2014 Volume 2 Issue 1 Pages 21-25
2014 Volume 2 Issue 1 Pages 21-25
Aim: Various methods to reduce postpartum hemorrhage due to placenta previa have been suggested. The aim of this study is to evaluate the usefulness of vertical compression sutures (VCS) for controlling bleeding in patients with a placenta previa.
Methods: We analyzed 115 patents with placenta previa and compared 38 patients before the introduction of VCS and 77 patients after its introduction. The 77 patients were divided into 2 groups, 63 women in whom VCS were not used (Non-VCS Group) and 14 women who received VCS (VCS Group); the groups were compared.
Results: The average blood loss during surgery was 1,910±1,536 ml before the introduction of VCS and 1,530±699.0 ml after its introduction. The rate of patients with hemorrhage > 2,000 ml was 37% (14/38) before VCS were introduced and 19% (15/77) after their introduction (P<0.05). VCS were used in 14 cases and were effective in all cases. The average intraoperative blood loss was 1,443±655.8 ml in the Non-VCS group and 1,919±778.1 ml in the VCS Group (P<0.05). The rate of patients with hemorrhage > 2,000 ml was 13% (8/63) in the Non-VCS group and 50% (7/14) in the VCS Group (P<0.05).
Conclusions: VCS is effective for controlling bleeding with a placenta previa.
After placental removal, massive hemorrhage commonly occurs in women with a placenta previa. Moreover, many of these women develop disseminated intravascular coagulation (DIC) shortly after this massive hemorrhage, which makes hemostasis even more difficult. Various methods to reduce this massive hemorrhage have been suggested, such as intrauterine gauze packing,1) interrupted sutures,1) stepwise uterine vessel ligation,2) internal iliac artery ligation,3) original or modified B-Lynch sutures,4,5) transcatheter arterial embolization (TAE),6) use of Bakri balloon tamponade,7,8) and hysterectomy.9) In 2005, Hwu et al.10) reported their use of vertical compression sutures (VCS) as a method of controlling hemorrhage from the separated surface of the lower uterine segment in cases of placenta previa or placenta accreta. The advantages of VCS are that the time required for suturing is extremely short and the procedure itself is simple. Before August 2007, we used intrauterine gauze packing, internal iliac artery ligation or hysterectomy if hemostasis could not be achieved by the usual methods, such as the administration of oxytocic drugs, bimanual compression of the lower uterine segment, or direct sutures applied to the separated surface. As we consider VCS to be a first-line treatment for bleeding when the usual methods are not effective, we have been using the original or modified hemostatic technique for placenta previa to control bleeding from the separated surface since September 2007.
In this study, we evaluated the effectiveness of VCS to control massive bleeding due to placenta previa.
It is a retrospective study based on hospital records. The study group comprised patients treated in our hospital for placenta previa from January 2001 through December 2012. Patients in whom placenta accreta had been highly suspected prior to surgery were excluded. In this period, there are 115 patients with placenta previa. We tried to control bleeding by methods other than hysterectomy in all case because we avoid surgical complications due to emergency hysterectomy. 38 patients were treated before the introduction of VCS and 77 patients were treated after its introduction. Among the latter group, VCS were employed in 14 cases. The investigated parameters were clinical characteristics of the patients (maternal age, parity, weeks of gestation, newborn weight, and primary placental location), intraoperative blood loss and the rate of patients with intraoperative blood loss > 2,000 ml, and the rate who required a hysterectomy. 77 patients after VCS were introduced were divided into 63 in whom VCS were not used and 14 who received VCS. These 2 groups were compared about intraoperative blood loss and the rate of patients with intraoperative blood loss > 2,000 ml.
The time required for VCS a few minutes. The surgical procedure for VCS is described below. (1) Cesarean section (CS) with a median incision was performed in the usual manner. The bladder was reflected downward to adequately expose the underlying lower uterine segment before making the uterine incision. (2) After placental removal, in cases in which bleeding is not controlled via suturing or if areas of hemorrhage cannot be identified because of active bleeding from the entire separated surface, we apply VCS to the lower segment. USP No. 0 Vicryl Rapide with a 1/2 Circle 40-mm taper point needle (Ethicon, Inc., Somerville, NJ, USA) was used to place a suture through the anterior wall of the lower uterine segment, according to a previously described method.10) With our method,11) the suture was placed through both the anterior and posterior wall (Figure 1), taking care to avoid the rectum. When we tried to perform original method, but it’s difficult to find the needle through the anterior wall of lower uterine segment because of massive bleeding from the entire separated surface. We think our method, penetrating both the anterior and posterior wall at one time, is easier to perform and more reliable than the original method. In case of adhesions to the posterior wall and the rectum, we perform original method. (3) After placing the sutures, the knots were cinched up as tightly as possible to compress the lower uterine segment by approximating the anterior and posterior walls. (4) The lower transverse uterine incision was then closed in two layers with USP No. 0 Vicryl Plus (Ethicon, Inc.) sutures and observed for hemostasis. (5) Before abdominal closure, the vagina was swabbed; this confirms that any continued blood loss is minimal.
