2013 Volume 51 Issue 6 Pages 603-611
2013 Volume 51 Issue 6 Pages 603-611
An objective of this study is to search how physical examination and diet consultation can influence those risk factors of cardiovascular disease. The subjects were 326 pilots of the “B” airline company in Korea whose total cholesterol values were over 220 mg/dl on their regular physical examinations from April 2006 to December 2008. They were divided into two groups, one who had diet consultation (an intervention group) and a control group. The physical examination components used to each group were body mass index (BMI), total cholesterol (TC), high density lipoprotein (HDL), low density lipoprotein (LDL) and triglyceride (TG). The behavioral, anthropometric and biomedical measurements were collected at each visit. This study compares and investigates the changes of serum cholesterol and also the health-behavior at each physical examination. Within the intervention group significant improvements were observed for total cholesterol, BMI (body mass index) and HDL (high density lipoprotein). The normalizing rates for cholesterol level to decrease down to lower than 200 mg/dl were 17.7% in intervention group and 8.7% in control group, which is statistically significantly higher among the intervention group. The odds ratio of diet consultation was 2.80 (95% CI=1.35–5.79), which indicates that it is a significantly contributing factor to normalize the serum cholesterol value down to lower than 200 mg/dl. Based on result, it is recommended to have regular physical examination and intensive management with diet and exercise consultation.
Among air crews in aviation industry, pilots particularly are responsible for transporting the passengers and the safety of flight and, therefore, must not only have sufficient flight experience and capability of controlling the aircraft but also maintain physical conditions appropriate for flight duties. In order to evaluate the physical aptitude of the air pilots for flight duties, the International Civil Aviation Organization (ICAO) has established a standard for physical examination of air crews which was recommended to every country1). According to the regulation stipulated in this standard, each country is responsible to monitor the physical conditions of pilots and issue physical examinations certificates. In conformity with this regulation, Korea has designated specialized doctors for physical examinations of air pilots who regularly performs physical examinations of air pilots in accordance with the physical examinations standard and evaluate the aptitude of pilots for flight duties2).
However, this standard specifies only the minimum requirements for the safety of aviation. Private airline companies are applying stricter regulations in physical examinations spending more than fifty thousand dollars per pilot for examinations as well as comprehensive health care in order to ensure that they maintain optimal health throughout their service time for the safety of hundreds of passengers3). Those airline companies with in-house medical centers using it for systematic health control, in fact, show low inaptitude-for-flight-duties rate of compared with other airliners who are, therefore, applying their own health control standards to ensure that air pilots are kept in finest health conditions4). In the United States, implementation of effective health control programs by airliners did reduce medical inaptitude-for-flight-duties rate to one third of previous rate resulting in annual saving of 6 million dollars5).
Cardiovascular disease has been universally known as the most common cause of temporary non-flight duty (duty not involving flight) and permanent grounding of air pilots. A study on permanent grounding cases of air pilots in Korea for the past 21 yr (1970−1990) revealed that cardiovascular diseases and malignant tumors were the most significant medical reasons for permanent grounding covering 27% of overall cases6) and cardiovascular diseases was reported as the most frequent cause (50%) of permanent groundings of pilots over the age of 45 in the airliners in the United States7). Cardiovascular diseases are indeed the medical conditions that most seriously threaten the safety of aviation because they can cause sudden pilot incapacitation or death during flight8, 9).
Some of the risk factors for cardiovascular diseases including hypertension, smoking, high cholesterols blood, lack of physical exercise, obesity, diabetes are known to be corrigible by many studies carried out since the Framingham Heart Study which is a long-term, ongoing cardiovascular study on residents of the town of Framingham, Massachusetts10). These various risk factors for cardiovascular diseases can be treated with good dietary habit, regular exercise, non-smoking, moderation in drinking and weight control11,12,13). Dietetic therapy, in particular, is very important in preventing and treating the cardiovascular diseases14, 15).
Therefore, it is very important to control hyperlipidemia an independent risk factor for cardiovascular diseases, and reduce the related risk factors in order to maintain the cardiovascular health of pilots whose duties have such vocational requirements that can cause irregular mealtime due to personal flight schedule, mental stress about the safety of flight and imbalance of biorhythm due to long light and time difference. There have been some studies on risk factors relating to the blood concentration of lipid, but virtually no analytic study on the management of blood cholesterol or preventive intervention against cardiovascular diseases.
