2013 Volume 51 Issue 4 Pages 406-416
2013 Volume 51 Issue 4 Pages 406-416
We explored the associations of job strain with sleep and alertness of shift working female nurses and nursing assistants. Participants (n=95) were recruited from the Finnish Public Sector Study, from hospital wards that belonged to the top or bottom quartiles on job strain. Participants’ own job strain was at least as high in high-strain group or low in low-strain group as the ward’s average. The study included three-week measurements with sleep diary and actigraphy. Psychomotor Vigilance Test (PVT) was performed during one pre-selected morning and night shift and a day off. Sleep efficiency before morning shifts was lower in the high-strain than low-strain group (p=0.03). Low-strain group took more often (72 vs. 45%; p<0.01) and longer naps (62 vs. 35 min; p=0.01) before the first night shift than high-strain group. Difficulties initiating sleep were more common in high-strain group, especially after evening shifts (p<0.01). High-strain group had more often at least one lapse in PVT during the night shift (p=0.02). Average sleep duration (06:49h) and efficiency (89%) did not differ between these groups. In conclusion, high job strain is associated with difficulties initiating sleep and reduced psychomotor vigilance in night shifts. Shift working contributed to impaired sleep in both high and low job strain group. Individual and organization-based actions are needed to promote sufficient sleep in shift working nurses, especially with high job strain.
Nursing work is stressful1), affectively intense, decision-rich2), typically includes numerous interruptions3) and carries a risk for medical errors4). There is substantial evidence to suggest that long-term exposure to stress may adversely affect not only nurses health, increasing the risk of various diseases, such as coronary heart disease5) and depression6) and the risk for disability pensioning7) but also put patients at risk8). Impaired recovery and compromised sleep may be important mediators between stress and illnesses9). For shift workers, long-term stress may increase the probability of a co-manifestation of several individual health risk factors, such as sedentary lifestyle, high blood pressure and cholesterol levels, that predispose to chronic disease10).
Psychosocial stress, in general, is assumed to have a negative effect on sleep11, 12) but relatively little research exists on work-related stress and sleep13) when sleep is measured not merely with subjective methods. Psychosocial stress can potentially lead to impaired sleep through direct and indirect pathways. Heightened arousal with elevated cortisol secretion increases difficulties in initiating sleep14) and sleep fragmentation15). Long-term psychosocial stress may also lead to health risk behaviors, such as smoking, physical inactivity and unhealthy diet10), which in turn affect negatively on sleep.
The hypothesis that work-related stress, such as job strain -a condition of high job demands combined with low control at work16) -causes sleep disruption17) and adversely affects sleep18) has been supported by cross-sectional questionnaire studies of daytime workers19). For example, in an earlier study the prevalence of disturbed sleep was 30% among the high-strain workers based on the Karasek’s model versus 5% in the low-strain group20). Work stress produces significant psycho-physiological activation and especially a high level of work-rumination is a strong predictor of sleep complaints19). It is possible that job strain impairs sleep more among shift workers that are exposed to the additional causes of insomnia due to working in shifts. Shift work is closely tied up with shortened or disturbed sleep in morning and night shifts, problems to fall asleep in connection with quick returns -that is to say a morning shift after an evening shift- and problems to wake up too early during the day sleep21,22,23).
Assessing psychosocial work environment in the most precise and unbiased way is a major challenge in psychosocial working conditions research24). We face this challenge by using a hospital ward level estimation of job strain to reduce subjectivity bias that may arise for example from negative affectivity24). Also, integrating research on job stressors and working times is needed25), since studies of job strain are mainly conducted among daytime workers19).
To our knowledge, there are no studies that have measured both exposure to job strain and sleep quantity in shift work. Despite extensive research among nursing staff, we found no earlier research reporting shift-specific sleep lengths or sleep disturbances according to job stress. We used daily actigraphic measures to estimation of sleep length and quality in different shifts during one natural shift cycle of 3 wk. We hypothesized that a) sleep quantity, quality and alertness are impaired by shifts among female nursing personnel and that b) these impairments are exacerbated among those who are exposed to job strain.
The participants were recruited from The Finnish Public Sector Study survey 2008 respondents (N=52 891, response rate 72%). From this sample, native Finnish speaking female health care professionals (hence referred to as “nurses” for brevity) with night shift work were identified (n=5,615) (Fig. 1). The present sample included participants from 5 hospitals or health care districts and 4 cities in Southern Finland. The nurses were from 59 wards, which had an average of 37 employees.

