2023 Volume 23 Issue 2 Pages 24-27
2023 Volume 23 Issue 2 Pages 24-27
This report describes the case of a 52-year-old woman with oral lichen planus due to a dental metal allergy, who was treated successfully by removing metal restorations and replacing them with a zirconia centered non-metal based fixed partial denture (FPD). Following basic periodontal treatment, all intraoral metal restorations were removed, and provisional restorations were placed. After approximately 3 months of follow-up, allergic symptoms had resolved, and the patient received the definitive prosthetic treatment. A monolithic zirconia FPD was selected for the molars, and a porcelain layered zirconia FPD was selected for the anterior dentition. The patient wished to improve the form of the contralateral maxillary anterior tooth, for which a laminate veneer restoration was planned. For the placement of the zirconia FPDs, alumina blasting was applied to the inner surface of the FPDs, and the placement operation was performed according to the instruction manual for the adhesive resin luting agent used. After completion of prosthetic treatment, maintenance was performed every 4 months, and 4 years and 4 months have passed. The periodontium was in good condition, and there was no evidence of secondary caries, debonding, fracture of the FPDs, or abnormal jaw function. Allergic symptoms are in remission, and the FPDs are in good condition based on patient satisfaction.
Dental metal allergy is a type of contact dermatitis brought on by a known or suspected allergic reaction to metallic materials used in dental procedures that are placed in the oral cavity. Since it was first reported in 1928, the prevalence and etiology of this allergy have been investigated in several clinical, in vitro, and animal studies [1]. However, the causes of dental metal allergies remain poorly understood despite a recent increase in the number of affected individuals [1]. The basis of dental metal allergy treatment is the identification and removal of suspected metals and modification of the environment to avoid contact with the allergen (removal and replacement therapy). This report describes the case of a patient with oral lichen planus due to a dental metal allergy, who was treated successfully by removing the suspected metal allergens and replacing them with a zirconia centered non-metal based fixed partial denture (FPD).
A 52-year-old woman presented to the Prosthodontic Department, Meikai University Hospital, in October 2018. The patient’s chief complaint was that she wished to have all intraoral metal elements removed. The patient’s medical history included a blister on the central part of the palate in August 2018, which led to a visit to a nearby dentist. The patient was prescribed a mouthwash, but had contact pain on the palate and difficulty eating; thus, the patient visited the oral surgery department of Meikai University Hospital for a thorough examination. After a thorough examination, a metal allergy was suspected, and the patient was referred to the Prosthodontic Department for removal of metal restorations in the oral cavity. The patient presented with a slightly erythematous central palate with mild ulceration. The patient’s mouth had several metallic restorations (Fig. 1). Histopathological examination and the results of a patch test led to the diagnosis of a masticatory disorder due to oral lichen planus caused by gold, palladium, and tin metal allergies.
Periodontal histology revealed periodontal pockets of 2-4 mm, with no signs of tooth mobility. Examination revealed secondary dental caries in inlays at teeth #24 and #37. The palate exhibited gingival erythema, blistering, and contact pain. The treatment strategy involved removing the metals from the tooth and replacing them with provisional restorations. As the FPDs were seated on the molars, prosthodontic treatment was performed using zirconia. Since the patient wished to improve the crown form and color of the left maxillary anterior tooth, a laminate veneer restoration was planned as an esthetic solution, and consent was obtained accordingly. Restorative and prosthodontic treatments are shown in Table 1.
At the start of the treatment, the patient was given a thorough explanation of the treatment method and precautions to be taken in cases of suspected metal allergies. Informed consent was obtained from the patient. After basic periodontal treatment, all intraoral metal restorations were removed, and provisional restorations (Unifast III, GC Corp., Tokyo, Japan) were placed using provisional cement (Hybond Temporary Cement Hard, Shofu Inc., Kyoto, Japan). Subsequently, tooth #37 was restored with a composite resin material (Gracefil LoFlo, Putty, GC Corp.).
