Abstract
Aim: Chronic inflammation is associated with atherosclerosis development. Chronic kidney disease (CKD) is an independent risk factor for cardiovascular events and is associated with chronic inflammation. We aimed to investigate the influence of C-reactive protein (CRP), an important marker of inflammation, on the clinical outcomes of patients with CKD and stable coronary artery disease (CAD) undergoing percutaneous coronary intervention (PCI).
Methods: Among patients with stable CAD and CKD who underwent PCI, 516 patients whose CRP levels were available before the PCI procedure were identified. The patients were divided into two groups according to the CRP levels: those with CRP ≥ 2.0 mg/L (high-CRP group) and those with CRP <2.0 mg/L (low-CRP group). The primary endpoint of this study was the occurrence of major adverse cardiac events (MACE), defined as a composite of cardiac death, myocardial infarction, and unplanned revascularization.
Results: Overall, the mean age of the patients was 72.5±9.7 years, and 20.7% were female. The median CRP level was 1.43 mg/L (0.6–4.9 mg/L). The median follow-up period was 3.6 years. The occurrence of MACE was significantly higher in the high-CRP group than in the low-CRP group (log-rank p<0.001). Notably, the incidence rate of cardiac death was significantly higher in the high-CRP group (log-rank p<0.001). According to the multivariable analysis, CRP level ≥ 2.0 mg/L was found to be a significant predictor of MACE (hazard ratio [HR]: 1.54, 95% confidence interval [CI]: 1.04–2.28, p=0.003), as well as estimated glomerular filtration rate (HR: 0.98, 95% CI: 0.97–0.99, p<0.01).
Conclusion: High-CRP levels adversely affect long-term cardiac events in patients with stable CAD and CKD.
Introduction
Chronic inflammation is associated with atherosclerosis development through multiple pathways with the contribution of cytokines and immune cells1). Recently, considerable attention has been focused on chronic inflammation as a residual risk factor for cardiovascular disease2). Increased inflammation is more frequently observed in patients with chronic kidney disease (CKD)3). Atherosclerosis and CKD are mutually aggravating factors that form a vicious cycle of pathology4-6), and CKD is an independent risk factor for cardiovascular events7, 8). In addition, chronic inflammation plays an important role in the development of cardiovascular disease and adverse events in patients with CKD3).
C-reactive protein (CRP) is one of the most important and commonly used markers of inflammation and has been reported to be associated with cardiovascular events9, 10). More recently, CRP has also been used as an indicator of treatment targets in patients with atherosclerosis11). Moreover, CRP is a marker of systemic inflammation and has effects on cardiac, vascular, and noncardiovascular disease or events9, 12-15). Previous reports have shown an association between increased CRP levels and adverse outcomes. However, few reports have specifically focused on cardiac events. Further accumulation of data is required to clarify the clinical significance of residual risk factors after contemporary treatment among various populations. In this study, we aimed to investigate the influence of CRP levels on clinical outcomes, especially focusing on cardiac events, in CKD patients with stable coronary artery disease (CAD).
Methods
Subjects
This was a single-center observational study. Among the patients with CKD and stable CAD who underwent percutaneous coronary intervention (PCI) at Nagoya University Hospital between 2006 and 2021, 516 patients with CKD whose CRP levels before the PCI procedure were available were identified and enrolled in the first procedure during the study period. Patients with acute coronary syndrome and those without CRP data were excluded. Data regarding baseline characteristics, medications, laboratory and echocardiographic results, and PCI procedures were obtained from the medical records. This study was approved by our institutional ethics committee and performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients.
Laboratory Examinations and Definitions
Serum CRP levels were measured using blood samples obtained at the time of admission for the PCI procedure. The patients were divided into two groups according to the CRP levels: those with CRP ≥ 2.0 mg/L (high-CRP group) and those with CRP <2.0 mg/L (low-CRP group)11).
The estimated glomerular filtration rate (eGFR) was calculated using the revised Japanese equation: eGFR (mL/min/1.73 m2)=194×serum creatinine−1.094×age−0.287×0.739 (in females)16). CKD was defined as a baseline eGFR<60 mL/min/1.73 m2. In this study, the patients were further stratified into those with eGFR ≥ 45 mL/min/1.73 m2 or those with eGFR<45 mL/min/1.73 m2.
Clinical Outcomes
The primary endpoint of this study was the occurrence of major adverse cardiac events (MACE), defined as a composite of cardiac death, myocardial infarction, and unplanned revascularization17). Cardiac death was defined as death due to a cardiac cause, sudden death, or death due to an unknown cause. Myocardial infarction was defined according to the fourth universal definition of myocardial infarction (type 1)18). Unplanned revascularization was defined as coronary revascularization for acute coronary syndrome or unplanned elective revascularization due to progressive angina pectoris. Preplanned multistage PCI was excluded. Clinical follow-up was performed during routine clinical visits or via telephone interviews.
