2021 Volume 8 Issue 1 Pages 107-111
2021 Volume 8 Issue 1 Pages 107-111
Aneurysms of the large basilar artery (BA) occasionally cause cranial nerve palsy and motor disorder through mass effect. Since 1967, five cases of cerebral aneurysm leading to parkinsonism have been reported. Herein, we describe a rare case of progressive parkinsonism caused by the recurrence of a large aneurysm of the basilar tip after stent-assisted coil embolization. A 66-year-old man visited our hospital with an asymptomatic large aneurysm (maximum diameter, 21 mm) of the BA tip. Magnetic resonance imaging (MRI) revealed no perianeurysmal edema. Coil embolization with a Y-configuration stent with cross-placement was performed. Although thrombus formation occurred and the perforator infarction was complicated, complete occlusion was achieved. Three months later, the patient developed progressive and severe parkinsonism. MRI revealed mild enlargement of the aneurysm and perianeurysmal mesencephalic edema with minor neck recurrence. A trial administration of levodopa and additional stent-assisted coil embolization were performed. Levodopa dramatically improved parkinsonism; thus, the patient’s symptoms were controlled by a continuous levodopa regimen. In a large BA-tip aneurysm patient, moderate regrowth and minor neck recurrence occurred after initial treatment, and chronic compression of the midbrain caused secondary parkinsonism. In such cases, it is important to consider levodopa administration and therapeutic strategies to prevent recurrence or regrowth.
Aneurysms of the large basilar artery (BA) tip or the BA–superior cerebellar artery (BA–SCA) bifurcation occasionally cause cranial nerve palsy and motor disorder as a result of the mass effect.1,2) Lenga et al.1) and Haemmerli et al.2) analyzed 30 giant aneurysms in the posterior circulation and demonstrated that the volume of the aneurysm, rather than the degree of lateral projection or the amount of brainstem compression, was the most pertinent factor in the development of neurological disorders. Cranial nerve palsy was present in half of their cases, and a motor deficit was found in one-third; however, parkinsonism was not reported.1) Al-Jehani et al.3) reported a case of BA-tip aneurysm that caused hemi-parkinsonism, which improved after coil embolization of the aneurysm; they pointed out that only five cases of cerebral aneurysms causing parkinsonism, including theirs, have been reported since 1967. We describe a single rare case of a large aneurysm of the BA tip treated with stent-assisted coil embolization whose subsequent recurrence caused progressive parkinsonism.
A 66-year-old man visited our hospital with a large, asymptomatic aneurysm (maximum diameter, approximately 21 mm) at the BA tip. The patient had a history of chronic kidney disease and had been undergoing continuous hemodialysis for two decades. He had no other pertinent medical history. At the time of hospitalization, he was neurologically intact, without any parkinsonism. Computed tomographic angiography revealed a large aneurysm at the BA tip and that both posterior communicating arteries were hypoplastic. Magnetic resonance imaging (MRI) showed no perianeurysmal edema. The bilateral posterior cerebral arteries arose around a lower part of the aneurysm dome.
After providing written informed consent, the patient hoped to undergo endovascular treatment. Following discussion, coil embolization with cross-placement of a Y-configuration stent was deemed appropriate as an adjunctive technique because of the flow diversion effect. In accordance with our routine protocol, 100 mg of aspirin and 75 mg of clopidogrel were administered daily for 2 weeks before treatment.
