Abstract
Cases in which malignant lymphoma (ML) is detected in urine cytology are rare; to the best of our knowledge, only eight cases of non-Hodgkin lymphoma that were detected on urine cytology have been reported. Herein, we report a case of diffuse large B-cell lymphoma (DLBCL) that was detected on urine cytology, focusing on the cytological findings. A 75-year-old man was referred to our hospital because of fever. Computed tomography showed a dense soft tissue lesion in the right lower ureter. Right hydronephrosis, a thickened bladder wall, and enlargement of the para-aortic, right external iliac, and inguinal lymph nodes were also observed. Clinically, upper tract or bladder urothelial carcinoma was suspected and urine cytology was performed. A small number of isolated atypical cells were detected, which showed high nuclear–cytoplasmic ratios, nuclear membrane irregularities, fine chromatin, and enlarged prominent nucleoli with scant clear cytoplasm. Liquid-based cytology with immunocytochemistry revealed that the atypical cells were positive for LCA and negative for CK AE1/AE3, suggesting the possibility of ML. In addition to urine cytology, atypical cells were observed in the urine sediment test. Bladder and inguinal lymph node biopsies were performed and a histological diagnosis of DLBCL (NOS, activated B-cell subtype) was made. Familiarity with and recognition of the characteristic cytopathological findings of ML on urine cytology are important for making a correct diagnosis.
INTRODUCTION
Urine cytology is a non-invasive, inexpensive method that is widely used to detect urothelial carcinoma (UC). In contrast, other types of malignancies are rarely detected on urine cytology, especially nonepithelial tumors, such as malignant lymphoma (ML)9). In most cases, ML in the urinary tract occurs secondary to non-Hodgkin lymphoma, arising from the adjacent lymph nodes9,12). Although histological findings of non-Hodgkin’s lymphoma in the bladder tissue are frequently reported, to our knowledge, there have been only a few detailed descriptions of the cytological findings of diffuse large B-cell lymphoma (DLBCL)9,11). Herein, we report a case of ML detected on urine cytology, based on liquid-based cytology (LBC) findings.
CASE PRESENTATION
The patient was a 75-year-old Japanese man who was being followed up for idiopathic interstitial pneumonia and was referred to our hospital because of a high fever. Medical history of the patient included prostate cancer, idiopathic interstitial pneumonia and diabetes mellitus.
Computed tomography (CT) showed right hydronephrosis and hydroureter, and a radio-dense soft tissue lesion, found in the right lower ureter approximately 3 cm upstream from the ureteric inlet to the ureteric portion (Fig. 1a). Impaired transit due to right ureteral carcinoma was suspected. Irregular wall thickening of the bladder was also
observed, suggesting bladder UC (Fig. 1b). In addition, multiple enlarged para-aortic, right external iliac, and inguinal lymph nodes were observed, suggesting lymphoproliferative disease.
Urine cytology was performed using BD SurePathTM (BD, Becton Dickinson, Ltd., Wokingham, UK) LBC, and stained using the Papanicolaou method. Cytological examination revealed atypical cells with high nuclear–cytoplasmic (N/C) ratios, nuclear enlargement, and nuclear membrane irregularities. Immunocytochemistry revealed that these cells were positive for LCA but negative for CK AE1/AE3. Urine cytology suggested the possibility of ML.
