2025 Volume 19 Issue 1 Article ID: oa.2024-0090
2025 Volume 19 Issue 1 Article ID: oa.2024-0090
Objective: Computed tomography (CT) and magnetic resonance imaging of cerebral perfusion are useful in determining the indication of mechanical thrombectomy (MT) for acute ischemic stroke. RAPID (iSchemaView, Menlo Park, CA, USA) is the most common software for analyzing brain perfusion images worldwide, but various other software are also available. The optimal threshold value for each software is different, and each has its characteristics. This study investigated the relationship between the quantitative evaluation of ischemic core volume (ICV) and the Alberta Stroke Program Early CT Score (ASPECTS) using CT Perfusion 4D (GE Healthcare Inc., Milwaukee, WI, USA), a software used in our hospital.
Methods: Among patients who underwent MT between April 2015 and February 2023, those with modified Rankin Scale: 0–2, obstruction by embolic mechanism, and thrombolysis in cerebral infarction: 2b or higher were selected retrospectively. Patients with middle cerebral artery M1 segment (M1) and internal carotid artery (ICA) occlusions (90 and 46 patients) were included. We quantitatively analyzed ICV at relative cerebral blood flow (rCBF) <20% and cerebral blood volume (CBV) <1 mL/100 g and evaluated the relationship with ASPECTS scores in 3 groups: M1 + ICA, M1, and ICA occlusion groups.
Results: The median ICV was rCBF <20%: 44.7 cm3 and CBV <1 mL/100 g: 34.6 cm3, and there was no statistically significant difference between the 2 groups (p = 0.23). There was a negative correlation between ICV and ASPECTS scores in each occlusion group in all groups.
Conclusion: The quantitative evaluation of ICV at rCBF <20% and CBV <1 mL/100 g was negatively correlated with the ASPECTS score in GE’s CT Perfusion imaging analysis software.
For acute ischemic stroke (AIS), it is important to estimate the extent of ischemia in large vessel occlusion (LVO) using diagnostic imaging.1) For ischemic core and penumbra assessment, the Alberta Stroke Program Early Computed Tomography (CT) Score (ASPECTS), which is used as an early marker of ischemic changes in non-contrast CT (NCCT),2) CT Perfusion (CTP), and diffusion-weighted image (DWI) are used as diagnostic imaging. In 2018, the DAWN3) and DEFUSE 3 trials4) were conducted to demonstrate the efficacy of mechanical thrombectomy (MT) in case selection based on ischemic core volume (ICV) and perfusion abnormality assessment in cerebral infarction due to LVO with onset >6 hours. In the DAWN and DEFUSE 3 studies, RAPID (iSchemaView, Menlo Park, CA, USA) was used to analyze CTP or DWI perfusion images. Although RAPID is one of the most useful software tools for brain perfusion image analysis, it has not yet been widely used in Japan. There are various other types of software for brain perfusion image analysis, such as Vitrea (Canon, Tochigi, Japan) and PMAneo (Micron, Tokyo, Japan). While some use the same analysis parameters as RAPID, others have different analysis algorithms.5) Therefore, it is important to understand the optimal threshold values and characteristics of the software used at your facility. In our hospital, CTP is used for image evaluation of AIS, and CT Perfusion 4D (GE Healthcare Inc., Milwaukee, WI, USA) is used as the software for cerebral perfusion image analysis. Previous studies using CT Perfusion 4D have been reported by Christipher et al. and Liu et al. Christopher et al. reported that the optimal ischemic core parameters are relative cerebral blood flow (rCBF) <20% for patients within 90 minutes from CTP to reperfusion.6) In a comparison study with RAPID, Liu et al. reported that the ICV estimation of ischemic core parameters with cerebral blood volume (CBV) <1 mL/100 g showed excellent agreement with that of RAPID.7) However, these previous studies have not reported the relationship between the ASPECTS score assessed by NCCT before MT and ICV using CT Perfusion 4D. In this study, we performed a retrospective analysis of patients who underwent MT at our hospital and compared the ICV at rCBF <20% and CBV <1 mL/100 g with the ASPECTS.
