2017 Volume 63 Issue 2 Pages 112-115
2017 Volume 63 Issue 2 Pages 112-115
The patient was an 86-year-old woman with back pain after a fall. She had no neurological findings at the initial visit. Plain radiographs and magnetic resonance imaging (MRI) showed diffuse idiopathic skeletal hyperostosis (DISH) and a Th10 fracture. Two weeks later, she started gait exercise with immobilization by a rigid orthosis. Twenty-five days later, she presented with paralysis and numbness of her legs. Computed tomography (CT) showed anterior expansion in the vertebral body of Th10. MRI showed an intramedullary high-intensity area on T2-weighted images at the same level. She was diagnosed as having delayed paraplegia after a Th10 fracture and transferred to our hospital for surgery. Laminectomy of Th10, posterior fusion from Th7 to L1 with pedicle screws and hooks to Th6 and L1 laminae, anterior fusion from Th9 to Th11 with a plate, and autologous bone grafting were performed simultaneously. The patient’s paralysis improved, and she started gait exercise with no limitation of bed rest and without an orthosis after surgery. At 8 days after surgery, she again presented with low back pain and paralysis in her legs. CT revealed an L1 fracture, which was the caudal end of the surgical fusion. The decreased kyphosis after surgery compared to that at pre-injury might have caused a subsequent horizontal shear force to L1 when the patient sat on the bed and when she walked. In conclusion, to avoid postoperative adjacent vertebral fracture after fusion, appropriate correction of spinal alignment to that at pre-injury is needed for vertebral fractures in patients with DISH.
Diffuse idiopathic skeletal hyperostosis (DISH) is a systemic condition leading to ossification of ligaments and entheses1). It has been reported that patients with DISH who develop vertebral fractures are at risk for delayed paraplegia due to its anatomical characteristics2-4). Therefore, rigid fixation with instrumentation is recommended for such cases2-4). However, long fusion may cause junctional failure5,6). A case of adjacent vertebral fracture after simultaneous combined anterior and posterior fusion for a thoracic vertebral fracture in a patient with DISH is reported.
An 86-year-old woman with no significant past medical history presented with acute back pain after a fall and was transferred to her local hospital. Plain radiographs showed a bone bridge spanning more than four intervertebral bodies without a narrow intervertebral space (Figure 1a, b). Magnetic resonance imaging (MRI) showed a Th10 fracture (Figure 1c). She was diagnosed as having DISH and a Th10 fracture. She underwent conservative treatment because of her extreme age and no clear instability. She started gait exercise at 2 weeks after injury with immobilization by a rigid orthosis. Twenty-five days after injury, she presented with bilateral leg paralysis and numbness. Since delayed paraplegia was suspected, she was transferred to our hospital for surgical treatment. On admission, she had bilateral leg paralysis (grade 3 on manual muscle testing: MMT) below the iliopsoas and hypoesthesia of the anterior thighs. She had no bladder or bowel dysfunction. A lateral plain radiograph showed a decreased local kyphotic angle (Figure 2a). Computed tomography (CT) showed anterior expansion with a bone defect in the Th10 vertebral body and subsequent decreased kyphosis due to distraction-extension injury (reverse Chance fracture) (Figure 2b) and ossification of the ligamentum flavum at bilateral T10/11. MRI showed an intramedullary high-intensity area on T2-weighted images (Figure 2c), indicating instability and non-union at the same level. She underwent surgery 50 days after the injury. Laminectomy of Th10, partial laminotomy of Th11, Th7-L1 posterior fusion with pedicle screws and additional stabilization with laminar hooks to Th6 and L1 laminae to avoid back out of the screws, Th9-11 anterior fusion with a plate, and autologous bone grafting were performed simultaneously (Figure 3). In situ fusion in the prone position was done with no alignment correction. After surgery, her paralysis improved, and she started gait exercise with no limitation. Eight days after surgery, she presented with low back pain and paralysis (grade 2 on MMT) in her legs with no apparent cause. CT revealed an L1 fracture in the middle of the vertebral body, which was the caudal end of the fusion (Figure 4b). The patient refused further surgical treatment and werewas transferred back to the previousinitial hospital. She was bedridden thereafter because of the pain, and theher paralysis did not improve. Finally, shethe patient was die of pneumonia 4 month after surgery.

