2020 年 20 巻 2 号 p. 85-112
2020 年 20 巻 2 号 p. 85-112
The purpose of this study was to collect information on foot problems, current footwear use, and indoor footwear design preferences in patients with diabetes mellitus in Thailand. This descriptive study obtained data from 539 patients with type 2 diabetes who had moderate to high risk of developing foot ulcers. A self-reported survey covering patient characteristics, foot problems, current footwear use, and preferred indoor footwear designs was conducted. The qualitative data were analyzed using descriptive statistics. Variables related to footwear design were evaluated by Spearman's rank correlation. The results showed that 55.8% (n = 301) of respondents had been diagnosed as type 2 diabetes more than 10 years. Foot complications such as numbness, calluses, and ulcers were reported by 20%–65% of respondents. Nearly half the respondents (n = 252, 46.8%) walked barefoot, 38.5% (n = 207) wore slippers or flip-flops, and 5.4% (n = 29) wore clog shoes inside the house. Slippers or flip-flops (n = 230, 42.7%), closed shoes (n = 135, 25.2%), and clog shoes (n = 99, 18.4%) were the most commonly worn outdoor footwear. The most preferred indoor footwear design preferences were easy to wear (i.e., slip-on type) (n = 424, 78.8%), breathability (n = 282, 53.7%), and a flexible upper material (n = 167, 31.8%). However, only weak correlation between the characteristics of respondents and their indoor footwear design preferences was found. These findings suggest that a large proportion of patients with type 2 diabetes walk barefoot at home most of the time, which can lead to foot ulcers. Health care professionals should emphasize the benefits of using indoor footwear and avoiding walking barefoot whenever possible. Affordable and acceptable footwear that accommodates personal preferences should be designed for patients with diabetes, particularly for indoor activities.
Diabetic foot problems are common worldwide and affect a large number of patients and their families. In Thailand, the estimated prevalence of diabetes mellitus as of 2014 was 5 million in a population of 67 million. A marked decrease in the number of individuals living with type 2 diabetes in Asia is not expected to occur any time soon [1]. Inadequate management of diabetes has the propensity to increase the risk of significant complications, including diabetic foot ulcers [2].
In an effort to protect the foot from excessive pressure, at-risk patients with diabetes should be instructed not to walk barefoot, either with or without socks, nor in thin-soled standard slippers, whether at home or outside [3]. People with diabetes at moderate to high risk of foot ulceration should be encouraged to wear shoes or slippers at all times, both indoors and outdoors [4–5]. Many studies have assessed the benefits of appropriate footwear in the prevention of foot ulcers and their recurrence in people with diabetes [6–7], and inappropriate footwear has been implicated as one of the primary causes of foot ulcers. This issue must be addressed in Thailand because a history of foot ulcers can increase the mortality risk in individuals with diabetes [8]. Different types of footwear exist for various purposes, and it is essential to understand that footwear needs can vary across different cultures. In addition, suboptimal adherence with indoor footwear has been reported in many countries [9, 28] and may also vary according to geographic location [10]. Ultimately, specialized footwear is only useful if worn [11]. There are currently no data on what type of footwear is used by people with diabetes and their preferences in terms of indoor footwear. Such information is needed to guide future development of novel footwear designs that might benefit people with diabetes and increase adherence.
The primary objective of this study was to collect information on foot problems and current footwear use in patients with diabetic mellitus in Thailand. The secondary objective was to ascertain their preferences for indoor footwear design.
This descriptive study obtained data from 539 patients who were detected with type 2 diabetes at a moderate to high risk of developing foot ulcers according to the national practice guideline [4]. Participants were recruited at seven facilities (Siriraj Hospital, Vachiraphuket Hospital, Sawanpracharak Hospital, Maharat Nakhon Rachasima Hospital, Vejcharak Hospital, Phaholpolpayuhasena Hospital, and Abhaibhubejhr Hospital) in different regions of Thailand from May 2019–2020. The sample size was calculated based on the prevalence of diabetic foot ulcers in the Thailand Diabetes Registry Project [12], which was 5.9%. The inclusion criteria were age 18 years or older, type 2 diabetes with a moderate to high risk of developing foot ulcers, ability to walk without an assistive device, and understanding of the Thai language. Individuals with other types of diabetes were excluded. The study was approved by the Siriraj Institutional Review Board (COA no. Si 349/2019) and other institutions, including Niigata University of Health and Welfare (18163–190618), and was carried out in accordance with the principles described in the Declaration of Helsinki
Three certified pedorthists with more than 10 years' experience in foot problems, including the first author (SS) and one co-author (GS) developed a questionnaire and tested it with five patients from the Diabetic Foot Clinic at Siriraj Hospital. Minor revision was made based on patient feedback. The questionnaire included four sections that focused on patient characteristics, diabetic foot problems, current footwear use, and preferred indoor footwear designs included the cost of footwear (see Appendix A and B for questionnaires). The final version of the questionnaire was shared with the research assistants at each of the seven participating centers, who distributed it to potential participants and invited them to enroll in the study. Each study participant provided informed consent, completed the questionnaire, and returned it to the research assistant. All data were summarized as descriptive statistics and presented as the frequency. The relationship between patient characteristics and indoor footwear design preferences were analyzed using Spearman's rank correlation (rho). All statistical analyses were performed using SPSS Statistical Software v22 (IBM Corp., Armonk, NY).
