2025 Volume 19 Issue 1 Article ID: cr.2024-0104
2025 Volume 19 Issue 1 Article ID: cr.2024-0104
Objective: Herein, we present a novel flow reversal technique using dual-balloon inflation that can provide enhanced catheter stability and reliable embolic protection for percutaneous antegrade stenting in a patient with right common carotid artery (CCA) stenosis.
Case Presentation: A 75-year-old female patient with post-radiation right CCA stenosis initially underwent stenting using distal filter protection, which resulted in transient left upper limb paralysis caused by embolic infarction. After restenosis at 6 months, retreatment was performed using dual-balloon occlusion with the 9-F balloon guiding catheter in the innominate artery and the 8-F balloon guiding catheter in the right subclavian artery. Intraoperative ultrasonography confirmed a successful flow reversal, and debris was captured from the aspirated blood. The patient was discharged without neurological deficits, and postoperative imaging showed no new ischemic lesions.
Conclusion: The novel flow reversal technique using dual-balloon inflation can be effective and safe for treating right CCA stenosis by achieving both reliable embolic protection and improved catheter stability.
The optimal endovascular treatment for stenosis originating from the right common carotid artery (CCA) remains unclear due to technical challenges caused by its anatomical characteristics.1) Open retrograde stenting has a high stability for guiding the catheter and can effectively prevent cerebral embolization by clamping the internal carotid artery or CCA. However, this approach is more invasive than percutaneous antegrade stenting. Hence, it has inherent risks such as neck hematoma and cranial nerve injury.2,3) Percutaneous antegrade stenting is less invasive. Nevertheless, it is associated with a high risk of periprocedural cerebral embolization. To decrease such a risk, various techniques, including proximal flow control methods (such as flow reversal or flow arrest) and distal protection using filters, have been explored.4) Herein, we present a novel flow reversal technique using 2-balloon guiding catheters for percutaneous antegrade stenting in the treatment of right CCA stenosis. This method is believed to be more effective in preventing cerebral embolization during stent deployment and angioplasty.
A 75-year-old female patient was introduced to our neurosurgical department for the treatment of right CCA stenosis. The patient had a history of poorly controlled diabetes mellitus and papillary thyroid carcinoma that was treated with right hemithyroidectomy and postoperative radiotherapy 45 years back. She had a history of social drinking, but she never smoked. The patient did not experience an ischemic stroke event. Magnetic resonance angiography (MRA) showed severe stenosis at the origin of the CCA (Fig. 1A). Magnetization-prepared rapid acquisition with gradient echo (MP-RAGE) identified a stable carotid plaque as an iso-intense signal (Fig. 1B). Computed tomography angiography revealed severe stenosis. However, calcification was not observed. Carotid ultrasonography revealed a heterogeneous plaque with mixed low- and high-echoic components. No significant plaque mobility was observed. Before the initial treatment, resting iodine-123 N-isopropyl-p-iodoamphetamine single-photon emission computed tomography (IMP-SPECT) revealed cerebral blood flow in the middle cerebral artery territory as follows: 36 ml/min/100 g each on the right and the left sides. After acetazolamide administration, the corresponding values increased to 54 ml/min/100 g on the right and 60 ml/min/100 g on the left, indicating preserved resting blood flow and vascular reactivity. Before surgery, the patient received aspirin at a dose of 100 mg/day and clopidogrel at a dose of 75 mg/day for 14 days.