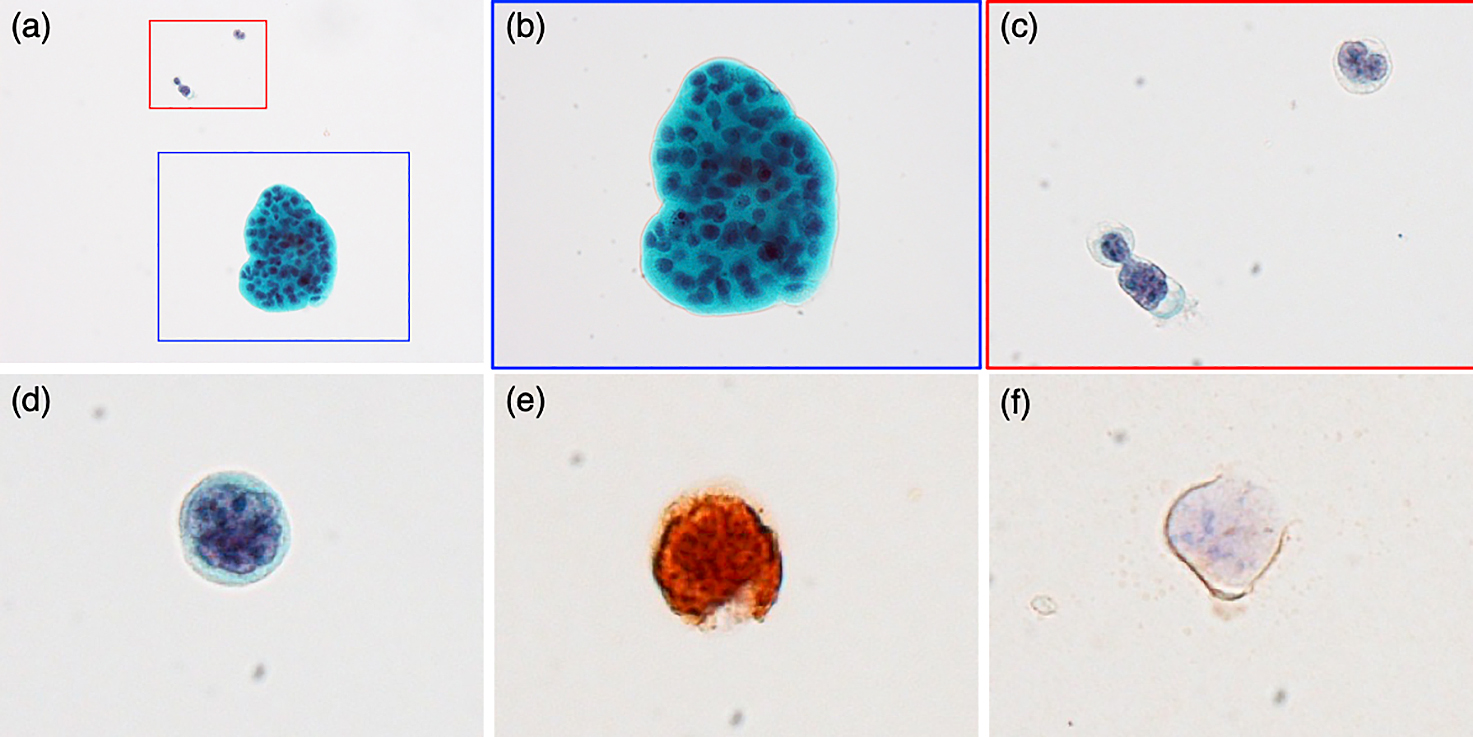
Urine sediment test findings revealed a few grayish-white cells with high N/C ratios, relatively different cell sizes, and prominent nucleoli in the unstained sediment (Fig. 2a). Sternheimer’s staining revealed that the nuclei were stained blue, although some were poorly stained (Fig. 2b). Although these characteristic findings raised the possibility of atypical lymphoid cells, the results of the urine sediment test showed atypical cells due to the low number of cells. Serum tumor markers, including CEA, CA19-9, SCC, IgG4, and soluble IL-2 receptor (S-IL2R) were evaluated, and the S-IL2R value was 4987 U/ml (normal range: 122–496 U/ml). All other markers were within the normal ranges. Cystoscopy revealed a nonpapillary tumor in the bladder.

Bladder and inguinal lymph node biopsies were performed, fixed in 10% neutral-buffered formalin, and embedded in paraffin. Sections of thickness 4 μm were made, then stained with hematoxylin and eosin. Immunohistochemistry was performed using the Bond-3 automated immunostainer platform (Leica Microsystems, Bannockburn, IL, USA) according to the manufacturer’s protocol. Antibodies against CD20, CD3, Ki-67, bcl-2, bcl-6, CD10, MUM1, CD21, c-Myc, and cyclin D1 were used for immunohistochemical staining. EBER-ISH was also performed. Histological and immunohistochemical findings revealed the characteristic features of DLBCL.
