Abstract
Aims: Volume elastic modulus (VE), an index of arterial elasticity, and arterial diameter of the brachial artery can be automatically measured by a newly developed oscillometric device. We investigated the associations of VE with flow-mediated vasodilation (FMD), an index of endothelium-dependent vasodilation, nitroglycerine-induced vasodilation (NID), an index of endothelium-independent vasodilation, and intima-media thickness (IMT) of the brachial artery and association of oscillometrically measured brachial artery diameter with ultrasonographically measured brachial artery diameter in patients with cardiovascular risk factors.
Methods: Oscillometric measurements of VE and brachial artery diameter and ultrasound measurements of brachial artery diameter, FMD, NID, and IMT of the brachial artery were performed in 50 patients with cardiovascular risk factors.
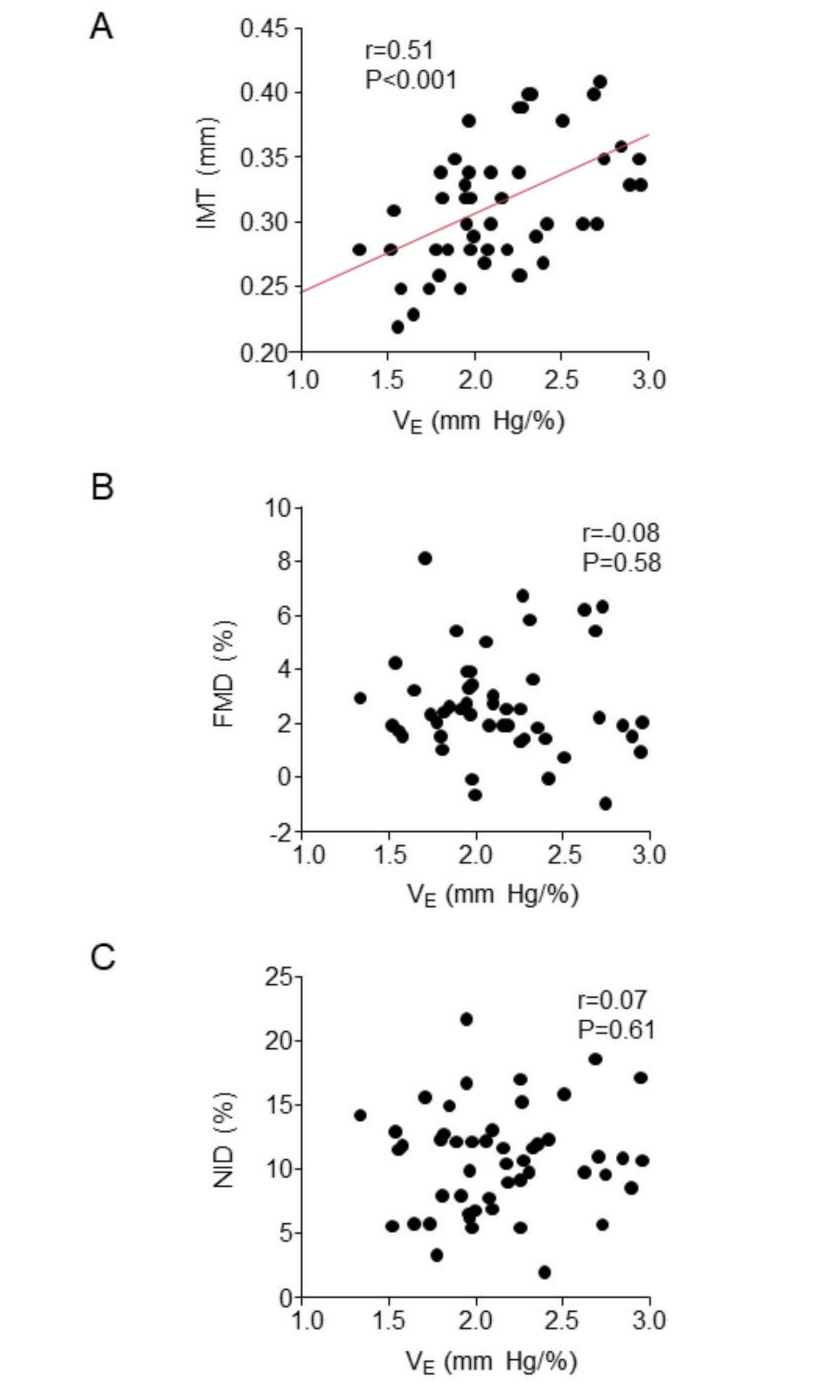
Results: The mean values were 2.1±0.4 mmHg/% for VE, 0.31±0.05 mm for brachial IMT, 4.48±0.70 mm for oscillometric brachial artery diameter, and 4.30±0.55 mm for ultrasound brachial artery diameter. VE significantly correlated with brachial IMT (r=0.51, P<0.001), whereas there was no significant correlation of VE with FMD (r=-0.08, P=0.58) or NID (r=0.07, P=0.61). Multivariate analysis revealed that VE was significantly associated with brachial IMT (β=0.33, P=0.04). Oscillometric brachial artery diameter significantly correlated with ultrasound brachial artery diameter (r=0.79, P<0.001). The Bland-Altman plot showed good agreement between oscillometric brachial artery diameter and ultrasound brachial artery diameter (mean difference, -0.17 mm; limits of agreement, -1.03 mm to 0.69 mm).
Conclusions: In patients with cardiovascular risk factors, VE may represent atherosclerotic structural alterations of the vascular wall but not vascular function. The accuracy of oscillometric measurement of brachial artery diameter is acceptable.
Introduction
Measurements of vascular function and structure of the brachial artery are useful for assessing atherosclerosis and predicting subsequent cardiovascular events
1-
5)
. Health Chronos TM-2772 (A&D Company, Tokyo, Japan), a newly developed oscillometric device, enables automatic assessments of volume elastic modulus (V
E) and arterial diameter calculated from the estimated cross-sectional area of the brachial artery
6,
7)
.
Elastic modulus is one of the indices of arterial elasticity. Vascular smooth muscle tone and structural characteristics of the arterial wall are major determinants of arterial elasticity
8,
9)
. A previous clinical study in which healthy young men were recruited showed that arterial elasticity is directly affected by endothelium-derived nitric oxide (NO) through the regulation of vascular smooth muscle tone, indicating the possibility that endothelial function is associated with arterial elasticity in healthy individuals
9)
. However, it remains unclear whether endothelial function is associated with arterial elasticity in patients with cardiovascular risk factors.
