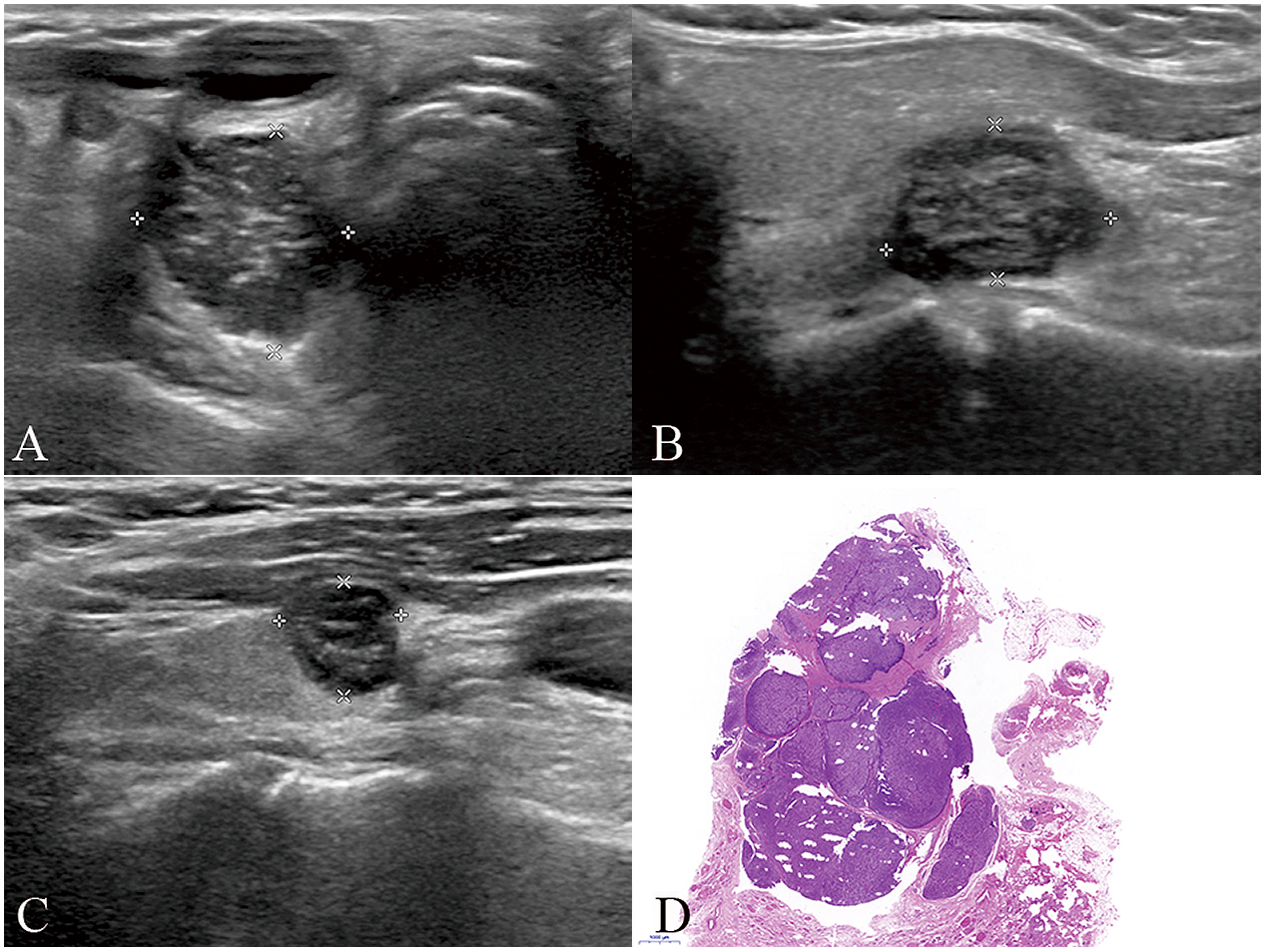
On sonography, multiple recurrent foci were identified in 26 relapses (26/29 [89.7%]). The median size of the largest recurrent lesion at each relapse was 1.8 cm (range 0.8–3.8 cm), while the median total size of all the recurrent PC lesions at each relapse was 2.8 cm (range 0.8–7.8cm). Ultrasound images showed hypoechoic solid nodules in 28 relapses (28/29 [96.6%]), inhomogeneous echo-texture in 28 relapses (28/29 [96.6%]), intralesional echogenic septa-like structures in 21 relapses (21/29 [72.4%]) (Fig. 1), intralesional cystic change in two relapses(2/29 [6.9%]), infiltrative or blurred boundary in 20 relapses (20/29 [69.0%]) (Fig. 2), irregular shape in 22 relapses (22/29 [75.9%]), marked vascularization on color Doppler imaging in 19 relapses (19/29 [65.5%]) (Fig. 3), contralateral recurrence in three relapses (3/29 [10.3%]), and subcutaneous recurrence in 10 relapses (10/29 [34.5%]) (Fig. 4). None of the recurrent lesions showed calcification. The largest size of the recurrent lesions in the neck demonstrated no significant correlation with the iPTH level (r = 0.262; p = 0.170). However, the total size of all the recurrent lesions identified using ultrasound showed a fairly positive correlation with the iPTH level (r = 0.450; p = 0.014) (Fig. 5).