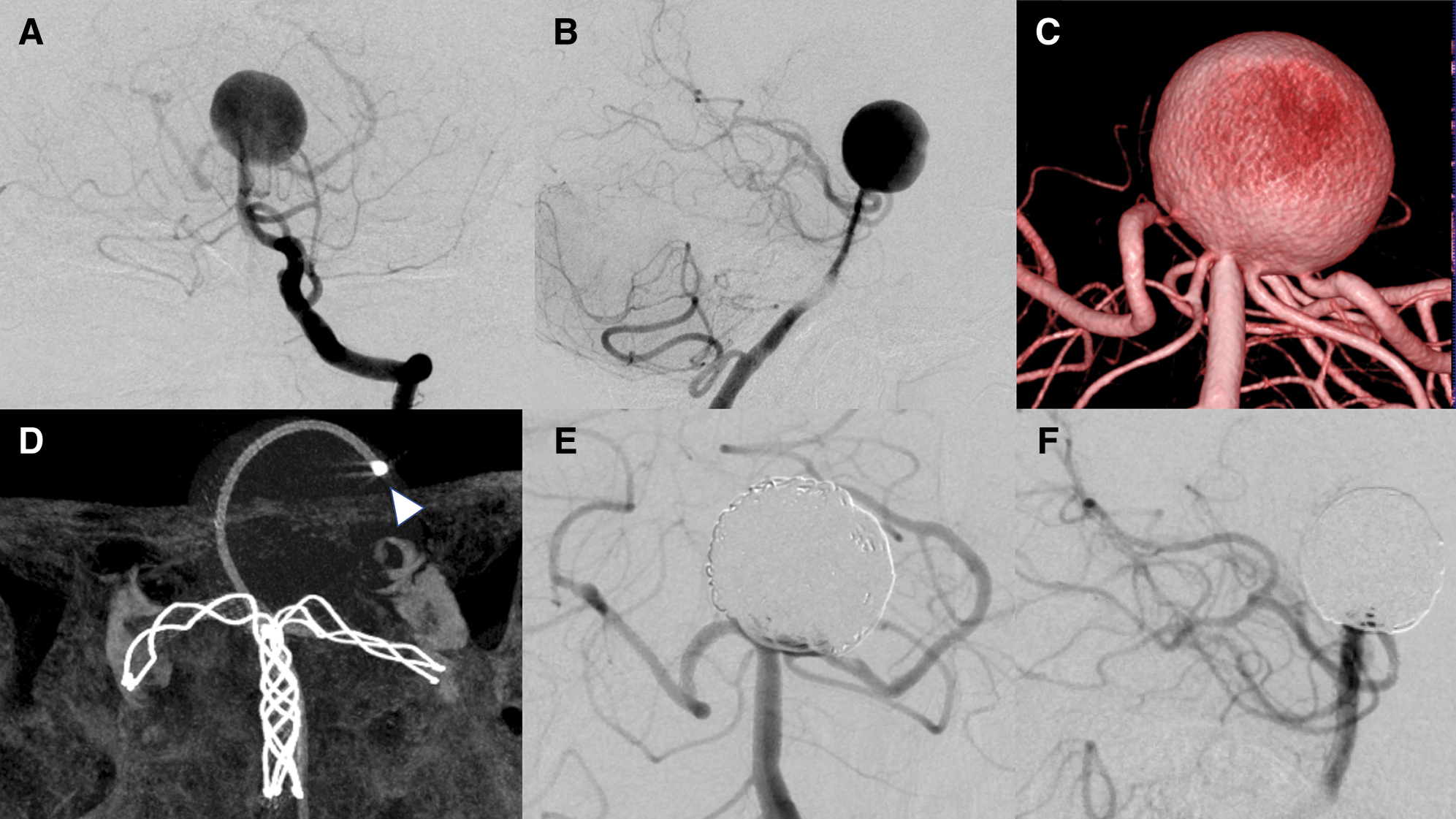
After the placement of guiding catheters in the bilateral vertebral arteries with systemic heparinization, digital subtraction angiography (DSA) and three-dimensional rotational angiography (3DRA) were performed (Figs. 1A–1C). Y-configuration stenting for cross-placement was established with dual LVIS stents (MicroVention Terumo, Aliso Viejo, CA, USA). After imaging with cone-beam computed tomography with diluted contrast dye (Fig. 1D), coil embolization was initiated through a jailed microcatheter. The procedure was completed with sufficient patency of each vessel branch and almost total occlusion of the aneurysm (Figs. 1E and 1F). The postoperative course was relatively uneventful, except for the occurrence of perforator vessel infarction (Figs. 2A and 2B). The patient experienced slight gait disturbance, which improved a few days later because the infarction area was limited.