Of 505 consecutive cases of MT performed for LVO at our hospital between April 2015 and February 2023, modified Rankin Scale:8) 0–2, occlusion by embolic mechanism, thrombolysis in cerebral infarction: 90 patients with middle cerebral artery M1 segment (M1) and 46 patients with internal carotid artery (ICA) occlusions with 2b or higher score were selected retrospectively. The details of patient selection are shown in Fig. 1 as a flowchart. ASPECTS was determined after at least 2 neurosurgeons or neurologists evaluated them and reached a consensus, using NCCT before MT. ICV at rCBF <20% and CBV <1 mL/100 g was analyzed with CT Perfusion 4D (GE Healthcare Inc.) using GE Healthcare’s Advantage Workstation (Version 4.7) as the imaging system. In the image processing, the healthy ICA was selected as the input function for all arteries. However, since this is a retrospective study, ICV in each ischemic core parameter was not performed before MT in actual clinical practice. For the statistical analysis between the 2 groups, a t-test (test of means by paired samples) was used. Next, the correlation coefficients between ICV and ASPECTS scores were determined by dividing the patients into M1 + ICA, M1, and ICA occlusion groups. In this study, the outliers (values deviating from the regression line of ICV and ASPECTS by more than 2σ) are included. The relationship between ICV and ASPECTS scores for rCBF <20% and CBV <1 mL/100 g was compared with that of ICV in DWI-ASPECTS, which is shown in the Guidelines for the proper use of percutaneous vascular cerebral thrombus recovery devices, 5th edition.1) DWI-ASPECTS is reported that 0.5 to 0.9 points lower than CT-ASPECTS in the same patients9–11). Therefore, the criterion for the relationship between CT-ASPECTS and ICV in this study is set as DWI-ASPECTS + 0.9. The values of ICV versus DWI-ASPECTS indicated as theoretical values in this study are shown in Table 1. The causes of the outliers were examined. Spearman’s rank correlation coefficient test was used for statistical analysis. EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) was used as the statistical analysis software in this study. The research within our submission has been approved by the ethics institutional review board of Japanese Red Cross Ise Hospital (ER2024-36).

| DWI-ASPECTS | 10 | 7 | 6 | 5 | 3 |
| ICV | 0 | 25 | 50 | 70 | 100 |
ASPECTS, Alberta Stroke Program Early Computed Tomography Score; ICV, ischemic core volume; DWI, diffusion-weighted image
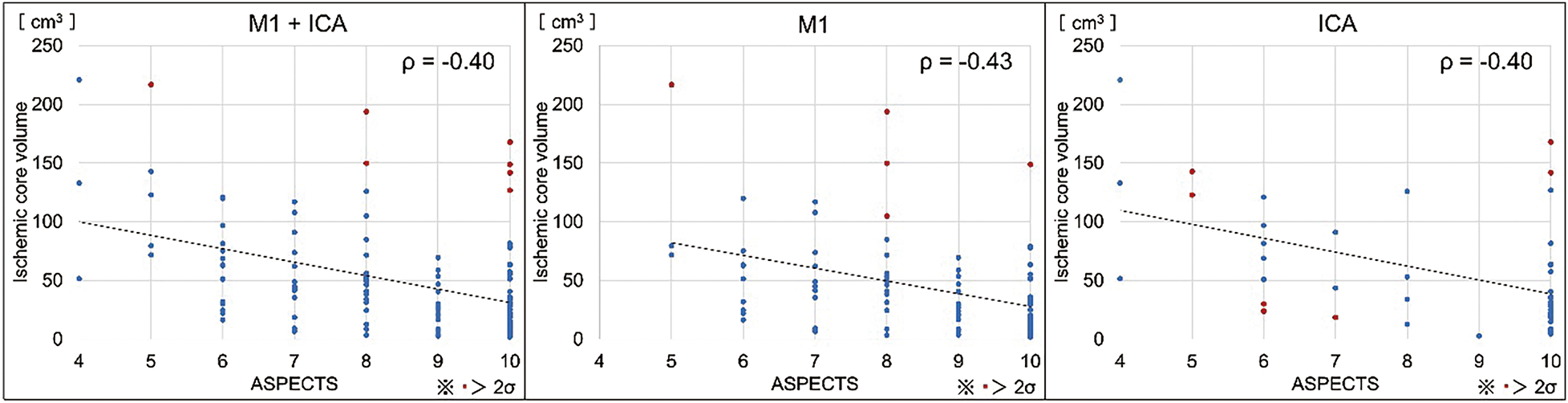
The number of cases per ASPECTS score is shown in Table 2. The median ICV for each parameter was 44.7 cm3 (interquartile range [IQR]: 26.5–61.0) for rCBF <20% and 34.6 cm3 (IQR: 18.9–58.9) for CBV <1 mL/100 g, with no statistically significant difference between the 2 groups (p = 0.23) (Fig. 2). Next, the relationship between ICV and ASPECTS scores for rCBF <20% was ρ = –0.40 (p <0.001) for the M1 + ICA occlusion group, ρ = –0.44 (p <0.001) for the M1 occlusion group, and ρ = –0.40 (p <0.001) for the ICA occlusion group, showing a negative correlation among all groups (Fig. 3). Of these, 7, 5, and 10 cases in the M1 + ICA, M1, and ICA occlusion groups were outliers. The relationship between ICV and ASPECTS scores for CBV <1 mL/100 g was also negative in all groups: ρ = –0.40 (p <0.001), ρ = –0.43 (p <0.001) and ρ = –0.40 (p <0.001) in the M1 + ICA, M1, and ICA occlusion groups, respectively (Fig. 4). Of these, 7, 5, and 7 cases in the M1 + ICA, M1, and ICA occlusion groups were outliers. The regression lines of ICV and ASPECTS for rCBF <20% and CBV <1 mL/100 g are compared with the regression lines of DWI-ASPECTS and ICV shown in the theoretical values, and the results are shown in Fig. 5. An analysis of covariance (ANCOVA) was performed on these results. The results of the statistical analysis showed that parallelism was maintained in the regression lines of all the groups. Therefore, as can be seen in Fig. 5, the relationship between CT-ASPECTS and ICV for each group is higher than that between DWI-ASPECTS and ICV, which is shown as a theoretical value.
