2020 Volume 6 Issue 1 Pages 74-80
2020 Volume 6 Issue 1 Pages 74-80
Takayasu arteritis (TAK) is classified as large-vessel vasculitis caused by inflammation. It is often difficult to identify on clinical examination, and 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) plays an indispensable role in diagnosing TAK by detecting the location and grade of the inflammatory lesions. The clinical utility of 18F-FDG PET has been established by clinical evidence, and 18F-FDG PET was added to the Japanese national health insurance listing in April 2018. In TAK, 18F-FDG uptake shows typical findings and is easily distinguished, except from physiological uptake. Particularly, the clinical significance of 18F-FDG PET is that can present not only with stenosis but also without stenosis in the arteries, which means that therapeutic intervention is possible before irreversible stenosis develops in the arteries. Additionally, 18F-FDG PET has superior diagnostic accuracy because it allows quantitative analysis using the maximum standardized uptake value. The analysis is used for the assessment of disease activity of TAK and can be utilized for therapeutic intervention in case of repeating remission during the follow-up term.
Takayasu arteritis (TAK), classified as a large-vessel vasculitis, is an inflammatory disease of unknown etiology (1). It causes stenotic or dilated lesions, predominantly in the aorta and its main branches. However, the initial diagnosis is often difficult using medical examination alone because it manifests as various symptoms without specific markers. Therefore, 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) is useful and unique for diagnosing TAK as it can detect the location of the inflammatory lesions. The clinical utility of 18F-FDG PET has been established by clinical evidence. 18F-FDG PET was added to the Japanese national health insurance listing in April 2018 and has since been available for determining the lesion site and disease activity in patients with TAK.
This disease is common in young female in Asia and the Middle East than in Europe and North America (2). Particularly, peak age of onset is the latter half of teens and early twenties in female patients (3). In Japan, more than 5000 cases are registered and the number of patients increases by 200 to 400 every 3 years, however the rate of increase has been suppressed in recent years (3).
In TAK, the lesions are located mainly in the thoracic aorta, abdominal aorta, and their primary branches (the common carotid, subclavian, brachiocephalic, and renal arteries). They can also be located in the coronary and pulmonary arteries. In Japanese people, the three branches in the neck are common locations (4).
Histopathologically, the walls of these blood vessels, particularly from the media to the adventitia, show inflammatory cellular infiltration, necrosis of the vascular smooth muscle cells, destruction of the elastic fibers, and fibrosis. These lead to reactive changes that cause fibrous thickening of the intima, resulting in luminal narrowing of the blood vessels. Whereas, destruction of elastic fibers may lead to loss of blood vessel elasticity and separation between the media and adventitia, causing the development of dilated lesions such as aortic aneurysms (5).
Generally, TAK can trigger various symptoms in organs throughout the body. Clinically, its symptoms are roughly classified into systemic symptoms due to immune response (e.g., pyrexia and general malaise) and ischemic symptoms due to site of vascular stenosis. TAK used to be termed a “pulseless disease.” Pulselessness in the brachial and radial arteries and a large difference in blood pressure between the right and left arms are the most common findings of this disease, which can be explained by the narrowing of the arteries.
Blood tests for the disease reveal inflammatory findings, such as elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), but there are no markers specific to the disease (6). In some cases, TAK could be diagnosed as fever of unknown origin, and a definitive diagnosis is challenging. Therefore, imaging is essential to understand the clinical presentation of the disease.
In TAK, inflammatory cells, such as white blood cells, aggregate at the sites of inflammation. Since 18F-FDG is a glucose analog, it accumulates through the glucose transporter (GLUT).
Various types of white blood cells travel to the lesion via an immune response to antigens that are yet to be identified in this disease. In particular, T cells and natural killer cells exert a cytotoxic action, and macrophages and neutrophils stimulated by cytokines migrate, causing inflammation to spread from the media to adventitia of the blood vessels (5). GLUT1 and GLUT3 are expressed in the white blood cells (7), and the respiratory burst activated in the course of inflammation consumes abundant glucose, causing injected 18F-FDG to be taken up into the inflammatory cells via GLUT (8). Therefore, 18F-FDG accumulates in proportion to the degree of inflammation. The standardized uptake value (SUV) tends to be high in neoplastic diseases but not so much in inflammatory diseases, such as TAK. This is attributable to differences in pathological activity between tumor cells and inflammatory cells in autoimmune diseases.
The first clinical study on TAK using 18F-FDG PET was reported by Webb et al. in 2004; it included 18 patients with TAK, and 18F-FDG PET showed a sensitivity of 92% and specificity of 100% (9). Subsequently, reports have suggested the usefulness of 18F-FDG PET (10). Kobayashi and Numano reported the first cut-off maximum SUV (SUVmax) in their study involving 14 patients with TAK, showing a sensitivity and specificity of 90.9% and 88.8%, respectively, for a cut-off of 1.3 (11).