Discussion
Although parathyroid carcinoma is a rare disease, local relapse is common. The recurrence rate of PC reported in previous studies ranged from 42% to 72% [7-9], and depends on the biological characteristics of PC or the surgical extent [10]. In contrast, Hsu et al. reported a favorable long-term prognosis of PC with disease-specific survival (DSS) rates of 94.1% at 5 years and 90% at 10 years [11]. In this regard, relapse instead of death became the major issue in pertinent cases. As the first-line modality to surveil postoperative patients with pHPT, ultrasound plays a pivotal role in the evaluation of cervical recurrence of PC [12]. We found that US could provide valuable evidence to diagnose PC recurrence in the neck in patients with persistent or recurrent hyperparathyroidism. The diagnosis should be considered even in pHPT patients with initial benign histopathologic diagnosis.
To our knowledge, there are limited data on the role of neck ultrasound in the assessment of recurrent lesions of PC, let alone the detailed US features of the condition. Electron et al. found that the sensitivity of ultrasound to detect secondary deposits of PC was 69%, which was inferior to sestamibi scan (79%), magnetic resonance imaging (93%) and selective venous catheterization with PTH measurement (83%). We partly ascribe the relatively low sensitivity of US to unfamiliarity with the US features of these recurrent tumor foci. Dotzenrath et al. reported that ultrasonography correctly identified 11 out of 13 sites of recurrence (84.6%), while MIBI identified none in one test (0/1). Accodingly, they positioned ultrasound and CT as the most sensitive procedures for detecting recurrences in the neck or mediastinum. Relevant studies have shown discrepancies in diagnostic efficiency using different imaging procedures, which highlights the importance of institutional experience with a specific imaging modality for detecting parathyroid recurrent lesions.
Unlike thyroid carcinoma recurrences, cervical recurrent foci of PC mainly originate from remnant tumor cells rather than metastases to lymph nodes. The intralesional heterogeneous appearance with echogenic septa-like structures was relatively specific according to our analysis. Yazgan et al. conducted a one-to-one comparison of sonograms with histopathological sections in parathyroid disorders, and demonstrated that hypoechoic areas in ultrasound mostly matched with the chief cells, while the hyperechoic areas mainly represented connective and fat tissue [13]. Although they targeted the more prevalent parathyroid adenomas as the research objects, we can deduce that cellular nodules divided by broad fibrous bands in a large proportion of the PC samples could present as hypoechoic nodules with hyperechoic septa-like structure on sonography, similar to the recurrent foci of PC. The boundaries of the lesions could either be clear or infiltrative. DeLellis reported a case with metastatic parathyroid carcinoma in the lung, which was indistinguishable from a parathyroid adenoma, suggesting that oval or round nodules with sharp demarcation could be recurrent or metastatic tumors of PC as well [14]. Nonetheless, most recurrent PC lesions still exhibit an infiltrative boundary, especially those with large sizes, showing that the margin features align with the primary PC lesions [15]. Color Doppler revealed marked vascularity in most of the targeted lesions. The uneven vessels, radial in nature, observed in the recurrent tumor foci were similar to primary lesions and could facilitate the diagnosis [16]. In addition, 34.5% (10/29) of the relapses occurred subcutaneously, which was attributed to capsule spillage and seeding of cells by a previous report. We agree with this theory because the subcutaneous lesions appear more frequently along the access route of the first operation [17]. With regard to the relationship between serum intact parathyroid hormone level and size of the recurrent lesions, we discovered that the total size of all the lesions rather than the size of the largest lesion at ultrasonography correlated significantly with the iPTH levels. Moreover, an extremely high iPTH level was a risk factor for distant metastasis or lesions in the mediastinum which are hard to reach by ultrasound. In such a scenario, advanced imaging modalities such as enhanced CT, magnetic resonance imaging and positron emission tomography have been suggested for full evaluation.