After approximately 3 months of follow-up, the patient received the definitive prosthetic treatment, as the allergic symptoms had resolved. Owing to the presence of vital teeth in the planned treatment area, the amount of tooth preparation was considered. For the subjective symptoms of clenching, monolithic zirconia FPDs were selected as the materials (Luxen Multi A2, Geomedi Co., Ltd., Fukuoka, Japan) for the molars, as the tooth structure of the abutment tooth was compromised and the possibility of FPD fracture was low. A porcelain layering zirconia FPD (Luxen Multi A2, Geomedi Co., Ltd., Vintage ZR, Shofu Inc.) was selected for the FPDs, including the maxillary right anterior tooth, because of its esthetic color reproduction. In addition, the patient wished to improve the form of the contralateral maxillary anterior tooth; therefore, laminate veneer restoration using lithium disilicate glass ceramics (IPS e.max Press HT A2, Ivoclar Vivadent AG, Schaan, Liechtenstein) was selected. During the fabrication of the maxillary right anterior FPDs and maxillary left anterior laminate veneer, a diagnostic wax-up was performed. The final tooth form was confirmed by the patient, dental technician, and dentist (Fig. 2a-c). Airborne-particle abrasion (50 µm aluminum oxide, Zest Dental Solutions, San Diego, CA, USA) was performed on the inner surface of the FPD, and it was placed successfully according to the manufacturer’s instructions for the adhesive resin luting agent used (ResiCem EX, Shofu Inc.). Airborne-particle abrasion was not performed on the laminate veneers due to the possibility of cracking in the thin layer shell of the lithium disilicate glass ceramic. Therefore, an adhesive resin cement with a self-etching glass ceramic primer was used (Variolink Esthetic LC, Ivoclar Vivadent AG). All abutment teeth were cleaned with a brush cone before luting.

Intraoral photographs of initial examination
a: frontal view, b: maxillary occlusal view, c: mandibular occlusal view, d: right lateral view, e: left lateral view
Table 1 Restorative and prosthodontic treatments
| Tooth | Treatment detail | Material | Manufacturer |
|---|---|---|---|
| #37 | composite resin filling | Gracefil Loflo, Putty | GC (Tokyo, Japan) |