Statistical Analysis
Continuous variables are expressed as mean±standard deviation or median (interquartile range). Categorical variables are expressed as numbers and percentages. Continuous variables were compared using the Student’s t-test or Mann–Whitney U test, and categorical variables were compared using the chi-square or Fisher’s exact test. Time-to-event data were evaluated using the Kaplan–Meier method, and the differences in event rates between the groups were evaluated using the log-rank test. Cox proportional hazard regression analyses were used to evaluate the associations between clinical events and variables. Multivariable Cox regression analysis was performed with adjustment for variables with p<0.2 on univariate analysis and judged to be of clinical significance. Hazard ratios (HRs) are presented with 95% confidence intervals (CIs). Statistical significance was set at p<0.05. All statistical analyses were performed using SPSS Statistics version 28 (IBM Corp., Armonk, NY, USA).
Result
Overall, the mean age of the patients was 72.5±9.7 years, and 79.3% were male. The median CRP level was 1.43 mg/L (interquartile range, 0.6–4.9 mg/L). Of the 516 patients, 220 (42.6%) were classified into the high-CRP group and 296 into the low-CRP group. Table 1 shows the baseline characteristics of the patients. No significant differences in age, sex, body mass index, hypertension, or diabetes mellitus between the two groups were observed. Patients in the high-CRP group had less frequent dyslipidemia than those in the low-CRP group. Left ventricular ejection fraction was significantly lower in the high-CRP group (55.1%±14.1% vs. 61.7%±12.3%, p<0.001). The baseline eGFR level was significantly lower in the high-CRP group than in the low-CRP group (35.1±19.0 vs. 45.2±14.8 mL/min/1.73 m2, p<0.001), and the prevalence of dialysis was higher in the high-CRP group than in the low-CRP group (21.4% vs. 8.4%, p<0.001).
Table 1. Baseline characteristics of patients
|
All patients (n = 516)
|
High-CRP (n = 220)
|
Low-CRP (n = 296)
|
p-value*
|
| Age, years |
72.5±9.7 |
72.9±10.0 |
72.2±9.5 |
0.45 |
| Male, n (%)
|
409 (79.3%) |
177 (80.5%) |
232 (78.45%) |
0.57 |
| Body mass index, kg/m2
|
23.4±3.8 |
23.2±4.2 |
23.6±3.4 |
0.18 |