The flow chart of the study.
An invitation letter was sent to the workplace of nurses fulfilling the following inclusion criteria (n=422): night shift work, age 30–58 yr, native Finnish speaker, Body Mass Index (BMI) under 35 kg/m2, and at least 3 years work experience in the same ward. Age limits were set to ensure exposure to working life and to minimize the probability of retiring. Volunteers with coronary heart disease, insulin-treated diabetes mellitus, and pregnant or breast feeding mothers were excluded. The participants were not screened for sleep disorders. The main reasons for exclusion were changing ward or workplace (n=22) or quitting night shift work (n=21) after the 2008 survey.
Job strain was determined with three questions on job demand (JD) i.e. pace and pressure of work tasks and nine questions on job control (JC) i.e. individual autonomy over work timing and methods26) using a 5 -point Likert -type scale ranging from 1 (strongly disagree) to 5 (strongly agree) derived from Karasek’s Job Content Questionnaire (JCQ)16). As described elsewhere26), the high (HJS) and low (LJS) job strain groups were divided by grouping the wards with at least 5 respondents on the JD and JC scales at the ward level, using median split to identify HJS (high demands and low control) and LJS (low demands and high control) wards. With these cut-off points, we identified nurses from these wards who belonged to the HJS- or LJS-groups based on their individual mean scores of JD and JC. To increase contrast between job strain groups, the nurses belonging to the quartile with the least strain in the HJS-group and the most strain in the LJS-group were excluded. The mean values for job demands/job control were 4.56/3.20 in the HJS-group and 2.64/4.11 in the LJS-group (Mean Difference 1.92/–0.90, p<0.01). The reliability coefficients for JCQ for the invited (n=422) were good (Cronbach’s α=0.87 for JD and α=0.80 for JC).
The representativeness of the 95 participants was tested by comparing them to the 422 invited. There were no statistical differences (p-values >0.11) in responses on the 2008 survey between participated and invited on age, education level, work experience, number of children, BMI, habitual sleep length, sleep need, or sleep disturbances. More participants were from the LJS-group than the HJS-group (p<0.01) and fewer from the two major health care districts (p<0.01).
The study was approved by the Ethical Committee of the Hospital district of Helsinki and Uusimaa. Written informed consent was obtained from each participant. The participants were compensated for travelling expenses and paid 50 Euros compensatory allowance for participation.
Background variablesThe study included an Internet questionnaire featuring questions about work shifts and work conditions and typical coping strategies in stressful situations. The background variables were education level, physical activity (times per week, at least 30 min/d, during past 3 months), BMI, number of children, smoking, alcohol consumption, medication use, stressful life events during past 12 months27), morningness-eveningness questionnaire28) and Beck Depression Inventory (BDI-II)29). There was no missing data in the Internet questionnaires, as answering to all questions was required.
ParticipantsOf the 95 participants, 42 (44%) were in the HJS-group and 53 (56%) in the LJS-group. The participants worked most often in medical-surgical wards (45%, n=43) and intensive care or emergency units (15%, n=14). Their mean age was 47.2 yr (range 31–59), with no significant difference between the job strain groups. Shift work experience, family care-giving responsibility, stressful life-events, chronotype, BMI, smoking, alcohol or caffeine consumption (Table 1), medication use or measurement season showed no stress group differences either. Two of the participants in HJS-group scored points typical for clinical depression according to the BDI-II compared to none in LJS-group (p=0.19). The proportion of nurses was higher in the LJS-group (81%) than in the HJS-group (60%, p=0.02). The participants in the LJS-group were physically more active than the HJS-group (p<0.01).