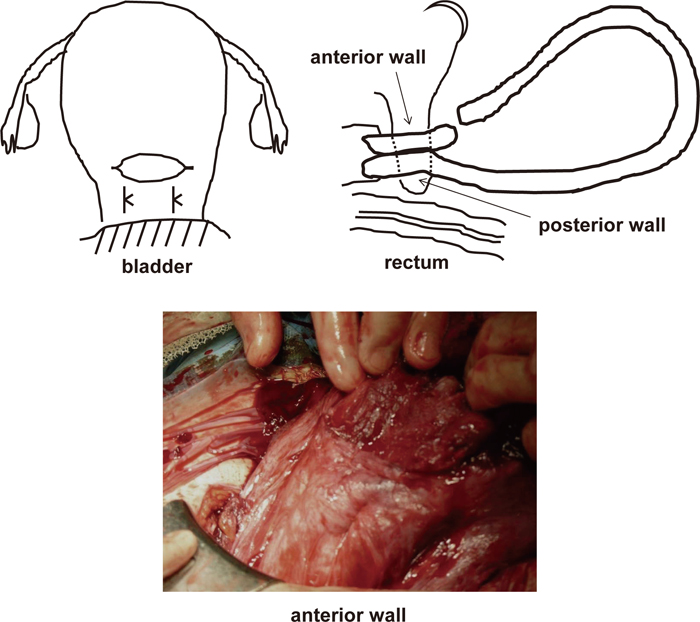
Vertical compression sutures in the lower segment.
With our method, vertical compression sutures was placed through both the anterior and posterior wall, taking care to avoid the rectum.
Student’s T-test, Chi-square test or Fisher’s exact test were used for statistical tests: a P value>0.05 was considered to indicate a statistically significant difference.
There were significant difference in maternal age and new born weight in the clinical characteristics of patients before and after VCS introduction. On the other hand, there was no significant difference in placental location. (Table 1).
| Before VCS introduction (n=38) | After VCS introduction (n=77) | P-value | ||
|---|---|---|---|---|
| Maternal age | 33.4±4.28 | 35.4±4.09 | <0.05 | |
| Parity | 0.61±0.92 | 0.43±0.59 | 0.11 | |
| Weeks of gestation | 35.6±2.70 | 36.1±4.77 | 0.29 | |
| Newborn weight (g) | 2,428±605.4 | 2,610±489.3 | <0.05 | |
| Primary placental location | Anterior | 14 | 23 | 0.45 |
| Posterior | 24 | 54 |
VCS, vertical compression sutures.
As shown in Table 2, the average intraoperative blood loss (±SD) was 1,910±1,536 ml before VCS were introduced and 1,530±699.0 ml after their introduction; thus, intraoperative blood loss tended to be smaller after the introduction of VCS. The rate of patients with hemorrhage > 2,000 ml was 37% (14/38) before VCS were introduced and 19% (15/77) after their introduction; the rate of patients with hemorrhage > 2,000 ml decreased after the introduction of VCS (P<0.05). The rate of patients who required a hysterectomy was 5% (2/38) before VCS were introduced and 0% (0/77) after their introduction; no patient required a hysterectomy after their introduction.
| Before VCS introduction (n=38) | After VCS introduction (n=77) | P-value | |
|---|---|---|---|
| Blood loss during surgery (ml) | 1,910±1,536 | 1,530±699.0 | 0.07 |
| Blood loss during surgery > 2,000 ml | 37% (14/38) | 19% (15/77) | <0.05 |
| Hysterectomy | 5% (2/38) | 0% (0/77) | 0.11 |
VCS, vertical compression sutures.