PATHOLOGY FINDINGS
Urinary cytology revealed a few epithelial clusters and isolated cells (Fig. 3a). The nuclei of the epithelial cells were small and regularly arranged, and umbrella cells were observed at the edges of cell clusters (Fig. 3b). Isolated cells showed abnormal findings, such as high N/C ratios, nuclear membrane irregularity, fine chromatin, and enlarged prominent nucleoli with scanty clear cytoplasm (Fig. 3c). Several atypical cells showed cleaved nuclei (Fig. 3d). Using a few residual LBC samples, we performed immunocytochemistry, which revealed that the isolated atypical cells were positive for LCA, but negative for CK AE1/AE3 (Fig. 3e, f). The small number of atypical cells was not sufficient to determine a cytological diagnosis; however, the cytomorphological and immunocytochemical findings suggested the possibility of ML.

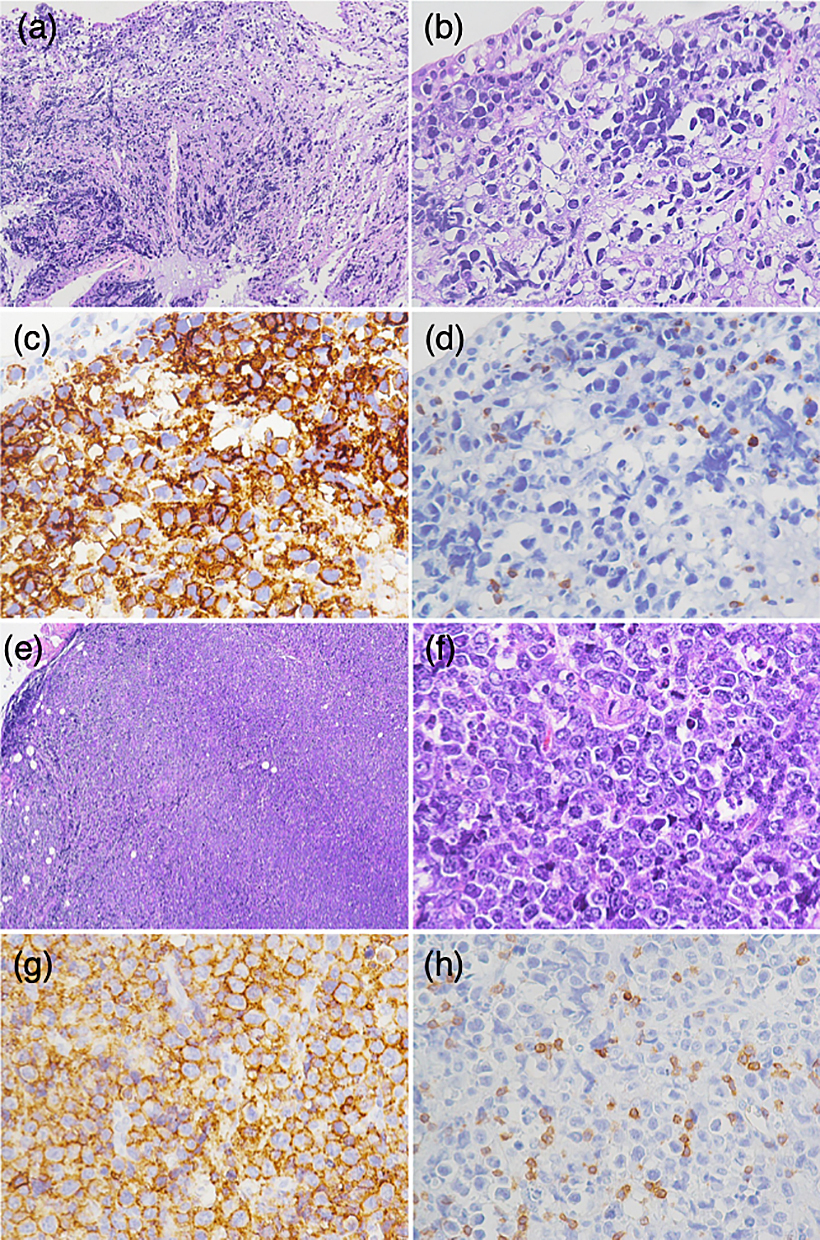
Bladder biopsy showed a diffuse proliferation of large lymphoid cells under the urothelium (Fig. 4a, b). The urothelium was infiltrated by tumor cells that were diffusely positive for CD20 and negative for CD3 (Fig. 4c, d). Inguinal lymph node biopsy showed that the normal lymph node architecture was disrupted by diffusely proliferating tumor cells that were similar in size to large lymphoid cells (Fig. 4e, f). Immunohistochemistry showed that these tumor cells were positive for CD20, bcl-2, bcl-6, MUM1, and c-Myc, and negative for CD3, CD10, CD21, and cyclin D1 (Fig. 4g, h). The Ki-67 labeling index was high (80%) and EBER-ISH was negative. The histopathological diagnosis was DLBCL, NOS, of the activated B-cell subtype. After the final diagnosis, the patient was referred to another hospital.