| Hypertension, n (%)
|
416 (80.6%) |
175 (79.5%) |
241 (81.4%) |
0.59 |
| Diabetes mellitus, n (%)
|
275 (53.3%) |
119 (54.1%) |
156 (52.7%) |
0.76 |
| Dyslipidemia, n (%)
|
375 (72.7%) |
148 (67.3%) |
227 (76.7%) |
0.02 |
| Current smoker, n (%)
|
93 (18.0%) |
41 (18.6%) |
52 (17.6%) |
0.76 |
| Prior MI, n (%)
|
117 (22.7%) |
54 (24.5%) |
63 (21.3%) |
0.38 |
| Previous PCI, n (%)
|
148 (28.7%) |
65 (29.5%) |
83 (28.0%) |
0.71 |
| Previous CABG, n (%)
|
61 (11.8%) |
32 (14.5%) |
29 (9.8%) |
0.10 |
| Dialysis, n (%)
|
72 (14.0%) |
47 (21.4) |
25 (8.4) |
<0.001 |
| Laboratory data
|
|
|
|
|
| eGFR, mL/min/1.73m2
|
40.9±17.4 |
35.1±19.0 |
45.2±14.8 |
<0.001 |
| Hemoglobin, g/dl |
12.3±2.0 |
11.6±2.0 |
12.7±1.8 |
<0.001 |
| Albumin, g/dl |
3.7±0.55 |
3.4±0.52 |
3.9±0.47 |
<0.001 |
| Triglyceride, mg/dl |
135.3±28.3 |
131.4±73.4 |
138.1±75.4 |
0.31 |
| HDL-cholesterol, mg/dl |
44.2±13.3 |
40.0±11.9 |
47.2±13.5 |
<0.001 |
| LDL-cholesterol, mg/dl |
90.9±28.3 |
92.9±28.6 |
89.6±28.0 |
0.20 |
| HbA1c (NGSP), % |
6.4±1.0 |
6.5±1.1 |
6.4±0.90 |
0.28 |
| LVEF, % |
58.9±13.5 |
55.1±14.1 |
61.7±12.3 |
<0.001 |
| Medication
|
|
|
|
|
| Statin, n (%)
|
408 (79.7%) |
160 (73.7%) |
248 (84.1%) |
0.004 |
| ACE-I/ARB, n (%)
|
294 (57.4%) |
119 (54.8%) |
175 (59.3%) |
0.31 |
| β-blocker, n (%)
|
241 (47.1%) |
113 (52.1%) |
128 (43.4%) |
0.05 |
MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; LVEF, left ventricle ejection fraction; ACE-I, angiotensin converting enzyme inhibitor, ARB, Angiotensin II receptor blocker
*Comparison between patients in the high-CRP and low-CRP groups
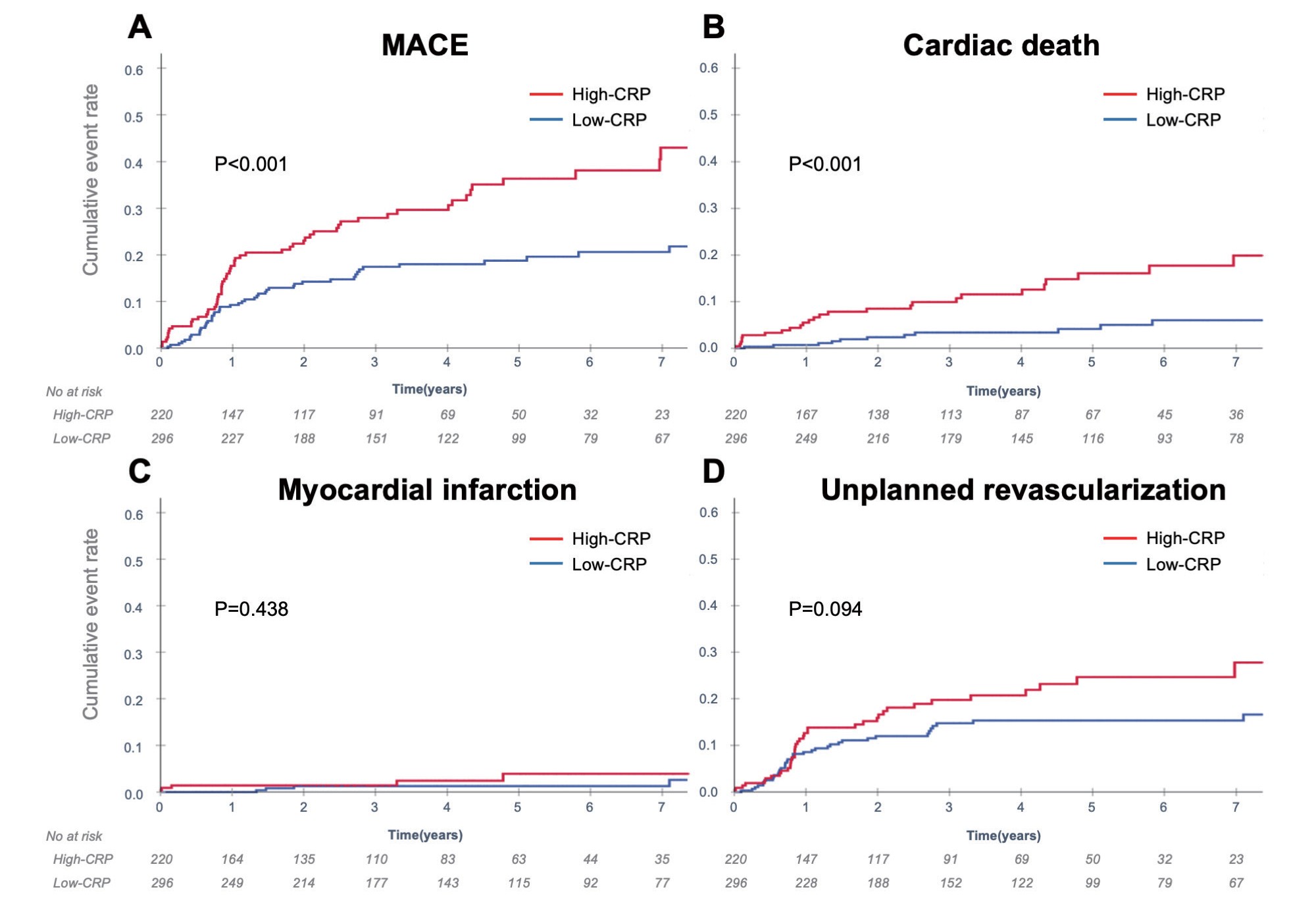
The median follow-up period was 3.6 years (interquartile range, 1.5–6.5 years). The Kaplan–Meier event curves for MACE and each component are presented in Fig.1 and Table 2. The occurrence of MACE was significantly higher in the high-CRP group than in the low-CRP group. Notably, the incidence rate of cardiac death was significantly higher in the high-CRP group, and the rate of unplanned revascularization tended to be higher in the high-CRP group. Even in the analysis after excluding dialysis patients, the occurrence of MACE was significantly higher in the high-CRP group than in the low-CRP group (Supplementary Fig.1).
