2019 Volume 127 Issue 1 Pages 55-63
2019 Volume 127 Issue 1 Pages 55-63
Recent studies suggest that acquired syphilis evolved in the Old World from a non-sexually transmitted treponeme originating in the New World during early European expansion and colonization. However, when and via which route the bacteria were introduced into Asia remains uncertain. This study examined the first paleopathological evidence of syphilitic infection in an individual from the 19th century AD in South Korea. The individuals from a site identified as the middle and late Joseon period were examined for the presence of the skeletal lesions that are indicative of an acquired syphilitic infection. Direct macroscopic observation of the skeletal remains was conducted alongside radiological analysis. One individual displayed extensive pathologies throughout the cranial and postcranial skeleton. Treponematosis is the only disease that best explains the pattern of lytic cranial lesions and widespread bilateral symmetrical periosteal new bone of the postcranial elements. To date, paleopathological evidence of treponemal disease in Asia is severely limited. In this regard, this study provides meaningful data for studying the history of infectious disease in Asia. This study represents the only known archaeological case in South Korea.
Treponematosis is a chronic infectious disease caused by bacteria of the genus Treponema (de Melo et al., 2010; Walker et al., 2015), and its geographical origins have been intensely debated for nearly 500 years. All paleopathological evidence from the Old World and the New World (Brothwell, 1976; Kennedy, 1990; Pàlfi et al., 1992; Zhang, 1994; Rao et al., 1996; Mays et al., 2003; Suzuki et al., 2010) indicates that acquired syphilis did not exist prior to several hundred years ago, and that it evolved from a progenitor similar to yaws in the New World prior to being transmitted to the Old World (Harper et al., 2011). An evaluation of 54 published reports of pre-Columbian, Old World treponemal disease failed to identify Old World treponemal disease cases that exhibit definitive diagnoses and a secure pre-Columbian date (Harper et al., 2011; Zuckerman and Harper, 2016). The most recent studies suggest that acquired syphilis evolved in the Old World from a non-sexually transmitted treponeme originating from the New World during early European expansion and colonization (Armelagos et al., 2005; Harper et al., 2011; Zuckerman and Harper, 2016).
However, when and via which transmission route the bacteria were introduced into Asia remains uncertain. Furthermore, paleopathological evidence of treponemal disease in Asia is severely limited, and thus the geographical distribution of treponematosis in Asia is infrequently discussed. A few probable cases of treponematosis from China and India (e.g. Brothwell, 1976; Kennedy, 1990; Zhang, 1994; Rao et al., 1996; Suzuki et al., 2010), the Philippine Islands (Melendo and Postigo, 1995), and among the Chamorro people in the Mariana Islands have been reported (Suzuki, 1984; Rothschild and Heathcote, 1993). In addition, a few cases of lesions possibly due to acquired syphilis have been reported from archaeological sites in Japan (Suzuki, 1984).
Historical records of syphilis indicate that the disease was introduced in Asia from the outside world and then spread to China, Korean, and Japan at nearly the same time (Suzuki, 1984). Treponematosis was certainly firmly established by the mid-16th century in the urban populations of Japan (Johnston, 2009). However, to date, no skeletal case of treponemal infection had been reported among the archaeological populations of South Korea. In this study, we examined the largest-scale archaeological population of the middle and late Joseon period in Korean history to obtain evidence of skeletal lesions that are indicative of an acquired syphilitic infection. Ultimately, this research aimed to contribute to our understanding of the spread of treponemal disease in the Asia during a transitional period bridging antiquity and the modern era. In addition, this study provides important clues to the paleopathological diagnosis of syphilitic skeletal infection.