Together with computed tomography (CT) and magnetic resonance imaging (MRI), 18F-FDG PET is a useful imaging modality for the diagnosis of TAK and is supported by solid evidence (9–11). 18F-FDG PET was added to the Japanese national health insurance listing in April 2018 and has since been available for determining the lesion site or disease activity in patients who have been diagnosed with large-vessel vasculitis. However, patients undergoing 18F-FDG PET/CT are exposed to approximately 5 mSV of radiation; therefore, sufficient caution should be exercised when testing women in the second or third decade of life, who are commonly affected by this disease.
1. AortaIn TAK, although PET can be used for diagnosis, PET/CT simplifies the identification of the lesion site. The reason is that PET helps obtain information in the longitudinal direction of the body, but its imaging ability in the horizontal plane of the body is less than desirable. In vasculitis, inflammation is often present in multiple blood vessels, and anatomically identifying the inflammation sites is important. CT provides additional information on the cross-section of the body, allowing for more a reliable and easier diagnostic method.
Because of the relatively large diameter of the ascending aorta, aortic arch, pulmonary artery, descending aorta, and abdominal aorta, the “ring sign” around the affected vessel wall is a typical finding of TAK and is highly reproducible (Figure 1).
However, in arteriosclerotic plaques, such as vascular wall calcification, increased 18F-FDG uptake may be observed if macrophages have been activated (12). Therefore, in the elderly patients with arteriosclerosis, caution is required in the diagnosis of vasculitis to avoid a false-positive result.

Comparison of whole-body PET with PET/CT.
The patient was a 23-year-old woman with TAK.
Circumference: Whole-body PET images rotated by 45°. 18F-FDG uptake is in the aortic arch.
Middle: 18F-FDG PET/CT imaging. 18F-FDG uptake in the shape of a ring is seen around the ascending aorta. PET/CT fusion imaging simplifies the anatomical identification of the lesion site.
The primary branches of the aorta, such as the common carotid, subclavian, brachiocephalic, and vertebral arteries, have a relatively small diameter. Due to the low spatial resolution of PET, ring sign-like findings on aortic PET/CT are not likely to manifest. Distinguishing between the vascular walls and lumens is difficult, and as 18F-FDG uptake appears to be present in the blood vessels, differentiation from physiological uptake is necessary. An increased uptake caused by TAK is typically focal or diffuse in the blood vessel. This feature is more evident on whole-body images, enabling the identification of 18F-FDG uptake resulting from this disease even in the primary branches (Figure 2).

18F-FDG PET of the primary branch arteries.
The patient was a 23-year-old woman with active-phase TAK.
Above: Whole-body PET.
Bottom: From left to right, PET/CT shows the brachiocephalic, left carotid, and left subclavian arteries with strong 18F-FDG uptake.
The findings of the primary branches are clinically important. Compared to MR angiography, 18F-FDG uptake can be seen in the blood vessels without stenosis, indicating inflammation (Figure 3). Such findings allow for therapeutic intervention before stenosis progression, which is clinically significant.

Comparison of 18F-FDG PET/CT with MRA.
The patient was a 20-year-old woman with TAK who underwent imaging for an untreated condition.
A: Magnetic resonance angiography.
B: Whole-body 18F-FDG PET.
C: 18F-FDG PET /CT imaging.
From left to right, the red arrow shows the left and right carotid arteries, the aortic arch, and the proximal and distal parts of the left subclavian artery.
In cases of a primary branch stenosis progressing irreversibly in patients with significant ischemic symptoms, bypass graft surgery with an artificial blood vessel is a treatment option. However, special attention should be paid to graft-related findings on 18F-FDG PET. While 18F-FDG PET is useful for the diagnosis of vascular graft infections (13), 18F-FDG uptake is observed even in the absence of infections (Figure 4). Artificial substances used in grafting are recognized as foreign objects, inducing immune responses. This presumably leads to the aggregation of macrophages and other cells, resulting in 18F-FDG accumulation (14). Therefore, to diagnose TAK, 18F-FDG PET assessment of a blood vessel graft should be performed comprehensively in consideration of the patient's clinical course, blood test results, and other relevant information.
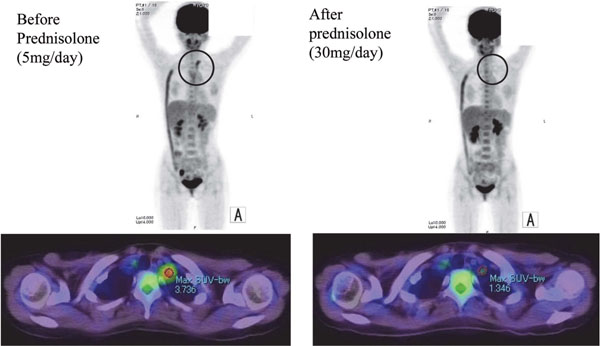
18F-FDG PET can assess the therapeutic effect of corticosteroids in cases of relapse.
A 23-year-old woman with TAK was on corticosteroids 5 mg/day. ESR was 18 mm/h, but she had left arm pain with slight CRP elevation up to 1.1 mg/dL. 18F-FDG PET/CT showed uptake in the left subclavian artery, and SUVmax was elevated (left). After increasing the prednisolone dose to 30 mg/day, the uptake disappeared, and SUVmax decreased (right). Strong 18F-FDG uptake on her right side was due to an artificial graft, from the right axial artery to the right external iliac artery.