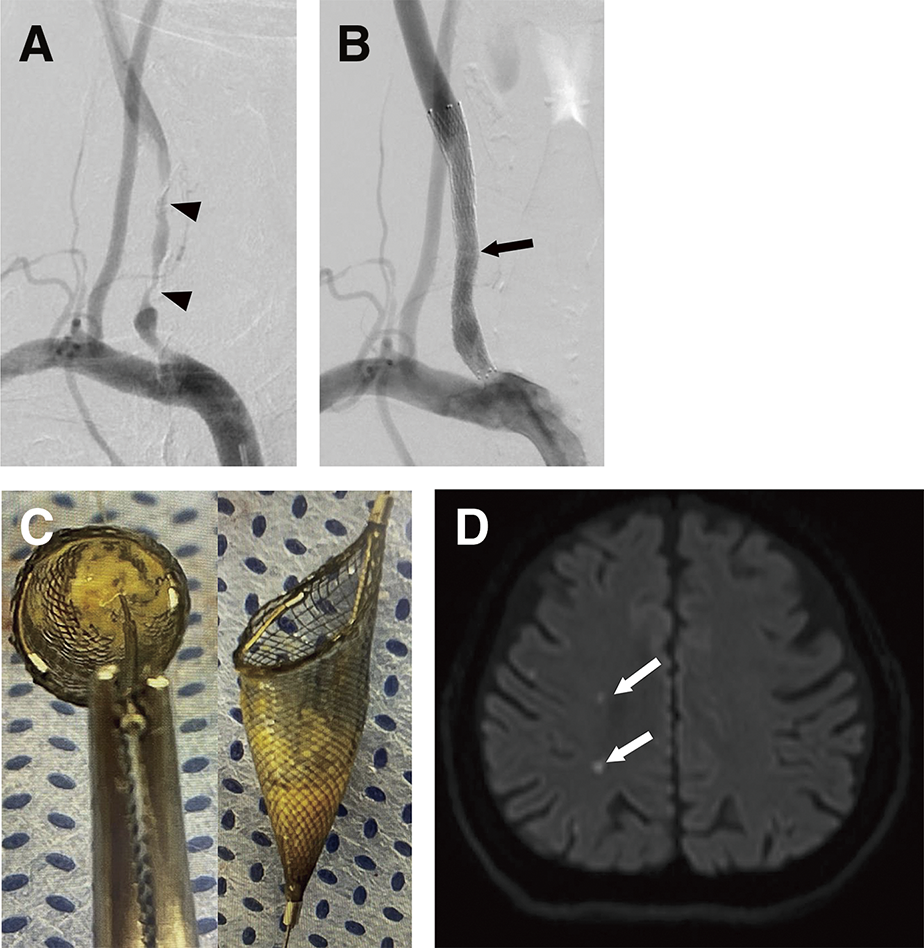
The endovascular procedure was performed under local anesthesia. The patient’s activated clotting time was maintained at >300s. An 8-F balloon guiding catheter was inserted into the innominate artery via the transfemoral access. The 5.0-mm SpiderFX (Covidien, Mansfield, MA, USA) was placed into the right internal carotid artery for cerebral embolic protection. Pre-dilation was performed with 5.0 × 30-mm Sterling balloon catheters (Boston Scientific, Marlborough, MA, USA) at 6 atm. The 8 × 60-mm Protégé RX stent (Medtronic, Minneapolis, MN, USA) was deployed at the lesion (Fig. 2A and 2B). After the stent placement procedure, a large amount of debris was found in the filter (Fig. 2C). The patient presented with left upper limb paralysis immediately after the procedure. Diffusion-weighted imaging (DWI)-MRI revealed multiple hyperintense spots in the right cerebral hemisphere, which caused the patient’s symptoms (Fig. 2D). Her symptoms improved within an hour, and the patient was discharged within 7 days. Post-treatment IMP-SPECT demonstrated no evidence of hyperperfusion phenomenon.
Restenosis of the right CCA was observed 6 months after the intervention. Ultrasonography showed an increased blood flow velocity at 390 cm/s at the origin of the right CCA. MRA revealed a decreased blood flow in the right CCA distal to the stent site. These findings worsened over time, and the patient was scheduled to undergo endovascular retreatment 9 months after the first therapy. During the initial treatment, a large amount of plaque was captured in the filter, indicating that the plaque was unstable. Based on this finding, flow reversal was selected as the embolic protection strategy during the retreatment.
Preoperatively, aspirin at a dose of 100 mg/day and clopidogrel at a dose of 75 mg/day were administered for 14 days. Under local anesthesia, a 9-F sheath was placed in the right femoral artery. The 9-F Branchor balloon guiding catheter (Asahi Intecc, Aichi, Japan) was guided to the innominate artery. Angiogram of the innominate artery showed severe stenosis at the proximal end of the stent (Fig. 3A). The 8-F Optimo balloon guiding catheter (Tokai Medical Products, Aichi, Japan) was directly punctured into the right brachial artery and inserted into the right subclavian artery at the bifurcation of the vertebral artery. Preoperatively, MRA (Fig. 1A) demonstrated well-developed contralateral vertebral artery flow, indicating that adequate blood flow to the brainstem would be maintained through the contralateral vertebral artery during the procedure. Aspiration was conducted using the 8-F Optimo balloon guiding catheter in the right subclavian artery. In addition, to return the blood collected with the debris from the stenotic lesion during angioplasty, a 4-F sheath was inserted into the right femoral vein. Under dual-balloon inflation, flow reversal in the right CCA was established by connecting the 8-F Optimo balloon guiding catheter in the right subclavian artery to the 4-F sheath in the right femoral vein via a transfusion filter (Optimo chamber; Tokai Medical Products). Then, pre-dilation with the 6.0 × 20-mm Sterling balloon guiding catheter was performed on the ASAHI CHIKAI 14 guidewire, (Asahi Intecc) which served as the primary axis for lesion crossing and treatment (Fig. 3B). After adequate vessel dilatation was confirmed (Fig. 3C), the PRECISE stent (9.0 × 30 mm; CardinalHealth, Cordis, Santa Clara, CA, USA) was deployed at the site of stenosis (Fig. 3D). Intraoperative ultrasonography confirmed the presence of flow reversal under aspiration via both balloon catheters (Fig. 3E and 3F). After post-dilation with the 6.0 × 20-mm Sterling balloon dilatation catheter, debris was detected in the blood that was aspirated via the 8-F Optimo balloon guiding catheter (Fig. 3G). Hemostasis was achieved by manual compression at all access sites, including the femoral artery, brachial artery, and femoral vein. No complications were observed at the puncture sites. Post-treatment IMP-SPECT demonstrated no evidence of hyperperfusion phenomenon. There were no areas of hyperintensity in the brain on postoperative DWI-MRI. The patient was discharged without neurological deficits.

