Volume 63, Issue 2
Displaying 1-48 of 48 articles from this issue
- |<
- <
- 1
- >
- >|
-
2003 Volume 63 Issue 2 Pages 1-10
Published: 2003
Released on J-STAGE: March 29, 2014
Download PDF (11295K)
Technology and instrument
-
2003 Volume 63 Issue 2 Pages 26-28
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (786K) -
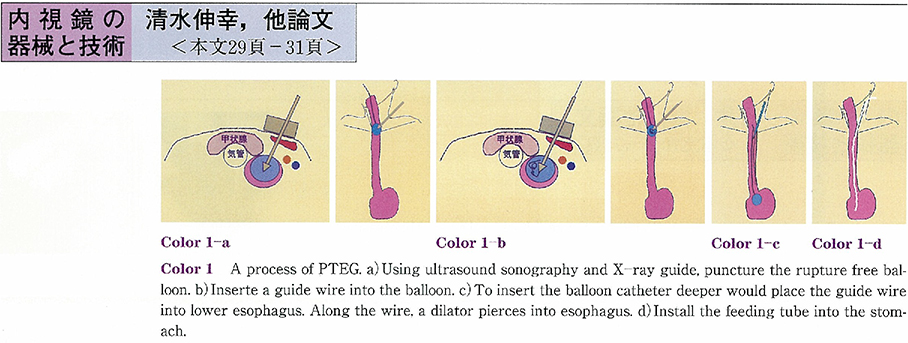
J-tube insertion and percutaneous trans-esophageal gastrotubing (PTEG) for long term enteral feeding2003 Volume 63 Issue 2 Pages 29-31
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (537K) -
2003 Volume 63 Issue 2 Pages 32-35
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (547K)
Clinical study
-
2003 Volume 63 Issue 2 Pages 36-40
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (748K) -
2003 Volume 63 Issue 2 Pages 41-45
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (606K) -
2003 Volume 63 Issue 2 Pages 46-50
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (553K) -
2003 Volume 63 Issue 2 Pages 51-55
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (678K) -
2003 Volume 63 Issue 2 Pages 56-59
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (1338K) -
2003 Volume 63 Issue 2 Pages 60-63
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (435K)
Case report
-
2003 Volume 63 Issue 2 Pages 64-67
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (1611K)
Technology and instrument
-
2003 Volume 63 Issue 2 Pages 68-69
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (176K) -
2003 Volume 63 Issue 2 Pages 70-71
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (672K)
Case report
-
2003 Volume 63 Issue 2 Pages 72-73
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (232K) -
2003 Volume 63 Issue 2 Pages 74-75
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (516K) -
2003 Volume 63 Issue 2 Pages 76-77
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (498K) -
2003 Volume 63 Issue 2 Pages 78-79
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (234K) -
2003 Volume 63 Issue 2 Pages 80-81
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (697K) -
2003 Volume 63 Issue 2 Pages 82-83
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (202K) -
2003 Volume 63 Issue 2 Pages 84-85
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (525K) -
2003 Volume 63 Issue 2 Pages 86-87
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (648K) -
2003 Volume 63 Issue 2 Pages 88-89
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (846K) -
2003 Volume 63 Issue 2 Pages 90-91
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (510K) -
2003 Volume 63 Issue 2 Pages 92-93
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (607K) -
2003 Volume 63 Issue 2 Pages 94-95
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (838K) -
2003 Volume 63 Issue 2 Pages 96-97
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (991K) -
2003 Volume 63 Issue 2 Pages 98-99
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (878K) -
2003 Volume 63 Issue 2 Pages 100-101
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (550K) -
2003 Volume 63 Issue 2 Pages 102-103
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (257K) -
2003 Volume 63 Issue 2 Pages 104-105
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (596K) -
2003 Volume 63 Issue 2 Pages 106-107
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (1072K) -
2003 Volume 63 Issue 2 Pages 108-109
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (669K) -
2003 Volume 63 Issue 2 Pages 110-111
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (957K) -
2003 Volume 63 Issue 2 Pages 112-113
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (1065K) -
2003 Volume 63 Issue 2 Pages 114-115
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (958K) -
2003 Volume 63 Issue 2 Pages 116-117
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (1083K) -
2003 Volume 63 Issue 2 Pages 118-119
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (737K) -
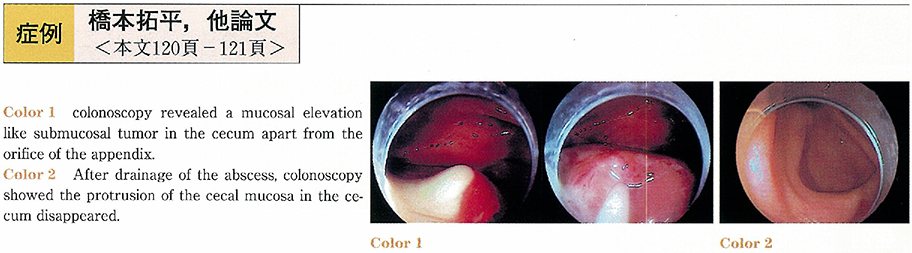
2003 Volume 63 Issue 2 Pages 120-121
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (601K) -
2003 Volume 63 Issue 2 Pages 122-123
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (352K) -
2003 Volume 63 Issue 2 Pages 124-125
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (960K) -
2003 Volume 63 Issue 2 Pages 126-127
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (187K) -
2003 Volume 63 Issue 2 Pages 128-129
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (437K) -
2003 Volume 63 Issue 2 Pages 130-131
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (676K) -
2003 Volume 63 Issue 2 Pages 132-133
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (621K) -
2003 Volume 63 Issue 2 Pages 134-135
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (916K) -
2003 Volume 63 Issue 2 Pages 136-137
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (714K) -
2003 Volume 63 Issue 2 Pages 138-139
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (553K) -
2003 Volume 63 Issue 2 Pages 140-141
Published: November 25, 2003
Released on J-STAGE: March 29, 2014
Download PDF (1073K)
- |<
- <
- 1
- >
- >|