The population examined for syphilitic infection was from the 2-C area of the Eunpyeong site in Seoul, South Korea. Eunpyeong is a cemetery site located on the north-eastern border of the city wall (Figure 1). This mortuary place was built in the border region of the capital city due to a law that prohibited the burying of dead bodies inside the capital city during the Joseon period (Kang, 2009). The Central Institute of Cultural Heritage with the permission of the Cultural Heritage Administration of Korea (approval number: 2006-583) conducted the archaeological investigation of the site from September 2006 to October 2007. The Eunpyeong cemetery consists of 3466 excavated graves, but only 665 individuals were recovered. In the current research, we examined 196 individuals housed at the Department of Anthropology, Seoul National University whose remains allow analysis of their biological characteristics. The skeletal remains date to a period spanning the mid-15th to the early 20th centuries based on relative dating of burial types and grave goods (Central Institute of Cultural Heritage, 2009). Absolute dating based on the rings of trees used for coffins also estimated that most burials were constructed from the 15th to 17th centuries (Central Institute of Cultural Heritage, 2009). Most individuals examined in this research were from lime-mortar burials, although the Eunpyeong site contains both lime-mortar and earth-pit type burials. In general, skeletal remains in lime-mortar burials are well preserved due to the air-sealing effect of this technique, and it is accepted that individuals in lime-mortar burials were of higher socioeconomic status than those buried in earth-pit burials. The grave goods excavated usually consist of pottery, jade products, and bronze items.

Geographic location of the Eunpyeong cemetery site in Seoul, Korea.
In our examination of a total of 196 individuals, definite signs of syphilitic infection were found in one individual registered as EP-2(L). This individual was discovered by construction workers prior to the archaeological excavation. The EP-2 burial was comprised of two interments, possibly a husband (left side; EP-2(L)) and his wife (right side; EP-2(R)). Saryepyeonlam, a book of funerary ceremonies, describe that during the Joseon period, it was customary for a husband’s coffin to be situated to the right of his wife (Kim et al., 2011). Accelerator mass spectroscopy analysis by the National Center for Inter-University Research Facilities at Seoul National University (SNU11-R104) dates the skeleton to the 19th century (three calibrated ages: AD 1800, 1810, 1865), the late Joseon period. The EP-2(L) individual was presumed to have been buried in a lime-mortar burial type since the skeletal remains are better preserved than those from an earth-pit type.
The skeleton was fairly complete and in a relatively well-preserved condition; an intact cranium, mandible, all major limb bones, pectoral and pelvic girdles, and some vertebrae were represented. Only a portion of the left condylar process of the mandible and the epiphyseal parts of the limb bones and some hand and foot bones were fragmentary. Standard anthropological analysis of the EP-2(L) skeleton was conducted to reconstruct the biological profile. Sex estimation was based on pelvic and cranial morphology (Phenice, 1969; Brothwell, 1981; Buikstra and Ubelaker, 1994; Ubelaker, 1999; Bass, 2005). The age at death estimate was based on degenerative changes in the auricular surface and pubic symphysis (Lovejoy et al., 1985; Brooks and Suchey, 1990; Buikstra and Ubelaker, 1994), the palatal and ectocranial suture closures (Meindl and Lovejoy, 1985), and dental wear (Brothwell, 1981) in the skull. The individual was estimated to be a male, aged 40–60 years.
Pathological manifestations considered to be diagnostic of treponemal disease were the presence of caries sicca (Aufderheide et al., 1998; Ortner, 2003), gummatous lesion (Aufderheide et al., 1998; Buckley and Dias, 2002), certain distributions of gummatous and non-gummatous lesions (Steinbock, 1976; Resnick and Niwayama, 1981; Aufderheide et al., 1998; Buckley and Dias, 2002), and the systemic and bilaterally symmetrical deposition of new periosteal bone (Steinbock, 1976). Macroscopic observation and radiographs were employed to examine the pathological changes and the extent of the periosteal lesions.
