Volume 85, Issue 1
Displaying 1-50 of 50 articles from this issue
- |<
- <
- 1
- >
- >|
-
2014 Volume 85 Issue 1 Pages 1-12
Published: 2014
Released on J-STAGE: December 17, 2014
Download PDF (11974K)
Technology and instrument
-
2014 Volume 85 Issue 1 Pages 36-39
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (776K) -
2014 Volume 85 Issue 1 Pages 40-42
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (364K)
Clinical study
-
2014 Volume 85 Issue 1 Pages 43-46
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (254K) -
2014 Volume 85 Issue 1 Pages 47-50
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (283K) -
2014 Volume 85 Issue 1 Pages 51-54
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (261K)
Technology and instrument
-
2014 Volume 85 Issue 1 Pages 56-57
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (1125K) -
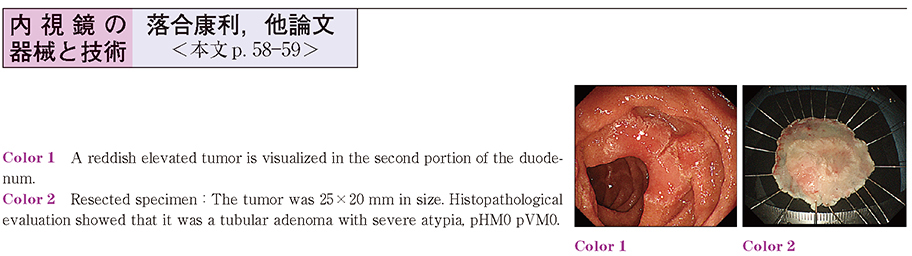
2014 Volume 85 Issue 1 Pages 58-59
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (870K) -
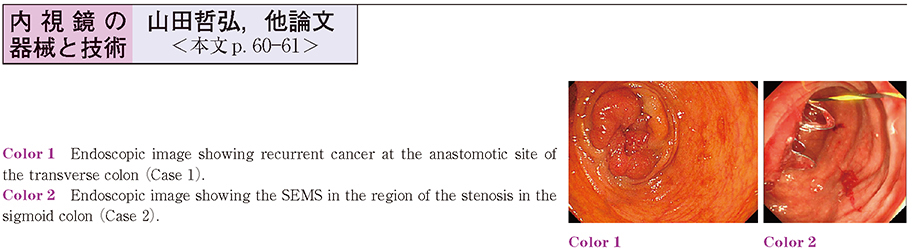
2014 Volume 85 Issue 1 Pages 60-61
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (919K)
Clinical study
-
2014 Volume 85 Issue 1 Pages 62-63
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (559K)