Nitroglycerine-induced vasodilation (NID) of the brachial artery, an index of endothelium-independent vasodilation, has been used as a control test for flow-mediated vasodilation (FMD). However, NID of the brachial artery itself is impaired in patients with cardiovascular risk factors and cardiovascular disease
2,
4)
. Although the precise mechanisms underlying the impairment of NID in patients with cardiovascular risk factors have not been fully elucidated, it is postulated that impaired vascular smooth muscle cell (VSMC) relaxation by reactive oxygen species (ROS) and limited vasodilation due to atherosclerotic structural alterations of the vascular wall, such as vascular calcification and thickening of the intima-media layer due to an increase in connective tissue matrix and proliferation of VSMCs, may be involved in the impairment of NID of the brachial artery
10-
13)
. Arterial elasticity may also be affected by atherosclerotic structural alterations of the vascular wall, indicating the possibility that vascular elasticity is associated with NID of the brachial artery. However, the associations between V
E, NID, and intima-media thickness (IMT) of the brachial artery are unclear.
Arterial enlargement is regarded as an early indicator of the progression of atherosclerosis
14-
18)
. A previous study showed a good agreement between brachial artery diameter assessed by the oscillometric approach (oscillometric brachial artery diameter) and brachial artery diameter assessed by ultrasound (ultrasound brachial artery diameter) in a relatively small number of healthy subjects. However, there is little information on the reliability of the oscillometric brachial artery diameter in patients with cardiovascular risk factors.
Aim
The purposes of this study were (1) to investigate the associations of V
E with FMD, NID, and IMT of the brachial artery and (2) to investigate the association of oscillometric brachial artery diameter assessed by using Health Chronos TM-2772 with ultrasound brachial artery diameter in patients with cardiovascular risk factors.
Methods
Participants
Healthy subjects without hypertension, diabetes mellitus, dyslipidemia, smoking habit, and a history of cardiovascular disease on annual medical checkups were recruited for the establishment of fundamental data on V
E in subjects without cardiovascular risk factors. Subject with blood pressure ≥ 140/90 mm Hg on the measurement day were excluded.
Participants with cardiovascular risk factors were recruited from the Cardiology Outpatient Clinic at Hiroshima University Hospital. Eligible patients were at least 20 years of age with hypertension, dyslipidemia, diabetes mellitus, smoking habit, or cardiovascular disease. Patients with contraindications to nitrate administration and patients who had received nitrate treatment were excluded. Hypertension was defined as treatment with oral antihypertensive drugs or systolic blood pressure of more than 140 mm Hg and/or diastolic blood pressure of more than 90 mm Hg measured in a sitting position on at least 3 different occasions
19)
. Diabetes mellitus was defined according to the American Diabetes Association recommendation
20)
. Dyslipidemia was defined in accordance with the third report of the National Cholesterol Education Program
21)
. Smoking status was classified into three categories: never smoker, ex-smoker, and current smoker. One pack-year was equivalent to 20 cigarettes per day for 1 year. Cardiovascular disease was defined as a history of coronary artery disease and/or stroke. The estimated glomerular filtration rate (eGFR) was calculated using the Japanese eGFR equation
22)
. Vascular tests were performed without withholding medications. The ethics committees of our institutions approved the study protocol. The study was executed in accordance with the Helsinki Declaration of 1975. Written informed consent for participation in the study was obtained from all participants. The protocol was registered in the Japan Registry of Clinical Trials (jRCTs062180013).
Study Protocol
Subjects fasted the previous night and abstained from alcohol, smoking, caffeine, and antioxidant vitamins on the day of the vascular tests. The subjects were kept in the supine position in a quiet, dark, and air-conditioned room (constant temperature of 23℃ to 26℃) throughout the study. A 23-gauge polyethylene catheter was inserted into the left deep antecubital vein to obtain blood samples. Oscillometric measurements of V
E and estimated cross-sectional area of the brachial artery and ultrasound measurements of baseline diameter, FMD, NID, and IMT of the brachial artery were performed at least 20 min after maintaining the supine position. Vascular tests were performed by skilled and trained physicians without detailed knowledge of the baseline clinical characteristics of the subjects.
Oscillometric Measurements of V
E and Estimated Cross-Sectional Area of the Brachial Artery
Oscillometric measurements of V
E and estimated cross-sectional area of the brachial artery were performed by using Health Chronos TM-2772 (A&D Company, Tokyo, Japan). Detailed information on the measurement principles of V
E and cross-sectional area of the brachial artery by using Health Chronos TM-2772 is provided in the online-only Data Supplement. In brief, this device has a main control unit and two cuffs for oscillometric blood pressure measurement and plethysmography at the left and right brachial arteries. In order to obtain a pressure (diastolic blood pressure-cuff pressure)-area (cross-sectional area of the brachial artery) curve as an appropriate logarithmic curve, the cuff pressure was decreased at regular intervals for recording several calibrated plethysmograms
7)
. V
E and estimated cross-sectional area were obtained from the pressure-area curve. V
E was defined as the increase in pressure (blood pressure-cuff pressure) per 1% increase in the cross-sectional area at the pressure point of P
0+50 mm Hg, where P
0 was the lowest cuff pressure that was required to completely collapse the brachial artery at the end of diastole. The estimated cross-sectional area was defined as the cross-sectional area at the point where a pressure (blood pressure-cuff pressure) was equal to the diastolic blood pressure
6)
. The values of V
E and estimated cross-sectional area on the right side were used for analyses. Oscillometric brachial artery diameter was calculated as 2×(estimated cross-sectional area/3.14)
0.5. A recent study has shown that intra-observer reliability was 0.93 for V
E and 0.92 for brachial artery diameter (Spearman rank correlation coefficient) and that inter-observer reproducibility was 0.81-0.90 for V
E and 0.85-0.89 for brachial artery diameter in 20 healthy subjects
23)
.