In total, 539 patients with type 2 diabetes and a moderate to high risk of developing foot ulcers responded to the questionnaire. More than half of the respondents were female (n = 305, 56.6%) and the mean age was 62.58 ± 13.02 years (aged between 20 and 98 years old). Fifty-two percent of the respondents (n = 281) were retired, 41% (n = 225) were in employment, and the remainder was unemployed. Sixty-eight percent (n = 368) had no income or earned less than 10,000 baht (320 USD) per month. When asked about their diabetic status, 55.8% (n = 301) answered that they had had diabetes for more than 10 years and 78.1% (n = 421) had visited a foot clinic at least once for a foot evaluation in the past 6 months; however, as many as 21.0% (n = 113) had not visited their doctor at all (Table 1).
 |
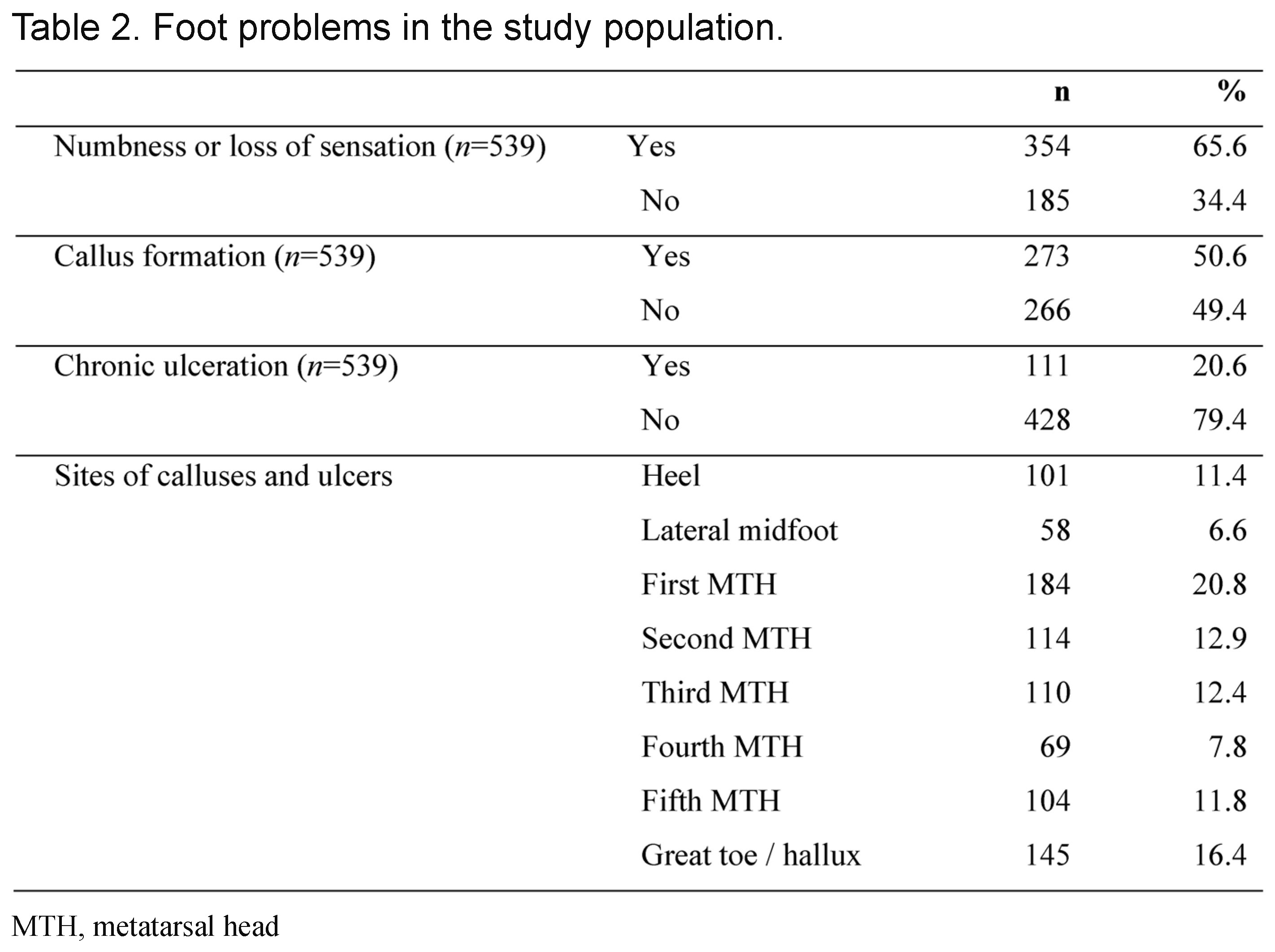
Data for foot problems are shown in Table 2. The majority of participants (n = 354, 65.6%) reported numbness or loss of sensation in the feet either sometimes or most of the time, while 34.4% (n = 185) had never experienced these problems. Further exploration of the data showed that 50.6% (n = 273) had calluses and nearly 21% (n = 111) had a chronic foot ulcer. The most commonly reported sites for foot calluses and ulcers were found under the head of the first metatarsal (n = 184, 20.8%), great toe or hallux (n = 145, 16.4%), and head of the second metatarsal (n = 114, 12.9%).
 |
Nearly half of the respondents (n = 252, 46.8%) reported walking barefoot inside the house, 38.5% (n = 207) reported wearing slippers or flip-flops, 5.4% (n = 29) reported wearing clog shoes, and the remaining 9.3% (n = 50) wore other types of footwear. All but four respondents reported wearing shoes when outdoors. The types of footwear most commonly worn outdoors were slippers or flip-flops (n = 230, 42.7%), closed shoes (n = 135, 25.2%) and clog shoes (n = 99, 18.4%) (Figure 1).

Indoor and outdoor footwear habits in patients with type 2 diabetes at moderate or high risk of developing foot ulcers.
With respect to indoor footwear design preferences, 78.8% of respondents (n = 424) preferred shoes that can be worn easily (i.e., slip-on type) followed by shoes that could be adjusted by fastening with Velcro straps (n = 102, 18.9%). Others preferred shoes with a different closing system (n = 13, 2.5%). More than half of respondents (n = 282, 53.7%) preferred footwear with breathability and 31.8% (n = 167) liked footwear that was made of a flexible material. Seventy-one percent (n = 382) preferred black shoes. The majority of respondents (n = 413, 76.7%) considered themselves likely to buy new indoor shoes if the shoes matched their needs and cost less than 1,000 baht (approximately 32 USD) (Table 3). However, weak correlation was found between the characteristics of respondents and footwear design preferences. (Table 4).