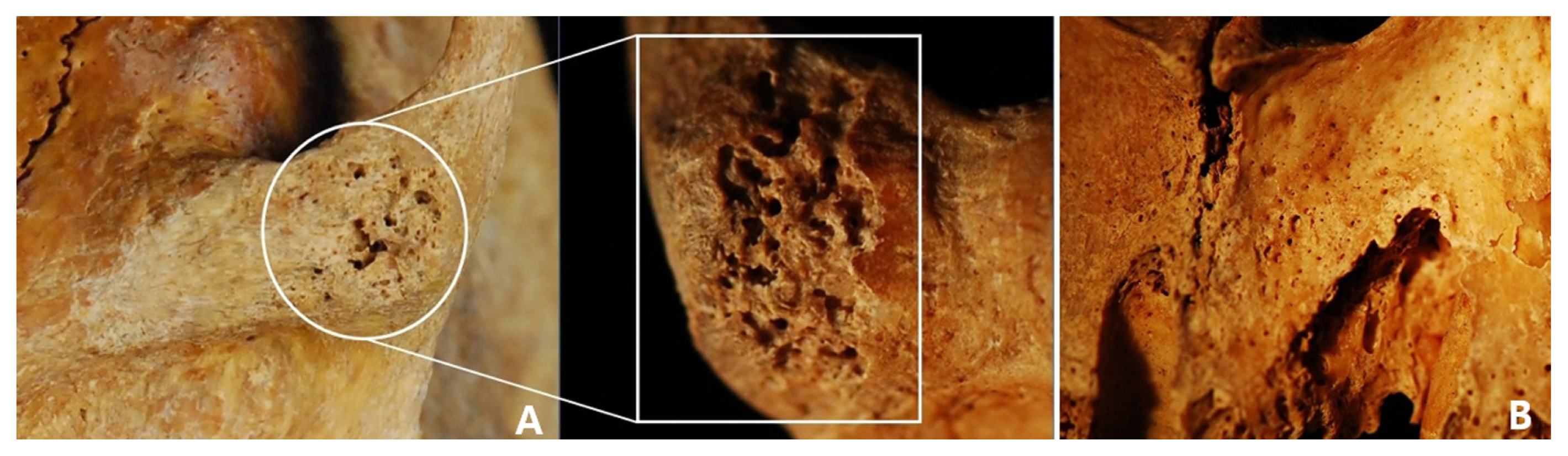
Pathological lesions are extensive throughout the cranial and postcranial skeleton. The cranium displayed pathological changes on the ectocranial surface of the cranial vault, specifically surface pitting and perforations with lytic lesions on the right frontal and parietal bones around the lateral end of the coronal suture (Figure 2A). In the right parietal bone, lytic lesions are evident macroscopically (Figure 2B). The right temporal bone had an abnormally thick margin at the superior portions because of the remodeling of newly deposited bone. No pathological changes were visible in the left temporal bone. The occipital bone was unaffected.

Lesions on the ectocranial surfaces of the cranium. (A) Lytic lesion on right frontal and parietal bones (right: close-up view of the lesion). (B) Lesions on the right parietal bone. (C) Porosity in the superior portions of the both orbit.
In the facial bones, the superior portions of the both orbit areas displayed porosity. In particular, the right orbit had more severe pitting than the left (Figure 2C). The zygomatic bone showed osteolytic lesions in the inferior surface, superior to the temporomandibular joint (Figure 3A). Fine pitting was clearly visible on the subnasal portion of the left maxilla. Additionally, the anterior maxillary alveolar process associated with the left premaxilla displayed porosity and a destructive remodeling around the alveolar socket (Figure 3B).
(A) Lytic lesions in the inferior surface of the left zygomatic bone (right: close-up view of the lesion). (B) Porosity and destructive remodeling around the alveolar socket of the anterior maxillary alveolar process.
Some evidence of dental disease was observed (Figure 4A–F, Table 1). The maxillary right central incisor, right second molar, and left lateral incisor had been lost post-mortem, and the left central incisor and the right first molar were lost ante-mortem. In the mandible, the right lateral incisor and left canine were lost post-mortem, and the left second molar was lost ante-mortem. Inflammatory lesions due to periodontal disease were visible on the alveolar portions of both jaws. Carious lesions were identified in the left first molar of the maxilla and in both left and right first molars in the mandible. Linear enamel hypoplasia was observed on both left and right canines and premolars in the mandible.

