2016 Volume 4 Issue 2 Pages 53-64
2016 Volume 4 Issue 2 Pages 53-64
Initial treatment is crucial for saving the lives of patients with primary postpartum hemorrhage (PPH). Interventional radiology (IR) has become a major focus as a potential treatment for primary PPH because of its prompt hemostasis, low invasiveness, and the possibility of preserving fertility. Establishing and disseminating a management algorithm that allows for smooth communication between medical staff involved in the treatment is essential for prompt IR. IR for primary PPH consists of transcatheter arterial embolization (TAE) and balloon occlusion. Emergency introduction of infrarenal intraaortic balloon occlusion (IABO) can be useful for achieving temporary hemostasis in patients in critical condition. TAE has a high chance of successful hemostasis in cases of atonic bleeding. IR can also be introduced for other bleeding etiologies, but the order of priority — with respect to surgery and IR — has to be evaluated appropriately according to bleeding etiology, hemodynamic stability, human resources, and accessibility to operating and angiographic rooms. Patient transportation must also be considered for intensive and invasive treatment if conservative treatment is not successful.
Postpartum hemorrhage (PPH) is still a leading cause of maternal mortality. PPH is defined as blood loss of more than 500 ml following vaginal delivery, or of more than 1,000 ml following cesarean delivery. PPH within 24 h of delivery is termed primary PPH, whereas PPH occurring more than 24 h after delivery is termed secondary PPH. Generally, the patient’s condition is more critical in primary PPH than in secondary PPH, with a risk of maternal death. Prompt and appropriate multidisciplinary treatment is a priority for saving the life of a patient with primary PPH. Recently, attention has been focused on interventional radiology (IR), a potential treatment for PPH with demonstrated efficacy in achieving hemostasis. To help interventional radiologists and obstetricians to understand the utility of IR for PPH, and to standardize the indication and technique of IR, a guideline of IR for PPH was published by the Japanese Society of Interventional Radiology in 2012.1) This article describes the utility of IR in the management of primary PPH.
IR is a minimally invasive treatment methodology using imaging modalities including fluoroscopy, ultrasound, and CT. The IR techniques used for primary PPH include transcatheter arterial embolization (TAE) and arterial balloon occlusion.
TAE for obstetric and gynecologic bleeding was first described in 1979 by Heaston et al.2) Since then, the use of IR for PPH has increased, reportedly with a high success rate (80–90%).3,4) TAE is a method used to arrest bleeding by introducing embolic material from the catheter placed at the bleeding artery. In most cases, bilateral uterine arteries or the anterior division of internal iliac arteries are the first choices for embolization, even without extravasation observed, because of the high possibility of bleeding from these arteries or their branches. However, other bleeding arteries may have to be evaluated in particular occasions. This issue will be discussed later.
Temporary balloon occlusion of the artery is usually introduced in a situation of deteriorating hemodynamic status, or to obtain hemodynamic stability in an emergency situation. Temporary arterial balloon occlusion can stop bleeding simply by inflation of the balloon catheter at a site proximal to the bleeding point. In PPH, the occlusion level can be at the infrarenal abdominal aorta, bilateral common iliac artery, or internal iliac artery: the more proximal the occlusion, the more effective it will be, because it will eliminate blood flow from collateral pathways. The infrarenal position in the abdominal aorta is chosen to occlude blood flow from the ovarian artery, which is one of the major collateral pathways.5)
The techniques of TAE and balloon occulusion are relatively easy to perform, and physicians with a certain level of experience may be able to treat primary PPH successfully. However, primary PPH carries a risk of sudden exacerbation, with the pateint’s general condition possibly progressing to disseminating intravascular coagulation (DIC). In this very critical situation, the technical difficulty of performing IR will increase because treatment of primary PPH becomes a “race against time”. The operator needs to select an appropriate strategy, rapidly access the bleeding source, and perform an embolization.