Ultrasound Measurements of IMT, FMD, and NID of the Brachial Artery
Brachial IMT, baseline diameter, FMD, and NID of the brachial artery were measured by using UNEXEF38G (UNEX Co., Nagoya, Japan), an ultrasound instrument specialized for FMD and NID measurements that is equipped with a high-resolution linear array transducer (10-MHz). This device has an automated edge detection system for continuous measurement of brachial artery diameter. Detailed information on measurements of IMT, FMD, and NID of the brachial artery is provided in the online-only Data Supplement. In brief, measurement of IMT was automatically performed on A-mode images of the far wall of the brachial artery obtained from each of 10 cardiac cycles at the end of diastole. A total of 21 points over a 3-mm length of IMT in the 10-mm longitudinal image were measured and the mean value per image was automatically calculated. The average of mean values obtained from 10 cardiac cycles was defined as IMT of the brachial artery. FMD measurements were performed using a protocol in which an occlusion cuff was placed around the forearm and was inflated to 50 mm Hg above systolic blood pressure for 5 min to induce reactive hyperemia with continuous assessment of the diameter change during reactive hyperemia. The change in brachial artery diameter in response to a sublingual tablet of 75 µg nitroglycerine was used for assessment of NID.
Statistical Analysis
The results are presented as means±SD. All reported probability values were 2-sided, and a probability value of <0.05 was considered statistically significant. Univariate linear regression analyses were performed to assess relationships among the variables. Multiple linear regression analyses were performed to identify independent variables associated with V
E and NID of the brachial artery from the covariates with
P<0.10 in the univariate linear regression analysis with age and sex forced into the models. The data were processed using JMP version pro 14 (SAS Institute, Cary, NC).
Results
In August 2015, a total of 66 men without cardiovascular risk factors or a history of cardiovascular disease (mean age, 39.9±12.4 years) were enrolled. Mean V
E was 2.1±0.4 mmHg/% in healthy men without cardiovascular risk factors.
Between January and December in 2019, a total of 50 patients (mean age, 65.8±9.4 years; age range, 39-84 years) were enrolled. The baseline clinical characteristics are summarized in
Table 1
. Of the 50 subjects, 30 (60.0%) were men, 50 (100%) had hypertension, 42 (84.0%) had dyslipidemia, 12 (24.0%) had diabetes mellitus, 3 (6.0%) were current smokers, 5 (10.0%) had coronary artery disease, and 7 (14.0%) had stroke. The mean values were 2.8±1.9% for FMD, 10.8±4.1% for NID, 4.30±0.55 mm for ultrasound brachial artery diameter, 0.31±0.05 mm for brachial IMT, 4.48±0.70 mm for oscillometric brachial artery diameter, and 2.1±0.4 mm Hg/% for V
E. No adverse events occurred during the vascular tests.
Table 1.
Clinical Characteristics of Subjects
| Variables |
All (
n = 50)
|
| Age, y |
65.8±9.4 |
| Male,
n (%)
|
30 (60.0) |
| Body mass index, kg/m
2
|
25.4±4.5 |
| Systolic blood pressure, mm Hg |
128.0±15.1 |
| Diastolic blood pressure, mm Hg |
78.5±9.1 |
| Heart rate, bpm |
66.0±12.0 |
| Total cholesterol, mg/dL |
193.9±40.1 |
| Triglycerides, mg/dL |
185.2±211.0 |
| HDL cholesterol, mg/dL |
59.7±18.3 |
| LDL cholesterol, mg/dL |
105.5±29.1 |
| Glucose, mg/dL |
110.0±44.0 |
| HbA1c, % |
5.8±1.1 |
| eGFR, ml/min/1.73 m
2
|
64.0±14.3 |
| Smoking status,
n (%)
|
|
| Never smoker |
27 (54.0) |
| Ex-smoker |
20 (40.0) |
| Current smoker, |
3 (6.0) |
| Smoking, pack year |
21.6±32.8 |
| Complication |
|
| Hypertension,
n (%)
|
50 (100) |
| Dyslipidemia,
n (%)
|
42 (84.0) |
| Diabetes mellitus,
n (%)
|
12 (24.0) |
| Coronary artery disease,
n (%)
|
5 (10.0) |
| Stroke,
n (%)
|
7 (14.0) |
| Medications,
n (%)
|
|
| Antihypertensive drugs |
49 (98.0) |
| Calcium channel blockers, % |
43 (86.0) |
| ARBs/ACEIs |
36 (72.0) |
| β-Blockers |
5 (10.0) |
| Diuretics |
14 (28.0) |
| Aldosterone antagonists |
4 (8.0) |
| Lipid-lowering drugs |
28 (56.0) |
| Antidiabetic drugs |
9 (18.0) |
| FMD, % |
2.8±1.9 |
| NID, % |
10.8±4.1 |
| Baseline brachial artery diameter, mm |
4.30±0.55 |
| Brachial IMT, mm |
0.31±0.05 |
| Baseline brachial artery diameter calculated from estimated cross-sectional area, mm |
4.48±0.70 |
| V
E, mmHg/%
|
2.1±0.4 |
HDL indicates high-density lipoprotein; LDL, low-density lipoprotein; HbA1c, hemoglobin A1c; eGFR, estimated glomerular filtration rate; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; FMD, flow- mediated vasodilation; NID, nitroglycerine-induced vasodilation; IMT, intima-media thickness; VE, volume elastic modulus.
Relationships between V
E and Variables
V
E was significantly higher in men than in women (2.3±0.4 mm Hg/% vs. 1.9±0.3 mm Hg/%,
P<0.001) without a significant difference in age between men and women (64.7±10.3 years vs. 67.5±7.9 years,
P=0.31). V
E was significantly higher in patients who had ever smoked than in patients who had never smoked (2.3±0.4 mm Hg/% vs. 2.0±0.4 mm Hg/%,
P=0.02). There was no significant difference in V
E between patients with and those without dyslipidemia (2.1±0.4 mm Hg/% vs. 2.0±0.4 mm Hg/%,
P=0.46) or between patients with and those without diabetes mellitus (2.2±0.4 mm Hg/% vs. 2.1±0.4 mm Hg/%,
P=0.33). Univariate regression analysis revealed that V
E significantly correlated with smoking pack-year (r=0.37,
P=0.009) and brachial IMT (r=0.51,
P<0.001)
(
Fig. 1A)
, whereas there was no significant correlation of V
E with FMD (r=-0.08,
P=0.58) or NID (r=0.07,
P=0.61)
(
Table 2)
(
Fig.1B and 1C)
. There was no significant association of V
E with dyslipidemia (β=0.10,
P=0.47) or diabetes mellitus (β=0.14,
P=0.33). Multivariate linear regression analysis revealed that brachial IMT was significantly associated with V
E (β=0.33,
P=0.04)
(
Table 3)
.