Maxillary and mandibular dentition. (A) The dental arcade of the palate was relatively narrow (white arrow: ante-mortem tooth loss). (B) The right side of alveolar portion of the maxilla. (C) The left side of the alveolar portion of the maxilla (white arrow: abscess). (D) Anterior view of mandible. (E)–(F) The right and left side of the mandible (white arrow: carious lesions).
| Upper | Lower | |||
|---|---|---|---|---|
| Left | Right | Left | Right | |
| Central incisor | AMTL | PM missing | Present | Present |
| Lateral incisor | PM missing | Present | Present | PM missing |
| Canine | Present | Present | PM missing | Present |
| 1st premolar | Present | Present | Present, LEH | Present, LEH |
| 2nd premolar | Present | Present | Present | Present |
| 1st molar | Present, caries | AMTL | Present, caries | Present, caries |
| 2nd molar | Present | PM missing | AMTL | Present, caries |
| 3rd molar | Present | Present | Present | Present |
AMTL, ante-mortem tooth loss; PM, post-mortem; LEH, linear enamel hypoplasia; Present, the tooth is preserved in its socket
Both clavicles had reactive changes on their superior and inferior surfaces. The inferior surfaces displayed cavitating lesions with irregular margins and were abnormally thick due to the remodeling of newly deposited bone (Figure 5). In particular, the midshaft of the right clavicle was more severely affected by remodeling than the left side. Osteolytic lesions were visible on the costal tuberosity and conoid tubercle, and more severe in the right clavicle than the left. Both scapulae exhibited irregular margins in the axillary border and abnormal porosity and perforation around the glenoid cavities. Among the cervical, thoracic, and lumbar vertebrae that had been preserved, degenerative joint disease was visible on the apophyseal and intervertebral joint surfaces in the cervical vertebrae. The articular surfaces in the dens of the axis and atlas had been severely affected and manifested coalescent porosity and eburnation (Figure 6).

The right clavicle. (A) The inferior surface. (B) Close-up view of the lateral end.
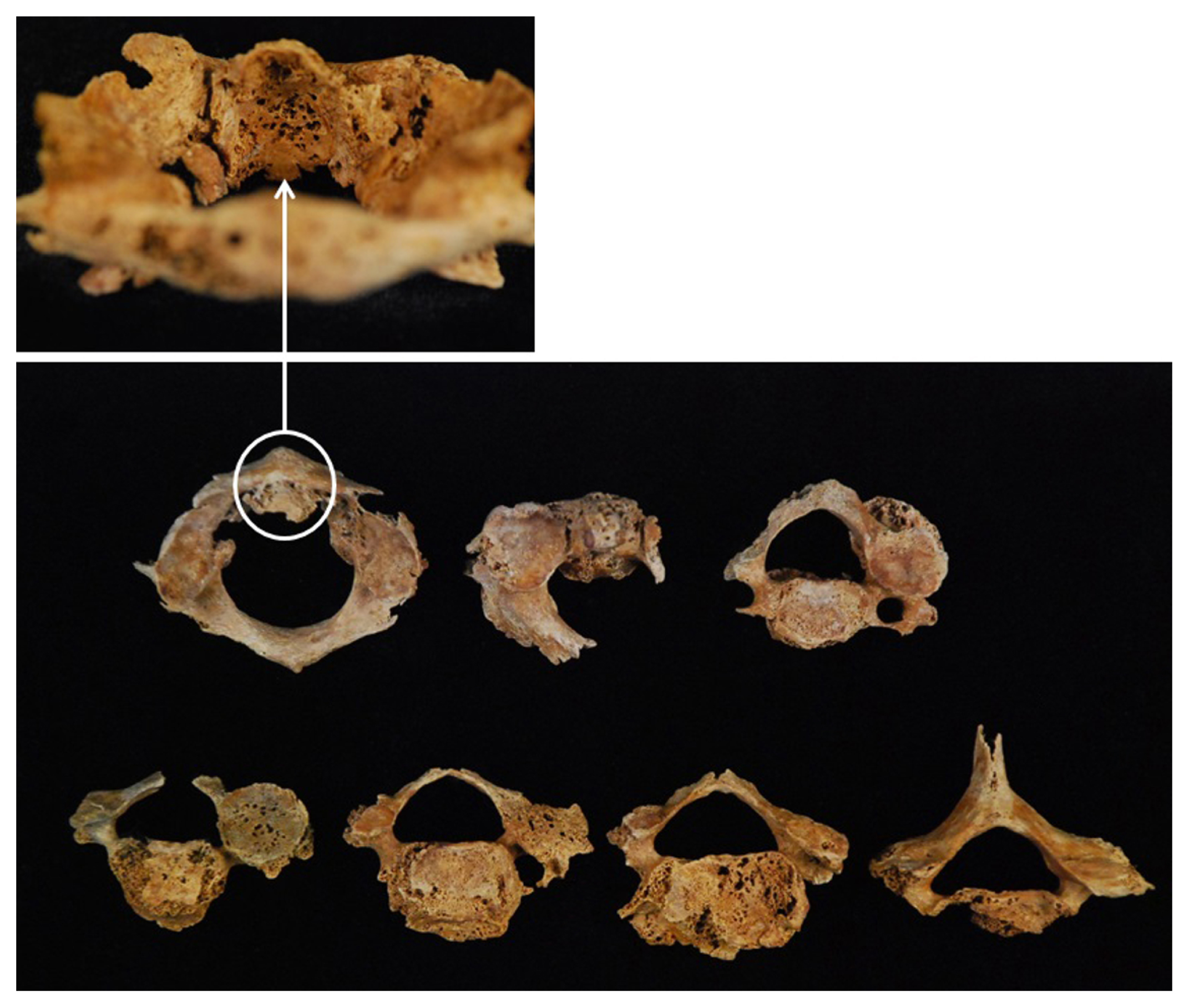
Cervical vertebrae, close-up view of the atlas showing coalescent porosity and eburnation.
Bilateral symmetrical periosteal reaction affected scapulae, clavicles, arms, and legs. The most apparent pathological changes were extensive periostitis on most of the long bones, especially those of the lower limbs (Figure 7). The shafts of the femur, tibia, and fibula were covered with thick layers of woven periosteal new bone. Well-defined lytic lesion was observed on the supracondylar portion of the posterior surfaces of the right femur. The tibiae and fibulae were covered with patches of woven bone on the surfaces, especially in the midshaft regions. On the posterior diaphysis of the left tibia, lytic lesions were