IR can be performed under local anesthesia, which represents an advantage over surgical operation. Manipulation of the catheter and detection of the bleeding point is not disrupted by surrounding organs, tissues, adhesion, or hemorrhage. The hemostatic effect is prompt if catheterization and subsequent embolization is performed appropriately. Repeatability is another advantage; repeat IR can be considered if recurrence of bleeding occurs after TAE. Moreover, IR is available even after surgical operation (e.g., hysterectomy, arterial ligation), although the technical difficulty of the procedure may increase if bleeding continues from an anastomotic root. The greatest advantage of IR is the possibility of maintaining fertility; this will be discussed in more detail later. The high success rate of IR is another advantage.
One disadvantage of IR is radiation exposure. A previous report demonstrated a mean estimated absorbed radiation dose of up to 58.6 cGy (range: 20–73 cGy) for an ovary in TAE.6) However, radiation during TAE depends greatly on the procedure protocol.7) To decrease the radiation dose, repeat digital subtraction angiography, the field of view, pulse rate frequency, fluoroscopy time, and distance between the patient and image intensifier should all be minimized. A pelvic arteriogram can be skipped when the cause of bleeding is obvious, such as uterine atony, and with an experienced operator in IR for PPH. There has been no report of IR-induced skin reactions, or children being born with malformations. Other disadvantages of IR include the possibility of complications arising from catheterization and embolization, the possibility of re-bleeding, and the need for skilled operators and specialized facilities to perform angiography.
Prompt recognition and diagnosis is essential for the successful management of primary PPH.8) The presentation of PPH is often dramatic, although bleeding may be slower and seemingly less noteworthy; this, however, may ultimately result in critical blood loss and shock. The major factor in the adverse outcomes associated with primary PPH is a delay in initiating appropriate management. An important aspect influencing the outcomes of primary PPH is the performance of the commander. Although the obstetrician will likely be the primary commander, the anesthesiologist — in the operating suite — or the emergency physician could be the commander at a critical point. The commander has to perceive the situation comprehensively and assess all of the necessary and available treatment measures.
The order of priority in the choice of treatment measures has to be modified depending on the cause of PPH, available human resources, accessibility of the operating suite or angiographic suite, and the patient’s vital signs. The first-line treatment for PPH includes removal of the causative factor(s), especially surgically correctable injuries such as uterine rupture, inversion, and genital tract lacerations, blood transfusions, and the administration of uterotonic drugs such as oxytocin and prostaglandin analogs in conjunction with external massage of the uterus and uterine compression. The usefulness of a Bakri balloon for uterine atony has been reported recently.9,10,11) The timing of the decision to shift to a more intensive, invasive, and aggressive treatment should be appropriate and not subject to delay.
The commander should summon an interventional radiologist at the time when abnormal bleeding is observed, regardless of the severity of PPH, because IR is a useful and important measure for any type of pathogenesis or situation.12) Surgery should be the priority for traumatic bleeding, including uterine rupture, inversion, and genital tract lacerations. Nevertheless, in such situations, IR can still be helpful, if introduced promptly before any surgical intervention, for achieving a safer and more comfortable operation by reducing the bleeding speed and improving hemodynamic status. If there is massive bleeding from the placenta previa, it is ideal to introduce IR immediately in the operating room. Emergency introduction of arterial balloon occlusion can recover and maintain hemodynamic stability during hysterectomy or TAE. Atonic bleeding is the most frequent bleeding pathogenesis among primary PPH. IR for atonic bleeding has been shown to have high technical and clinical success rates of nearly 100%.13) Indeed, IR is a preferred priority hemostatic measure for atonic bleeding. If an institution has poor medical resources, the commander must arrange transfer of the patient to an advanced treatment hospital without delay.