SUVmax is semi-quantitative marker presenting the degree of FDG uptake. SUVmax can be measured by placing the regions of interest at the sites of 18F-FDG uptake in the vascular wall using the workstation software. However, since SUVmax measured using this method varies across facilities, they should be interpreted with caution.
Generally, SUVmax is significantly higher in patients with acute-phase TAK than in those with non-acute phase TAK (remission achieved) (11, 15). For that reason, quantitative evaluation can be additionally used for diagnosis (15). At our facility, vascular SUVmax ranged from 2.1 to 5.3 in 45 patients with acute-phase TAK. However, the quantification should be performed carefully in order to avoid a false-positive 18F-FDG uptake.
Assessment of disease activity by 18F-FDG PET during treatment of TAKThe lack of disease-specific hematological markers inconvenience the diagnosis of TAK. Matrix metalloproteinase 3 is widely used as a marker for this disease, but it tends to increase after administration of steroids and may therefore not be used as a reference in some cases (3, 16). Therefore, to evaluate the disease state, hematological markers, such as CRP and ESR, are the only choice. Particularly, CRP and ESR are markedly elevated in the first onset of TAK.
However, CRP and ESR have some limitations. In patients experiencing a relapse during maintenance therapy with steroids or immunosuppressants, evaluating the disease state by CRP/ESR is often difficult. For example, even in a temporary remission state, some patients may show a mild elevation of CRP to approximately 0.5–1.0 mg/dL. Furthermore, since cases of relapse is under administration of steroid therapy, a marked elevation of CRP/ESR is suppressed. Therefore, it may be difficult to determine whether a slight elevation of these levels is due to a relapse or is within the range of variation. In addition, ESR is easily affected by other factors, such as anemia, and there are only a few disease activity indices, other than CRP, for TAK. Therefore, 18F-FDG uptake can be an indicator suggesting the presence of inflammation and may be used as an index to determine the therapeutic effect.
Patients with first-onset TAK are started on high-dose steroids (prednisolone, 20–30 mg/day) as the initial treatment, followed by gradual dose reduction, and the treatment is continued at a maintenance dose (5–10 mg/day). The disadvantage is a potential relapse at the time of dose reduction. Therefore, steroid tapering is done while evaluating a potential relapse using CRP. Once patients are on the maintenance dose, the success of the initial therapy can be confirmed by checking for the disappearance of the 18F-FDG uptake, which is indicative of the presence of localized inflammation, in addition to CRP levels suggesting the presence of systemic inflammation (Figure 4). During maintenance dose, the evidence of optimal interval of FDG-PET for observation has not been established yet. We recommend FDG-PET when it is difficult to assess recurrence phenomenon such as showing slight elevation of CRP with clinical symptoms, provided that the benefit of FDG-PET is superior than the risk of radiation, particularly in case of the young female patients.
To verify whether 18F-FDG uptake could be used as a quantitative marker, our group collected data on SUVmax and its target-to-background ratio (TBR) relevant to this disease, and we performed a statistical analysis. We defined the acute phase in accordance with the NIH guidelines (17) and found that SUVmax and CRP were elevated in acute-phase cases. However, although the SUVmax values were also high in cases of relapse, the CRP levels were not so high. (Figures 5A and B). In addition, the receiver operating characteristic curve analysis revealed that a cut-off SUVmax of 2.1 strongly correlated with the disease state and that the diagnostic accuracy of quantitative values was actually high (Figure 5C) (15). These results suggest that SUVmax and TBR reflect the disease state in patients with a suspected relapse during maintenance therapy and is therefore considered useful for therapeutic assessment.

Comparisons of CRP and SUVmax among patients who were untreated, relapsing on treatment, and stable on treatment for TAK
All of the 39 patients with TAK were enrolled in this study. At first, the case were classified to active and inactive cases according to NIH score of TAK. Moreover, the active cases were divided into untreated and relapsing on treatment groups, and the inactive cases were defined as ‘stable on treatment’. SUVmax in the two active groups were significantly higher than that in the stable on treatment group. CRP was statistically different among untreated, relapsing, and stable cases. SUVmax did not differ between untreated and relapsing cases.
C: Comparisons of ROC curves between SUVmax, TBR, CRP, and ESR
To detect active cases, AUCs in SUVmax (95.4%) and TBR (91.4%) were statistically superior to those in CRP (84.7%) and ESR (72.7%) (p<0.05).
However, the use of 18F-FDG PET for determining the therapeutic effect is yet to be insured under the Japanese health insurance system.
Evidence has been accumulated to support the use of 18F-FDG PET in TAK, and its usefulness had gradually been validated. In April 2018, the use of 18F-FDG PET in patients with TAK was added to the Japanese national health insurance listing, and the modality is expected to be used more frequently in the future. While the use of 18F-FDG PET has many benefits from a diagnostic standpoint, radiation exposure should be taken into consideration as the disease commonly affects young women. To that end, further studies are desired to explore the appropriate use of 18F-FDG PET as a therapeutic intervention before progression of vascular stenosis through an early diagnosis and rapid assessment of disease activity.
None.
None.
None.