| High Job Strain n=42 | Low Job Strain n=53 | p-value1 | DF | t-value | |||||
| Mean | SD | Mean | SD | ||||||
| Age (yr) | 47.7 | (6.4) | 46.7 | (7.5) | 0.52 | 93 | 0.64 | ||
| BMI (kg/m2) | 26.7 | (4.1) | 25.6 | (4.0) | 0.20 | 93 | 1.29 | ||
| Shift work experience (yr) | 18.7 | (7.9) | 16.9 | (7.6) | 0.27 | 90 | 1.11 | ||
| Caffeine doses per 24 h | 4.6 | (1.9) | 4.0 | (1.9) | 0.14 | 93 | 1.51 | ||
| % | (n) | % | (n) | p-value2 | |||||
| Education | 0.02 | ||||||||
| Nurse3 | 60 | (25) | 81 | (43) | |||||
| Nursing assistant4 | 40 | (17) | 19 | (10) | |||||
| Physical activity5 | <0.01 | ||||||||
| <3 × week | 29 | (12) | 6 | (3) | |||||
| ≥3 × week | 71 | (30) | 94 | (50) | |||||
| Family care-giving responsibility6 | 0.51 | ||||||||
| Yes | 62 | (21) | 69 | (31) | |||||
| No | 38 | (13) | 31 | (14) | |||||
| Stressful life event7 | 0.34 | ||||||||
| Yes | 66 | (27) | 75 | (39) | |||||
| No | 34 | (14) | 25 | (13) | |||||
| Cigarette smoking | 0.98 | ||||||||
| Yes | 19 | (8) | 19 | (10) | |||||
| No | 81 | (34) | 81 | (43) | |||||
| Alcohol consumption | 0.85 | ||||||||
| Never/seldom | 45 | (19) | 47 | (25) | |||||
| Regularly8 | 55 | (23) | 53 | (28) | |||||
| Chronotype | 0.90 | ||||||||
| Morning-type | 45 | (19) | 51 | (27) | |||||
| Evening-type | 55 | (23) | 49 | (26) | |||||
1Independent samples t-test, 2Pearson χ2, 3Nurse, midwife, public health nurse, X-ray nurse, deaconess-nurse, 4Nursing assistant, practical nurse, nursery nurse, mental nurse, 5 ≥30 min/d, during past 3 months, 6Children under 18 yr, 7During the past year, 8 ≥2 times/month, 24 g alcohol per time.
During the three-week field study, the participants’ sleep-wake rhythm was measured by actigraphy (Actiwatch AW7, Cambridge Neurotechnology Ltd, Cambs, UK) and a sleep diary. The actigraph was continuously worn on the non-dominant wrist, except at moments of hygiene concern at the work place. Actigraphy data were scored using 1 min epochs and analyzed with Actiwatch Activity and Sleep Analysis 7-software (Cambridge Neurotechnology Ltd, Cambs, UK).
The Internet questionnaire included questions about habitual sleep length and amount of sleep needed to feel rested on a continuous scale, and frequency (never/seldom, quite seldom, quite often or often/frequently) of difficulties in initiating sleep, difficulties in maintaining good sleep, and excessive daytime sleepiness during the past four weeks. Sleep efficiency (SE) was measured by actigraphy and calculated from the ratio of the time asleep to the time in bed. The limit of reduced SE was set to be <85%30). Sleep was classified insufficient if there was a 20% discrepancy between the actual sleep amount and the subjective evaluation of sleep need.
In the sleep diary the participants kept a record of times at which they went to sleep and got up, and their working hours. The nurses reported self-evaluated sleep latency, being awake during the night, ease of waking up, number of and duration of naps, the amount of alcohol or caffeinated drinks and use of sleep promoting medication.
The actigraphy data collection lasted on average 20.6 d (range 8–25 d) covering 95% of intended measurements. The sleep diaries were filled in with 95% of values.
Psychomotor vigilance test (PVT)31) was done during pre-selected, controlled work shifts: (i) a morning shift after at least two earlier morning shifts, (ii) a night shift after a morning or evening shift and (iii) the second consecutive day off. PVT was installed on HP ipaq 514 mobile phone (Hewlett-Packard Company, Palo Alto, CA, USA). A 5-min version of the PVT was done in (i) the morning shift between 12–15 and in the evening between 19–21, (ii) before night shift between 19–21, and at work between 02–04 and (iii) on a day-off between 12–15 o’clock. To minimize the effect of learning, the nurses were instructed to practice the PVT three times32) before the first test day. Answering was done by pressing the zero button. Reaction times >500 milliseconds were regarded as lapses. PVT tests were completed in 97% of planned tests.
Work shiftsThe data on work hours and work shifts during the field measurement period was obtained from realized rosters (n=88), or without the roster (n=7), from the sleep diary. The three-week rosters included on average 6 morning, 3 evening, 2 night, and 1 extended shifts. The nurses in the HJS-group had on average one morning shift more and one extended shift less than the nurses in the LJS-group (7 vs. 6, p=0.01 and 0 vs. 1, p=0.02). The morning shifts were mainly timed 7:00–15:00, the evening shifts 14:00–22:00 and night shifts 21:00–07:00. There was no statistical difference between job strain groups in total number of work hours, number of work shifts or night shifts during the field measurements.