Arterial ligation and hysterectomy provide a quick hemostatic measure for primary PPH during Cesarean operations. The outcome of hypogastric artery ligation is relatively unfavorable, with a reported success rate of 42%.14,15) Emergency hysterectomy is associated with high mortality because of the difficulty involved in hemostatic manipulation of swollen tissue due to congestion and bleeding.3) IR after hysterectomy or arterial ligation failure is often complex and challenging. By the time IR is performed, the patient has usually received multiple liquid and blood transfusions, which may lead to the development of systemic complications, such as DIC and acute respiratory distress syndrome (ARDS). Moreover, bleeding after ligation and hysterectomy is frequently attributed to arterial redistribution through rich collateral pathways or surgical damage to the tissues. Multiple and unexpected arteries may be associated with bleeding. Collateral arteries tend to be narrow and tortuous. More advanced IR techniques might be required in such cases. Thus, IR may be considered a first-line hemostatic measure for cases where IR is feasible and available promptly, or if the patient can withstand transportation to a more advanced hospital equipped with IR systems and a trained interventional radiologist.16)
Before starting the IR procedure, the interventional radiologist has to collect patient information, including the cause and amount of bleeding, vital signs, previous treatment (e.g., hysterectomy, ligation, intrauterine balloon tamponade), and blood transfusions already given. Based on this information, the interventional radiologist can evaluate the degree of urgency and decide on the size of the sheath introducer, whether to use a unilateral or bilateral approach – or a temporary balloon occlusion, where to catheterize, the choice of embolic material, and the embolic level.
If a patient is in critical condition due to massive bleeding, infrarenal IABO has to be considered to resuscitate and maintain hemodynamic stability in addition to other resuscitation measures. Embolization should not be super selective, as super selective catheterization may prolong the procedure time and thereby worsen the patient’s condition. It is essential to reduce the bleeding speed as soon as possible by performing gelatin sponge embolization from the bilateral anterior internal iliac artery or the main trunk of the internal iliac artery, even without an angiogram. This strategy is called “damage control interventional radiology (DCIR)”, for which the IR technique has to be rapid, minimal, but sufficiently effective to recover hemodynamics, rather than pursuing meticulous technical perfection.17) In most cases, angiography of patients in shock demonstrates vasoconstriction and no extravasation. The embolic material may not reach the bleeding point under conditions of vasoconstriction. Moreover, most of these patients will present with severe coagulopathy. Thus, the embolized artery may be recanalized and bleeding may recur after recovery from