| #36 | monolithic zirconia crown | Luxen Multi A2 | Geomedi (Fukuoka, Japan) |
| #45-47, pontic: #46 | monolithic zirconia 3-unit fixed partial denture | Luxen Multi A2 | Geomedi |
| #16, 17 | monolithic zirconia crown | Luxen Multi A2 | Geomedi |
| #24, 25, 26, 27 | monolithic zirconia crown | Luxen Multi A2 | Geomedi |
| #11-15, pontic: #12 | porcelain layering zirconia 4-unit fixed partial denture | Luxen Multi A2 | Geomedi |
| Vintage ZR | Shofu (Kyoto, Japan) | ||
| #21, 22, 23 | laminate veneer | IPS e.max Press HT A2 | Ivoclar (Schaan, Liechtenstein) |
#14, missing at the first visit
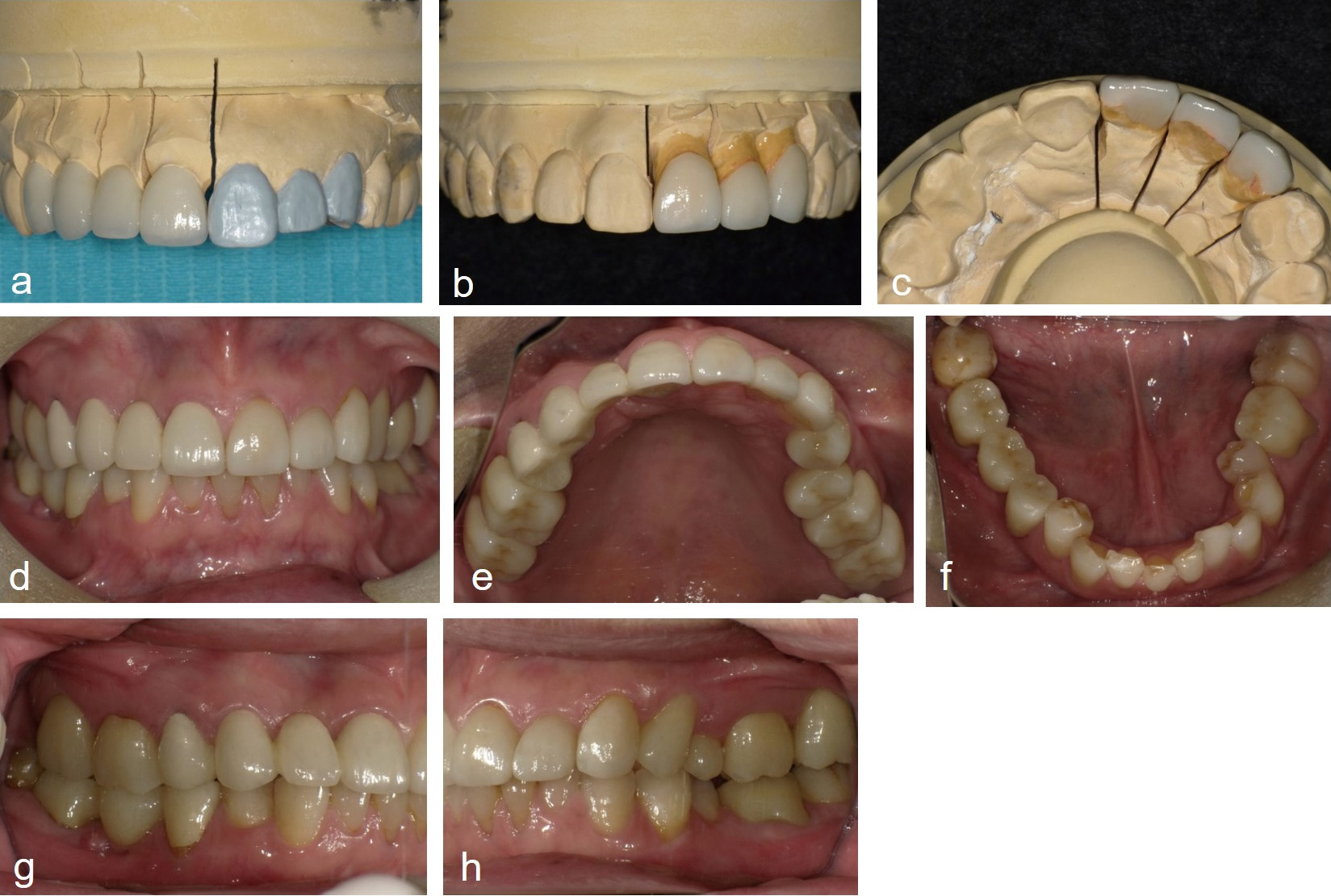
a: diagnostic wax-up of laminate veneer on maxillary left anterior teeth, b: frontal view of laminate veneer on maxillary left anterior teeth, c: lingual view of laminate veneer on maxillary left anterior teeth, d: frontal view of intraoral photographs at the end of treatment, e: maxillary occlusal view of intraoral photographs at the end of treatment, f: mandibular occlusal view of intraoral photographs at the end of treatment, g: right lateral view of intraoral photographs at the end of treatment, h: left lateral view of intraoral photographs at the end of treatment
After completion of the prosthetic treatment, maintenance was performed every 4 months, and 4 years and 4 months have passed (Fig. 2d-h). Due to the high strength of zirconia, there was concern about the wear of the antagonist teeth; however, the occlusal contact area of the interocclusal record taken at the time of maintenance showed no obvious wear (Fig. 3a, b). At the end of treatment, blisters were still present on the plantar; however, they disappeared by the time of maintenance (Fig. 3c-e). The periodontium was in good condition, and there was no evidence of secondary caries, debonding, fracture of the FPDs, or abnormal jaw function. Allergic symptoms are currently in remission, and the FPDs are in good condition based on patient satisfaction. Furthermore, the patient was instructed to wear a night guard at bedtime due to the subjective symptoms of clenching. The long-term prognosis of monolithic zirconia restorations remains unknown and will continue to be carefully monitored.