found amid porotic woven bone. In addition, woven and lamellar bone formations caused circumferential enlargement in the lower limbs. Cortical thickening and narrowing of the medullar cavity were seen on the anterior–posterior radiographs of the shafts of the femur. The shafts exhibited prolific diaphyseal thickening and prominent layers of remodeled new bone. The proximal shafts of both humeri were affected by shallow lytic lesions and woven periosteal new bone formation. The proximal ends of both radii also showed osteolysis, which was likely the result of osteolytic destruction. Bilateral symmetrical changes were also observed in the ulnae, both of which exhibited periostitic lesions around the proximal and distal ends.

Close-up view of the periosteal surface of the right femur (A) and the left tibia (B). On the anteroposterior radiographs of the femora and tibiae, the entire diaphysis is thickened by new bone apposition and medullary cavities are narrowing due to the cortical thickening.
The morphology and distribution of the pathological changes in this case from the Joseon period cemetery in South Korea are indicative of a chronic systemic disease. The widespread and bilaterally symmetrical presence of remodeled periosteal bone in the limb bones is typical of treponemal disease. However, periosteal reactions alone are not pathognostic of treponemal disease in archaeological skeletal remains; various causes lead to periosteal reaction and it is evidence of non-specific infections (Ortner, 2003; Weston, 2012; Betsinger and DeWitte, 2017). Nevertheless, specific and identifiable bacterial infections such as tuberculosis, treponematosis, and leprosy (Weston, 2008) cause periosteal new bone formations (Ortner, 2003).
Treponemal disease preferentially affects the tibia, clavicle, femur, ulna, hands, and feet, along with the frontal bone of the cranium (Hackett, 1975; Steinbock, 1976; Ortner and Putschar, 1985; Bogdan and Weaver, 1992; Powell, 1992; Aufderheide et al., 1998; Buckley and Dias, 2002). The tibia, the bones surrounding the nasal cavity, and the cranial vault are frequently involved because syphilis is a blood-borne infection. The metaphyses of the long bones, which are well vascularized, are typically the sites where periostitis begins initially (Hong, 1997). It is characterized by the formation of subperiosteal bone in response to periosteal inflammation. In many cases, apposition results in the thickening of the bones (Steinbock, 1976). In the EP-2(L) skeleton, the most apparent pathological changes were extensive osteolytic and osteoblastic lesions distributed on most appendicular bones. In particular, lesions in the distal femora, the anterior surfaces of the tibiae, and midshafts of the fibulae have a sclerotic border. These characteristics are evidence of chronic periostitis caused by a specific pathogen.