vasoconstriction. Careful and repeated angiographic observation is needed during this procedure. The importance of massive and quick replacement of coagulation factors should also be noted. Hemostasis will not be achieved without replacement of coagulation factors. If the patient undergoes a surgical operation, infrarenal IABO should be retained, and balloon occlusion should be applied during the operation. Inflation and deflation of the balloon should be controlled according to the bleeding situation and the patient’s hemodynamic status. The feasibility of a 40-min IABO was demonstrated in a previous report, although there is no consensus on the time window for balloon inflation or the decision to introduce heparinization during balloon occlusion.18) The risk of forming a thrombus with arterial occlusion must also be noted.
The supply of coagulation factors is a fundamental issue in the treatment of primary PPH. Any measures including IR will not be effective under a coagulopathy. In TAE, hemostasis is achieved by slowing down the blood flow via mechanical occlusion of the artery with embolic material, which leads to blood clotting. Clotting will not occur with coagulopathy because bleeding from distal fine arteries where the embolic material does not reach will continue through collateral pathways (Figure 1). There are several indicators for DIC including prothrombin time (PT), expressed as international normalized ratio (INR) values, activated partial thromboplastin time (APTT), and fibrinogen and D-dimer levels. Several studies have suggested that fibrinogen levels may be an independent predictor of the severity of PPH.19,20)
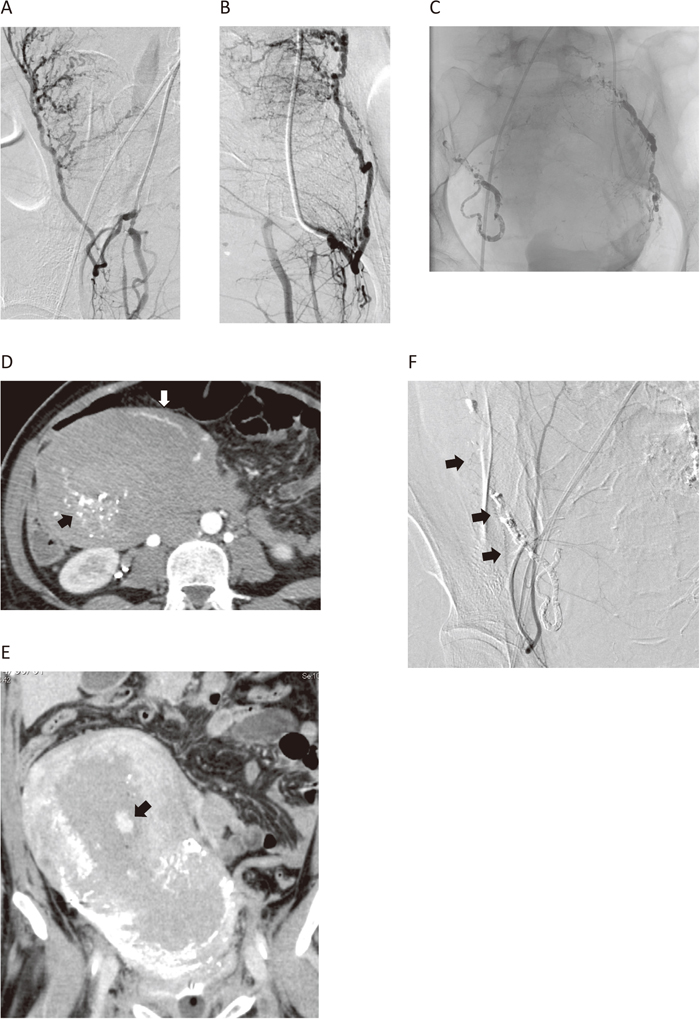
A 30-year-old woman transferred from another hospital due to atonic bleeding.
On arrival, her clinical presentation and laboratory data were as follows: blood pressure (BP), 70/40 mmHg; heart rate (HR), 117; shock index, 1.5; plasma fibrinogen level, 71 mg/dl. Angiograms of the right (A) and left (B) uterine arteries demonstrated dilatation but no extravasation. Embolization using a gelatin sponge followed by n-butyl 2-cyanoacrylate (NBCA) (C) failed to stop bleeding. On the CT scan after suspending angiography, the peripheral myometrium showed arterial enhancement (D, white arrow) without NBCA deposition (D, black arrow), indicating continuous blood flow through an anastomosis into the periphery of the myometrium. The CT image in the delayed phase shows extravasation in the uterus (E, arrow) indicating slow but continuous active bleeding. Retrospectively, peripheral enhancement of the uterine artery from the uterus round ligament artery was noted on the angiogram from the inferior epigastric artery (F, arrows).
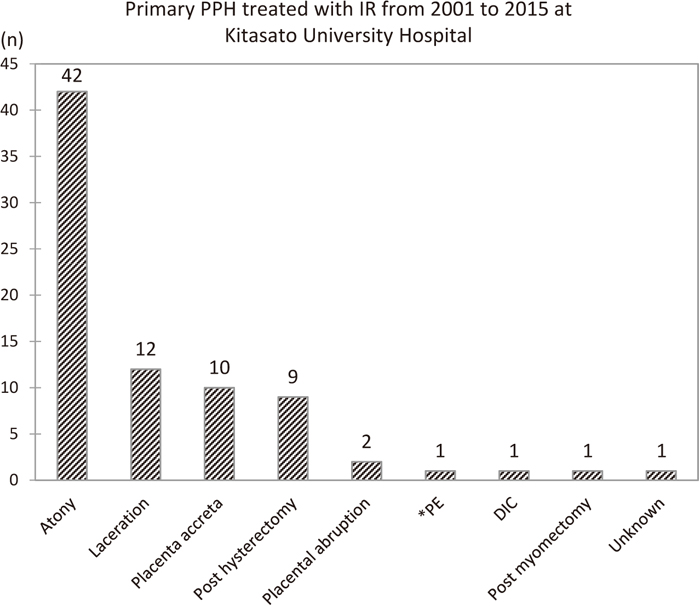