 |
 |
This study comprehensively investigated foot problems in people with type 2 diabetes in Thailand, the footwear currently used by this population, and patient preferences for indoor footwear design. Over half of the respondents had had a diagnosis of diabetes for more than 10 years. The majority of the respondents reported having visited a foot clinic for at-risk foot examination at least once in the previous 6 months. This is in line with international guidelines [3, 13,14] and the standard of care in Thailand [4], which recommend an annual foot screening and monitoring for possible foot ulceration. In particular, patients at moderate to high risk of foot ulcers should be examined every 1–6 months [13–15]. Early detection and management of risk factors are important in preventing and reducing the risk of foot ulcers [2, 16–18]. Importantly, a visit to a foot clinic is an opportunity for the healthcare provider to educate, train and ensure patients in regards to the self-care ability and knowledge of diabetic foot care.
The majority of respondents described numbness and/or loss of protective sensation in the feet. Respondents often reported calluses (50.6%) followed by ulcers (20.6%). Most calluses and ulcers were found on the plantar surface of the first metatarsal head (20.8%), hallux (16.4%) and second metatarsal head (12.9%). This is in line with previous reports of calluses and ulcers being found most often under the first metatarsal head, hallux, and second metatarsal head, which are sites of friction and compression pressure [19, 20]. In neuropathic patients with diabetes, foot deformity, shear stress [19] and ill-fitting shoes [21] may be risk factors of callus formation. Studies by Hui-sheng et al. [22] and Sauseng et al. [23] found that maximum peak pressure was higher at the hallux and metatarsal heads in people with diabetes. To prevent the callus formation and reduce the incidence of ulcers in people with diabetes and those at risk for foot problems, we suggest that annual foot screening, with a particular focus on the high-risk areas of the foot may be needed. In addition, most plantar pressure can be managed conservatively by wearing appropriate footwear to redistribute the mechanical pressure [19] and avoid the improper shoe fitting.