| ASPECTS | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|
| M1 + ICA | 3 | 5 | 16 | 12 | 21 | 18 | 61 |
| M1 | 0 | 3 | 9 | 9 | 17 | 17 | 35 |
| ICA | 3 | 2 | 7 | 3 | 4 | 1 | 26 |
ASPECTS, Alberta Stroke Program Early Computed Tomography Score; ICA, internal carotid artery; M1, middle cerebral artery M1 segment



Based on the reports on CT Perfusion 4D (GE Healthcare Inc.) by Christopher and Liu et al.6,7), we set the ischemia core parameters in this study as rCBF <20% and CBV <1 mL/100 g and compared them with the ASPECTS score. The results showed that the quantitative ICV values of rCBF <20% and CBV <1 mL/100 g were negatively correlated with the ASPECTS score in the CT Perfusion 4D, GE Healthcare’s CTP image analysis software. In addition, ICV in each ASPECTS was higher than in the relationship between DWI-ASPECTS and ICV shown in the Guidelines for the proper use of percutaneous vascular cerebral thrombus recovery devices, 5th edition.1) Demeestere et al.2) reported no significant difference in the identification accuracy of ischemic core region estimation between ASPECTS and CTP for cases of extensive irreversible cerebral infarction. On the other hand, some cases with normal or near-normal NCCT in the ASPECTS evaluation (ASPECTS: 8–10) may be misclassified as small ischemic core lesions, although some of them may already have extensive irreversible cerebral infarction. It has been suggested that ischemic core estimation by CTP may be more reliable and accurate than ASPECTS because of its lower false positive and false negative rates. Furthermore, since ASPECTS is based on manual visual scoring, different observers are expected to give different scores. Additionally, the relationship of ICV in DWI-ASPECTS, as shown in the Guidelines for the proper use of percutaneous vascular cerebral thrombus recovery devices, 5th edition1), is based on a theoretical value. The high value of the relationship between ICV and ASPECTS score in the present results may be due to the fact that, as reported by Demeestere et al.2), there were cases with high ASPECTS scores in the actual clinical results, even though a certain ICV was estimated by CTP. Another factor may be that the present study included a certain number of outliers due to the relatively small number of cases in this study. In fact, about 70% of the outliers with rCBF <20% were cases of ICA occlusion. This may be because the imaging analysis of rCBF is based on the evaluation of relative values to the healthy side. Additionally, ICA occlusion may cause ischemia over a wide area, resulting in a large decrease in cerebral blood flow on the affected side compared to the healthy side. Furthermore, some outlier cases with CBV <1 mL/100 g showed poor imaging analysis. When a series of low perfusion areas are observed from the affected side to the healthy side, these cases should be evaluated with caution because inappropriate ischemic cores may also be observed on the healthy side. Figure 6 shows the cases in which the image analysis was performed properly and the cases in which the image analysis was not performed properly. In addition, there were cases of motion artifacts and poor circulation as patient-dependent effects. Considering the possibility that ICV may be overestimated in these cases is necessary. Therefore, it is considered that the judgment of the indication of MT will be more accurate if each qualitative image is evaluated mutually with the quantitative results. In CT Perfusion 4D, the quantitative evaluation of ischemic core at rCBF <20% and CBV <1 mL/100 g was suggested to have a negative correlation with the ASPECTS score, but in some clinical cases, values that do not correlate with the ASPECTS score are calculated. Therefore, it is important to correctly understand the characteristics of the software used in your institution for cerebral perfusion imaging analysis.

The quantitative evaluation of ICV at rCBF <20% and CBV <1 mL/100 g was negatively correlated with the ASPECTS score in CT Perfusion imaging analysis software of GE Healthcare Inc.
The authors thank Crimson Interactive Pvt. Ltd. (Ulatus) – www.ulatus.jp for their assistance in manuscript translation and editing.
The authors declare that there are no conflicts of interest related to this work.