Statistical analysisStatistical analyses were conducted by PASW 18.0 (Chicago, IL, USA). Pearson Chi-square test (χ2), Student’s t-test, Fisher’s exact test, one-way analysis of variance (ANOVA) or Mann-Whitney U-test were used to compare job strain group differences in individual and job characteristics depending on the variable and the normality of the distribution of the variable. Age and education level were used as covariates. A p-value <0.05 indicates statistically significant result throughout the study.
Analyses adjusted for age showed that the HJS- and LJS-groups did not differ with respect to the self-reported habitual sleep length.
The actigraphy data showed that the main sleep period lasted, on average, 06:46 h in the HJS-group and 06:51 h in the LJS-group on average (Table 2) with no group differences in connection with different shifts or the pre-selected shifts.
| Sleep length (h) | Reduced sleep efficiency (<85%) | |||||||
| High Job Strain | Low Job Strain | p -value1 | High Job Strain% (n) | Low Job Strain% (n) | p-value2 | |||
| Mean | Range | Mean | Range | |||||
| 3 weeks | 06:46 | 04:52–07:51 | 06:51 | 04:54–08:22 | 0.76 | 17 (7) | 9 (5) | 0.36 |
| Before morning shifts | 05:49 | 04:10–07:03 | 06:05 | 04:02–07:42 | 0.15 | 21(9) | 6 (3) | 0.03 |
| Quick returns3 | 05:22 | 03:19–07:31 | 05:50 | 03:53–08:17 | 0.06 | 17 (6) | 15 (7) | 1.00 |
| After evening shifts4 | 06:13 | 03:58–08:10 | 06:41 | 04:34–08:48 | 0.08 | 20 (8) | 11 (6) | 0.26 |
| After night shifts | 04:12 | 02:03–06:14 | 04:35 | 00:13–07:40 | 0.11 | 19 (8) | 10 (5) | 0.24 |
| After days off | 07:20 | 05:28–09:30 | 07:20 | 05:35–09:32 | 0.85 | 14 (6) | 21 (11) | 0.59 |
1Mann-Whitney U-test, 2Fisher’s exact test, 3Between evening and morning shift (n=84; HJS n=37, LJS n=47), 4Includes double shifts (morning and evening shift).
Sleep efficiency (SE) was more often reduced (<85%) before morning shifts in the HJS-group than LJS-group (21 vs. 6%, p=0.03) but not on average or in connection with other work shifts, quick returns (Table 2) or the pre-selected shifts. The average SEs were similar in both stress groups (HJS 89%, range 82–94% vs. LJS 89% range 84–95%) and SE varied very little in connection with different work shifts, being highest after night shifts (HJS 88%, range 81–94% vs. LJS 90%, range 79–96%).
The proportion of nurses with insufficient sleep was 38% in the HJS-group and 25% in the LJS-group, but the difference did not to reach statistical significance (p=0.15). The proportion of nurses’ who often had difficulties initiating sleep when working shifts, was higher in the HJS-group than in the LJS-group (p<0.01). Within shift categories this difference was observed in connection with evening shifts (p=0.01). Furthermore, the proportion of nurses having difficulties initiating sleep after waking up during the night was larger in the HJS-group than the LJS-group (p=0.03). The occurrence of any sleep disturbance at least 2–4 times a week was somewhat higher in the HJS-group, than in the LJS-group, but the difference did not reach statistical significance (p=0.15) (Table 3). No other stress group differences were found in sleep disturbances.