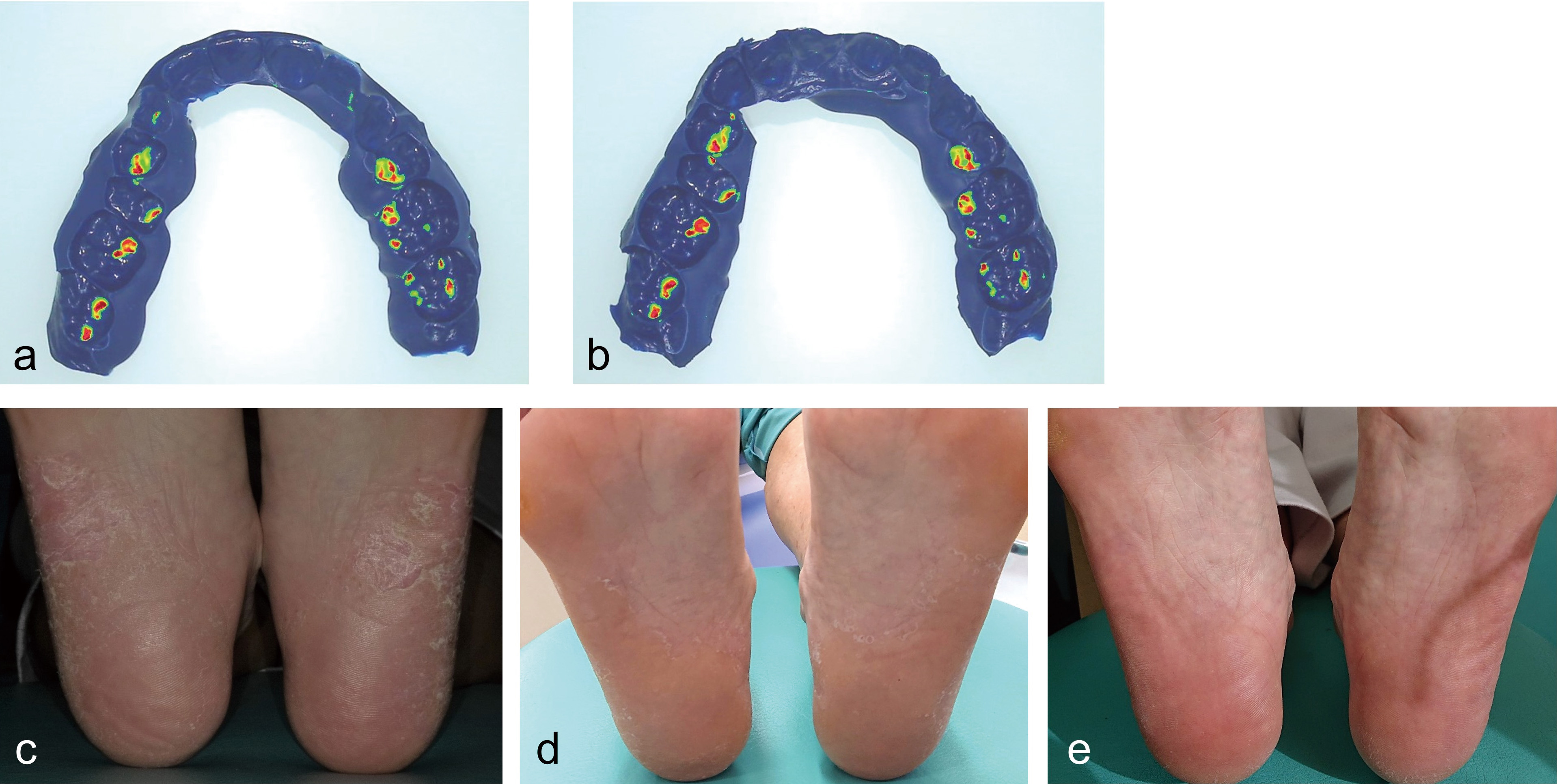
a: interocclusal record at the end of treatment, b: interocclusal record 3.5 years after completion of treatment, c: plantar photograph of the initial examination, d: plantar photograph during final prosthetic treatment, e: plantar photograph 3 years after completion of treatment
In this case, a monolithic zirconia FPD with a single zirconia material was selected due to all maxillary molar restorations being vital teeth, the limited amount of tooth material removed, the subjective symptoms of clenching, and the need to select a material with a high fracture resistance. As per the interocclusal record over a period of 3.5 years after placement, the occlusal contact areas of the entire dentition showed no change. A monolithic zirconia restoration finished with glazing was reported to show wear in all occlusal contact areas after 1 year, with a wear volume of less than 15 μm [2]. Furthermore, the average wear of natural teeth was reported to be 16.3 µm at 1 year [3], smaller than that produced by feldspar porcelain and lithium disilicate glass ceramics [3]. In addition, glazed monolithic zirconia restorations cause more wear to the antagonist enamel than polished monolithic zirconia restorations after 1 year of clinical use [4]. Therefore, in the present case, the occlusal contact surfaces of the FPD on the maxillary anterior teeth that occluded with the natural teeth were polish finished. However, since the left sided molars were finished with glazing in consideration of esthetics, it is necessary to observe the presence or absence of wear. The smooth surface of mirror-polished zirconia has been reported to have the least influence on the wear of the tooth among other computer-aided design/computer-aided manufacturing materials [5], whereas it was observed that the monolithic zirconia restoration caused around twice as much damage on the tooth enamel after two years of use when compared with that of the natural tooth [6]. Therefore, although good progress has been achieved, further long-term observations are required to determine changes in occlusal contacts.