Table 2. Clinical events during follow-up
|
All patients (n = 516)
|
High-CRP (n = 220)
|
Low-CRP (n = 296)
|
| MACE, n
|
116 |
62 |
54 |
| Cardiac death |
40 |
27 |
13 |
| Myocardial infarction |
10 |
5 |
5 |
| Unplanned revascularization |
80 |
38 |
42 |
MACE; major adverse cardiac events
Table 3 shows univariate and multivariable Cox regression analyses for MACE. According to the multivariable analysis, CRP ≥ 2.0 mg/L was found to be a significant predictor for MACE (HR: 1.49, 95% CI: 1.00–2.23, p=0.049), as well as body mass index (HR: 0.92, 95% CI: 0.87–0.98, p=0.004), eGFR (HR: 0.99, 95% CI: 0.97–1.00, p=0.006), and angiotensin-converting enzyme inhibitor-/angiotensin II receptor blockers use (HR: 1.74, 95% CI: 1.16–2.60, p=0.008).
Table 3. Univariate and multivariable Cox regression analyses for MACE
|
Univariate |
Multivariate |
| HR |
95% CI |
p-value
|
HR |
95% CI |
p-value
|
| Age |
0.99 |
0.98-1.01 |
0.56 |
0.99 |
0.97-1.01 |
0.44 |
| Male |
1.12 |
0.70-1.78 |
0.63 |
1.20 |
0.74-1.97 |
0.45 |
| Body mass index |
0.94 |
0.89-0.99 |
0.016 |
0.92 |
0.87-0.98 |
0.004 |
| Hypertension |
1.10 |
0.68-1.78 |
0.70 |
|
|
|
| Diabetes mellitus |
1.27 |
0.88-1.84 |
0.20 |
1.23 |
0.82-1.84 |
0.31 |
| Dyslipidemia |
0.73 |
0.49-1.08 |
0.12 |
0.82 |
0.54-1.25 |
0.37 |
| Current smoker |
0.99 |
0.60-1.61 |
0.96 |
|
|
|
| Prior MI |
1.30 |
0.86-1.95 |
0.22 |
|
|
|
| Previous PCI |
1.19 |
0.81-1.77 |
0.37 |
|
|
|
| Previous CABG |
0.66 |
0.33-1.30 |
0.23 |
|
|
|
| eGFR |
0.98 |
0.97-0.99 |
<0.001 |
0.99 |
0.97-1.00 |
0.006 |
| LVEF |
0.99 |
0.96-1.00 |
0.07 |
1.00 |
0.98-1.01 |
0.87 |
| CRP ≥ 2mg/L |
1.90 |
1.31-2.74 |
<0.001 |
1.49 |
1.00-2.23 |
0.049 |
| Statin |
0.58 |
0.39-0.86 |
0.07 |
0.74 |
0.48-1.15 |
0.18 |
| ACE-I/ARB |
1.50 |
1.01-2.22 |
0.04 |
1.74 |
1.16-2.60 |
0.008 |
| βblocker |
1.22 |
0.84-1.77 |
0.29 |
|
|
|
We further performed subgroup analyses with patients stratified according to baseline renal function. Fig.2 shows the subgroup analyses among the patients with eGFR ≥ 45 mL/min/1.73 m2 (n=290) and those with eGFR<45 mL/min/1.73 m2 (n=226). Among the patients with eGFR ≥ 45 mL/min/1.73 m2, no significant difference was observed in the occurrence of MACE between the two groups (Fig.2A), while the occurrence of MACE was significantly higher in the high-CRP group than in the low-CRP group among the patients with eGFR<45 mL/min/1.73 m2 (Fig.2B).
Discussion
The main findings of this study are as follows: in patients with CKD and stable CAD, (1) the median CRP level was 1.43 mg/L and 42.6% of the patients had a CRP level ≥ 2.0 mg/L; (2) patients with high CRP had lower renal function and were more frequently on dialysis; (3) the incidence of cardiac events was significantly higher in patients with high CRP, and the association was confirmed even after excluding dialysis patients; (4) high CRP (≥ 2.0 mg/L) was an independent predictor of long-term cardiac events as well as eGFR level; and (5) a significant association between high CRP and MACE was observed more prominently in patients with eGFR<45 mL/min/1.73 m2.