Primary PPH has many potential causes, with uterine atony being the most common. Figure 2 shows the causes of primary PPH treated with IR at Kitasato University Hospital from 2001 to 2015. The number of patients undergoing IR has increased with more widespread recognition of its utility. In the past 15 years, seven patients died from primary PPH. Table 1 provides a summary of cardiopulmonary arrest (CPA) patients. Of these, six were transported from other hospitals, and one suffered CPA due to a pulmonary thrombus during a Cesarean operation at Kitasato University Hospital; all underwent IR. None of the patients had angiograms demonstrating extravasation due to vasospasm, although bleeding continued (Figure 3). All of the patients died from severe DIC and multiple organ failure after resuscitation. Given that all but one were transferred from other hospitals, iatrogenic factors, including a delay in the diagnosis of abnormal bleeding, delay or lack of fluid and blood replacement, and delay in transfer, may have contributed to their deaths. In fact, recent studies have indicated that most reported deaths from PPH were preventable.21,22,23) However, it is clear that the condition of most patients deteriorated suddenly at some point, and they went into cardiac arrest. Thus, sensitivity to abnormal bleeding, and prompt and appropriate action for more aggressive treatment including transfer to an advanced treatment hospital, are essential in rescuing primary PPH patients. In our hospital, obstetricians inform the interventional radiologist when they recognize unusual PPH, or when they receive contact from another hospital about emergency transportation, regardless of the degree of severity or cause of bleeding. It is not uncommon that the patient takes a sudden turn for the worse in the ambulance, or that the information given regarding the bleeding cause and severity is inaccurate in transportation cases. Thus, staff must prepare for the worst by summoning medical personnel including a senior obstetrician, interventional radiologist, radiographer, and if necessary, an emergency physician and anesthesiologist, and giving an initial report to the blood transfusion department.
Summary of cases of primary postpartum hemorrhage (PPH) treated with interventional radiology (IR) at Kitasato University School of Medicine over 15 years.
* pulmonary embolism due to amniotic embolism.
| Case (year) | Age (years) (mean, 34) P=0.8* | Transfer | Cause | Blood loss from delivery to arrival (mean, 2,767 cc) P=0.6* | Hb on arrival (mean, 3.5±2.2 g/dl) P=0.004* | Time from delivery to CPA (mean, 141 min) | Time from delivery to arrival (mean, 172 min) P=0.4* | CPA |
|---|---|---|---|---|---|---|---|---|
| 1 (2001) | 37 | y | Laceration | 2,000 | 1.8 | 153 | 153 | On arrival |
| 2 (2002) | 29 | y | Atony | 2,200 | 4.8 | 94 | 94 | On arrival |
| 3 (2003) | 37 | y | Atony | 3,000 | 3.7 | 270 | 201 | Intraoperative after transfer |
| 4 (2006) | 33 | n | PE (amniotic embolism). | — | 2.0 | 0 | — | At delivery |
| 5 (2007) | 25 | y | Placental abruption | 4,000 | 7.0 After 2,500 cc of blood transfusion | 60 | 180 | At delivery |
| 6 (2007) | 40 | y | Atony | 2,900 | 1.4 | 270 | 185 | During IR after transfer |
| 7 (2013) | 33 | y | Atony | 2,500 | 6.7 | 180 | 210 | Before transfer |
Hb, hemoglobin; PE, pulmonary embolism; IR, interventional radiology.
