2014 Volume 2 Issue 1 Pages 33-35
2014 Volume 2 Issue 1 Pages 33-35
We report a case of patients with placental abruption which certified fetomaternal hemorrhage (FMH) after traffic injury. A 21-year-old multipara was admitted to private clinic after traffic accident on 29th week gestation. Cardiotocogram (CTG) showed sinusoidal-like pattern with tachycardia and she was transferred to our hospital. Her injury was also not severe, but due to abnormal CTG suggesting massive FMH, immediate cesarean section was performed. The infant was saved with the umbilical cord artery blood pH=7.243, and a maternal good postoperative course was observed. FMH was proved by maternal serum concentrations of hemoglobin F and alpha fetoprotein.
Maternal trauma including traffic accident is a well-known cause of the placental abruption.1) Placental abruption is not only a major cause of fetal death and cerebral palsy worldwide, but also lead to massive hemorrhage and severe disseminated intravascular coagulation syndrome on mother, maybe due to uncontrollable coagulation and fetomaternal hemorrhage (FMH, also known as feto-maternal transfusion syndrome).2) The reason of the disease is not simple, including uterine contraction, pregnancy induced hypertension, placentation failure or uterine malformation.
Here, we report the case of patient with placental abruption that developed after a traffic injury. It was able to save fetus after accurate decision by cardiotocogram (CTG) pattern, which showed sinusoidal-like pattern suggesting fetal acute anemia. As was expected, we could define FMH with maternal blood sample later.
Our patient was a 21-year-old multipara, whose previous pregnancy was uneventful and delivered normally. At the 29th week of gestation during the current pregnancy, she collided with a wall when she drove her car without seatbelt. Whether she struck her abdomen with steering wheel or not is unknown. She transferred to the private clinic. Maternal vital condition was stable and the consciousness was clear. On CTG, uterine contraction was unclear, but tachycardia of the fetus (180 b.p.m.) and sinusoidal-like pattern with loss of variability was defined (Figure 1). She was transferred to our hospital after suspect of maternal injury, threatened premature labor, placental dysfunction, and the possibility of fetal anemia with some unknown reason.
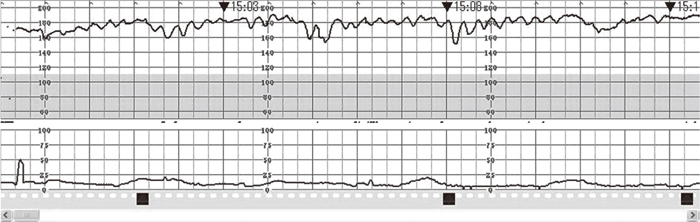
Cardiotocogram of the case in former private clinic. Within 1 hour after traffic accident.
On admission (1.5 hours after traffic accident), her consciousness was clear, her blood pressure was 102/63 mmHg with 100 b.p.m.. Pain on pressure was found on her right ilial crest, and subcutaneous bleeding was found on right thigh, but no other injury include lower was found. No vaginal bleeding or uterine cervical dilation was defined. No retroplacental hematoma was found on ultrasound. Continuous CTG examination was performed since admission, and on 2 hours 50 minutes after the traffic accident, the CTG showed fetal tachycardia to 195 b.p.m. with decreased variability, the weak uterine contraction every 10 minutes with mild late deceleration to 180 b.p.m. which recovered immediately. A decision to perform an emergency cesarean section was made immediately. After quick computed tomography examination to exclude maternal bone fracture and liver or vascular injury, a male infant weighing 1,240 g was delivered through a low transverse uterine incision under general anesthesia on 3 hours 50 minutes after the traffic accident; his Apgar score was 1 at 1 minute and 6 at 5 minutes with the umbilical cord artery blood pH=7.243. The baby was resuscitated by the neonatologists and transferred to NICU. The placenta contained 50% of retroplacental hematoma but her uterus did not showed Couvelaire symptom. A total of 700 g of blood was lost until the operation. After the operation, her blood hemoglobin concentration was 10.5 g/dl; platelet count, 18.7×104/μl; bioactivity of antithrombin III, 77%; and fibrinogen concentration, 298 mg/dl. Existence of hemoglobin F (HbF) (2.2%) and alpha fetoprotein (AFP; 7183 ng/ml) revealed FMH. Since there was no other pathological finding than retroplacental placenta, the FMH was regarded as a result of placental abruption. She discharged from hospital on the sixth postoperative day without receiving blood transfusion. The postpartum course was uneventful. The newborn’s cord blood also showed anemia of hemoglobin concentration 10.5 g/dl and hematocrit (Ht) 38.6%. He has some minor problem due to premature birth at 29th week of gestation, but vitally stable until 3 months of age.
FMH is the condition that also be shown in normal pregnant course,3) but the normal amount of fetal blood flow into maternal circulation is small.3) Maternal trauma, placental abruption or umbilical cord anomaly are the major cause of massive FMH.2) In our recent case, the massive FMH was occurred after placental abruption due to maternal trauma, which suspected by abnormal CTG pattern (sinusoidal-like pattern and fetal tachycardia) and proved by HbF and AFP in maternal circulation.
Traditionally, FMH have been tested by Kleihauer – Betke test and performed on maternal trauma patients, but the positive predictive value of the FMH is relatively low.4) Recently, HbF5) or AFP3) in maternal circulation, or increase of fetal middle cerebral artery peak systolic velocity (MCA-PSV) by ultrasound diagnosis6) are proposed as a marker for FMH. In our recent case, however, the most useful marker in the course was the abnormal CTG pattern, especially the sinusoidal rhythm, diagnosed by the first obstetrician in the private clinic, though it showed tachycardia and late deceleration that exclude this case from a typical “sinusoidal pattern”.7) Clear association of the sinusoidal pattern of the CTG and fetal anemia has been reported.8)
There is no accurate method to measure the amount of the fetal blood transfused to maternal circulation. One method to estimate the amount of fetal blood is to use the HbF rate. The amount of the fetal blood circulated in mother is estimated as ([maternal circulating blood volume]×[maternal Ht/neonatal Ht]×HbF ratio). In our case, the estimated amount is 93.32 g of fetal blood ([0.077×maternal weight 62 kg]×[maternal Ht on admission 34.3%/38.6]×0.022). The other method using maternal and fetal AFP to calculate the amount of the fetal blood flown into the maternal circulation is also developed,3) but unfortunately, the fetal AFP was not measured in our case. The estimated amount of the fetal blood flown into maternal circulation, calculated by their formula using the mean concentration of AFP in the newborn of 29th week gestation (266.745 mg/l) proposed by Bellini et al.,9) is 137.55 g of fetal blood. It seems that our calculation for the fetal blood loss seems overestimated in some reason, but at least, the fetus might be in critical condition due to massive FMH and saved by an immediate decision.
In case of traffic accident of the pregnant women, sometimes the condition is more severe than the first impression of the physician in outpatient clinic. The larger study showed that most of the critical perinatal condition after blunt injury came after minor injuries.10) Longer CTG examination for 4 to 6 hours may be sensitive to detect the critical condition of the fetus.10) Additionally, the proper use of seatbelt is widely known as the key of fetal and maternal safety.
None.