| High Job Strain | Low Job Strain | p-value1 | ||||
| % | (n) | % | (n) | |||
| Insufficient sleep2 | 38 | (16) | 25 | (13) | 0.15 | |
| Any sleep disturbance | ||||||
| 2–4 times/wk | 76 | (32) | 62 | (33) | 0.15 | |
| ≥5 times/wk | 31 | (13) | 25 | (13) | 0.49 | |
| Often difficulties in initiating sleep | ||||||
| All shifts | 76 | (32) | 42 | (22) | <0.01 | |
| Before morning shifts | 36 | (16) | 25 | (13) | 0.44 | |
| After evening shifts | 64 | (27) | 30 | (16) | 0.01 | |
| After night shifts | 24 | (10) | 19 | (10) | 0.19 | |
| After days off | 7 | (3) | 9 | (5) | 0.60 | |
| Often difficulties in initiating sleep after waking up | ||||||
| All shifts | 76 | (32) | 55 | (29) | 0.03 | |
| Before morning shifts | 48 | (20) | 32 | (17) | 0.45 | |
| After evening shifts | 45 | (19) | 28 | (15) | 0.26 | |
| After night shifts | 62 | (26) | 43 | (23) | 0.32 | |
| After days off | 19 | (8) | 13 | (7) | 0.78 | |
1Pearson χ2, 2Actual sleep amount ≤80% of subjective sleep need.
Approximately two thirds of the participants never used sleep promoting medication. The use of medication was lower during the past three months (HJS 12 vs. LJS 5%, p=0.08) than during the three-week field measurements (21 vs. 12%, p=0.27).
NappingNapping was very common; according to the sleep diaries, 93% (n=88) of the nurses took at least one nap and 22% (n=21) took naps at least twice a week. Total sleep length per 24 h increased only with few minutes with naps included (HJS 06:52 h vs. LJS 07:00h, p=0.30). Shift-specific sleep lengths of main sleep periods showed no significant difference between nappers and non-nappers; nappers slept on average 5 minutes longer before morning shifts and 15 minutes longer after night shifts than non-nappers.
Napping before the first night shift was common, and the proportion of nappers was higher in the LJS- than in the HJS-group (72 vs. 45%, p<0.01). The average nap duration before night shift was shorter in the HJS-group than in the LJS-group (35 vs. 62 min, p=0.01). The frequencies or durations of naps showed no other statistical differences between the stress groups (Table 4). Less than one third (29%, n=18) of those who had at least two consecutive night shifts, took naps between two consecutive night shifts. Taking naps during the night shift was exceptional, as only 4% had slept on duty at least once.
| Napping frequency | Nap duration (min) | |||||||||||
| High Job Strain | Low Job Strain | p-value1 | High Job Strain | Low Job Strain | DF | t-value | p-value | |||||
| % | (n) | % | (n) | Mean | SD | Mean | SD | |||||
| Nappers2 | 91 | (38) | 94 | (50) | 0.70 | 37 | (42) | 45 | (31) | 93 | –1.12 | 0.263 |
| After morning shift | 67 | (28) | 59 | (31) | 0.52 | 18 | (31) | 17 | (24) | 93 | 0.24 | 0.813 |
| Before 1st night shift | 45 | (19) | 72 | (38) | <0.01 | 35 | (59) | 62 | (68) | – | – | 0.014 |
| On a day off | 67 | (28) | 64 | (34) | 0.80 | 21 | (29) | 29 | (35) | 93 | –1.05 | 0.303 |
1Pearson χ2, 2At least once during 3-wk measurement, 3Independent samples t-test, 4Mann-Whitney U-test.
The proportion of nurses with at least one PVT lapse in the night shift was higher in the HJS-group than in the LJS-group (40 vs. 26%, p=0.02, controlled with education). There were no other statistically significant differences in the occurrence of lapses in PVT tests on workdays. However, the day off test showed a higher proportion of nurses with at least one lapse in the HJS-group (39 vs. 20%, p=0.03) (Fig. 2), but the difference was not statistically significant with education as a covariate. Mean PVT reaction times were similar in both job strain groups. Napping before or during the night shift before PVT test had no effect on the results.