Cranial lesions were found in the frontal, temporal, and parietal bones in EP-2(L). However, the perforating lesions on the cranium need to progress to the cavitating stage with an elevated sclerotic perimeter to be diagnosed as caries sicca, which is the most characteristic manifestation of treponematosis. Some authors have suggested that the skull is most commonly affected by tertiary syphilitic lesions (Ortner, 2003; Marden and Ortner, 2011; Walker et al., 2015) and that the characteristic caries sicca lesions do not develop until the tertiary stage of treponemal disease (Hackett, 1946). According to Hackett (1975), the developmental sequence of caries sicca begins with an initial clustering and confluent pits of the outer table, followed by a discrete sequence of focal superficial cavitation and the formation of unique radial scars, and progresses to nodular cavitation. The superficial cavitation and vermiculate perforations with osteolytic lesions on the EP-2(L) cranium resemble the initial phase with superficial osteitis as noted by Hackett (1983). Furthermore, the lytic lesions on the right parietal bone indicate that the bony destruction is developing contiguously from the initial phase of the caries sicca sequence. There is a possibility that the cranial lesions in this individual may have appeared transiently during the secondary stage (Steinbock, 1976; Resnick, 2002; Ortner, 2003).
EP-2(L) also exhibited inflammatory changes in the infraorbital surfaces of the maxilla and a destructive remodeling in the anterior maxillary alveolar process. Maxillary deformations accompany periostitic lesions in tertiary syphilis (Suzuki et al., 2010). However, these lesions can result from inflammation of the periosteal tissues and associated subperiosteal bone alteration, and can have various etiologies (Shang and Trinkaus, 2008).
Differential diagnoses for the lytic lesions in the skull are Langerhans cell histiocytosis, neoplasia, skeletal metastases, multiple myeloma, and hyperparathyroidism (Resnick and Niwayama, 1981; Cole and Waldron, 2011; Santos et al., 2013). We also considered pyogenic osteomyelitis and fungal infections as diagnostic options for periostitis in the postcranial bones (Mays et al., 2003). Based on the extent of skeletal involvement in EP-2(L), all options were not compatible and were thus rejected. Although differential diagnoses for lytic cranial lesions and periostitis in appendicular bones are very extensive, treponematosis is the only disease that best explains the pattern of lytic cranial lesions and widespread bilateral symmetrical periosteal new bone of the postcranial elements (Cole and Waldron, 2011). The lesions in the appendicular skeleton of EP-2(L) are strongly suggestive of treponemal disease. Trembly (1996) argued that individuals with periostitis of the tibia and two other limb bones could be diagnosed as having possible treponemal disease. In addition, the widespread oral pathologies in EP-2(L) demonstrate that he may have been experiencing a chronic hyperinflammatory reaction, which is consistent with the immunological and pathological data on syphilis (Carlson et al., 2011).
The differential diagnosis for the visible lesions in the EP-2(L) individual led us to conclude that treponemal infection, most probably acquired syphilis, may have been present during the Joseon period. Differentiating between treponemes on skeletal remains is difficult in paleopathology (Steinbock, 1976; Ortner and Putschar, 1985) because all human treponematoses are similar in pathogenesis and clinical manifestations (Giacani and Lukehart, 2014). Treponematosis infections occur in four clinically different diseases: acquired syphilis, bejel (endemic syphilis, non-acquired syphilis), yaws, and pinta. Of these, the first three affect skeletal tissue and produce similar bony lesions (Mays et al., 2003).