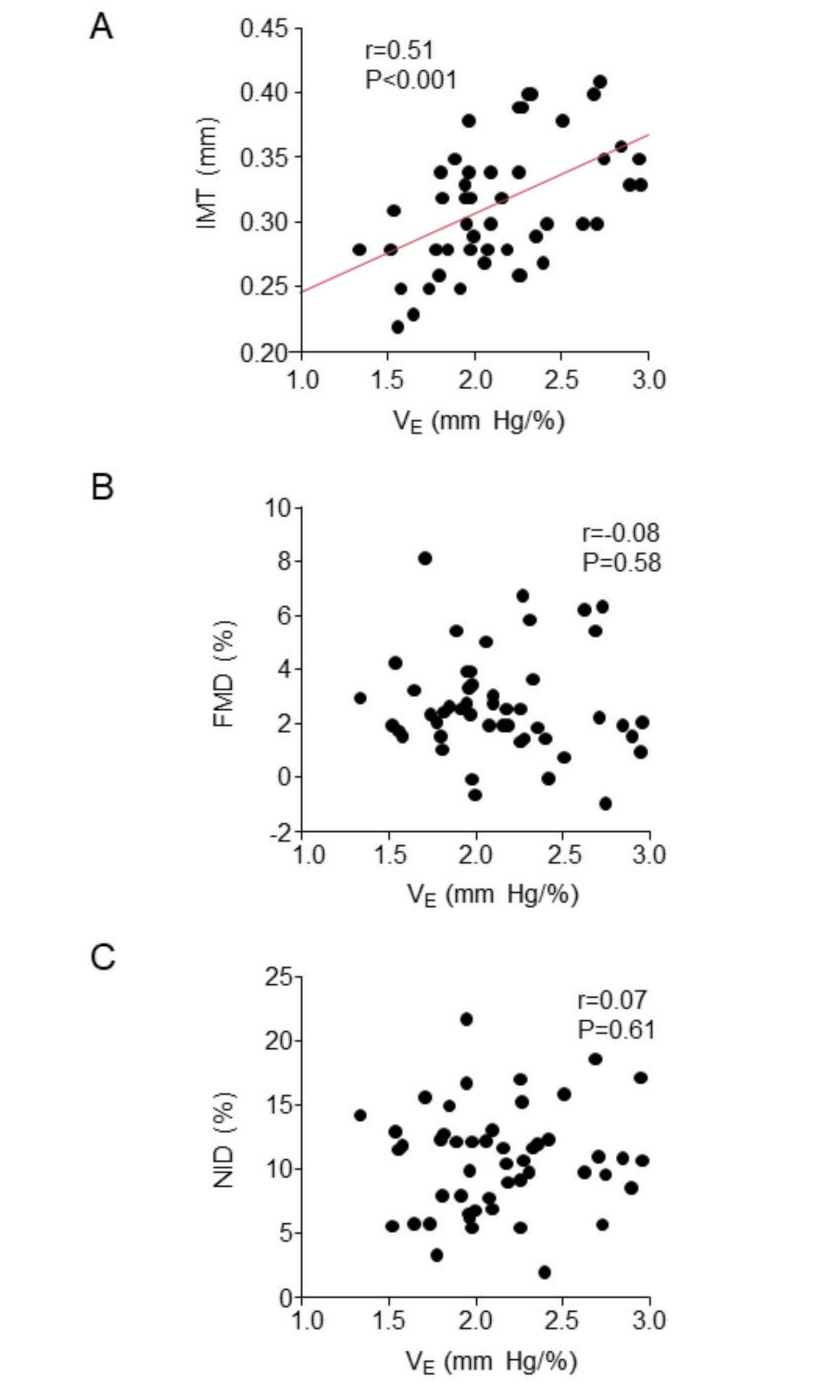
Table 2.
Univariate Regression Analysis of the Relationships Between V
E and Variables
| Variables |
V
E
|
NID |
| r |
P value
|
r |
P value
|
| Age, y |
0.17 |
0.23 |
-0.003 |
0.99 |
| Body mass index, kg/m
2
|
0.01 |
0.94 |
-0.24 |
0.09 |
| Systolic blood pressure, mm Hg |
-0.22 |
0.12 |
-0.04 |
0.80 |
| Diastolic blood pressure, mm Hg |
-0.04 |
0.80 |
0.11 |
0.47 |
| Heart rate, bpm |
-0.17 |
0.23 |
0.26 |
0.07 |
| Total cholesterol, mg/dL |
0.002 |
0.99 |
0.14 |
0.38 |
| Triglycerides, mg/dL |
0.16 |
0.29 |
0.07 |
0.63 |
| HDL cholesterol, mg/dL |
-0.10 |
0.52 |
0.09 |
0.56 |
| LDL cholesterol, mg/dL |
-0.04 |
0.77 |
0.04 |
0.77 |
| Glucose, mg/dL |
-0.04 |
0.79 |
-0.25 |
0.09 |
| HbA1c, % |
0.02 |
0.92 |
-0.29 |
0.07 |
| eGFR, ml/min/1.73 m
2
|
-0.07 |
0.620 |
0.12 |
0.44 |
| Smoking, pack year |
0.37 |
0.009 |
0.09 |
0.54 |
| FMD, % |
-0.08 |
0.58 |
0.23 |
0.11 |
| NID, % |
0.07 |
0.61 |
|
|
| Baseline brachial artery diameter, mm |
0.27 |
0.05 |
-0.38 |
0.006 |
| Brachial IMT, mm |
0.51 |
<0.001 |
0.23 |
0.12 |
| V
E, mm Hg/%
|
|
|
0.07 |
0.61 |
V
E indicates volume elastic modulus; HDL, high-density lipoprotein; LDL, low-density lipoprotein; HbA1c, hemoglobin A1c; eGFR, estimated glomerular filtration rate; FMD, flow-mediated vasodilation; NID, nitroglycerine-induced vasodilation; IMT intima-media thickness.