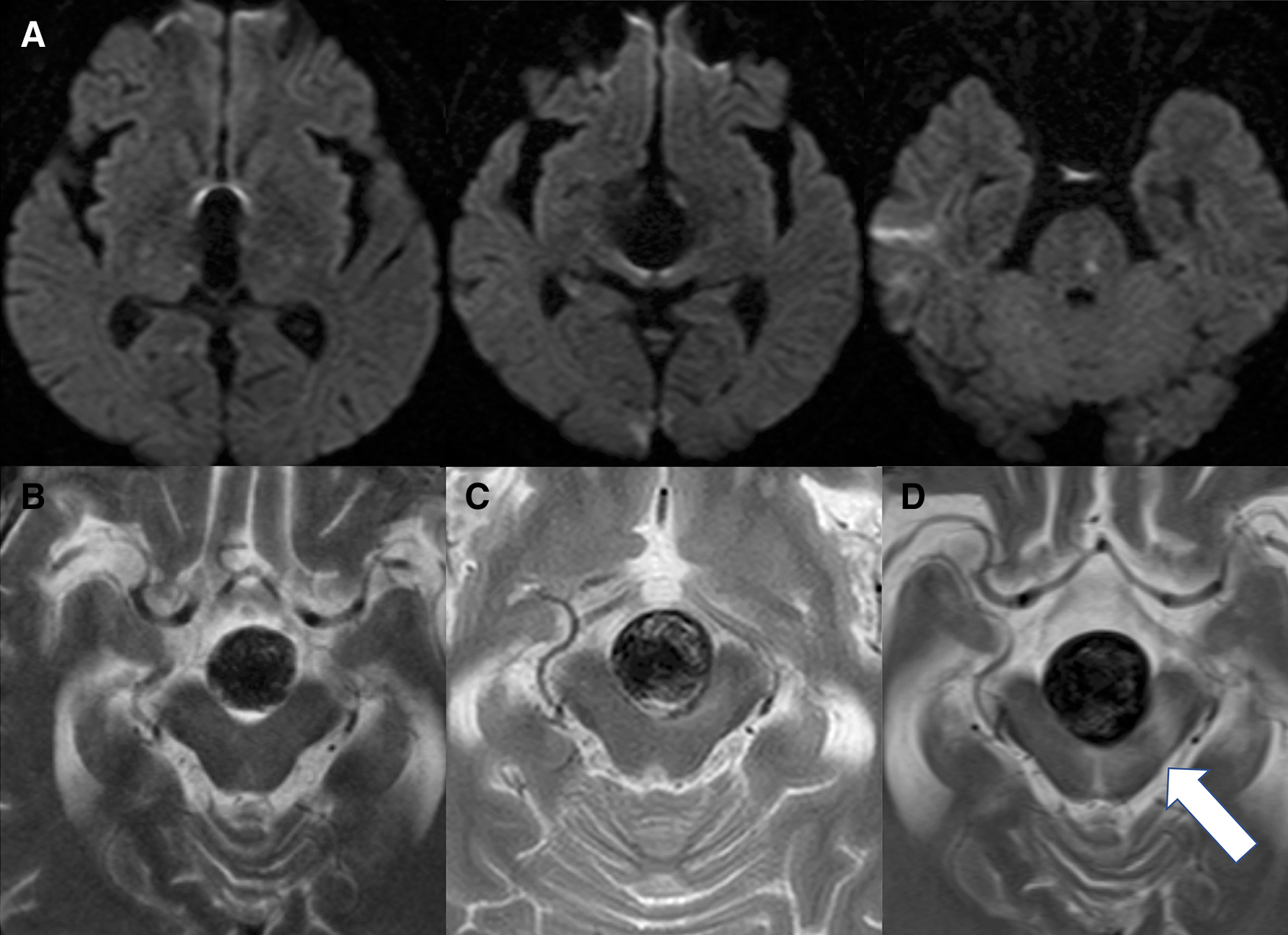
Two months after discharge, the patient showed transient diplopia and MRI showed mild perianeurysmal edema without aneurysm enlargement (Fig. 2C). Approximately 3 months after surgery, the patient began to develop progressive parkinsonism, starting with mask-like facies, rigidity and followed by short-stepped gait. Over the next month, progressive bradykinesia, consciousness disturbance and swallowing disorder developed, and the patient subsequently became bedridden. Modified Rankin scale score rapidly worsened, from 1 to 5. T2-weighted imaging revealed mild enlargement of the aneurysm (maximum diameter, 24 mm) and perianeurysmal mesencephalic edema resulting from compression of the aneurysm without hydrocephalus and any new hemorrhagic or ischemic lesion (Fig. 2D). However, the magnetic resonance angiographic source image did not reveal major recurrence. DSA revealed minor recanalization around the aneurysmal neck without body filling (Fig. 3A).