Therefore, this study aims to provide basic data for future development of cardiovascular diseases prevention program for air pilots by analyzing the possibility of regular physical examinations and dietary counseling in the correction of the risk factors of cardiovascular diseases in pilots of the “B” airline company who have high risk of hyperlipidemia with more than 200 mg/dl of total blood content of cholesterol. The objective of this study is to identify the factors that can affect the change and normalization of total blood content of cholesterol and to examine the effects of physical examinations and dietary counseling on blood content of lipid and health behavior.
Just over 1,800 pilots were employed at the “B” airline company in April, 2006. Among pilots of the “B” airline company who took regular physical examinations during the period from April 16, 2006 until December 31, 2008, total 326 pilots who found to have more blood content of total cholesterol of over 220 mg/dl and to have no experience of dietary counseling were selected as the subjects of this study. Among them, 130 pilots received dietary counseling for the first time as prescribed by the doctor and other 196 pilots did not. Those who resigned during the study period or were taking drugs which would affect this study results or have history of hypertension, diabetes and thyroid disease were excluded. All the pilots who participated in this study were voluntary and their written informed consents were obtained prior to study initiation. The experimental protocol related to this study was approved by the ethics committee of Yonsei University, Republic of Korea.
Procedure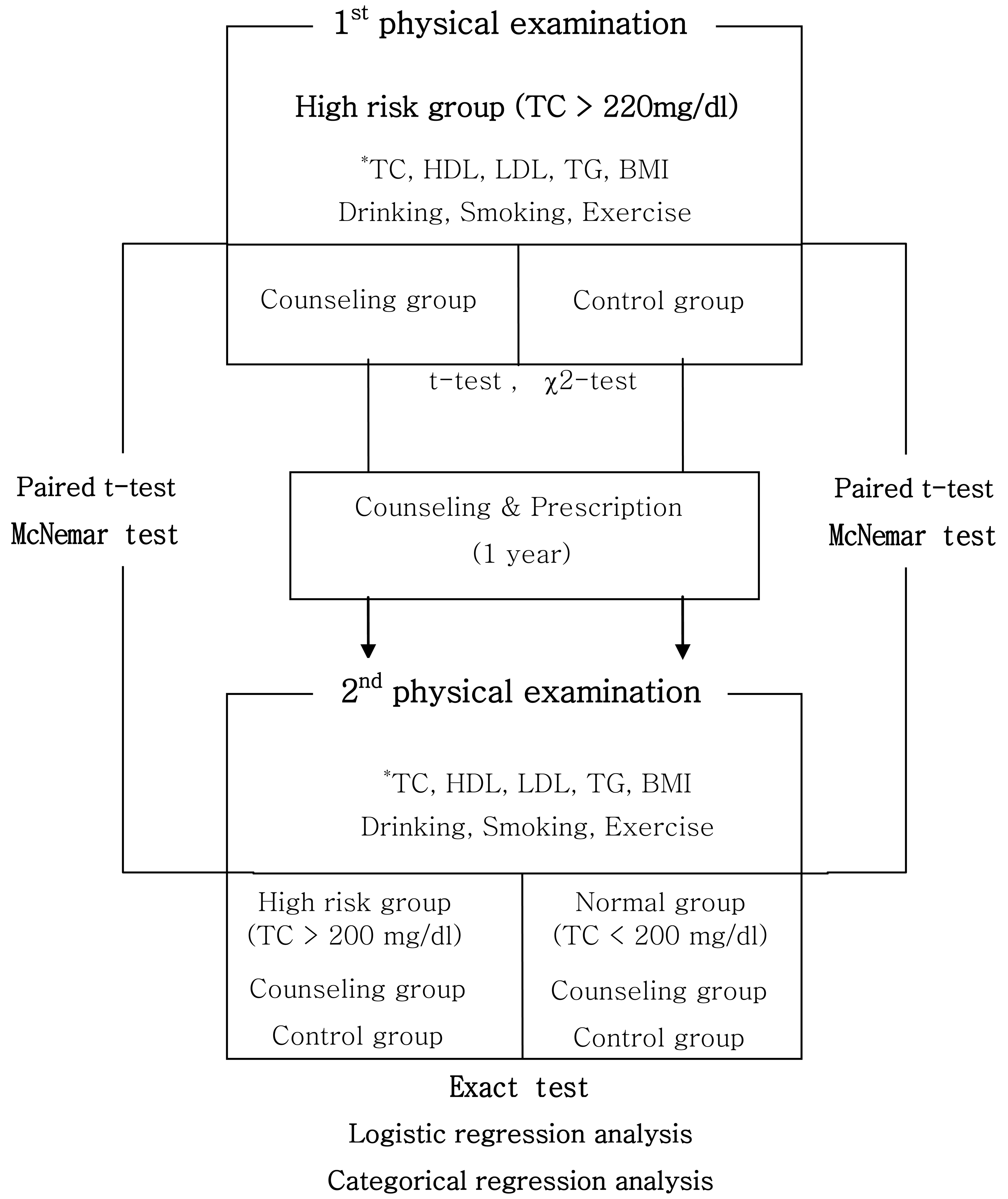
Flow chart of this study procedure.