Plain radiographs at the initial visit to the local hospital showing a bone bridge spanning more than four intervertebral bodies. (a, anteroposterior view; b, lateral view). T1-weighted MRI showing a Th10 vertebral fracture (c).
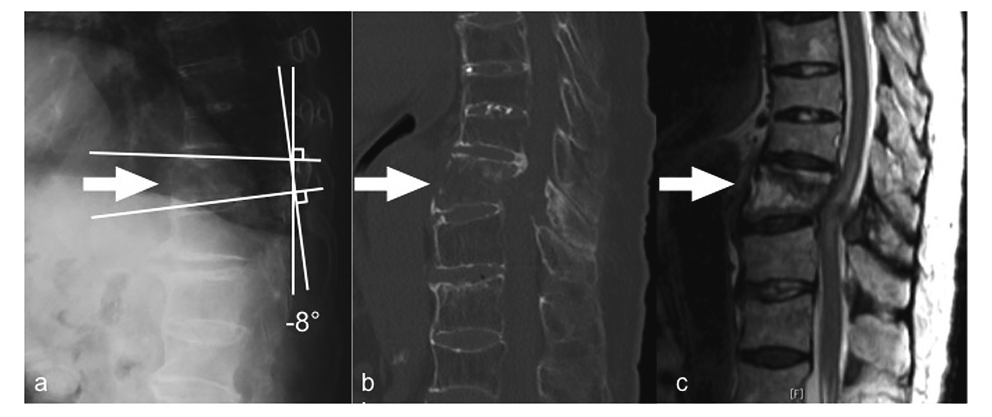
a, Lateral plain radiograph before surgery showing a decreased local kyphotic angle. b, Computed tomography (CT) before surgery showing anterior expansion with a bone defect in the ventral Th10 vertebral body and subsequent alignment change due to distraction-extension injury. c, T2-weighted MRI before surgery showing a bone defect at the ventral L10 vertebral body and an intramedullary high-intensity area at the Th10 level.

Anteroposterior (a) and lateral (b) plain radiographs immediately after anterior (from Th9 to Th11) and posterior (from Th7 to L1) fusion showing a decreased kyphotic angle.

Lateral plain radiograph (a), CT (b), and MRI (c) immediately after the postoperative L1 fracture showing the L1 vertebral fracture in the middle of the L1 vertebral body (arrow) and dorsal displacement at the L1 level. No alignment change is observed at the Th10 level (arrowhead).
DISH is diagnosed when ossification of the anterior longitudinal ligament is present on spine radiographs over at least four consecutive levels1). It has been reported that the prevalence of DISH ranges from 2.9% to 25%7,8). In addition, DISH is considered to have become more widespread due to its association with age, obesity, and type 2 diabetes mellitus9-12).
Some authors have suggested that patients with DISH are also at risk for vertebral fractures after minor impacts, comparable to the fracture mechanism in patients with ankylosing spondylitis13,14). On the other hand, vertebral fractures with DISH can cause serious instability, and rigid fusion using instrumentation is thus required, especially in patients with a neurological deficit2-4).
The present case showed a fracture at the caudal end of the fusion in the early stage after surgery. To date, no cases involving postoperative fractures after fusion for vertebral fractures with DISH have been reported. Inappropriate postoperative alignment may have been the reason for this fracture. It has been reported that patients with DISH have rigidity of the spine and kyphotic change15). Thus, the ability of spinal alignment to change and compensate would have been poor in this patient. The local kyphotic angle was 2° at the initial visit; however, when delayed paraplegia occurred, the angle was decreased to -8°. Finally, it was not corrected surgically, and it decreased to -11° (Figure 3). The decreased kyphosis could have caused a subsequent horizontal shear force to L1 when the patient sat on the bed and when she walked.
Therefore, this fracture might have been avoided if the alignment had been corrected to that at pre-injury. Pre-injury alignment should have been obtained after changing of the position to the prone position in surgery. For example, Takahashi et al.16) reported that a dome-shaped frame is useful at surgery to achieve inherent kyphosis in each patient with DISH.
As for the range of fusion, it has been reported that 3 above and 3 below fusion is reliable for fractures with DISH4). On the other hand, long fusion can cause junctional failure5,6). A long lever arm caused by long fusion might concentrate the mechanical stress at L1. Further study is needed to determine the appropriate range of fusion.
In conclusion, to avoid postoperative adjacent vertebral fracture after fusion, appropriate correction of spinal alignment to that at pre-injury is needed for vertebral fractures in patients with DISH.
None.