2016 Volume 4 Issue 1 Pages 6-10
2016 Volume 4 Issue 1 Pages 6-10
Although there are various causes of hemorrhage at the time of cesarean delivery, they are largely divided into bleeding from the separated surface of the placenta and atonic bleeding. A combination of hemostatic techniques such as balloon tamponade, compression suture, arterial ligation, transarterial embolization (TAE), and hysterectomy is important for successful hemostasis. When choosing a technique, features of local hemostatic techniques and vascular blockage techniques may need to be considered. Normal blood coagulation function is also important for achieving successful hemostasis.
Given advances in perinatal care, the maternal mortality rate in Japan decreased from 8.6 (out of 100,000) in 1990 to 3.8 in 2011.1) However, this rate has remained at the same level since 2007. The Japan Association of Obstetricians and Gynecologists established the Maternal Death Deliberation and Evaluation Committee in 2010 and has analyzed reported causes of maternal death. Obstetric hemorrhage was found to be the leading cause, accounting for 26% of all deaths; these events accounted for amniotic fluid embolism associated with disseminated intravascular coagulation (DIC) (36%), uterine rupture (13%), atonic bleeding (10%), premature separation of the normally implanted placenta (10%), lacerations (8%), and placenta accreta/placenta previa (5%).2) Cesarean section was most common delivery method (37%) associated with maternal death according to this report. Since critical obstetric hemorrhage occurs unexpectedly in a large volume, the prognosis is significantly influenced by whether rapid confirmation of hemorrhaging, early initiation of management including blood and other fluid transfusions, and timely hemostasis were performed.3,4)
In order to reduce the maternal mortality rate in the future, the most critical measures include enhancing the emergency transport network between high-level and primary health care institutions and providing appropriate treatment for patients with massive hemorrhage starting at the time of transport.
Although there are various causes of hemorrhage at the time of cesarean delivery, they are largely divided into bleeding from the separated surface of the placenta and atonic bleeding, and the volume of blood loss is based on cause and treatment of bleeding, as well as the time to myometrial suture. In order to prevent secondary atonic bleeding resulting from massive hemorrhage, it is necessary for clinicians to become familiar with hemostatic techniques and procedures so that they can respond more quickly.
(1) Bimanual compression, uterotonics, and balloon tamponadeSimilar to vaginal delivery cases, patients with atonic bleeding during cesarean delivery undergo bimanual compression and receive sufficient doses of uterotonics.5) When these methods are not sufficient for hemostasis, balloon tamponade is used.6)
The Bakri balloon tamponade is an easy-to-use device and achieves a high hemostasis rate of 84.0% to 91.7%.7,8) It is already recommended as the first-line therapy for massive hemorrhage in the guidelines of primary scientific societies worldwide9) and was approved for health insurance coverage in Japan in April 2013. At the time of performing this procedure, a balloon is inserted through the ostium of the uterus and 80 to 500 ml of saline is injected until hemostasis is achieved (Figure 1). Usually, 80 to 200 ml of saline is sufficient to achieve hemostasis. Since the Bakri balloon has a drainage port, it is easy to ascertain the volume of blood loss from the uterine cavity after insertion, allowing it to also be used for the tamponade test.4,10) In addition, as it is Latex-free, this device can be used in patients allergic to Latex.
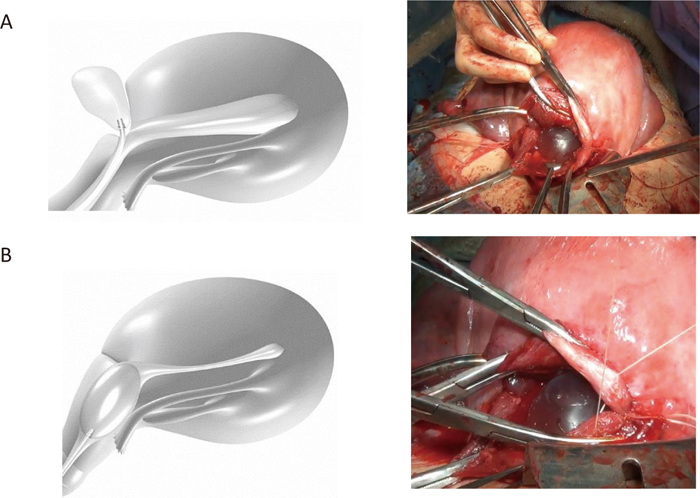
Balloon insertion during cesarean section.