Table 3.
Multiple Linear Regression Analysis of the Relationships among V
E and Variables
| Variables |
β |
SE |
P value
|
| Age, y |
0.12 |
0.007 |
0.43 |
| Men |
0.28 |
0.082 |
0.17 |
| Smoking, pack year |
0.02 |
0.002 |
0.91 |
| Baseline brachial artery diameter, mm |
0.08 |
0.110 |
0.61 |
| Brachial IMT, mm |
0.33 |
1.293 |
0.04 |
The adjusted r
2 was 0.26.
V
E indicates volume elastic modulus; IMT, intima-media thickness.
Univariate regression analysis revealed that NID significantly correlated with baseline brachial artery diameter (r=-0.38,
P=0.006)
(
Table 2)
. NID was significantly related with diabetes mellitus (β=-0.36,
P=0.001) but not with dyslipidemia (β=0.10,
P=0.49). Because of multicollinearity due to a strong correlation between glucose and HbA1c (r=0.93,
P<0.001), only HbA1c was entered into the multivariate model. Multivariate linear regression analysis revealed that men (β=0.40,
P=0.009), baseline brachial artery diameter (β=-0.54,
P<0.001), and HbA1c (β=-0.31,
P=0.02) were significantly associated with NID
(
Table 4)
. When diabetes mellitus was entered into the model instead of HbA1c, similar results were obtained: men (β=0.36,
P=0.01), baseline brachial artery diameter (β=-0.46,
P=0.002), and diabetes mellitus (β=-0.34,
P=0.01) were significantly associated with NID
(
Table 4)
.
Table 4.
Multiple Linear Regression Analysis of the Relationships among Nitroglycerine-induced Vasodilation and Variables
| Variables |
Model 1 |
Model 2 |
|
β |
SE |
P value
|
β |
SE |
P value
|
| Age, y |
-0.10 |
0.065 |
0.47 |
0.06 |
0.059 |
0.66 |
| Men |
0.40 |
0.588 |
0.009 |
0.36 |
0.573 |
0.01 |
| BMI, kg/m
2
|
-0.11 |
0.149 |
0.50 |
-0.09 |
0.134 |
0.53 |
| Heart rate, bpm |
0.13 |
0.048 |
0.34 |
0.18 |
0.042 |
0.18 |
| Baseline brachial artery diameter, mm |
-0.54 |
1.162 |
<0.001 |
-0.46 |
1.084 |
0.002 |
| HbA1c, % |
-0.31 |
0.473 |
0.02 |
|
|
|
| Diabetes mellitus |
|
|
|
-0.34 |
0.619 |
0.01 |
The adjusted r
2 were 0.31 for model 1and model 2.
BMI indicates body mass index.
Univariate regression analysis revealed that oscillometric brachial artery diameter significantly correlated with ultrasound brachial artery diameter (r=0.79,
P<0.001)
(
Fig.2A)
. In Bland-Altman plot analysis of ultrasound brachial artery diameter and oscillometric brachial artery diameter, the mean difference of ultrasound brachial artery diameter and oscillometric brachial artery diameter was -0.17 mm and limits of agreement (mean difference±2 standard deviations of the difference) ranged from -1.03 mm to 0.69 mm
(
Fig.2B)
.
Discussion
In the present study, we demonstrated that V
E was significantly associated with brachial IMT. Atherosclerotic structural alterations of the vascular wall may be a major determinant of arterial elasticity. In contrast, there was no association of V
E with FMD or NID of the brachial artery. Oscillometric brachial artery diameter significantly correlated with ultrasound brachial artery diameter. The Bland-Altman plot showed a good agreement between oscillometric brachial artery diameter and ultrasound brachial artery diameter, indicating that the oscillometric approach can be used for assessment of brachial artery diameter in patients with cardiovascular risk factors.
A previous study showed that administration of
N
G-monomethyl-
L-arginine, an NO synthase inhibitor, decreased arterial elasticity in healthy young individuals, indicating that arterial elasticity is directly affected by endothelium-derived NO through the regulation of vascular smooth muscle tone and that endothelial function is associated with arterial elasticity
9)
. However, there was no correlation between V
E and FMD of the brachial artery in the present study including patients with cardiovascular risk factors. The mean FMD value was 2.8±1.9% in the present study. Considering that the proposed cutoff value of FMD for normal endothelial function is about 7%
24)
, endothelial function was severely impaired in patients included in the present study. These findings indicate the possibility that the insignificant correlation between V
E and FMD of the brachial artery may be due to the small contribution of constitutively released NO to vascular smooth muscle tone and arterial elasticity in patients with endothelial dysfunction who had cardiovascular risk factors.
Atherosclerotic structural alterations of the vascular wall are considered to be associated with both decreased arterial elasticity and impaired NID of the brachial artery
8,
25)
. In the present study, brachial IMT was significantly associated with V
E but not with NID of the brachial artery. These findings suggest that atherosclerotic structural alterations of the vascular wall may be a major determinant of V
E, whereas the contribution of atherosclerotic structural alterations of the vascular wall to the impairment of NID of the brachial artery may be small, resulting in no significant correlation between V
E and NID of the brachial artery. Diabetes mellitus was significantly associated with impaired NID of the brachial artery in the present study. A previous experimental study showed that the expression levels of cGMP-dependent protein kinase in VSMCs are down-regulated by a high level of glucose through an increase in ROS, indicating that the vasodilatory response of VSMCs to nitroglycerine is functionally impaired by hyperglycemia-induced ROS in patients with diabetes mellitus. The impairment of NID of the brachial artery may be mainly due to functional impairment of VSMC relaxation in response to nitroglycerine but not due to atherosclerotic structural alterations. V
E and NID of the brachial artery may represent different pathophysiological aspects of atherosclerosis.