Case report
-
2014 Volume 85 Issue 1 Pages 64-65
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (487K) -
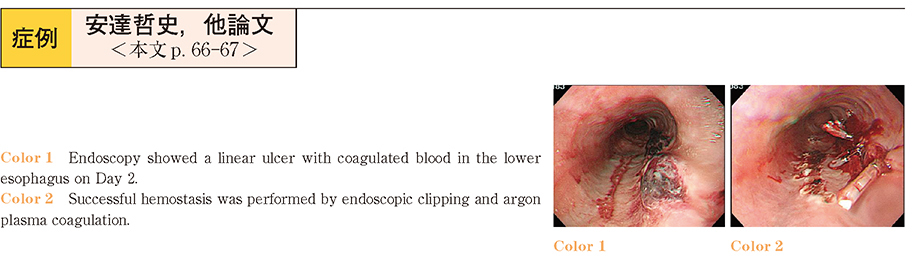
2014 Volume 85 Issue 1 Pages 66-67
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (273K) -
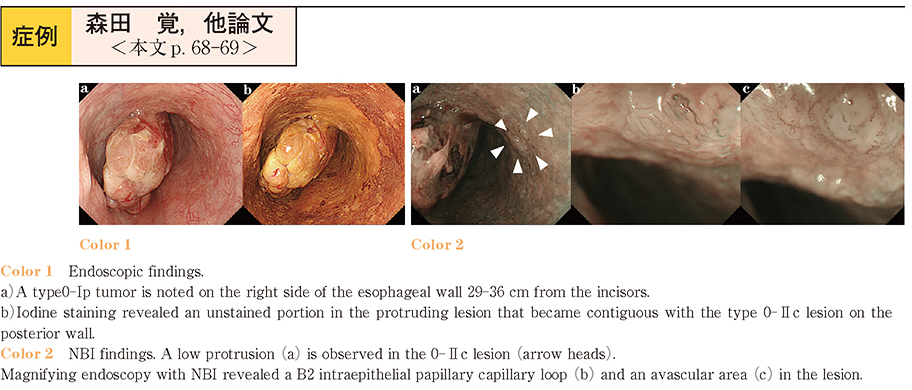
2014 Volume 85 Issue 1 Pages 68-69
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (948K) -
2014 Volume 85 Issue 1 Pages 70-71
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (633K) -
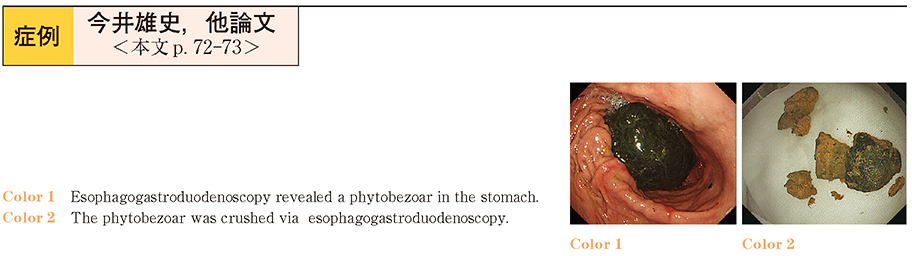
2014 Volume 85 Issue 1 Pages 72-73
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (789K) -
2014 Volume 85 Issue 1 Pages 74-75
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (273K) -
2014 Volume 85 Issue 1 Pages 76-77
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (223K) -
2014 Volume 85 Issue 1 Pages 78-79
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (894K) -
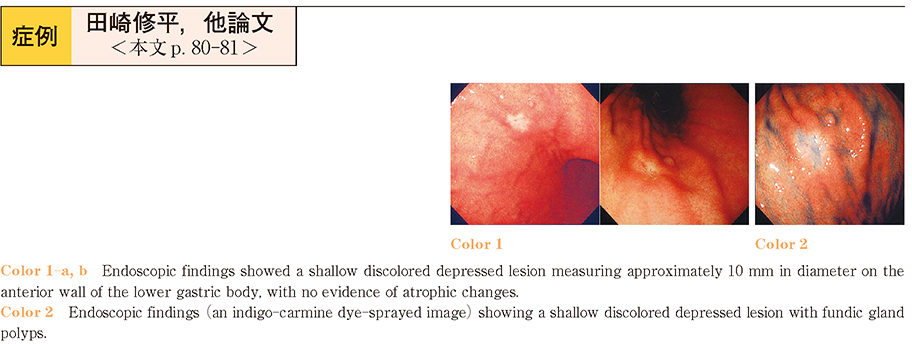
2014 Volume 85 Issue 1 Pages 80-81
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (623K) -
2014 Volume 85 Issue 1 Pages 82-83
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (252K) -
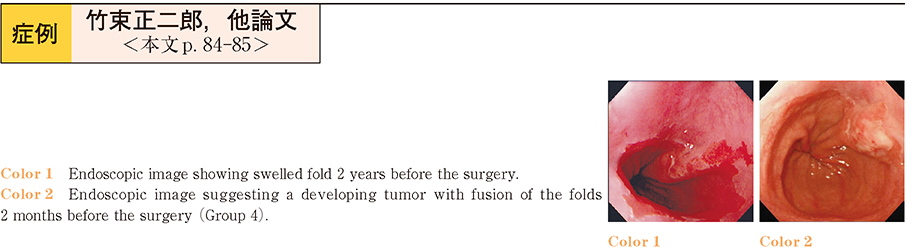