*TC : Total cholesterol, HDL : High-Density Lipoprotein, LDL : Low-Density Lipoprotein, TG : Triglyceride, BMI : Body Mass Index.
Personal records and computer data on regular physical examinations performed in the “B” airline company were used as the base data for this study. The subjects, who have over 220 mg/dl of total blood content of cholesterol and are at the risk of hyperlipidemia, were divided into two groups, “the intervention group” who have received dietary counseling for the first time and “the control group” who did not receive any dietary counseling, at the time of subject screening. As shown in the Fig. 1, the results of physical examinations performed and health behavior of the subject at the time of the screening of subjects were compared and analyzed with the results of the next physical examinations and health behavior after counseling and prescription conducted for one year since the 1st physical examination. The rates of normalization of total cholesterol content to below 200 mg/dl in the intervention and control group were compared and the factors that independently affect the changes in blood content of lipid were analyzed.
Method of investigation and measurement InvestigationOn each physical examination date, physical measurements of height, weight and body mass index (BMI) were taken for each subject as well as measurements of total cholesterol (TC), high density lipoprotein (HDL), low density lipoprotein (LDL) and triglyceride (TG). Personal data about age, title, work period, smoking, drinking and exercise activities were provided by the subject as guided by the investigator. For intervention group, data about nutrition counseling education and prescription were also collected from each subject.
MeasurementMeasurements of height and weight were taken using an automatic height/weight measuring instrument when the subject is wearing thin cotton trousers and a gown without shoes. BMI was measured as an obesity index calculated from the equation, weight (kg)/height (m) square and obesity was defined for the measurement value of over 25, overweight for over 23 but less than 25 and normal for below 23.
Blood tests were performed at the clinical laboratory of the “B” airline company using the blood samples taken from antecubital vein after fasting for more than 8 h. Biochemical measurements (TC, HDL, LDL and TG) from blood samples were taken using automatic analyzer of HITACHI model 7170 from April 2008.
For the collection of health behavior data, subjects were divided into non-smokers, abstinent smokers and smokers and the amount of smoking was recorded for the smokers and abstinent smokers. For drinking behavior, subjects were divided into drinkers and non-drinkers and the frequency and the amount of drinking were recorded for the drinkers. Exercise activities were recorded in the frequency and the duration of exercise for those who regularly perform exercises.
The doctor specialized in aviation health performed nutrition counseling and evaluated the general results of biochemical tests (TC, HDL, LDL and TG), BMI and individual health behavior to provide nutrition prescription on the physical examination day. After physical examination, nutrition counseling was carried out at the nutrition counseling room by a clinical dietitian who performed 1:1 counseling and provided dietary prescription. The contents of educational counseling consisted of survey on individual nutritional intake, evaluation of dietary habit, identification of dietetic problems, education on dietetic therapy related to hyperlipidemia and provision of individual dietetic prescription and leaflets about related diseases.