(A) Balloon was inserted through the uterine wound.
(B) Eighty to 200 ml of saline is sufficient to achieve hemostasis.
Uterine compression suturing is performed in the uterine corpus when bimanual compression can achieve a certain level of hemostasis during laparotomy but continuous compression of the uterine corpus is still required.9,11) We use the modified B-Lynch technique at our hospital. Although vertical compression suturing is performed for bleeding from the separated surface in cases of placenta previa, a method applicable to concurrent atonic bleeding has also been reported.
(3) Arterial ligation technique, TAE, hysterectomyWhen uterine compression suturing fails to achieve hemostasis, ascending branches of the left and right uterine arteries, the ovarian artery, and the main uterine artery are ligated for hemostasis (stepwise uterine devascularization).12) If hemostasis is still not achieved, transarterial embolization (TAE) or total hysterectomy are performed without hesitation.
At the time of massive hemorrhage, the volume of blood loss is determined by how quickly the cause of bleeding is identified and whether an appropriate procedure is performed, whereas the patient’s prognosis is influenced by whether myometrial suturing after caesarean delivery can be completed. Since continuous bleeding leads to secondary atonic bleeding, it is essential to choose a hemostasis technique as soon as massive hemorrhaging is detected.
Hemostatic techniques are largely divided into local hemostatic techniques and blood flow blockage/ligation by TAE or devascularization. It is critical to understand adverse reactions and complications that may arise in association with the uses of both of these techniques. Local hemostatic techniques include gauze compression, Z-suture at the bleeding site, balloon tamponade, the modified B-Lynch technique, and vertical compression suture; these techniques may damage surrounding organs such as the urinary bladder and rectum. Meanwhile, since arterial ligation and TAE block blood flow to the uterus, a greater variety of complications as compared with local hemostasis can occur. Postoperative complications include uterine infection, uterine muscle necrosis, Asherman’s syndrome, menstrual abnormalities such as hypomenorrhea and oligomenorrhea, impaired endometrial growth, and infertility; in addition, serious adverse reactions including miscarriage or premature birth, uterine rupture, placenta accreta, and massive hemorrhage in subsequent pregnancies, are also possible.13,14) Therefore, blood flow blockage and ligation should be performed only when local hemostatic techniques such as compression suturing and balloon tamponade are not effective.
As discussed above, the uterine compression suture technique is effective with bimanual compression, and it should be used for atonic bleeding nonresponsive to drugs and when continuous compression of the uterine corpus is considered necessary.
The B-Lynch suture technique, first reported as a uterine compression suture technique in 1997, employs catgut suturing for compression hemostasis and blood flow blockage at the bleeding surface.15) B-Lynch updated this method by altering the strings to be used in the suture, from catgut to Monocryl, in 2005.16) The technique now uses absorbable sutures such as Vicryl Rapide.17) By using Vicryl Rapide, the suture compression period can be shortened, thereby minimizing deformation of the uterus and necrosis after suturing.18)
It is difficult to achieve sufficient ligation with the original method employing one needle and suture. At our hospital, we use two needles and sutures for compression suturing as a modification of the B-Lynch suture technique, similar to the B-Lynch suture modifications advocated by Hayman et al.19) (Figure 2).

Modified B-Lynch suture technique.
(A) First, bilateral uterine incision margins are ligated to stop bleeding from the ascending branch of the uterine artery. Next, after confirming the urinary bladder is sufficiently detached inferiorly, the needle and suture enter the anterior wall and exit the posterior wall at the lower end of the lateral side of the incision wound simultaneously, while the operator carefully avoids damaging the rectum.