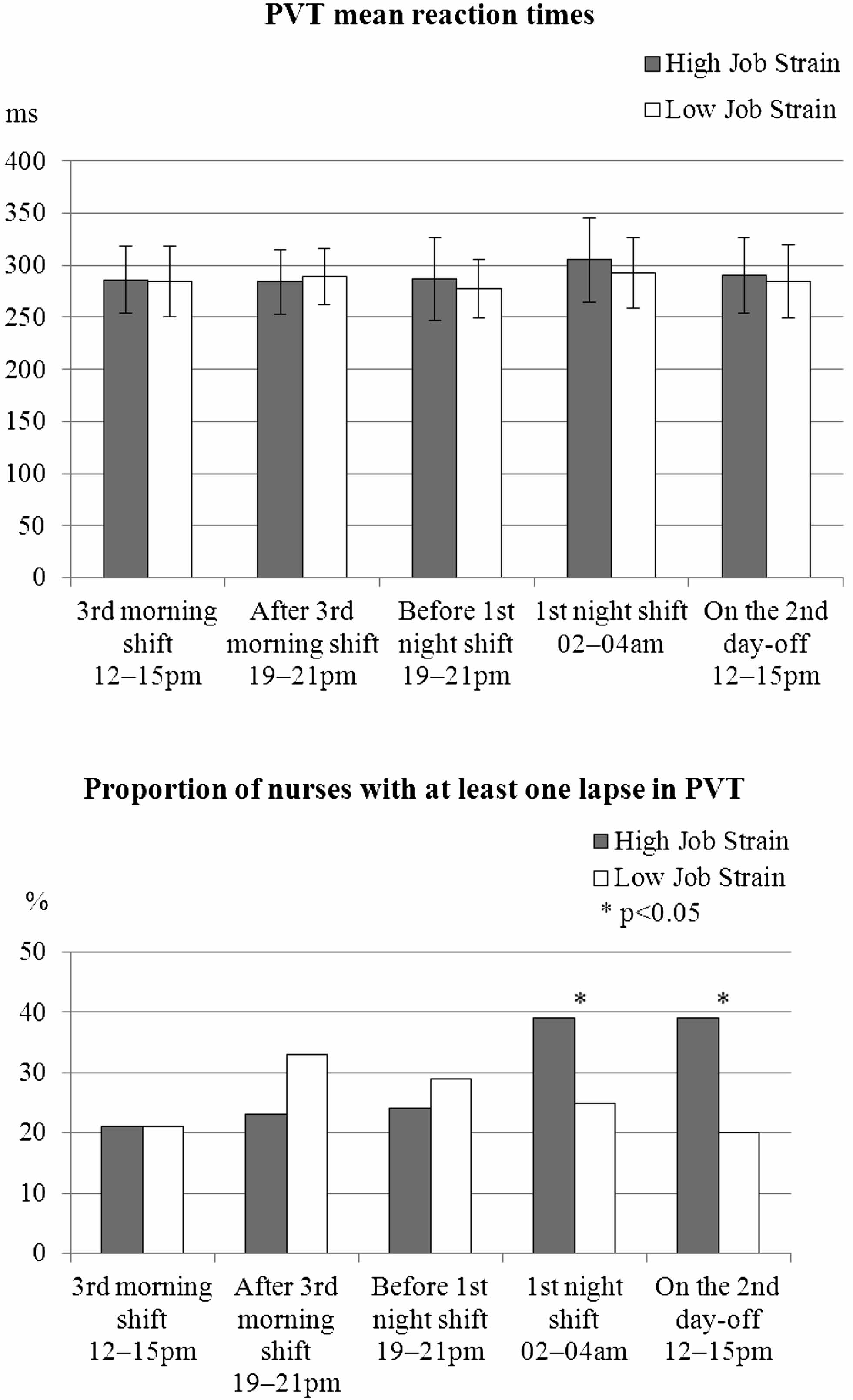
The mean reaction times with standard deviations and proportions participants with at least one PVT lapse in pre-selected shifts.
We repeated analyses with age and education level as covariates with no essential change in the results.
This is the first study to examine the relationship of exposure to job strain on shift-specific sleep quantity and quality, and alertness among shift working health care personnel. The results showed that job strain was associated with increased difficulties in initiating sleep in relation to all work shifts and especially after evening shifts. Reduced sleep efficiency was more common in the high-strain group before morning shifts. Job strain was related with higher amount of PVT lapses during the night shift and less and shorter naps before the night shift. Contrary to our hypothesis there were no general differences in sleep length or sleep efficiency according to job strain indicating that the additional burden of job strain becomes visible only in specific shift combinations.
We found job strain-related increases in sleep complaints in situations where shift workers typically face insomnia: sufficient napping before a night shift, daytime sleep after a night shift -or while going to sleep after evening shifts21,22,23). Few studies have investigated the effect of evening shifts on sleep33). Sleep difficulties after evening shifts are probably due to work rumination19) and inability to relax after a shift ending too close to sleep14). In addition to the earlier results19,20,21), in this data difficulties in initiating sleep after waking up were also more common in the HJS-group.