2014 Volume 85 Issue 1 Pages 84-85
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (532K) -
2014 Volume 85 Issue 1 Pages 86-87
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (747K) -
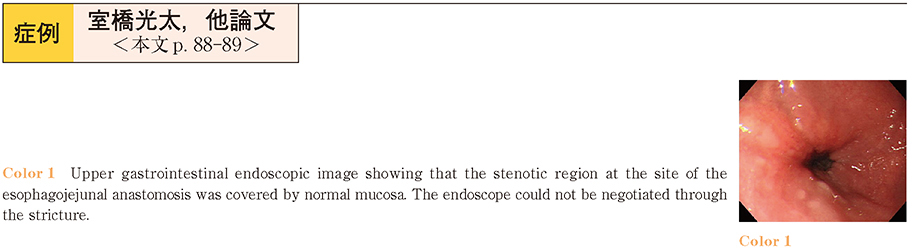
2014 Volume 85 Issue 1 Pages 88-89
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (407K) -
2014 Volume 85 Issue 1 Pages 90-91
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (265K) -
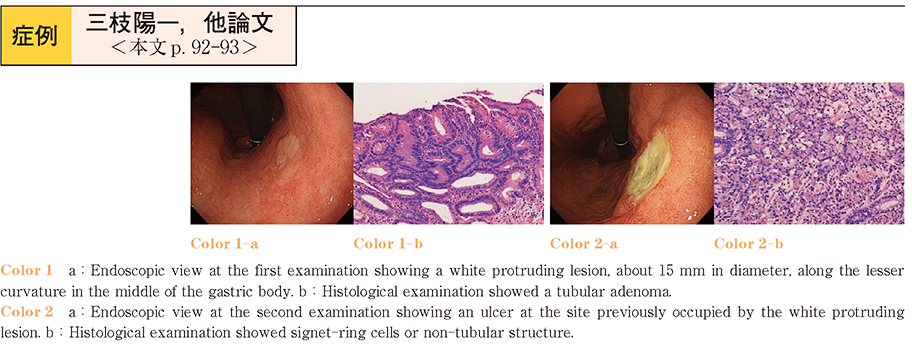
2014 Volume 85 Issue 1 Pages 92-93
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (436K) -
2014 Volume 85 Issue 1 Pages 94-95
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (413K) -
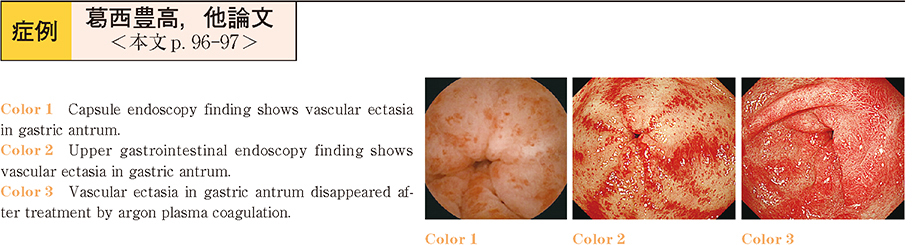
2014 Volume 85 Issue 1 Pages 96-97
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (210K) -
2014 Volume 85 Issue 1 Pages 98-99
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (217K) -
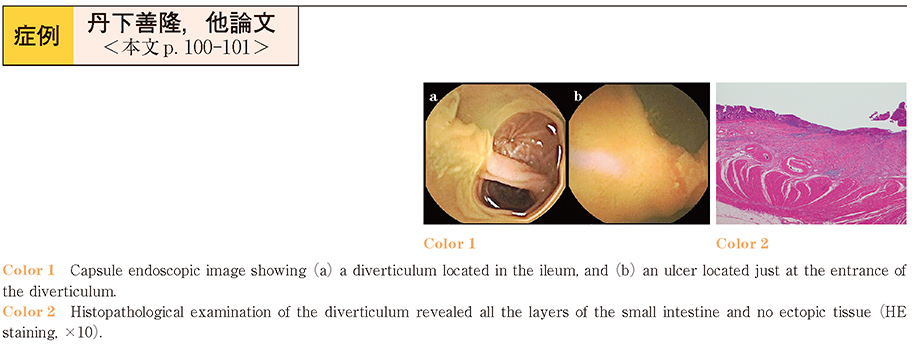
2014 Volume 85 Issue 1 Pages 100-101
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (332K) -
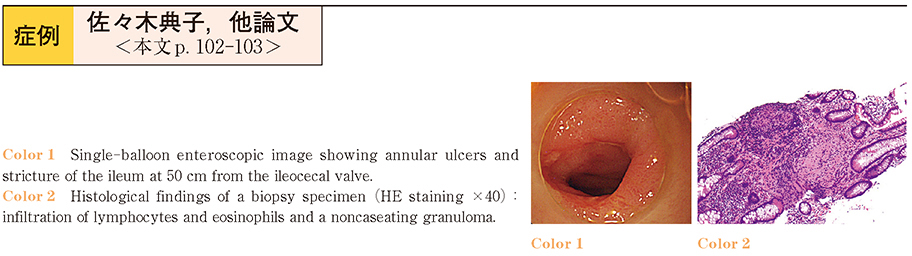
2014 Volume 85 Issue 1 Pages 102-103
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (463K) -
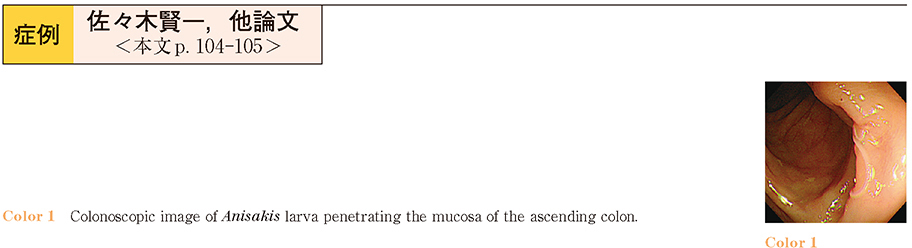