The brachial artery tends to be enlarged in patients with cardiovascular risk factors or cardiovascular disease
14,
17)
. We previously reported that the addition of baseline brachial artery diameter to Framingham risk score improved the diagnostic accuracy for patients with cardiovascular disease
17)
. The brachial artery may be enlarged in response to increased blood flow with the existence of cardiovascular risk factors for maintaining shear stress in an appropriate range, which is important for the properly functioning endothelium
26)
. In addition, a population-based cohort study showed that baseline brachial artery diameter was a predictor of future cardiovascular events in elderly individuals
18)
. These findings indicate that brachial artery diameter can be used as a marker of atherosclerosis. In the present study, estimated brachial artery diameter converted from estimated cross-sectional area assessed by the oscillometric approach correlated well with brachial artery diameter assessed by ultrasound in patients with cardiovascular risk factors. We also confirmed by the Bland-Altman plot that oscillometric brachial artery diameter agreed sufficiently well with ultrasound brachial artery diameter in patients with cardiovascular risk factors. These findings are consistent with the results of a previous study showing a significant correlation between oscillometric brachial artery diameter measured by using a prototype device and ultrasound brachial artery diameter in healthy individuals
7)
. Regardless of the presence or absence of cardiovascular risk factors, this oscillometric method may be a reliable approach for automatic measurement of brachial artery diameter, which may be helpful for cardiovascular risk assessment.
Although there is no clinical evidence that vascular elasticity of the brachial artery is useful for predicting cardiovascular events, V
E has been shown to be associated with the presence of coronary artery disease
27)
. In addition, brachial artery diameter has been shown to be useful for predicting cardiovascular events as a marker of atherosclerosis
18)
. By using Health Chronos TM-2772, V
E and brachial artery diameter can be simultaneously, noninvasively, and automatically measured in a short time of about 5 minutes, providing additive information for cardiovascular risk assessment in patients with cardiovascular risk factors in clinical practice.
There were some limitations in this study. First, there were no significant correlations between V
E and cardiovascular risk parameters, including age, blood pressure, lipid parameters, and HbA1c in the present study, suggesting that data are insufficient to define V
E as an index of arterial elasticity. A previous study showed that V
E assessed by a prototype of Health Chronos TM-2772 significantly decreased after nitroglycerine administration in healthy subjects, supporting the notion that V
E is an index of arterial elasticity since one of the major determinants of vascular elasticity is vascular smooth muscle tone
7)
. Second, female subjects without cardiovascular risk factors were not included in the present study. Moreover, to our knowledge, there has been no clinical study in which V
E was assessed by Health Chronos TM-2772 in healthy female subjects. Therefore, fundamental data on V
E in female subjects without cardiovascular risk factors have not been established. Third, our study had a small sample size. Moreover, all of the patients included in the present study had hypertension. Further studies are needed to determine whether the results obtained in the present study are applicable to other patients, including those without hypertension, in a large population.
Conclusion
V
E and brachial artery diameter can be automatically measured by using Health Chronos TM-2772 without safety concerns. V
E may represent atherosclerotic structural alterations of the vascular wall. There was no association between V
E and vascular function. Accuracy of the oscillometric measurement of brachial artery diameter was acceptable. Further studies are needed to determine whether each parameter alone or in combination can provide additive information to traditional cardiovascular risk factors as a prognostic marker of cardiovascular events.
Acknowledgements
We thank Megumi Wakisaka, Miki Kumiji, Ki-ichiro Kawano, and Satoko Michiyama for their excellent secretarial assistance.
Sources of Founding
Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898 to Y.H.) and a Grant in Aid of Japanese Arteriosclerosis Prevention Fund (to Y.H.).
|
SUPPLEMENT DATA
Methods
Oscillometric Measurement of Estimated Area and Volume Elastic Modulus (VE)
Oscillometric measurements of estimated area and VE of the brachial artery were performed by using Health Chronos TM-2772 (A&D Company, Tokyo, Japan). Detailed principle of the measurement was previously described
1, 2)
. This device has a main control unit and two cuffs for oscillometric blood pressure measurement and plethysmography at the left and right brachial arteries. The cuff was composed of three occlusive lumens, which enabled application of uniform pressure to the brachial artery under the central lumen. The outsides of the cuff were composed of a hard material in order to avoid expansion of the occlusive lumens with increases in arterial volume so that the volumetric changes of the brachial artery were accurately reflected by the changes of cuff pressure. For measurement of brachial artery absolute volume, the device initially sought the lowest cuff pressure (P0) required to completely collapse the brachial artery at end-diastole (volume = 0). The plethysmogram of the brachial artery was recorded at this cuff pressure. During the measurement, 0.25 cc of air was put into the central lumen cuff for a calibration, which enabled determination of the absolute volumetric changes of the brachial artery from the plethysmogram obtained under the condition of cuff inflation. The cuff pressure was decreased at regular intervals for recording calibrated plethysmogram several times in order to obtain a pressure (blood pressure-cuff pressure) -area (cross-sectional area of the brachial artery) curve as an approximate logarithmic curve. The brachial cross-sectional area was calculated by dividing the brachial artery volume by the brachial artery cuff length. The estimated area and VE were obtained from the pressure-area curve. The estimated area was defined as the cross- sectional area of the brachial artery at the point where a pressure (blood pressure-cuff pressure) was equal to the diastolic blood pressure. VE was defined as the increase in the pressure (blood pressure-cuff pressure) per 1% increase in the cross-sectional area at the pressure point of P0+50 mmHg.
Measurement of Brachial Intima-Media Thickness (IMT)
Before flow-mediated vasodilation (FMD) measurement, baseline longitudinal ultrasonographic images of the brachial artery, obtained at the end of diastole (defined as the R wave of an electrocardiogram) form each of 10 cardiac cycles, were automatically stored on a hard disk for off-line assessment of IMT using an UNEXEF 18G ultrasound unit (UNEX Co., Nagoya, Japan) with a linear, phased-array high-frequency (10-MHz) transducer
3)
. Measurement of IMT was automatically performed on A-mode images of the far wall of the brachial artery. The analysis system automatically chose the measurement point where an image of the posterior intimal interface was clearly obtained. If the measurement point was inappropriate, another clear image site could be manually selected for measurement. A total of 21 points over a 3-mm length of IMT in the 10-mm longitudinal image depicted in the analysis display were measured and the mean value per image was automatically calculated. IMT was measured at the same point in each image. The average of mean values obtained from 10 cardiac cycles was defied as IMT of the brachial artery.