In concordance with our hypothesis and earlier evidence17, 34), shortened sleep and mild sleep disturbances were highly prevalent among shift workers. The participants’ sleep measured with actigraphy was on average half an hour shorter than all shift working nurses in Finnish Public Sector Study (n=7,023) and almost an hour shorter than a survey of Finnish women shows (7:37h)34). The total sleep amount increased only by a few minutes with self-reported naps added to the average sleep length, likewise to the study of Ruggiero et al.35). About 30% of the nurses had an insufficient sleep length, which is similar to the study of Åkerstedt, Ingre, Broman & Kecklund36).
Job strain is associated with disturbances in the sleep-wake pattern. Our results in both job strain groups are in line with the findings of shift working: night shifts and morning shifts are particularly obstructing for sufficient sleep36,37,38). Also, in this study the sleep length was longer after the evening shift than after the morning or night shift. Participants’ sleep after night shifts was less than five hours, which is in agreement with research showing sleep shortening by 1–4 h after a night shift22, 39). Approximately six hours of sleep before a morning shift is comparable with earlier research reporting 2–4 h shortening of sleep38) before early morning shifts.
Job strain induced additional sleep complaints to these shift workers mainly after evening shifts and in napping before the first night shift. However, there were no significant differences in total sleep length, sleep efficiency or napping between the groups. After evening shifts, the difference in sleep length between the job strain groups was less than 30 min while sleep curtailment for all participants after night shifts was almost three hours compared to days off. We thus conclude that the role of work strain on the sleep of shift workers is probably of lower significance than the effect of shift working in general.
Job strain affected napping; there was a significant difference between the job strain groups in taking naps before the first night shift. In this data, two thirds took a nap before the first night shift. Earlier research has shown 56% of nurses and nursing assistants in a similar shift system nap before first night shift40). Among midwifes 40% of the night shifts were preceded with a nap41). Approximately one third of shift workers nap between the consecutive night shifts33, 36) but there are no earlier studies of the effect of job strain on napping. According to Härmä et al.40), non-napping nurses before a night shift had more insomnia symptoms. It is presumable work-related stress with difficulties in falling asleep is associated with poorer ability to nap before first night shift. Also non-optimal time for falling asleep may affect to ability to nap. Even then, majority of nurses in our data used naps to prepare themselves for the first night shift, probably from the experiences of severe sleepiness in the first night shift.
In previous studies of dayworkers42), high mental distress frequently was associated with reduced sleep efficiency. However, in study of shift workers, the shortened sleep of shift workers was often compensated for by high sleep efficiency43).The sleep efficiencies in this study were above 85% which is an indication of a consolidated sleep. The proportions of reduced SE did not differ between the stress groups in connection with the other work shifts except for morning shifts. Moreover, actigraphy measurement of sleep length measurement slightly overestimates total sleep time44). This strengthens the observation that shift working nurses suffer from insufficient sleep and the actual sleep durations are likely to be even shorter than reported in the present study. The 12% use of sleep promoting medication in the LJS-group equals the sleep medication use reported in a population study of Scandinavian females45). One fifth of the HJS-group used sleep medication during the field measurements, which equals to other study among the nursing staff46). We suggest that nurses may use sleep promoting medication to avoid cumulative stress and sleep deprivation.
There is lack of research of alertness in connection with work stress. In our data, the occurrence of at least one lapse in PVT was higher in high than low-strain nurses in the night shift. Importantly, these night shift tests were conducted in circadian rhythm and recovery controlled pre-selected shift arrangements, where sleepiness was pronounced in the HJS-group only. During night shift, especially the high-strain nurses might benefit from planned naps, which suppress sleepiness47, 48). However, job strain was not associated with other PVT scores. A recent study35) found no differences between night shift and day shift nurses in a standard 10-min PVT either.
As a whole, the associations of job strain with sleep in shift working health care staff were fewer than predicted based on earlier results21,22,23). In this group of shift workers, the additional burden of job strain on sleep and alertness becomes evident only in specific shift combinations. The effects of job strain on sleep may be emphasized among day workers19) and workers with extended work hours49).
Strengths and limitations of the studyThe strengths of this field study nested in on-going epidemiological study among nursing staff are: firstly, the measure of exposure to job stressors was based on a mean score from the same ward. This was likely to result in reduced effect of subjectivity on the measure and therefore in a less biased estimate of the environmental job strain.