Most respondents in this study used footwear outdoors. The types of footwear most commonly worn outdoors were slippers or flip-flops, closed shoes (including sports shoes, sneakers, and custom-made shoes), and clog shoes. Our finding that 42.7% of respondents wore slippers or flip-flops, which are considered inappropriate for people with diabetes, is comparable with reports from India and Australia [24, 25]. It also points to a need for the health care team to provide effective education about footwear and emphasize the benefits of appropriate footwear in the prevention of foot ulcers and their recurrence in people with diabetes [6, 26–28]. The majority of the respondents in our study did not use footwear inside the house; those who did were most likely to wear slippers or clog shoes. In a similar study conducted in Singapore, Nather et al. found that 54% of patients did not wear shoes at home and that 38% wore slippers [29]. Slippers or flip-flops are expected to be the most acceptable footwear used indoors by Thais in view of the cultural practice of removing shoes [30] before entering important landmarks, religious structures, and homes as well as the ease with which they can be put on and taken off. Previous studies conducted in Australia and New Zealand have also mentioned that higher temperature and humidity could be important determinants of footwear habits [31, 32].
Our findings suggest that overcoming low adherence with indoor footwear among people with diabetes in Thailand will be a significant challenge. Increasing habitual footwear use indoors is critically important but difficult to implement in this population. At a minimum, good advice and effective communication with a health care team can encourage patients with diabetes who are at intermediate to high risk of foot ulceration to improve footwear habits and avoidance of barefoot walking [5]. At the same time, adherence could be increased by improving the footwear designed specifically for use indoors and further promotion of the importance of footwear in people with diabetes. Patients with diabetes need to wear footwear at least 60% of the time [33], and patient adherence is key in this regard.
With regard to footwear design, unattractive appearance, high cost, and limited availability in a range of colors and styles are common reasons given by patients for poor adherence in wearing prescription shoes [9, 34–36]. The main focus of this study was to investigate current footwear use and ascertain their preferences for indoor footwear. We found that these people prefer indoor shoes that are easy to slip on and off, which is in line with a previous report of problems with putting shoes on and taking them off in older people [37]. An earlier study found the most critical factors in decisions regarding indoor and outdoor shoes to be comfort and fit, particularly ease of fastening [38]. Approximately half of our respondents preferred footwear made of a breathable material, which is likely to be more comfortable indoors or outdoors [39]. Respondents who had a higher income were willing to pay more for indoor footwear as long as their belief in its benefits. However, the majority of respondents were only likely to buy new indoor shoes if the shoes matched their needs and cost less than 1,000 baht (approximately 32 USD).
Three-quarters of our study participants preferred shoes that were in black color, followed by brown and gray. This is in line with earlier study of color preference according to product category showed that the Japanese, Vietnamese, and Dutch preferred achromatic colors for clothing, and black in particular [40]. Previous research has demonstrated that color is an integral part of many design processes [41]. Therefore, appropriate use of color can impact greatly on the success of a design.
The limitations of this study include the method used to recruit participants and the reliance on self-reporting. Participants were recruited through convenience sampling located centrally at seven facilities across Thailand, so there may have been a degree of selection bias with regard to geographic area of residence and the day-to-day activities of the participants. Furthermore, all data were self-reported and no physical assessments were performed. We were unable to make objective assessments, which might have affected some of the study data, primarily those for sensation. Finally, some questionnaire items were not completed by the responders yet all data provided in the returned questionnaires were included in the analysis. This may explain why our study did not find a strong correlation between participant demographics and footwear design preferences.
A large proportion of patients with type 2 diabetes at moderate to high risk of developing foot ulcers are aware of routine foot examination. Our data show many people with diabetes walk barefoot most of the time at home, which could be the cause of developing foot complications. Therefore, many foot problems could be prevented by following appropriate treatment and maintaining good communication with a professional health care team. We suggest that further research should focus on the design and development of affordable and acceptable indoor footwear that accommodates patient preferences for an attractive appearance, comfort, and availability in a wide range of colors. Hopefully, this strategy will empower patients and result in increased collaboration and improved adherence. Patients who perceive their footwear as attractive are likely to be more adherent with wearing shoes.
This study was supported by a Siriraj research grant (no. RO16232025) from the Faculty of Medicine, Siriraj Hospital, Mahidol University, Thailand.
There are no conflicts of interest to declare.