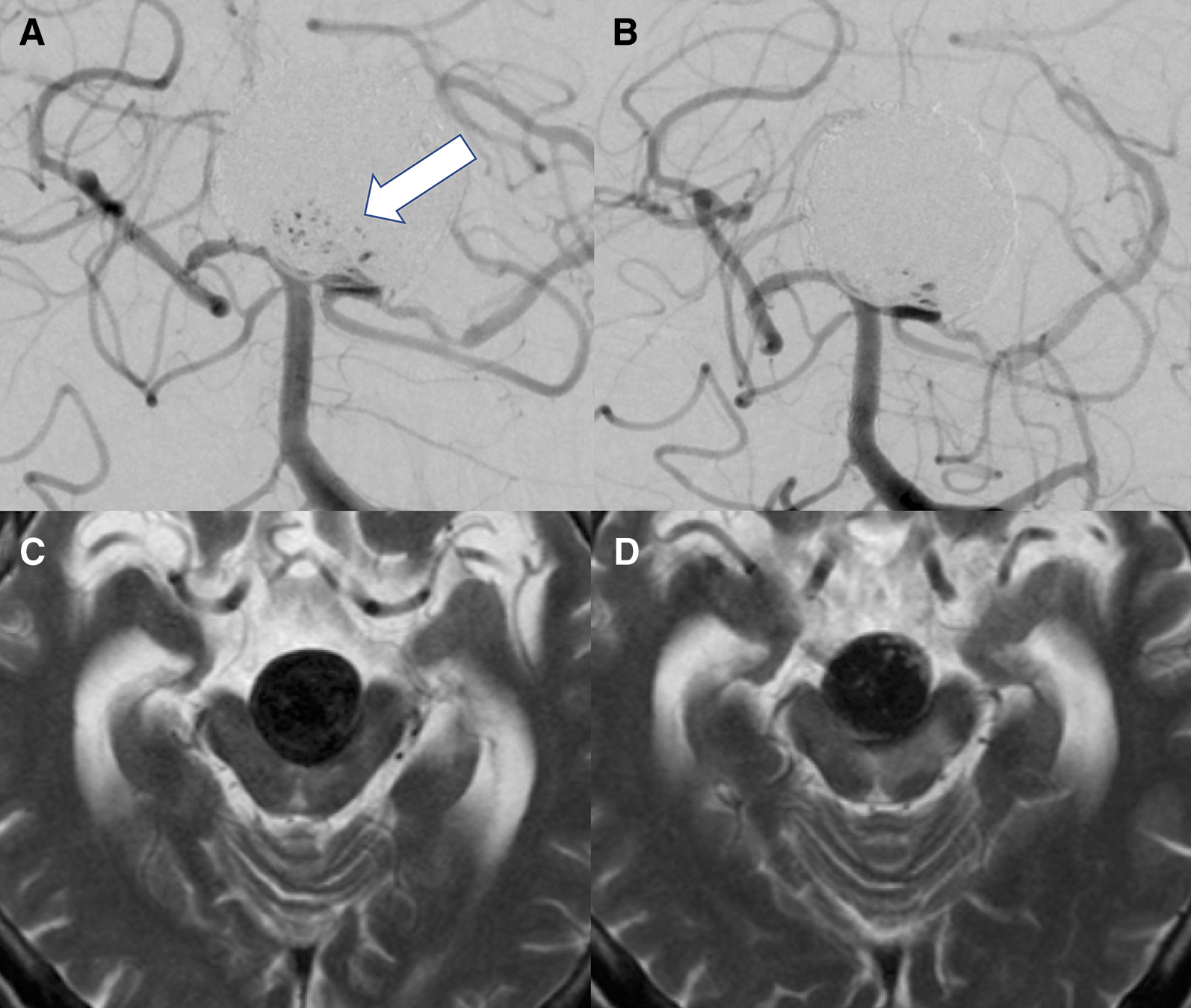
In view of the possibility of secondary parkinsonism resulting from chronic ischemia of the midbrain caused by the mass effect of the aneurysm, two treatments were planned: a trial administration of levodopa and the addition of a stent and coils to prevent further recurrence. First, oral levodopa 300 mg per day was started; a few days later, the patient’s consciousness and bradykinesia dramatically improved to the point where he was able to talk, swallow and move using a wheelchair. Second, additional embolization was performed. Following coil embolization to a maximum extent, another LVIS stent was deployed as an overlapping stent. The second embolization was completed without ischemic complications. After >6 months since the operation, the patient’s neurological status has not deteriorated, and outpatient follow-up has continued. Levodopa administration was also continued because MRI continued to demonstrate perianeurysmal edema without apparent worsening (Figs. 3C and 3D). At the worst status, the patient was close to being in a vegetative state, but presently he is showing neurological improvement in consciousness, parkinsonism, and daily activities while undergoing rehabilitation.
We made two important clinical discoveries in this case. Even a mild regrowth of a large basilar aneurysm might compress the midbrain with mass effect, which can lead to progressive parkinsonism. However, this development is rare, and this was the first case of parkinsonism to develop in our experience with large BA aneurysms. We also found that administration of levodopa was a suitable option for treating such secondary parkinsonism.