(B) Suturing is performed similarly on the opposite side.
(C) The sutures are ligated at the left and right of the uterine fundus, while an assistant strongly compresses the uterus with both hands.
Compression by sutures has long been considered the primary hemostatic mechanism in uterine compression suture techniques. However, we have evaluated changes in blood flow in the uterine artery before and after suturing by ultrasound tomography and confirmed the speed of blood flow to be reduced and resistance index values to be increased.17) Since 90% of blood flow in the pregnant uterus usually comes from the uterine artery, this technique is presumed to have two actions, a hemostatic effect on the bleeding surface via compression and uterine blood flow reduction.15) In addition, as the suture is shorter than that used in the B-Lynch suture technique, it can easily and effectively be used by anyone. Compression of the uterine fundus on the left and the right is expected to reduce blood flow from not only the uterine artery but also the bilateral ovarian arteries.
When blood gushes from the separated surface in cases with placenta previa, double vertical compression sutures, with compression suturing at the lower uterine body, are placed to achieve hemostasis (Figure 3). This technique can be used for concurrent atonic bleeding following massive hemorrhage.
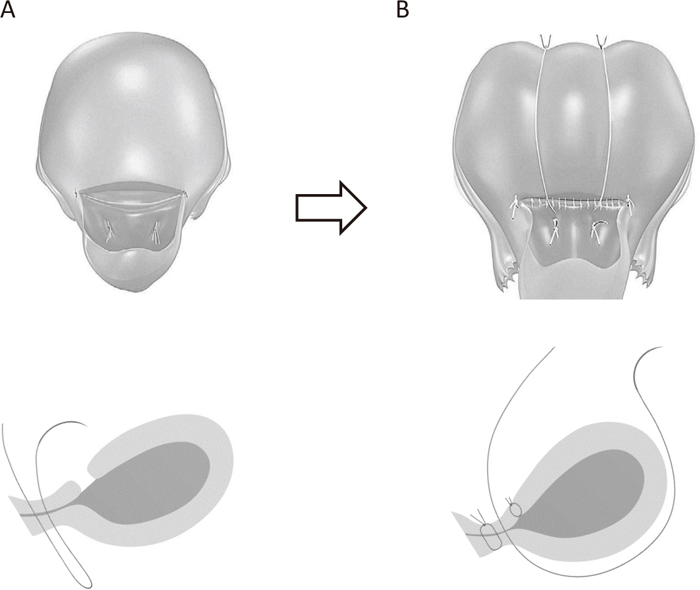
Double vertical compression sutures.
(A) Compression sutures at the lower uterine body are placed to achieve hemostasis.
(B) Additional sutures are placed, as with the modified B-Lynch suture technique.
Accordingly, the uterine compression suture technique is a hemostatic technique that should be mastered, especially at institutions where TAE cannot immediately be performed.
Although the hemostatic techniques described above can effectively suppress bleeding, normal blood coagulation function is important for achieving successful hemostasis. When DIC occurs, it causes secondary atonic bleeding, resulting in a vicious cycle of repeated massive hemorrhage.20,21) Therefore, when the amount of blood loss is large, the cause must be identified with prompt initiation of transfusions of blood and other fluids, as needed, based not only on the volume of blood loss but also general conditions, by applying the shock index as a reference. In cases with DIC, replenishing coagulation factors with fresh frozen plasma is the most important aspect of clinical management. Fibrinogen levels should be restored to 150 mg/dl or more as quickly as possible.3)
Balloon tamponade and the compression suture technique are easy to use and can effectively achieve hemostasis. They can be used by anyone and also at the time of transport from a primary health care institution to a high-level facility. Considering adverse reactions, TAE and arterial ligation should be performed only in patients in whom local hemostasis (e.g., balloon tamponade, compression suture) is unsuccessful. It is important to always have a protocol in place at each institution and to remain familiar with management methods that must be applied rapidly when critical hemorrhage is diagnosed.
None.