Analysis methodIn this study, the subjects who were at the risk of hyperlipidemia with TC of over 220 mg/dl were divided into the nutrition intervention group and the control group. After evaluating the homogeneity of the two groups using t-test and χ2-test, BMI, blood lipid profile and health behavior at the time of the first and the second physical examinations were analyzed using paired t-test and McNemar test. The rates of normalization of TC to below 220 mg/dl were then compared between the intervention group and the control group using exact test. In order to examine the contribution of nutrition counseling to the normalization of TC, the subjects were divided into sub-groups of those who experienced normalization of TC to below 200 mg/dl and those who did not at the second physical examination and these groups were then subjected to a logistic regression analysis controlling for age, position and work period. Multiple regression analysis was used to examine the effects of each factor on the changes in TC. The analysis of all the data was performed using SPSS 13.0.
| Intervention group (n=130) | Control group (n=196) | Total (n=326) | p-value* | ||
|---|---|---|---|---|---|
| Age (year) | 30–39 | n=61 (46.9%) | n=51 (26.0%) | n=112 (34.4%) | <0.001 |
| 40–49 | n=43 (33.1%) | n=81 (41.3%) | n=124 (38.0%) | ||
| 50–59 | n=26 (20.0%) | n=64 (32.7%) | n=90 (27.6%) | ||
| Position | Captain | n=65 (50.0%) | n=105 (53.6%) | n=170 (52.1%) | 0.075 |
| F/O | n=63 (48.5%) | n=78 (39.8%) | n=141 (43.3%) | ||
| FE | n=2 (1.5%) | n=13 (6.6%) | n=15 (4.6%) | ||
| Work period (year) | <10 | n=63 (48.5%) | n=65 (33.2%) | n=128 (39.3%) | 0.042 |
| 10–19 | n=57 (43.8%) | n=112 (57.1%) | n=169 (51.8%) | ||
| >20 | n=10 (7.7%) | n=19 (9.7%) | n=29 (8.9%) | ||
*χ2- test.
All the subjects were males of whom 38.0% was in their 40s, 34.4% in 30s and 27.6% in 50s. 51.8% of the subjects, the largest group, had the duration of employment of 10–19 yr. The number of subjects who received nutrition counseling intervention and who did not show significant difference between age and title sub-groups and the proportion of the intervention group was higher in younger subjects (Table 1).
Comparison of 1st physical examination result and health behavior between intervention and control group| Intervention group (n=130) | Control group (n=196) | p-value* | |
|---|---|---|---|
| TC (mg/dl) | 238.55 ± 13.83** | 234.45 ± 12.22 | 0.007 |
| HDL (mg/dl) | 49.71 ± 10.93 | 52.34 ± 11.63 | 0.041 |
| LDL (mg/dl) | 159.36 ± 17.36 | 152.54 ± 13.86 | <0.001 |
| TG (mg/dl) | 158.45 ± 97.25 | 150.51 ± 68.63 | 0.388 |
| BMI | 24.8 ± 2.18 | 24.26 ± 2.00 | 0.023 |
| Weight (kg) | 74.56 ± 8.03 | 72.07 ± 7.96 | 0.006 |
| SBP (mmHg) | 118.35 ± 9.75 | 117.71 ± 13.62 | 0.645 |
| DBP (mmHg) | 75.25 ± 7.48 | 75.79 ± 9.18 | 0.574 |
| FBS (mg/dl) | 94.58 ± 8.60 | 93.95 ± 8.91 | 0.526 |
*t-test ; **Mean ± SD.
Table 2 indicates a comparison of 1st physical examination result between intervention and control group. The values of TC, LDL, weight and BMI were significantly higher in intervention group than those in control group (p<0.01, p<0.001, p<0.05 respectively) whereas the value of HDL in intervention group was significantly lower than control group (p<0.05).
Comparison of physical examinations results between the intervention group and the control group| 1st result | 2nd result | t | p-value* | ||
|---|---|---|---|---|---|
| Intervention group | TC (mg/dl) | 238.55 ± 13.83** | 222.20 ± 22.01 | 8.13 | <0.001 |
| HDL (mg/dl) | 49.71 ± 10.93 | 48.68 ± 11.15 | 6.65 | <0.001 | |
| LDL (mg/dl) | 1,159.36 ± 17.36 | 145.63 ± 19.03 | 1.8 | 0.074 | |
| TG (mg/dl) | 158.45 ± 97.25 | 147.25 ± 83.35 | 1.62 | 0.107 | |
| BMI | 24.80 ± 2.18 | 24.54 ± 2.17 | 3.39 | 0.001 | |
| Control group | TC (mg/dl) | 234.45 ± 12.22** | 222.17 ± 16.99 | 10.96 | <0.001 |
| HDL (mg/dl) | 52.34 ± 11.63 | 51.3 ± 11.20 | 9.81 | <0.001 | |
| LDL (mg/dl) | 152.54 ± 13.86 | 142.24 ± 15.94 | 2.48 | 0.014 | |
| TG (mg/dl) | 150.51 ± 68.63 | 149.92 ± 70.63 | 0.13 | 0.895 | |
| BMI | 24.26 ± 2.00 | 24.24 ± 2.00 | 0.54 | 0.591 | |
*paired t-test; ** Mean ± SD.