In this case, a slight regrowth of the aneurysm caused a mass effect in which the midbrain was compressed. As a result, signs of progressive parkinsonism appeared. The occurrence of consciousness disorder may have been due to ascending reticular activation system disorder. However, the rapidly evolving symptoms were considerably improved by the administration of levodopa alone, suggesting that bradykinesia from parkinsonism mimicked consciousness disorder. To our knowledge, previous reports of parkinsonism related to aneurysm of the BA tip are limited to one case.3) In consideration of the pathophysiologic features, this case was very suggestive because parkinsonism appeared not before but after treatment. A similar mechanism by which chronic compression of the midbrain causes parkinsonism had also been reported in cases of midbrain hemorrhage,4) hydrocephalus,5) bilateral subdural hematoma,6) vascular compression of the cerebral peduncle by the PCA,7) and intracranial tumor.8,9) The pathophysiologic features of parkinsonism in the hydrocephalic state involve dysfunction in the nigrostriatal pathway or the cortico-striato-pallido-thalamo-cortical circuit or both.4) Curran and Lang classified parkinsonism caused by hydrocephalus into three types5) and stated that the type that responds to levodopa is related to dysfunction of nigrostriatal dopaminergic system, which is caused by torsion, central herniation, or direct compression of the midbrain by the expanding third and fourth ventricles.5,6,9) Their statement was pathophysiologically supported by results of animal experiments in which induced hydrocephalus caused a decrease in dopamine levels in the striatum and midbrain.6,10) This pathological mechanism suggests that the postoperative aneurysm enlargement has exacerbated our patient’s condition in developing parkinsonism.
Second, similar to the present case, levodopa was effective in the treatment of secondary parkinsonism in the earlier case. Although the neurologist we consulted initially believed that medication was not effective, trial administration of levodopa was performed, and the neurological symptoms improved. The additional stent-assisted coil embolization mildly alleviated the compression to the midbrain; however, levodopa 300–400 mg/day was continued, although dose reduction was considered. The present case shows similarities to a condition called “Vascular parkinsonism (VP)”. VP is defined as a condition of atypical parkinsonism that presents the clinical features of parkinsonism that presumably caused by cerebrovascular disease in contrast to typical Parkinson’s disease (PD).11) It is classically described as symmetrical lower-body parkinsonism with gait unsteadiness and absence of tremors and is said to have a low response rate to levodopa with approximately only 30%.12) In a previous review,11) two forms of VP were suggested: one related to basal ganglia infarcts with acute onset, and another one associated with diffuse subcortical white matter ischemia with insidious progression. In the former, the symptom mimicked those of PD because of damage to the basal ganglia, which is the target of dopamine reaction. In another rare case report of dural arteriovenous fistula with deep venous reflux showed progressive parkinsonism.13) In this case, cerebral hypoperfusion of bilateral lenticular nuclei and frontal lobe white matter were detected in imaging studies and also treated with levodopa and endovascular embolization, reflecting both forms of VP. In the conclusion of the review, all patients with clinically suspected VP, particularly those with lesions in or close to the nigrostriatal and other dopaminergic pathways evidenced by MRI, regardless of the disease onset or dominant clinical features, should receive a trial with levodopa in 450 mg/day or more for at least 1 year, before concluding an absence of response.11) The overall odds ratio for a good response to levodopa in VP with ischemic or hemorrhagic lesions in the nigrostriatal pathway versus no lesion in the nigrostriatal pathway was approximately 15. Strictly speaking, the present case is not a classic VP since it is not a disorder of a nigrostriatal pathway due to ischemic or hemorrhagic change. However, as mentioned above, compression from hydrocephalus, tumors, and aneurysms can cause circulatory disturbance of immediate fiber tract, which leads potentially to semblable parkinsonism.
Large aneurysms at the basilar tip have high annual rates of rupture, and the recurrence rate after transcatheter arterial embolization is also high. In the present case, moderate regrowth and minor neck recurrence occurred after initial treatment, and chronic compression of the midbrain caused secondary parkinsonism. The trial administration of levodopa improved parkinsonian symptoms. In such cases, levodopa administration should be attempted, and the initial treatment should be aimed at preventing recurrence or regrowth as much as possible.
The authors would like to thank Asuka E. Kropp for insightful discussion content and emendation.
The authors declare that there is no conflict of interest.