Previous studies have shown that CRP levels were higher in patients with CAD than in those without19). The reported median CRP level was 0.6–1.9 mg/L in patients with stable CAD20-25). By contrast, CRP levels in patients with CKD were shown to be higher than in those without CKD, and the median CRP level was 0.6–2.5 mg/L in patients with CKD26, 27). Furthermore, racial differences in CRP levels are believed to exist. In previous reports, the median CRP level in Japanese patients with stable CAD was 0.6–0.9 mg/L20, 22, 24) and seemed to be relatively low when compared to Western population. Although the reason for this has not been fully elucidated, genetic diversity and lifestyle differences might reflect CRP levels9). In this study, the median CRP level was 1.43 mg/L in the enrolled patients and 42.6% of the enrolled patients had a CRP level ≥ 2.0 mg/L. Considering that the included patients in this study had both stable CAD and CKD, the results would present a representative value in current clinical practice. In recent studies, CRP has been used as an indicator of treatment target11, 28). In the CANTOS study, which showed that the reduction in CRP levels with anti-inflammatory agents led to cardiovascular event reduction, the patients included as treatment targets were those with CRP levels ≥ 2 mg/L29). Therefore, our results suggest that a large number of Japanese patients with both CKD and CAD may be candidates for anti-inflammatory therapy in the near future.
Previous studies have shown that the incidences of cardiovascular events, all-cause mortality, revascularization, and myocardial infarction were significantly higher in the high-CRP group than in the low-CRP group among CAD patients10, 29-31). Recently, Nishio et al. showed that the presence of both high CRP and CKD was associated with a higher incidence of cardiovascular events, including cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke, in Japanese patients with stable CAD20). Our study included only patients with CKD, which is considered a high-risk cohort among patients with CAD, and specifically focused on cardiac events. The results showed that the incidence of composite cardiac events was significantly higher in patients with high-CRP levels in the population, and the results were in line with those of previous studies. Notably, the incidence of cardiac death was significantly higher in the high-CRP group. A previous report suggested an association between high-CRP levels and sudden cardiac death32), which may support our results. Furthermore, the incidence of unplanned revascularization was numerically higher in the high-CRP group in our study. Previous studies have shown that CRP is an independent risk factor for in-stent restenosis as well as disease progression in CAD33). Therefore, high CRP can be considered a risk factor and a useful predictor of adverse cardiac events following PCI in patients with CKD.
There are traditional and nontraditional risk factors for CAD in patients with CKD. From the early CKD stages, traditional risk factors, including hypertension, dyslipidemia, and diabetes, are frequently observed and contribute to the progression of atherosclerotic vascular disease and cardiovascular adverse events, as well as CKD progression34). Inflammation, vascular calcification, and increased proteinuria are considered nontraditional risk factors. Inflammation plays an important role in CKD itself34, 35). It is well known that statins have anti-inflammatory effects36). In this study, high CRP remained an independent predictor of long-term cardiac events, even after adjusting covariates, including statin use. The result may imply the existence of a residual inflammation in stable CAD patients with CKD undergoing contemporary treatment. Further, inflammatory substances are known to increase as CKD progresses3). However, little is known regarding the changes in the impact of such risk factors on outcomes, along with the progression of CKD. Importantly, in our study, a significant association between high-CRP level and cardiac events was observed only in patients with eGFR<45 mL/min/1.73 m2 and not in those with eGFR ≥ 45 mL/min/1.73 m2. The lack of significant impact of CRP in patients with eGFR ≥ 45 mL/min/1.73 m2 might be due to the small sample size, but at least, these results suggest that the impact of inflammation on adverse events increases as CKD progresses. That is, an intervention for inflammation might be more important than an intervention for traditional risk factors in advanced CKD patients37). Some studies have shown the importance of inflammation in cardiovascular events in dialysis patients38-40), but this study also confirmed the association among nondialysis patients.
This study has several limitations. First, it was a single-center observational study with a relatively small number of enrolled patients. Second, this study included only patients with stable CAD, and the presence of comorbidities, including infectious disease, malignant disease, and systemic inflammatory disease, was not fully evaluated. Third, this study could not determine the cut-off value of CRP for the studied population. Further accumulation of data is required to determine the specific cut-off values, which can be useful in clinical practice.
Conclusions
The presence of high CRP adversely affects long-term cardiac events in stable CAD patients with CKD. The impact of high-CRP level seems to be larger as CKD progresses. These results indicate potential candidates for future therapeutic interventions for chronic inflammation to reduce cardiac events.