We found that lymph node metastasis was rare in PC, which is concordant with a previous population-based analysis showing that the rate of positive lymph nodes ranged from 1.7% to 10.5% [18]. Of the 11 recurrences, only one (9.1%) presented with lymph node metastasis. In fact, most recurrent lesions were cancerous tissues implanting in the surrounding fibrous connective structures or muscle tissues. MIBI can successfully detect the recurrent sites most of the time, however, the consistency with US is somewhat limited, especially in cases with multiple lesions. We deemed that the efficiency of MIBI depends on the distribution of the cell types in the recurrent lesions. Cordes et al. concluded that the MIBI negativity of parathyroid adenomas resulted from the absence of oxyphilic cells with large numbers of mitochondria, probably leading to reduced bonding sites for the radiotracer [19]. Moreover, Bondeson et al. found that 50% of the parathyroid carcinomas in their series were composed of mainly chief cells, which could influence the detection sensitivity of MIBI [20].
In our study, 57.1% (12/21) of patients were diagnosed with benign parathyroid disease prior to the recurrence. This reflect the considerable uncertainty in terms of the pathological diagnosis of PC [21]. Importantly, well differentiated parathyroid carcinoma accounts for 80.4% of all the PC cases, which could harbor the same morphology as a parathyroid adenoma in most cases [22]. This may mislead clinicians when multiple hypoechoic lesions are observed on US imaging of these patients. During the process of data collection, we found that sonographers with more than 5 years of experience in tertiary centers had misdiagnosed the subcutaneous recurrence of PC as hemangioma or nodular fasciitis. As mentioned earlier, the definite diagnosis of PC based on pathology should meet at least one of the following criteria: unambiguous vascular invasion, perineural invasion, gross invasion into the adjacent anatomic structures and metastasis. Given that some parathyroid tumors do not explicitly show these traits, they may be categorized as atypical parathyroid adenoma or, not otherwise specified, adenoma after primary surgery. Nevertheless, onset of new lesions across the neck in combination with biochemical abnormalities should raise the suspicion of potential recurrence of PC, warranting a reoperation.
This study has some limitations that should be noted. Firstly, the sample size was relatively small due to the rarity of PC, rendering advanced statistical subgroup analysis impossible.Secondly, this retrospective study assessed only the static US images without cine-loop, which may limit the potential to detect additional ultrasound characteristics. In addition, we only evaluated the US features of the largest nodule in cases with multiple recurrent foci, which may have introduced bias. Lastly, Inter-rater variability, as well as the sensitivity or specificity of US for detecting the regional relapse of PC, were not assessed, and these concerns would be addressed in future studies.
In conclusion, patients who had undergone prior surgical treatment for hyperparathyroidism, and subsequently developed persistent or recurrent hypercalcemia could benefit from an ultrasound evaluation. Several ultrasound features of emerging lesions in the neck, including hypoechogenicity, heterogeneous texture, echogenic septa-like structures, multicentric distribution, and rich intralesional vascularization, may be indicative of locoregional recurrence of parathyroid carcinoma, regardless of the initial benign pathologic diagnosis and negative MIBI findings.
Abbreviations
pHPT, primary hyperparathyroidism; PC, parathyroid carcinoma; iPTH, intact parathyroid hormone; US, ultrasound; CT, computed tomography; MIBI, 99mTC sestamibi
Acknowledgements
This study was supported by a grant from the Tibet Autonomous Region Science and Technology Project (XZ201901-GB-04) and the Tibet Autonomous Region Organization and Aiding Project (XZ2019ZR ZY05(Z)).