Secondly, we used both actigraphy and sleep diary data to estimate the habitual sleep length, whereas many earlier studies only have sleep diary data38). Furthermore, the three-week actigraphy measurement period was of longer duration in this study than in most other studies, where such measurements have lasted mainly up to 7 nights.
The participants formed a homogenous sample of employees, which can be considered as a clear strength of the study. Our participants were highly very similar in aspects other than job strain: they were all relatively healthy shift working females who, for example, had similar amount of work hours and only two of them scored points typical for clinical depression. Thus, it is not likely that there were non-measured confounding factors between the groups. There was a significant difference between the stress groups in education level that had no confounding effect on sleep results.
There are some limitations in our study as well. The study sample of nursing employees was likely to result in reduced variance of job strain and power to establish clear cut between groups in sleep and alertness. High and low job strain groups did not differ in their level of stress as much as high and low stress groups typically do in studies of the general population or mixed occupational groups. Among nursing staff, the concept of low strain is relative, when for example majority of nurses in both groups had to often hurry at work.
Although we used exposure data from a prospective data set the design of analyzing the effect of job strain on sleep was cross-sectional, prohibiting us to draw conclusions regarding causality. Job Content Questionnaire was used to assess job strain at one time point, preventing us to follow changes in exposure to environmental job strain or capture the past pattern of exposure other than the participants had been working in the same ward for at least three years. Using the average job strain level of a ward may be a potential weakness if the atmosphere in the workplace is affected by influential individuals in the ward.
Polysomnography would have been an ideal method to detect changes in sleep, as stress has been shown to affect sleep architechture i.e. amount of slow wave sleep and REM sleep and number of awakenings50). We used a 5-min PVT instead of a 10-min PVT for practical reasons in the workplaces. Although the 5-min test is a viable alternative to the standard 10 min test, it may be less sensitive to detect sleepiness51). Nevertheless, the job strain group difference came up in the night shift, but the test might be too short to detect sleepiness in day-time tests. A useful addition to the data gathered would have been the social support aspects of the JCQ as well as personality factors to shift work tolerance. Also, it would have been useful to utilize the voluntary or involuntary nature of naps.
One third of the contacted individuals declined to participate in the study and only 24% of the employees fulfilling the inclusion criteria participated. We had no personal contact with potential study participants, which meant that we could not verify whether the nurses were actually reached or not. Also, the considerable time commitment that the study required has likely reduced the participation rate. On the other hand, the participated nurses represented the invited nurses and the field data collected was of very good quality; only a few (4%) participants refused or failed to follow through with the field measurements. More volunteers were from the LJS-group, and it is probable that most affected individuals were unwilling to participate52), which may have diluted the differences observed between the stress groups.
In future nested studies, it would be important to obtain a personal contact to potential study participants to enhance the participation rate. Apparently, when measuring the level of low job strain in health care staff or other homogenous samples, the concept of low strain is relative and the differences between high and low stress groups are likely to be rather limited. Therefore, larger sample sizes would be needed to detect group level differences in job strain. Quitting night shift work was common in this cohort of nursing professionals and it would be advantageous to study that group too.
Sufficient sleep is important to all shift workers due to its implications to alertness, recovery and health. More longitudinal studies exploring the effects of job strain on sleep and irregular working times are needed, because impaired sleep is associated with severe consequences like occupational injuries, reduced patient safety, and increased risk of development of several chronic diseases. Ability to control over own work times and sufficient recovery time between work shifts are useful in reducing occupational stress and related health outcomes53).
High job strain is associated with difficulties initiating sleep and reduced psychomotor vigilance in night shifts. Shift working contributed to impaired sleep in both high and low job strain group. Individual and organization-based actions are needed to promote good and sufficient sleep in shift working nurses, especially with high job strain.
This study was funded by The Academy of Finland (projects 124473, and 132944), The Work Environment Fund (project 107156), The SalWe Research Program for Mind and Body (TEKES -the Finnish Funding Agency for Technology and Innovation, grant 1104/10), the EU New OSH ERA and ERA-AGE2 Research Programmes. Mika Kivimäki is supported by a professorial fellowship from the Economic and Social Research Council, UK.
We thank Elise Koskenseppä for participant recruitment, Nina Lapveteläinen and Riitta Velin for arrangements for the field measurements, and Hanna Kaisa Hyvärinen and Jaana Pentti for statistical support.