The treatment of stenosis originating from the right CCA has significant challenges primarily due to difficulties in achieving catheter stability and preventing cerebral embolism during the procedure.1) Abe et al.5) reported a flow reversal technique, referred to as the counterflow technique, that uses an 8-F Optimo balloon guiding catheter (Tokai Medical Products) and a 2.6-F microballoon catheter inflated in the innominate artery and the right VA, respectively. However, this method potentially allows antegrade blood flow from the right thyrocervical trunk or the right internal mammary artery to the right CCA. Hence, there is a risk of procedure-related cerebral embolism (Fig. 4A).

The novel technique offers enhanced embolic protection while improving catheter support. By occluding the innominate artery by inflating the 9-F Branchor balloon guiding catheter (Asahi Intecc), superior catheter stability was achieved. Concurrently, the 8-F Optimo balloon guiding catheter was inflated in the right subclavian artery at the vertebral artery bifurcation. This dual-balloon approach combined with blood aspiration via the 8-F Optimo balloon catheter in the right subclavian artery at the vertebral artery bifurcation effectively flushed out procedure-related debris from the right CCA. The implementation of this 2-balloon inflation strategy with blood aspiration established a reliable retrograde flow reversal, thereby eliminating antegrade blood flow from the right thyrocervical trunk or the right internal mammary artery (Fig. 4B).
Notably, the retrograde flow in the right CCA was validated using intraoperative ultrasonography, which contributed significantly to procedural safety. Posttreatment MRI did not reveal any embolic complications, thereby further supporting the efficacy of our flow reversal technique under dual-balloon inflation. In cases of hypoplasia of the left vertebral artery, retrograde blood flow from the left vertebral artery to the right vertebral artery may be insufficient when the innominate artery is occluded, resulting in antegrade flow in the right vertebral artery maintained by collateral circulation through the external carotid artery. Flow reversal in the right CCA might still be achieved with innominate artery occlusion combined with intermittent aspiration or continuous blood removal into a vein. To confirm the need for additional right subclavian artery occlusion, it is advisable first to occlude the innominate artery and evaluate the right CCA flow direction using ultrasonography. Moreover, in patients with left vertebral artery hypoplasia, right subclavian or innominate artery occlusion may risk brainstem ischemia. If necessary, the occlusion should be as brief as possible to minimize this risk.
The current method is potentially effective. Nevertheless, its application may be limited in patients with poor cerebral ischemia tolerance due to the temporary blood flow interruption required by the procedure. The concomitant use of filter protection in the internal carotid artery is one possible solution for patients with limited cerebral ischemia tolerance. Despite the complexity of this technique, it offers flexibility to transition to filter protection in the event of ischemic symptoms arising from balloon-induced flow interruption. Consequently, meticulous patient selection is required prior to implementing this procedure. In cases where inadequate collateral blood flow to the right internal carotid artery is anticipated, it is essential to consider and prepare for the concurrent use of filter protection. This preparatory approach allows for a more comprehensive risk mitigation strategy, thereby potentially expanding the applicability of the technique to a broader patient population.
The novel flow reversal technique utilizing dual-balloon inflation is effective and safe for treating right CCA stenosis. This approach can enhance catheter stability and reduce the risk of cerebral embolism. Nevertheless, further investigation should be performed to completely establish the clinical utility of this technique.
The authors declare that they have no conflicts of interest.