DISCUSSION
Urothelial carcinoma accounts for most cases of malignancy that are detected by urine cytology. Although primary lymphoma of the urinary tract is extremely rare, representing at most 0.2% of all lymphomas, most cases result from secondary involvement of the urinary tract caused by local extension from the adjacent lymph nodes1). In this study, primary DLBCL of the pelvic lymph nodes with urinary tract involvement was considered because of the enlargement of the para-aortic, right external iliac, and inguinal lymph nodes. Even in secondary lymphomas, involvement of the genitourinary tract, including the kidney, bladder, prostate, testis, ureter/urethra, and penis, is very rare, accounting for less than 5% of all extranodal lymphomas11). Most cases require histological examination of the tissue to diagnose lymphoma, and the diagnosis of ML based on urine cytology is rare1). Only eight cases of non-Hodgkin lymphoma diagnosed by a combination of urine cytology and ancillary studies (e.g., immunocytochemistry [in cell block or cytospin], flow cytometry, and FISH on urine cytology) have been reported1,3,5–8,10,13).
Patients with lymphomatous urinary tract infiltrates may not have specific symptoms such as dysuria or hematuria7,9). Furthermore, CT did not reveal any obvious lesions in some cases1). Thus, urine cytology plays an important role in the initial diagnosis of lymphomatous lesions of the urinary tract. In the present case, the presence of a radio-dense soft tissue lesion in the right ureter and bladder wall thickening initially raised the suspicion of UC of the right upper tract or bladder. However, urine cytology indicated the possibility of ML, and the patient was finally diagnosed with DLBCL based on the histological examination of the bladder and inguinal lymph node biopsy. DLBCL has a subtype called double-expressor lymphoma, in which more than 40% of cells are positive for the MYC protein and more than 50% are positive for the BCL protein. This subtype is known to have a poor prognosis2). Since the tumor cells were positive for both bcl-2 and c-Myc by immunohistochemistry in this case, it was considered a double-expressor lymphoma. Although there were a few atypical cells in the urine cytology, we considered them meaningful enough to suggest the possibility of ML based on the cytomorphological and immunocytochemical findings thereof. In other words, a cytological diagnosis of ML may have been possible if the number of cells were sufficient.
The differential cytological diagnoses in the present case included those for atypical urothelial cells. Most malignant cases of urine cytology are UC, which was initially suspected in this case. ML cells commonly appear as single cells without any cellular clusters, whereas UC cells often exhibit epithelial clusters. However, depending on the case, single atypical cells with high N/C ratio, irregular nuclear contours, and irregular chromatin are mainly observed in UC, which could be a potential pitfall6,9). The treatments for these conditions differ significantly; therefore, it is imperative to distinguish between UC and ML cells using urine cytology. Moreover, capturing the differences in nuclear contours and chromatin patterns may be helpful. The nuclear shape (round, irregular, or occasionally cleaved) was an important characteristic in this case. Although nuclear membrane irregularity is an important feature for the diagnosis of UC, cleaved nuclei are uncommon in UC cells4). In addition, UC cells on urine cytology generally shows hyperchromasia or coarse chromatin6). In contrast, the atypical cells in this case had fine nuclear chromatin. According to a previous study, the differential diagnosis included inflammatory lesions, such as chronic cystitis or follicular cystitis9); however, due to the presence of abnormal cells with enlarged nuclei and nuclear contour irregularities in the present case it was possible to make a distinction from these lesions. Nonetheless, it is difficult to diagnose ML based on cytomorphological features alone, using urine cytology. Thus, ancillary tests such as immunocytochemistry or flow cytometry are necessary9). In the present case, although a small number of ML cells were detected on urine cytology and only CK AE1/AE3 and LCA could be used for immunocytochemistry, it would have been meaningful to add immunocytochemistry using LBC, based on cytomorphological features. In addition to urine cytology, characteristic atypical cells were detected in urine sediment tests. Altogether, the clinical information and urinary sediment findings, in conjunction with cytomorphology were crucial for making a cytological diagnosis. Moreover, immunocytochemistry may be required depending on the case, as it may assist in challenging diagnoses, such as ML by urine cytology.