2014 Volume 85 Issue 1 Pages 104-105
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (338K) -
2014 Volume 85 Issue 1 Pages 106-107
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (358K) -
2014 Volume 85 Issue 1 Pages 108-109
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (657K) -
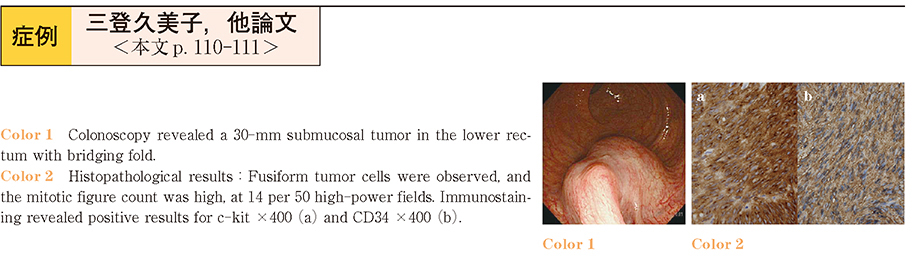
2014 Volume 85 Issue 1 Pages 110-111
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (408K) -
2014 Volume 85 Issue 1 Pages 112-113
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (564K) -
2014 Volume 85 Issue 1 Pages 114-115
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (493K) -
2014 Volume 85 Issue 1 Pages 116-117
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (708K) -
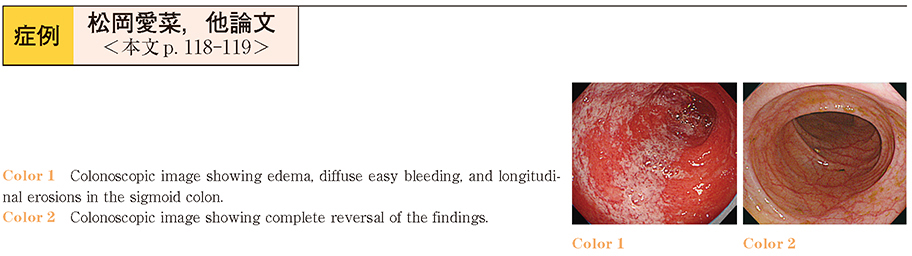
2014 Volume 85 Issue 1 Pages 118-119
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (284K) -
2014 Volume 85 Issue 1 Pages 120-121
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (552K) -
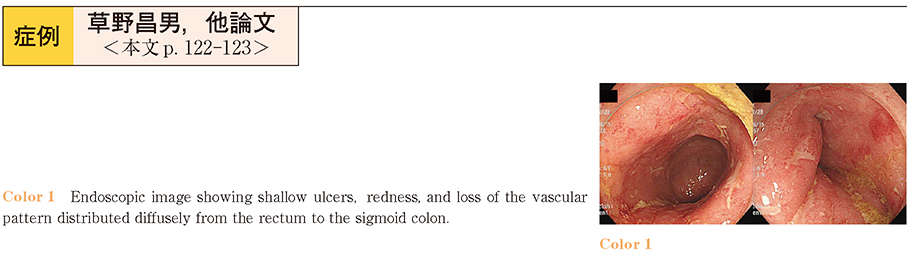
2014 Volume 85 Issue 1 Pages 122-123
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (506K) -
2014 Volume 85 Issue 1 Pages 124-125
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (773K) -
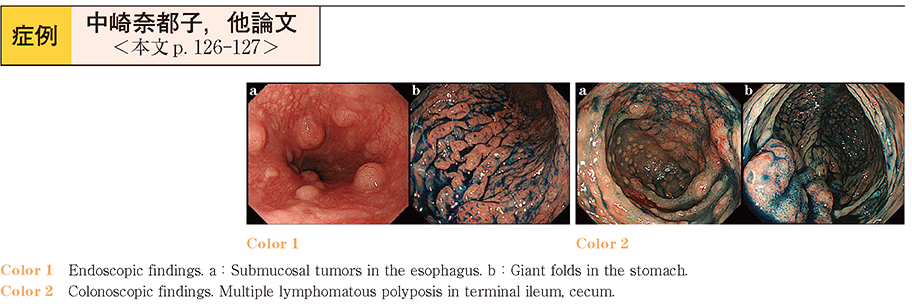