Acknowledgements
This work was supported by a grant from Grant-in-Aid for Scientific Research (KAKENHI) (No.22K16100) of the Ministry of Education, Culture, Sports, Science and Technology (MEXT) and Japanese Society for the Promotion of Science (JSPA).
Conflict of Interest
Hideki Ishii received speaking and lecture fees from Astellas Pharma Inc, AstraZeneca, Daiichi Sankyo Inc and MSD. Toyoaki Murohara received speaking and lecture fees from Bayer Pharmaceutical Co LTD. Toyoaki Murohara received funding grants and speaking and lecture fees from Daiichi Sankyo Co Ltd, Dainippon Sumitomo Pharma Co Ltd, Kowa Co Ltd, MSD, Mitsubishi Tanabe Pharma Corp, Nippon Boehringer Ingelheim Co Ltd, Novartis Pharma Kabushiki Kaisha, Pfizer Japan Inc, Sanofi-aventis and Takeda Pharmaceutical Co Ltd. Toyoaki Murohara received funding grants from Astellas Pharma Inc, Otsuka Pharmaceutical Co Ltd and Teijin Pharma Ltd. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1) Raggi P, Genest J, Giles JT, Rayner KJ, Dwivedi G, Beanlands RS and Gupta M: Role of inflammation in the pathogenesis of atherosclerosis and therapeutic interventions. Atherosclerosis, 2018; 276: 98-108
- 2) Liberale L, Montecucco F, Schwarz L, Luscher TF and Camici GG: Inflammation and cardiovascular diseases: lessons from seminal clinical trials. Cardiovasc Res, 2021; 117: 411-422
- 3) Barreto DV, Barreto FC, Liabeuf S, Temmar M, Lemke HD, Tribouilloy C, Choukroun G, Vanholder R, Massy ZA and European Uremic Toxin Work G: Plasma interleukin-6 is independently associated with mortality in both hemodialysis and pre-dialysis patients with chronic kidney disease. Kidney Int, 2010; 77: 550-556
- 4) Hage FG, Venkataraman R, Zoghbi GJ, Perry GJ, DeMattos AM and Iskandrian AE: The scope of coronary heart disease in patients with chronic kidney disease. J Am Coll Cardiol, 2009; 53: 2129-2140
- 5) Oberg BP, McMenamin E, Lucas FL, McMonagle E, Morrow J, Ikizler TA and Himmelfarb J: Increased prevalence of oxidant stress and inflammation in patients with moderate to severe chronic kidney disease. Kidney Int, 2004; 65: 1009-1016
- 6) Kugler E, Cohen E, Goldberg E, Nardi Y, Levi A, Krause I, Garty M and Krause I: C reactive protein and long-term risk for chronic kidney disease: a historical prospective study. J Nephrol, 2015; 28: 321-327
- 7) Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM and Pfeffer MA: Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med, 2004; 351: 1285-1295
- 8) Irie F, Iso H, Sairenchi T, Fukasawa N, Yamagishi K, Ikehara S, Kanashiki M, Saito Y, Ota H and Nose T: The relationships of proteinuria, serum creatinine, glomerular filtration rate with cardiovascular disease mortality in Japanese general population. Kidney Int, 2006; 69: 1264-1271
- 9) Arima H, Kubo M, Yonemoto K, Doi Y, Ninomiya T, Tanizaki Y, Hata J, Matsumura K, Iida M and Kiyohara Y: High-sensitivity C-reactive protein and coronary heart disease in a general population of Japanese: the Hisayama study. Arterioscler Thromb Vasc Biol, 2008; 28: 1385-1391
- 10) Liu Y, Jia SD, Yao Y, Tang XF, Xu N, Jiang L, Gao Z, Chen J, Yang YJ, Gao RL, Xu B and Yuan JQ: Impact of high-sensitivity C-reactive protein on coronary artery disease severity and outcomes in patients undergoing percutaneous coronary intervention. J Cardiol, 2020; 75: 60-65
- 11) Ridker PM, Libby P, MacFadyen JG, Thuren T, Ballantyne C, Fonseca F, Koenig W, Shimokawa H, Everett BM and Glynn RJ: Modulation of the interleukin-6 signalling pathway and incidence rates of atherosclerotic events and all-cause mortality: analyses from the Canakinumab Anti-Inflammatory Thrombosis Outcomes Study (CANTOS). Eur Heart J, 2018; 39: 3499-3507
- 12) Koenig W, Khuseyinova N, Baumert J and Meisinger C: Prospective study of high-sensitivity C-reactive protein as a determinant of mortality: results from the MONICA/KORA Augsburg Cohort Study, 1984-1998. Clin Chem, 2008; 54: 335-342