The 77 patients treated after the introduction of VCS were then divided into 63 for whom VCS were not used (Non-Vertical Compression Sutures Group; Non-VCS Group) and 14 who underwent this procedure (Vertical Compression Sutures Group; VCS Group); the two groups were compared. The volume of blood loss during surgery was 1,443±655.8 ml in the Non-VCS Group and 1,919±778.1 ml in the VCS group (P<0.05). The rate of patients with hemorrhage > 2,000 ml was 13% (8/63) in Non-VCS Group and 50% (7/14) in VCS Group; this rate was significantly less than that of the Non-VCS Group (P<0.05). VCS were able to stop the bleeding immediately in 14/14 (100%) of the patients. None of the 14 patients who received VCS developed complications such as impaired lochia discharge, postoperative uterine infection, or uterine necrosis. No abnormalities were observed during puerperium and normal menstrual pattern returned in all patients. Ultrasonography at the end of puerperium showed no abnormalities.
The incidences of placenta previa are increasing primarily due to the high CS rate12,13) and the rising number of assisted reproductive technology procedures.14,15) Bleeding due to placenta previa often rapidly develops into severe hemorrhage and on patients in whom hemorrhage exceeds 2,000 ml DIC often subsequently occurs. High levels of fibrin/fibrinogen degradation products in DIC may cause uterine atony, promote additional obstetric hemorrhage, and significantly impair the establishment of hemostasis.
The following points address the mechanism of bleeding from the separated surface of a placenta previa. Normally, after the placenta is removed, bleeding ceases via natural hemostasis secondary to myometrial contraction. In placenta previa, however, the placenta is abnormally located on the lower uterine segment, which is substantially thinner than the corporeal wall and does not contract as readily as the uterine corpus.16) Furthermore, the reduced thickness of the decidual layer of the lower uterine segment may allow trophoblast penetration of the uterine wall, causing difficulties with placenta removal (placenta accreta), thus further increasing the amount of bleeding.17) Because the separated surface of the lower uterine segment is supplied not only by the internal iliac artery but also by the external iliac artery system, via the adjacent bladder and the paracolpium, it receives an abundant blood supply; thus, hemostasis is difficult, with neither uterine artery ligation nor internal iliac artery ligation achieving high success rates. Moreover, uterine artery ligation does not appear to compromise subsequent fertility and obstetric outcome.18) We are of the opinion that the most important factor in surgery for placenta previa is to achieve effective hemostasis in the bleeding area as quickly as possible. Because VCS only involve the passage of a needle from the anterior wall through the posterior wall and suturing, it can be performed far more quickly than arterial ligation; furthermore, in the present study, it was found that it has an extremely high success rate in stopping bleeding. We believe that the mechanism of hemostasis by VCS is not only due to the direct compression of the anterior and posterior uterine walls but also may be due to reduced uterine blood flow from the lateral edge of the lower uterine segment to its medial part; this flow originates from the uterine artery and cervical-vaginal branch of the uterine artery and may also be another important source of bleeding. In cases in which this technique is unsuccessful, stepwise devascularization, TAE, or total hysterectomy is then performed. Even if complete hemostasis is not achieved, performing VCS reduces the degree of hemorrhage, thus gaining time to perform other procedures. As has recently been reported, combining these hemostatic techniques may further improve their effectiveness in stopping hemorrhage.19,20)
In the present study, the introduction of VCS reduced intraoperative blood loss and the rate of patients suffering massive hemorrhage > 2,000 ml; VCS were performed in 14 cases and were effective in 14 cases (100%), suggesting that VCS may be a highly effective hemostatic procedure. The volume of hemorrhage exceeded 2,000 ml in 50% of patients who underwent VCS. This shows that uncontrolled hemorrhage can easily exceed 2,000 ml in a short time in many cases, and in such patients, it is important to use VCS to promptly stop the bleeding. Before the introduction of VCS, more time was required to achieve hemostasis in such patients, meaning that they lost larger amounts of blood.
There have been only a few reported complications of VCS; however, uterine necrosis, uterine infection, uterine deformity, and intrauterine adhesions due to compression sutures have been reported.21) To minimize the potential for these complications, we use Vicryl Rapide and leave the compression sutures in place for as short a time as possible. A large study is required to evaluate complications and subsequent pregnancies.
The employment of VCS is an extremely effective hemostatic procedure for hemorrhage due to placenta previa. We now believe that VCS should be performed without delay in patients in whom hemorrhage exceeds 2,000 ml and hemostasis has been unsuccessful. This method is also a comparatively simple technique that can be performed rapidly, and it is applicable for use by non-specialists as well.
None.