As shown in Table 3, the results of physical examinations before and after the nutrition counseling in the intervention group showed that the values of TC and BMI have been significantly reduced at the second examination compared with the values measured at the first examination (p<0.001, p=0.001 respectively). The values of HDL increased with statistic significance (p<0.001). On the other hand, the comparison between the results before and after the nutrition counseling in the control group who did not receive nutrition counseling revealed statistically significant decrease in TC and LDL (p<0.001, p=0.014 respectively) and statistically significant increase in HDL (p<0.001) in general.
Comparison of normalization of total blood concentration of cholesterol relative to the performance vs. non-performance of counseling| Intervention group | Control group | p-value* | ||
|---|---|---|---|---|
| Total | Abnormalization | n=107 (82.3%) | n=179 (91.3%) | 0.015 |
| Normalization | n=23 (17.7%) | n=17 (8.7%) | ||
| 220≤TC<240 | Abnormalization | n=60 (80.0%) | n=125 (88.0%) | 0.113 |
| Normalization | n=15 (20.0%) | n=17 (12.0%) | ||
| 240≤TC | Abnormalization | n=47 (85.5%) | n=54 (100.0%) | 0.006 |
| Normalization | n=8 (14.5%) | n=0 (0.0%) | ||
*exact test.
Normalization rates of the blood content of total cholesterol to below 200 mg/dl in both groups were examined and the results showed 17.7% of normalization in the intervention group and 8.7% in the control group indicating significantly higher normalization rate in the intervention group (p=0.015). The content of cholesterol in each level was normalized in 8 subjects in the intervention group (14.5%) who originally had TC level of over 240 mg/dl, compared with the control group in which no subject showed normalization (p=0.006) (Table 4).
Factors for normalization of total blood content of cholesterol| β | SE | OR* | 95% CI | ||
|---|---|---|---|---|---|
| BMI | (23≤BMI<25) | 0.22 | 0.47 | 1.24 | 0.5–3.11 |
| (BMI≥25) | 0.08 | 0.49 | 1.09 | 0.42–2.82 | |
| Smoking | −0.36 | 0.38 | 0.69 | 0.33–1.46 | |
| Drinking | 0.09 | 0.38 | 1.1 | 0.53–2.29 | |
| Exercise | (<90 min/week) | 0.44 | 0.68 | 1.55 | 0.4–5.92 |
| (>90 min/week) | 0.86 | 0.67 | 2.36 | 0.64–8.76 | |
| Intervention group | 1.03 | 0.37 | 2.80** | 1.35–5.79 | |
*adjusted for age, position and work period. **adjusted for lifestyle factors (smoking, drinking and exercise).
In order to analyze the factors for the normalization of the blood content of total cholesterol, logistic regression analysis was performed to find the odd ratio using BMI and health behavior as independent variables and the normalization or non-normalization of TC as a dependent variable. Nutrition counseling was found to be the factor that most significantly contributed the normalization of TC with the odd ratio of 2.80 (95%CI=1.35–5.79) (Table 5).
Factors for changes in total blood content of cholestrol| β | SE | p-value | |
|---|---|---|---|
| Age | −0.354 | 0.190 | 0.071 |
| Drinking | −0.123 | 0.142 | 0.390 |
| Smoking | −0.213 | 0.139 | 0.135 |
| Exercise | −0.379 | 0.131 | 0.001 |
| BMI | −0.118 | 0.146 | 0.425 |
| Position | 0.488 | 0.190 | 0.003 |
| Counseling | −0.036 | 0.137 | 0.797 |
Adjusted R2=0.215.