- 13) Li S, Jing J, Li J, Wang A, Meng X and Wang Y: Elevated hs-CRP and Symptomatic Intracranial/Extracranial Artery Stenosis Predict Stroke Recurrence after Acute Ischemic Stroke or TIA. J Atheroscler Thromb, 2023; 30: 601-610
- 14) Takashima N, Nakamura Y, Miyagawa N, Kadota A, Saito Y, Matsui K, Miura K, Ueshima H and Kita Y: Association between C-Reactive Protein Levels and Functional Disability in the General Older-Population: The Takashima Study. J Atheroscler Thromb, 2023; 30: 56-65
- 15) Tanaka M, Imano H, Kubota Y, Yamagishi K, Umesawa M, Muraki I, Cui R, Hayama-Terada M, Shimizu Y, Okada T, Ohira T, Sankai T, Tanigawa T, Sato S, Kitamura A, Kiyama M, Iso H and and the CI: Serum High-Sensitivity C-Reactive Protein Levels and the Risk of Atrial Fibrillation in Japanese Population: the Circulatory Risk in Communities Study. J Atheroscler Thromb, 2021; 28: 194-202
- 16) Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A and Collaborators developing the Japanese equation for estimated GFR: Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis, 2009; 53: 982-992
- 17) Tashiro H, Tanaka A, Ishii H, Sakakibara K, Tobe A, Kataoka T, Miki Y, Hitora Y, Niwa K, Furusawa K and Murohara T: Lipid-rich large plaques in a non-culprit left main coronary artery and long-term clinical outcomes. Int J Cardiol, 2020; 305: 5-10
- 18) Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD and Group ESCSD: Fourth universal definition of myocardial infarction (2018). Eur Heart J, 2019; 40: 237-269
- 19) Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, Lowe GD, Pepys MB and Gudnason V: C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med, 2004; 350: 1387-1397
- 20) Nishio R, Dohi T, Takeuchi M, Takahashi N, Endo H, Doi S, Okai I, Iwata H, Okazaki S, Miyauchi K, Daida H and Minamino T: Combined impact of residual inflammatory risk and chronic kidney disease on long-term clinical outcomes in patients undergoing percutaneous coronary intervention. J Cardiol, 2022; 79: 509-514
- 21) Ndrepepa G, Braun S, Tada T, Guerra E, Schunkert H, Laugwitz KL and Kastrati A: Comparative prognostic value of low-density lipoprotein cholesterol and C-reactive protein in patients with stable coronary artery disease treated with percutaneous coronary intervention and chronic statin therapy. Cardiovasc Revasc Med, 2014; 15: 131-136
- 22) Suzuki S, Hashizume N, Kanzaki Y, Maruyama T, Kozuka A and Yahikozawa K: Prognostic significance of serum albumin in patients with stable coronary artery disease treated by percutaneous coronary intervention. PLoS One, 2019; 14: e0219044
- 23) Weaver JC, Ullah I, Qi M, Giannakopoulos B, Rye KA, Kockx M, Kritharides L and Krilis SA: Free Thiol beta2-GPI (beta-2-Glycoprotein-I) Provides a Link Between Inflammation and Oxidative Stress in Atherosclerotic Coronary Artery Disease. Arterioscler Thromb Vasc Biol, 2020; 40: 2794-2804
- 24) Hirano H, Kanaji Y, Sugiyama T, Hoshino M, Horie T, Misawa T, Nogami K, Ueno H, Hada M, Yamaguchi M, Sumino Y, Hamaya R, Usui E, Murai T, Lee T, Yonetsu T and Kakuta T: Impact of pericoronary adipose tissue inflammation on left ventricular hypertrophy and regional physiological indices in stable coronary artery disease patients with preserved systolic function. Heart Vessels, 2021; 36: 24-37
- 25) Karabag Y, Cagdas M, Rencuzogullari I, Karakoyun S, Artac I, Ilis D, Atalay E, Yesin M, Gursoy MO and Halil Tanboga I: Relationship between C-reactive protein/albumin ratio and coronary artery disease severity in patients with stable angina pectoris. J Clin Lab Anal, 2018; 32: e22457