2014 Volume 85 Issue 1 Pages 126-127
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (781K) -
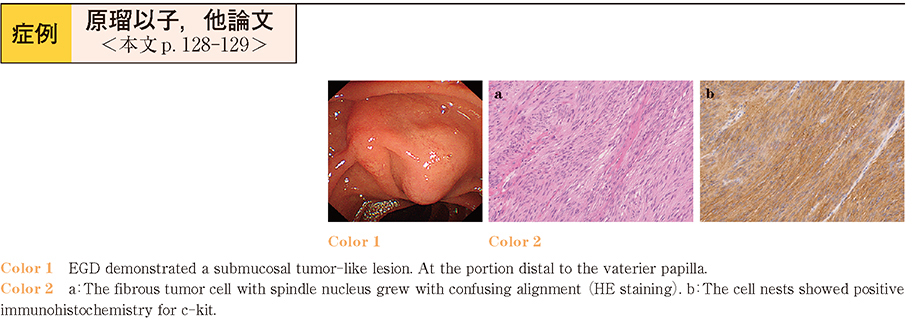
2014 Volume 85 Issue 1 Pages 128-129
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (486K) -
2014 Volume 85 Issue 1 Pages 130-131
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (584K) -
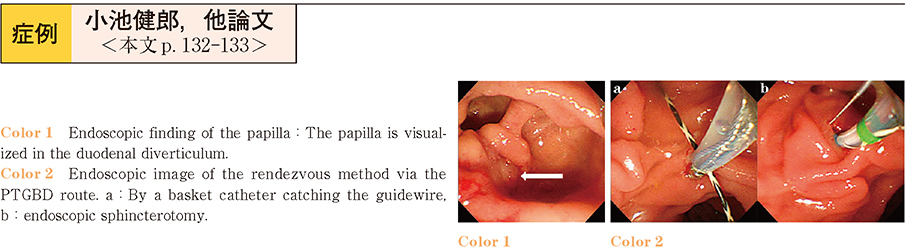
2014 Volume 85 Issue 1 Pages 132-133
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (408K) -
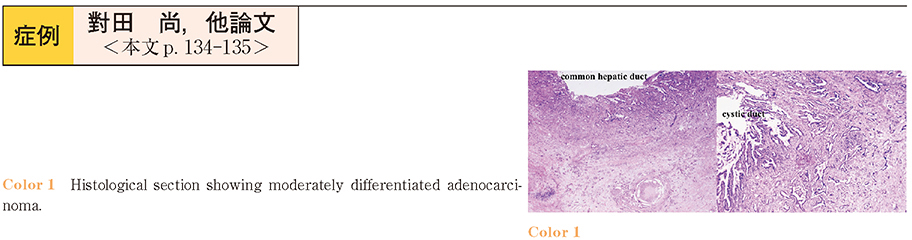
2014 Volume 85 Issue 1 Pages 134-135
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (793K) -
A case of bile duct cancer associated with pancreatobiliary maljunction without bile duct dilatation2014 Volume 85 Issue 1 Pages 136-137
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (540K) -
2014 Volume 85 Issue 1 Pages 138-139
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (429K) -
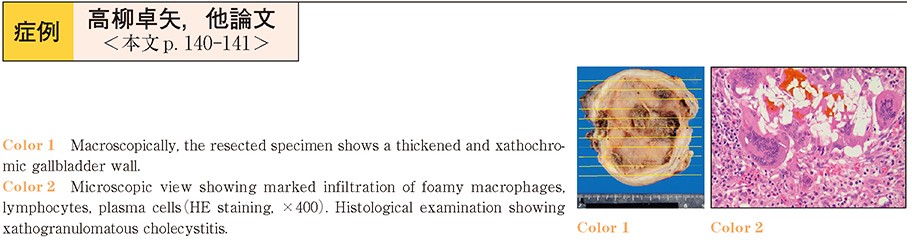
2014 Volume 85 Issue 1 Pages 140-141
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (420K) -
2014 Volume 85 Issue 1 Pages 142-143
Published: December 06, 2014
Released on J-STAGE: December 17, 2014
Download PDF (467K)
- |<
- <
- 1
- >
- >|