In order to examine the degree of contribution of each variable to the changes in total cholesterol, the changes in BMI and total cholesterol were categorized as numeric variable, the amount of drinking, smoking and the duration of exercise as ordered variables and the tile and nutrition counseling or non-counseling as nominal variables and categorical regression analysis was performed using the change in total cholesterol as a dependent variable. Results showed negative change (more decrease) in total cholesterol as the duration of exercise increased (p=0.001) and positive change (less decrease) in order of chief pilot, deputy pilot and aviation engineer (p=0.003). The intervention group tended to show lower total cholesterol but was not statistically significant (Table 6).
Those at higher risk of hyperlipidemia were generally older. Participants who undertook the counseling and exercise intervention were more likely to decrease their total cholesterol, BMI (body mass index) and HDL (high density lipoprotein) than those who were in the control group. These findings were similar to those of previous studies related to diet consultation and exercise intervention and can vary according to sample size, ethnicity and cultural reasons.
The activities of medical section in an airline company are different in each airline and in each country, but the prolongation of useful pilot life is the common purpose of health management in private aviation companies16). Cardiovascular disease is one of the common causes of permanent grounding or transfer to the duty not involving flight of air pilots and is also the most serious threat to the safety of flight17). As these diseases result in serious disabilities and aftereffects once they occur, preventive intervention against cardiovascular diseases has been considered as a very important issue. All the non-medication methods used to control these diseases are related to ‘life style modification’ which indicates that appropriate life style is an effective treatment value and the term emphasizes the importance of putting appropriate life style into practice18).
The composition of the subjects of this study who are at risk of hyperlipidemia consisted of 38% in their 40s and 34.2% in 30s indicating high risk in the ages below 50. Such a characteristic is considered to have been the result of rapid increase in blood content of cholesterol and intake of fatty foods for the past 20 yr. This trend is more announced in younger ages that have increased proportion of individuals at the risk of hyperlipidemia.
Comparison of physical examination results between the intervention group and the control group performed for the analysis of the effects of regular physical examinations and nutrition counseling revealed significant change in blood content of lipids in both groups. Blood content of total cholesterol and BMI decreased significantly in the intervention group while blood content of total cholesterol and LDL-C decreased significantly in the control group. HDL-C showed statistically significant decrease in both groups. In a study on the effects of regular medical checkups on the correction of health risk factors in general public who were the patients of university hospitals19) showed similar results as those of this study in that abnormalities in the measurements of clinical factors including cholesterol, blood pressure and uric acid generally showed significant decrease. As the results of physical examinations is directly related to the issuance of physical examination certificate and the safety of flight under the specific circumstances of vocational characteristics of the study subjects who participated in lifetime health program, the subjects in this study have relatively higher interest in their health and are well motivated for disease control, particularly as all the subjects in both the intervention group and the control group are at risk of hyperlipidemia. Therefore, the subjects are thought to have been more aware of the necessity of practicing the hyperlipidemia control activities.
The commercial airline pilots have regular physical examination at least over once per one year according to international regulation and cannot perform airline operation duty if they are below the body standard based on physical examination result. Thus, they strive to pass the body standard by doing exercise and dietary management. There was significant difference of TC, LDL and HDL in the control group between 1st and 2nd physical examination although there is no dietary intervention by dietitian, which implies that pilots who received hyperlipidemia judgment by doctor try to do personal management prior to 2nd physical examination. Based on the result, physical examination is necessary for sustaining health condition of pilots.
The changes in drinking, smoking and physical exercise behaviors in the intervention group and the control group measured at the second physical examination did not show significant difference between the two groups indicating low long-term conformity with the change of life style. Many studies have been carried out as the efforts to reduce the health risks on the introduction of health checkup system, strengthening of health education and improvement of conformity with the recommendations to individuals by the doctor. However, the effects of these programs on the changes in life style are limited and usually short-term and decrease as the elapse of time, according to the reports20). The study by Kellerman et al.21) on the subjects who participated in lifetime health program also reported that voluntary participation in the program tended to have the effect of decreasing the risk factors in smoking, drinking, exercising and wearing safety belt but without statistic significance. In other words, changes are less realized where voluntary efforts are necessary, indicating that systematic programs are necessary to promote individual recognition of the requirements for health.
Some of the studies noted that individualized, specific intervention and recommendation, rather than health campaign targeting general public which tend to be unsuccessful, is more necessary for behavioral changes for the correction of risk factors in life style including dietary habit22). Nutrition counseling performed in this study consisted of 1:1 individual intervention and education by clinical dietitian who performed individual investigation and analysis of food intake, evaluation of dietary habit and provision of dietary prescription. This intervention is considered to have contributed to the normalization of blood content of total cholesterol in the subjects who are at risk of hyperlipidemia.