- 26) Lee C, Park KH, Joo YS, Nam KH, Chang TI, Kang EW, Lee J, Oh YK, Jung JY, Ahn C, Lee KB, Park JT, Yoo TH, Kang SW and Han SH: Low High-Sensitivity C-Reactive Protein Level in Korean Patients With Chronic Kidney Disease and Its Predictive Significance for Cardiovascular Events, Mortality, and Adverse Kidney Outcomes: Results From KNOW-CKD. J Am Heart Assoc, 2020; 9: e017980
- 27) Amdur RL, Feldman HI, Gupta J, Yang W, Kanetsky P, Shlipak M, Rahman M, Lash JP, Townsend RR, Ojo A, Roy-Chaudhury A, Go AS, Joffe M, He J, Balakrishnan VS, Kimmel PL, Kusek JW, Raj DS and Investigators CS: Inflammation and Progression of CKD: The CRIC Study. Clin J Am Soc Nephrol, 2016; 11: 1546-1556
- 28) Nidorf SM, Fiolet ATL, Mosterd A, Eikelboom JW, Schut A, Opstal TSJ, The SHK, Xu XF, Ireland MA, Lenderink T, Latchem D, Hoogslag P, Jerzewski A, Nierop P, Whelan A, Hendriks R, Swart H, Schaap J, Kuijper AFM, van Hessen MWJ, Saklani P, Tan I, Thompson AG, Morton A, Judkins C, Bax WA, Dirksen M, Alings M, Hankey GJ, Budgeon CA, Tijssen JGP, Cornel JH, Thompson PL and LoDoCo2 Trial I: Colchicine in Patients with Chronic Coronary Disease. N Engl J Med, 2020; 383: 1838-1847
- 29) Ridker PM, MacFadyen JG, Everett BM, Libby P, Thuren T, Glynn RJ and Group CT: Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomised controlled trial. Lancet, 2018; 391: 319-328
- 30) Kalkman DN, Aquino M, Claessen BE, Baber U, Guedeney P, Sorrentino S, Vogel B, de Winter RJ, Sweeny J, Kovacic JC, Shah S, Vijay P, Barman N, Kini A, Sharma S, Dangas GD and Mehran R: Residual inflammatory risk and the impact on clinical outcomes in patients after percutaneous coronary interventions. Eur Heart J, 2018; 39: 4101-4108
- 31) Park DW, Yun SC, Lee JY, Kim WJ, Kang SJ, Lee SW, Kim YH, Lee CW, Kim JJ, Park SW and Park SJ: C-reactive protein and the risk of stent thrombosis and cardiovascular events after drug-eluting stent implantation. Circulation, 2009; 120: 1987-1995
- 32) Albert CM, Ma J, Rifai N, Stampfer MJ and Ridker PM: Prospective study of C-reactive protein, homocysteine, and plasma lipid levels as predictors of sudden cardiac death. Circulation, 2002; 105: 2595-2599
- 33) Baktashian M, Saffar Soflaei S, Kosari N, Salehi M, Khosravi A, Ahmadinejad M, Moohebati M, Ebrahimi M, Rahmani F, Khameneh-Bagheri R, Ahmadi M, Sadabadi F, Tayefi M, Bazhdanzadeh S, Ferns GA, Hashemi SM, Pasdar A and Ghayour-Mobarhan M: Association of high level of hs-CRP with in-stent restenosis: A case-control study. Cardiovasc Revasc Med, 2019; 20: 583-587
- 34) Jankowski J, Floege J, Fliser D, Bohm M and Marx N: Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation, 2021; 143: 1157-1172
- 35) McCullough PA: Why is chronic kidney disease the “spoiler” for cardiovascular outcomes? J Am Coll Cardiol, 2003; 41: 725-728
- 36) Ridker PM, Rifai N, Pfeffer MA, Sacks F and Braunwald E: Long-term effects of pravastatin on plasma concentration of C-reactive protein. The Cholesterol and Recurrent Events (CARE) Investigators. Circulation, 1999; 100: 230-235
- 37) Ridker PM, Tuttle KR, Perkovic V, Libby P and MacFadyen JG: Inflammation drives residual risk in chronic kidney disease: a CANTOS substudy. Eur Heart J, 2022;
- 38) Yeun JY, Levine RA, Mantadilok V and Kaysen GA: C-Reactive protein predicts all-cause and cardiovascular mortality in hemodialysis patients. Am J Kidney Dis, 2000; 35: 469-476
- 39) Panichi V, Rizza GM, Paoletti S, Bigazzi R, Aloisi M, Barsotti G, Rindi P, Donati G, Antonelli A, Panicucci E, Tripepi G, Tetta C, Palla R and Group RS: Chronic inflammation and mortality in haemodialysis: effect of different renal replacement therapies. Results from the RISCAVID study. Nephrol Dial Transplant, 2008; 23: 2337-2343
- 40) Qureshi AR, Alvestrand A, Divino-Filho JC, Gutierrez A, Heimburger O, Lindholm B and Bergstrom J: Inflammation, malnutrition, and cardiac disease as predictors of mortality in hemodialysis patients. J Am Soc Nephrol, 2002; 13 Suppl 1: S28-36