However, the three treponemes can be differentiated based on geography and climatic conditions (Mays et al., 2003) as presented Table 2. Whereas yaws is restricted to humid tropical environments, bejel can occur in temperate and arid rural regions, and acquired syphilis occurs in urban populations (Ortner, 2003; Powell and Cook, 2005; Walker et al., 2015). Yaws is most commonly acquired during childhood (Marden and Ortner, 2011) but can produce lesions in adults (Powell and Cook, 2005; Marks et al., 2015). The Korean climate is unsuitable for yaws, which thus can be eliminated as a possible diagnosis in EP-2(L). Bejel is usually found in warm, dry regions of developing countries and is transmitted via physical contact in populations living under unhygienic conditions (Mays et al., 2003); like yaws, bejel is usually acquired during childhood. Both yaws and bejel can reappear later in life as the latency period is 2–10 years (Giacani and Lukehart, 2014). Acquired syphilis is transmitted through sexual contact and the infection and age of onset typically occur later than for the other variants (Hoeprich, 1994). The epidemiology of acquired syphilis is most consistent with the present case.
| Feature | Yaws | Bejel | Acquired syphilis |
|---|---|---|---|
| Geographical distribution | Western/Central Africa, Southeast Asia, Pacific Islands | Sahelian Africa, Saudi Arabia | Global |
| Climatic conditions | Tropical | Hot and dry | All |
| Peak age of lesion incidence | Children (<15 years) | Children (2–15 years) | Adults |
According to the historical literature, acquired syphilis was prevalent in China and Joseon by c. 1510 (Shin, 2008). In particular, Soo-Kwang Lee (1563–1628), a Korean scholar during the middle Joseon period, stated in his book Jibong yuseol that syphilis originated from China between 1506 and 1521. Furthermore, in the first annual report issued by the Jejoongwon (the first Western-style government hospital in Korea) in 1886, syphilis was the most common disease in Korea at the time, followed by malaria. Syphilis was not only prevalent but many patients went untreated (Allen and Heron, 1886) as penicillin was not invented until the mid 20th century. Seok-Young Ji (1855–1935), a physician during the late Joseon period who contributed greatly to the elimination of smallpox in Korea, stated that syphilitic patients comprised approximately 70–80% of the visitors to his surgery (Ji, 1902).
Meanwhile, in China and Japan during the early modern period, toxic mercury chloride compounds were widely used to treat syphilis (Trambaiolo, 2015), evidence of its prevalence to some degree in both countries. Clearly, syphilis is thought to have appeared only at the beginning of the 16th century through contact with Europeans. A 1502 Ming dynasty medical text mentions acquired syphilis in the lower Yangtze region for first time in East Asia (Hernandez and Hudson, 2015). Most sources of this period referred to the disease as ‘Cantonese sores’ or ‘plum-blossom sores,’ a term that evoked the resemblance of the chancre to a plum-blossom (Chen et al., 2013). The first documented acquired syphilis outbreak in Japan dates to 1512–1513, a decade after the disease was first reported in China (Suzuki, 1984; Hernandez and Hudson, 2015), and spread rapidly throughout Japan (Trambaiolo, 2015). Paleopathological studies have reported a large number of cases of syphilis in archaeological remains from the Edo period (1603–1868) (Giannakopoulou and Suzuki, 2012). The rapid spread may be blamed on the licensed prostitute quarters that existed prior to the 20th century, where an unspecified number of men became infected with sexually transmitted diseases, and subsequently infected other members of society (Shin, 2008).
In Korea, licensed prostitute quarters were set up in the early 20th century during the Japanese colonial period. Based on the Japanese Resident-General of Korea’s inspection in 1906, the incidence of syphilis among prostitutes was high, up to 46% (Shin, 2009). In this context, Korean society may have experienced a dramatic rise in the incidence of syphilis in the late 19th and early 20th centuries. Thus, skeletal remains from this period are of significance in understanding the characteristics of acquired syphilis within the Korean peninsula, its prevalence in the Korean population and the rest of East Asia, and the disease transmission route and historical context. In this regard, the present study provides significant insight into syphilitic infection in the population prior to the modern period.
This work was supported by the Sejong University (Research Grant for Young Researchers, 2018), the Korea Government (MSIT) (National Research Foundation of Korea, 2018R1A5A7023490), and the Seoul National University (Interdisciplinary Research Grant, 2015).