The results of categorical regression analysis using the change in total cholesterol level as an independent variable indicated statistically significant effect of increased exercise on the decrease of total cholesterol. Exercise generally promotes metabolism of sugar and its use by muscles and accelerates the use of fat in muscular tissues contributing the correction of factors for hyperlipidemia23). However, whilst appropriate amount is obviously know to be beneficial, prescription of the amount and the types of exercise is still to be studied further.
There are several limitations in this study. First, medical records on the evaluation of dietary habits of the subjects in the control group were not sufficient for the analysis of the effects of nutrition counseling, so detailed evaluation of risk factors in dietary habits and measures for improvement for the intervention group and the control group were not possible. Second, a prescription by doctor was determined based on biochemical test results (TC, LDL, TG and FBS), BMI and personal health behavior of subjects. However, two groups (intervention and control) were not selected with identical criteria because there is respective difference of prescription among doctors. Additionally the subjects’ participation interests in dietary consultation were not reflected perfectively to this study. They were voluntary and interested in the counseling and therefore perhaps more likely to listen to the counseling. Third, questionnaires were filled in by air pilots themselves and collected without personal confirmation procedure. Therefore, we had a limitation that some of the answers may have been manipulated to avoid individual disadvantage. Fourth, although nutrition counseling was given on 1:1 basis, long-term intervention was not possible due to vocational characteristics of the air pilots including different personal schedules. Therefore, voluntary participation in changed behavior was difficult with only short-term intervention. Additionally it is suggested that the further studies which can match intervention and control group based on age, position and work period should be performed henceforth to overcome the their differences at baseline between two groups. Furthermore, because the other factors, which were not measured in this study, to affect the level of TC are diet factors (fat, salt, sugar and caffeine intake) and flight time of aircrew, the further study regarding this subject should be performed in the future. Fifth, baseline adjustments of TC between intervention group and control group were not applied to these results. As a result, it should be considered that baseline differences of TC between intervention group and control group may be swaying the results obtained from this study. Finally, our finding that all the pilots investigated in this study were at high risk could be due to regression to the mean, which would be derived from that the baseline differences were our greatest limitation.
In conclusion, this study on the effects of physical examinations and nutrition counseling is considered meaningful in that it analyzed the risk factors related to cardiovascular diseases and guided the subjects of high risk to the improvement of life style that can lead to the prevention of cardiovascular diseases. Cardiovascular disease prevention program for air pilots in the future would be better employing the comprehensive, continuous preventive approach encompassing all the risk factors in one program instead of implementing separate risk factor reducing programs for individual risk factor (smoking, diet, exercise, etc). Such program should be structured based on health behavior theory employing, for instance, health recognition models. Also, in order to overcome the limitation posed by vocational characteristics of air pilots’ duties, method of providing health education programs overcoming the limitation of time and space should be developed.
The results obtained from this study were as follows:
First, results from the consecutive two physical examinations revealed statistically significant decrease of total cholesterol and BMI and statistically significant increase of HDL in the intervention group at the second physical examination after the nutrition counseling. In the control group, however, total cholesterol and LDL levels showed statistically significant decrease while HDL level showed statistically significant increase.
Second, the rate of normalization of blood content of total cholesterol in two groups, which were divided based on the provision or non-provision of nutrition counseling, was 17.7 in the intervention group and 8.7% in the control group indicating statistically significant high rate in the intervention group as compared with the control group.
Third, the only factor that significantly contributed to the normalization of blood content of total cholesterol to below 200 mg/dl was nutrition counseling that showed odd ratio of 2.80 (95%CI=1.35–5.79).
Fourth, Analysis of factors that have independent effects on the change in total cholesterol level in blood revealed statistically significant decrease of total cholesterol as the duration of exercise increased. Statistically significant increase of total cholesterol appeared in order of chief pilot, deputy pilot and aviation engineer.
In conclusion, it was found in this study that nutrition counseling was the significantly contributing factor for the normalization of blood content of cholesterol and the increased exercise was found to be the factor that has independent effect on the change in blood content level of total cholesterol.