Disclosure
None of the authors have any potential conflicts of interest associated with this research.
References
- 1 Sadler C, Gow KW, Beierle EA, Doski JJ, Langer M, et al. (2014) Parathyroid carcinoma in more than 1,000 patients: a population-level analysis. Surgery 156: 1622–1629; discussion 1629–1630.
- 2 Shane E (2001) Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab 86: 485–493.
- 3 Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM (2007) Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer 109: 1736–1741.
- 4 Lloyd RV, Osamura RY, Klöppel G, Rosai J (2017) WHO Classification of Tumours of Endocrine Organs (4th). International Agency for Research on Cancer (IARC), Lyon, France.
- 5 Betea D, Potorac I, Beckers A (2015) Parathyroid carcinoma: challenges in diagnosis and treatment. Ann Endocrinol (Paris) 76: 169–177.
- 6 Kebebew E, Arici C, Duh QY, Clark OH (2001) Localization and reoperation results for persistent and recurrent parathyroid carcinoma. Arch Surg 136: 878–885.
- 7 Busaidy NL, Jimenez C, Habra MA, Schultz PN, El-Naggar AK, et al. (2004) Parathyroid carcinoma: a 22-year experience. Head Neck 26: 716–726.
- 8 Iihara M, Okamoto T, Suzuki R, Kawamata A, Nishikawa T, et al. (2007) Functional parathyroid carcinoma: long-term treatment outcome and risk factor analysis. Surgery 142: 936–943.
- 9 Harari A, Waring A, Fernandez-Ranvier G, Hwang J, Suh I, et al. (2011) Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab 96: 3679–3686.
- 10 Hu Y, Bi Y, Cui M, Zhang X, Su Z, et al. (2019) The influence of surgical extent and parafibromin staining on the outcome of parathyroid carcinoma: 20-year experience from a single institute. Endocr Pract 25: 634–641.
- 11 Hsu KT, Sippel RS, Chen H, Schneider DF (2014) Is central lymph node dissection necessary for parathyroid carcinoma? Surgery 156: 1336–1341.
- 12 Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, et al. (2016) The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg 151: 959–968.
- 13 Yazgan AK, Topaloglu O, Cuhaci FN, Ozdemir D, Alkan A, et al. (2020) Mapping of parathyroid neoplasms based on grey scale ultrasound images and histopathological whole slide images. Ann Diagn Pathol 46: 151492.
- 14 DeLellis RA (2011) Parathyroid tumors and related disorders. Mod Pathol 24 Suppl 2: S78–S93.
- 15 Liu R, Xia Y, Chen C, Ye T, Huang X, et al. (2019) Ultrasound combined with biochemical parameters can predict parathyroid carcinoma in patients with primary hyperparathyroidism. Endocrine 66: 673–681.
- 16 Sidhu PS, Talat N, Patel P, Mulholland NJ, Schulte KM (2011) Ultrasound features of malignancy in the preoperative diagnosis of parathyroid cancer: a retrospective analysis of parathyroid tumours larger than 15 mm. Eur Radiol 21: 1865–1873.
- 17 Kim SS, Jeon YK, Lee SH, Kim BH, Kim SJ, et al. (2014) Distant subcutaneous recurrence of a parathyroid carcinoma: abnormal uptakes in the (99m)Tc-sestamibi scan and (18)F-FDG PET/CT imaging. Korean J Intern Med 29: 383–387.
- 18 Lo WM, Good ML, Nilubol N, Perrier ND, Patel DT (2018) Tumor size and presence of metastatic disease at diagnosis are associated with disease-specific survival in parathyroid carcinoma. Ann Surg Oncol 25: 2535–2540.
- 19 Cordes M, Dworak O, Papadopoulos T, Coerper S, Kuwert T (2018) MIBI scintigraphy of parathyroid adenomas: correlation with biochemical and histological markers. Endocr Res 43: 141–148.
- 20 Bondeson L, Sandelin K, Grimelius L (1993) Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol 17: 820–829.
- 21 Schulte KM, Talat N (2012) Diagnosis and management of parathyroid cancer. Nat Rev Endocrinol 8: 612–622.
- 22 Hundahl SA, Fleming ID, Fremgen AM, Menck HR (1999) Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S. between 1985–1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 86: 538–544.