In conclusion, the detection of ML by urine cytology may be associated potential pitfalls. Although this condition is rare, it is important to recognize its characteristic cytopathological findings. Moreover, careful cytomorphological and immunocytochemical workup is necessary when isolated atypical cells with fine chromatin, enlarged and cleaved nuclei are detected on urine cytology.
DISCLOSURE
The authors declare no conflicts of interest in association with the present study.
REFERENCES
- 1 AbdullGaffar, B., Kamal, M.O., Khalid, M., Samuel, R., AlAbsi, N. and AlAwadi, F. 2010. Can kidney posttransplant lymphoproliferative disorder be detected in voided urine? A case report. Acta Cytol. 54: 221–224.
- 2 Alaggio, R., Amador, C., Anagnostopoulos, I., Attygalle, A.D., de Oliveira.A, I.B. Berti, E., et al. 2022. The 5th Edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 36: 1720–1748.
- 3 Arora, M. and Cossor, F.I. 2012. Diagnosis of extracavitary primary effusion lymphoma by urine cytology. Blood 119: 2707.
- 4 Barkan, G.A., Wojcik, E.M., Nayar, R., S-Prince, S., Quek, M.L., Kurtycz, Daniel F.L., et al. 2016. The Paris system for reporting urinary cytology: The quest to develop a standardized terminology. Acta Cytol. 60: 185–197.
- 5 Dormady, S.P., Mariappan, M.R., Kao, D. and Gotlib, J. 2006. Use of urine flow cytometry to verify relapse of Burkitt’s lymphoma in the genitourinary system. J. Clin. Oncol. 24: 4515–4516.
- 6 Hamele-Bena, D. and Gonzalez, A.A. 2017. Urinary tract involvement of mantle cell lymphoma diagnosed by urine cytology. Diagn. Cytopathol. 45: 1125–1127.
- 7 Jiménez-Hernández, M., López-Guillermo, A., Cobo, F., Blade, J., Aquilar, L., Villamor, N., et al. 2002. Bladder involvement of diffuse large B-cell lymphoma diagnosed by a cytological study of the urine. Leuk Lymphoma. 43:187–189.
- 8 Lobo, J., Henrique, R., Monteiro, P. and Lobo, C. 2017. ALK-negative anaplastic large cell lymphoma with urinary bladder involvement diagnosed in urine cytology: A case report and literature review. Diagn. Cytopathol. 45: 354–358.
- 9 Murro, D., Slade, J.M., Lamzabi, I. and Gattuso, P. 2015. Hematologic lesions in urine cytology. J. Am. Soc. Cytopathol. 4: 107–112.
- 10 Sarid, N., Kay, S., Angel, A., Trakhtenbrot, L., Amit, O., Herishanu, Y., et al. 2015. Diagnosis of relapsed Burkitt’s lymphoma in a urine sample: An unusual “FISHing” expedition. Isr. Med. Assoc. J. 17: 648–649.
- 11 Schniederjan, S.D. and Osunkoya, A.O. 2009. Lymphoid neoplasms of the urinary tract and male genital organs: A clinicopathological study of 40 cases. Modern Pathology 22: 1057–1065.
- 12 Venyo, A.K. 2014. Lymphoma of the urinary bladder. Adv. Urol. 2014: 327917.
- 13 Yam, L.T. and Janckila, A.J. 1985. Immunocytochemical diagnosis of lymphoma from urine sediment. Acta Cytol. 29: 827–832.