To test for metal allergy, a patch test is performed in a specialized setting, such as by a dermatologist. After a metal allergy has been diagnosed, it is desirable to conduct a metal elemental analysis to confirm the possibility that an allergenic metal is present in the oral cavity. In this case, a patch test result led to the diagnosis of gold, palladium, and tin metal allergies. However, a metal elemental analysis was not performed at the patient's request.
Although the short-term prognosis of monolithic zirconia restorations has been reported and the success and survival rates were high [7,8], the long-term prognosis remains unknown and should be continuously monitored in the future. Furthermore, the labial and incisal surfaces of the maxillary left anterior teeth were reduced by 0.2-1.0 mm to improve the tooth form, and the laminate veneer covered the incisal edge of the tooth. Therefore, some of the dentin was partially exposed. Accordingly, there is more concern about debonding of laminate veneers in such cases than in those where the abutment bonding surface is enamel only. It has been reported that porcelain laminate veneers without incisal coverage have a higher failure rate than porcelain laminate veneers with incisal coverage [9]; however, it is necessary to observe progress to ensure that there is no debonding or breakage.
In the present case, zirconia centered non-metal based FPDs were considered useful prostheses after metal removal for lichen planus due to dental metal allergy. For a good long-term prognosis, material selection according to the case, appropriate bonding, and continuous maintenance according to the material selected are important.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
SM: conceptualization, investigation, methodology, validation, investigation, resources, data curation, writing original draft, review, and editing. TF: review and editing. YK: FPDs fabrication, review, and editing. MF: supervision, formal analysis, review, and editing. All authors read and approved the final version of the manuscript.
The authors declared no potential conflicts of interest with respect to this report, authorship, and/or publication of this article.
1) TF: t-fujita@dent.meikai.ac.jp, NA
2) YK: boss@e-job.co.jp, NA
1) MF: m-fujisawa@dent.meikai.ac.jp, https://orcid.org/0000-0001-9507-769X