Measurement of FMD and Nitroglycerine-Induced Vasodilation (NID)
Vascular response to reactive hyperemia in the brachial artery was used for assessment of endothelium- dependent FMD. A high-resolution linear artery transducer was coupled to computer-assisted analysis software (UNEXEF18G, UNEX Co, Nagoya, Japan) that used an automated edge detection system for measurement of brachial artery diameter. A blood pressure cuff was placed around the forearm. The brachial artery was scanned longitudinally 5 to 10 cm above the elbow. When the clearest B-mode image of the anterior and posterior intimal interfaces between the lumen and vessel wall was obtained, the transducer was held at the same point throughout the scan by a special probe holder (UNEX Co) to ensure consistency of the image. Depth and gain setting were set to optimize the images of the arterial lumen wall interface. When the tracking gate was placed on the intima, the artery diameter was automatically tracked, and the waveform of diameter changes over the cardiac cycle was displayed in real time using the FMD mode of the tracking system. This allowed the ultrasound images to be optimized at the start of the scan and the transducer position to be adjusted immediately for optimal tracking performance throughout the scan. Pulsed Doppler flow was assessed at baseline and during peak hyperemic flow, which was confirmed to occur within 15 s after cuff deflation. Blood flow velocity was calculated from the color Doppler data and was displayed as a waveform in real time. The baseline longitudinal image of the artery was acquired for 30 s, and then the blood pressure cuff was inflated to 50 mm Hg above systolic pressure for 5 min
4)
. The longitudinal image of the artery was recorded continuously until 5 min after cuff deflation. Pulsed Doppler velocity signals were obtained for 20 s at baseline and for 10 s immediately after cuff deflation. Changes in brachial artery diameter were immediately expressed as percentage change relative to the vessel diameter before cuff inflation. FMD was automatically calculated as the percentage change in peak vessel diameter from the baseline value. Percentage of FMD [(peak diameter - baseline diameter)/baseline diameter] was used for analysis. Blood flow volume was calculated by multiplying the Doppler flow velocity (corrected for the angle) by heart rate and vessel cross-sectional area (-r2). Reactive hyperemia was calculated as the maximum percentage increase in flow after cuff deflation compared with baseline flow.
The response to nitroglycerine was used for assessment of endothelium-independent vasodilation. After acquiring baseline rest images for 30 seconds, a sublingual tablet (75 µg nitroglycerine) was given, and image of the artery were recorded continuously until the dilation reached a plateau after administration of nitroglycerine
5)
. We carefully checked in the mouth to confirm that tablet had been dissolved and absorbed a few minutes after administration of nitroglycerine. Subjects in whom the sublingually administered nitroglycerine tablet was not dissolved during the measurement were not included in this study. Nitroglycerine-induced vasodilation was automatically calculated as a percent change in peak vessel diameter from the baseline value. Percentage of NID [(peak diameter - baseline diameter)/baseline diameter] was used for analysis.
|
|
References
1) Otsuka T, Munakata R, Kato K, Kodani E, Ibuki C, Kusama Y, Seino Y and Kawada T: Oscillometric measurement of brachial artery cross-sectional area and its relationship with cardiovascular risk factors and arterial stiffness in a middle-aged male population. Hypertens Res, 2013; 36: 910-915
2) Tomiyama Y, Yoshinaga K, Fujii S, Ochi N, Inoue M, Nishida M, Aziki K, Horie T, Katoh C and Tamaki N: Accurate quantitative measurements of brachial artery cross-sectional vascular area and vascular volume elastic modulus using automated oscillometric measurements: comparison with brachial artery ultrasound. Hypertens Res, 2015; 38: 478-484
3) Iwamoto Y, Maruhashi T, Fujii Y, Idei N, Fujimura N, Mikami S, Kajikawa M, Matsumoto T, Kihara Y, Chayama K, Noma K, Nakashima A and Higashi Y: Intima-media thickness of brachial artery, vascular function, and cardiovascular risk factors. Arterioscler Thromb Vasc Biol, 2012; 32: 2295-2303
4) Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, Kajikawa M, Matsumoto T, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C, Tomiyama H, Takase B, Yamashina A and Higashi Y: Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart, 2013; 99: 1837-1842
5) Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, Kajikawa M, Matsumoto T, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C and Higashi Y: Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler Thromb Vasc Biol, 2013; 33: 1401-1408
|
References
- 1) Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK and Deanfield JE: Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet, 1992; 340: 1111-1115
- 2) Adams MR, Robinson J, McCredie R, Seale JP, Sorensen KE, Deanfield JE and Celermajer DS: Smooth muscle dysfunction occurs independently of impaired endothelium-dependent dilation in adults at risk of atherosclerosis. J Am Coll Cardiol, 1998; 32: 123-127
- 3) Iwamoto Y, Maruhashi T, Fujii Y, Idei N, Fujimura N, Mikami S, Kajikawa M, Matsumoto T, Kihara Y, Chayama K, Noma K, Nakashima A and Higashi Y: Intima-media thickness of brachial artery, vascular function, and cardiovascular risk factors. Arterioscler Thromb Vasc Biol, 2012; 32: 2295-2303
- 4) Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, Kajikawa M, Matsumoto T, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C and Higashi Y: Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler Thromb Vasc Biol, 2013; 33: 1401-1408
- 5) Kajikawa M, Maruhashi T, Hida E, Iwamoto Y, Matsumoto T, Iwamoto A, Oda N, Kishimoto S, Matsui S, Hidaka T, Kihara Y, Chayama K, Goto C, Aibara Y, Nakashima A, Noma K and Higashi Y: Combination of Flow-Mediated Vasodilation and Nitroglycerine-Induced Vasodilation Is More Effective for Prediction of Cardiovascular Events. Hypertension, 2016; 67: 1045-1052
- 6) Otsuka T, Munakata R, Kato K, Kodani E, Ibuki C, Kusama Y, Seino Y and Kawada T: Oscillometric measurement of brachial artery cross-sectional area and its relationship with cardiovascular risk factors and arterial stiffness in a middle-aged male population. Hypertens Res, 2013; 36: 910-915
- 7) Tomiyama Y, Yoshinaga K, Fujii S, Ochi N, Inoue M, Nishida M, Aziki K, Horie T, Katoh C and Tamaki N: Accurate quantitative measurements of brachial artery cross-sectional vascular area and vascular volume elastic modulus using automated oscillometric measurements: comparison with brachial artery ultrasound. Arterioscler Thromb Vasc Biol, 2015; 38: 478-484
- 8) Bank AJ, Wang H, Holte JE, Mullen K, Shammas R and Kubo SH: Contribution of collagen, elastin, and smooth muscle to in vivo human brachial artery wall stress and elastic modulus. Circulation, 1996; 94: 3263-3270
- 9) Kinlay S, Creager MA, Fukumoto M, Hikita H, Fang JC, Selwyn AP and Ganz P: Endothelium-derived nitric oxide regulates arterial elasticity in human arteries in vivo. Hypertension, 2001; 38: 1049-1053
- 10) Munzel T, Afanas’ev IB, Kleschyov AL and Harrison DG: Detection of superoxide in vascular tissue. Arterioscler Thromb Vasc Biol, 2002; 22: 1761-1768
- 11) Liu S, Ma X, Gong M, Shi L, Lincoln T and Wang S: Glucose down-regulation of cGMP-dependent protein kinase I expression in vascular smooth muscle cells involves NAD(P)H oxidase-derived reactive oxygen species. Free Radic Biol Med, 2007; 42: 852-863
- 12) Ruetten H, Zabel U, Linz W and Schmidt HH: Downregulation of soluble guanylyl cyclase in young and aging spontaneously hypertensive rats. Circ Res, 1999; 85: 534-541
- 13) Nigam A, Mitchell GF, Lambert J and Tardif JC: Relation between conduit vessel stiffness (assessed by tonometry) and endothelial function (assessed by flow-mediated dilatation) in patients with and without coronary heart disease. Am J Cardiol, 2003; 92: 395-399
- 14) Montalcini T, Gorgone G, Gazzaruso C, Sesti G, Perticone F and Pujia A: Large brachial and common carotid artery diameter in postmenopausal women with carotid atherosclerosis. Atherosclerosis, 2008; 196: 443-448
- 15) Holubkov R, Karas RH, Pepine CJ, Rickens CR, Reichek N, Rogers WJ, Sharaf BL, Sopko G, Merz CN, Kelsey SF, McGorray SP and Reis SE: Large brachial artery diameter is associated with angiographic coronary artery disease in women. Am Heart J, 2002; 143: 802-807
- 16) Montalcini T, Gorgone G, Gazzaruso C, Garzaniti A and Pujia A: Large Brachial Artery Diameter and Metabolic Syndrome in postmenopausal women. Atherosclerosis, 2010; 210: 458-460
- 17) Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, Iwamoto A, Kajikawa M, Matsumoto T, Oda N, Kishimoto S, Matsui S, Hashimoto H, Aibara Y, Yusoff FM, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C, Tomiyama H, Takase B, Kohro T, Suzuki T, Ishizu T, Ueda S, Yamazaki T, Furumoto T, Kario K, Inoue T, Koba S, Watanabe K, Takemoto Y, Hano T, Sata M, Ishibashi Y, Node K, Maemura K, Ohya Y, Furukawa T, Ito H, Ikeda H, Yamashina A and Higashi Y: Brachial artery diameter as a marker for cardiovascular risk assessment: FMD-J study. Atherosclerosis, 2018; 268: 92-98
- 18) Yeboah J, Crouse JR, Hsu FC, Burke GL and Herrington DM: Brachial flow-mediated dilation predicts incident cardiovascular events in older adults: the Cardiovascular Health Study. Circulation, 2007; 115: 2390-2397
- 19) Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, Ito M, Ito S, Iwashima Y, Kai H, Kamide K, Kanno Y, Kashihara N, Kawano Y, Kikuchi T, Kitamura K, Kitazono T, Kohara K, Kudo M, Kumagai H, Matsumura K, Matsuura H, Miura K, Mukoyama M, Nakamura S, Ohkubo T, Ohya Y, Okura T, Rakugi H, Saitoh S, Shibata H, Shimosawa T, Suzuki H, Takahashi S, Tamura K, Tomiyama H, Tsuchihashi T, Ueda S, Uehara Y, Urata H and Hirawa N: The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res, 2019; 42: 1235-1481
- 20) American Diabetes Association: clinical practice recommendations 1999. Diabetes Care, 1999; 22 Suppl 1: S1-114
- 21) Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). Jama, 2001; 285: 2486-2497
- 22) Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A and Collaborators developing the Japanese equation for estimated GFR: Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis, 2009; 53: 982-992
- 23) Ito K, Ito K, Saito K, Akasaka K and Fujii S: Estimation of cross-sectional vascular area andvolume elastic modulus in brachial arteries using automated oscillometric measurements: reproducibility between examiners and intra-rater reliability in medical laboratory. Rinsho Byori, 2020; 68: 383-389
- 24) Maruhashi T, Kajikawa M, Kishimoto S, Hashimoto H, Takaeko Y, Yamaji T, Harada T, Han Y, Aibara Y, Mohamad Yusoff F, Hidaka T, Kihara Y, Chayama K, Nakashima A, Goto C, Tomiyama H, Takase B, Kohro T, Suzuki T, Ishizu T, Ueda S, Yamazaki T, Furumoto T, Kario K, Inoue T, Koba S, Watanabe K, Takemoto Y, Hano T, Sata M, Ishibashi Y, Node K, Maemura K, Ohya Y, Furukawa T, Ito H, Ikeda H, Yamashina A and Higashi Y: Diagnostic Criteria of Flow-Mediated Vasodilation for Normal Endothelial Function and Nitroglycerin-Induced Vasodilation for Normal Vascular Smooth Muscle Function of the Brachial Artery. J Am Heart Assoc, 2020; 9: e013915
- 25) Maruhashi T, Kihara Y and Higashi Y: Assessment of endothelium-independent vasodilation: from methodology to clinical perspectives. J Hypertens, 2018; 36: 1460-1467
- 26) Chung WB, Hamburg NM, Holbrook M, Shenouda SM, Dohadwala MM, Terry DF, Gokce N and Vita JA: The brachial artery remodels to maintain local shear stress despite the presence of cardiovascular risk factors. Arterioscler Thromb Vasc Biol, 2009; 29: 606-612
- 27) Munakata R, Otsuka T, Uchiyama S, Shimura T, Kurihara O, Kimata N, Inami T, Murakami D, Ohba T, Takano M, Ibuki C, Seino Y and Shimizu W: Volume elastic modulus of the brachial artery and coronary artery stenosis in patients with suspected stable coronary artery disease. Heart Vessels, 2016; 31: 1467-1475