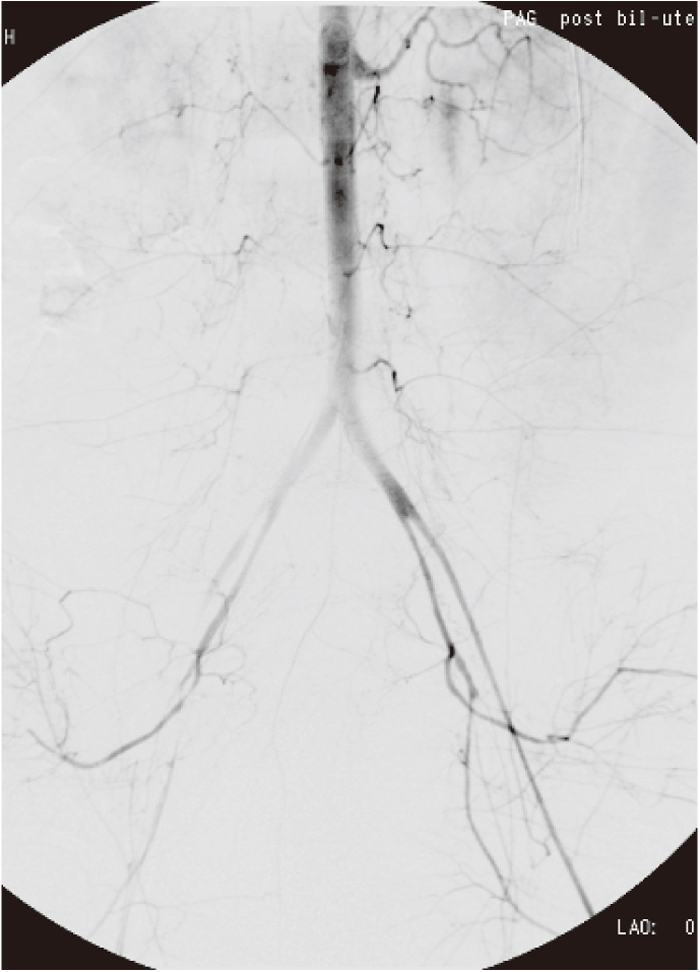
A 40-year-old woman transferred due to atonic bleeding. On arrival, she was promptly intubated because of vital shock (shock index, 1.1) and unconsciousness. Her laboratory data showed severe anemia (blood hemoglobin: 1.4 g/dl, platelets: 14,000×104/μl) and coagulopathy (fibrinogen: 50 mg/dl, prothrombin time: 110, activated partial thromboplastin time: 200). The reported blood loss before transfer, 2,900 cc, was considered to be an underestimate. Her angiogram demonstrated diffuse vasoconstriction but no extravasation. A procedure was performed under resuscitation for cardiac arrest. Although embolization of the bilateral internal iliac arteries using a gelatin sponge successfully stopped bleeding, the patient eventually died after embolization.
The IR procedure is usually performed under local anesthesia, although this depends on the patient’s condition. After introducing a sheath and catheterization, embolization is performed. The most important procedural issues are promptness, and making proper choices with respect to the artery to catheterize and the level of embolization (the latter is made according to a comprehensive assessment of the patient’s condition, laboratory data, and bleeding pathogenesis). Embolization is generally performed bilaterally, because there are rich collaterals and connections between both sides in the pelvis. If there is no extravasation but bleeding does not stop after embolization of pelvic arteries, there is a possibility of bleeding from the anastomotic root. The interventional radiologist needs to evaluate every possible collateral artery to find the bleeding source. Table 2 shows the collaterals that can be responsible for PPH.
| · Ovarian artery · Uterus round ligament artery · External pudendal artery · Deep circumflex iliac artery · Lumbar artery · Iliolumbar artery · Superior and middle rectal artery · Inferior mesenteric artery · Medial sacral artery |
The femoral arterial sheaths may be left in place even with hemodynamic stabilization at the conclusion of the procedure, to provide rapid access if the patient becomes hemodynamically unstable following treatment.
Atonic bleeding is a feasible and accepted indication for TAE. Ligation and hysterectomy used to be performed for atonic bleeding. Today, however, TAE is preferred as a first-line measure for atonic bleeding if IR is available 24 h a day, 365 days a year. Embolization of the bilateral uterine artery or anterior internal iliac artery using gelatin sponges will be effective in most cases. TAE can be performed even without extravasation, and where extravasation is not always observed.3,4) Atonic bleeding sometimes presents with comorbid bleeding factors such as genital tract lacerations and placenta previa. The management strategy should be modified depending on these factors.
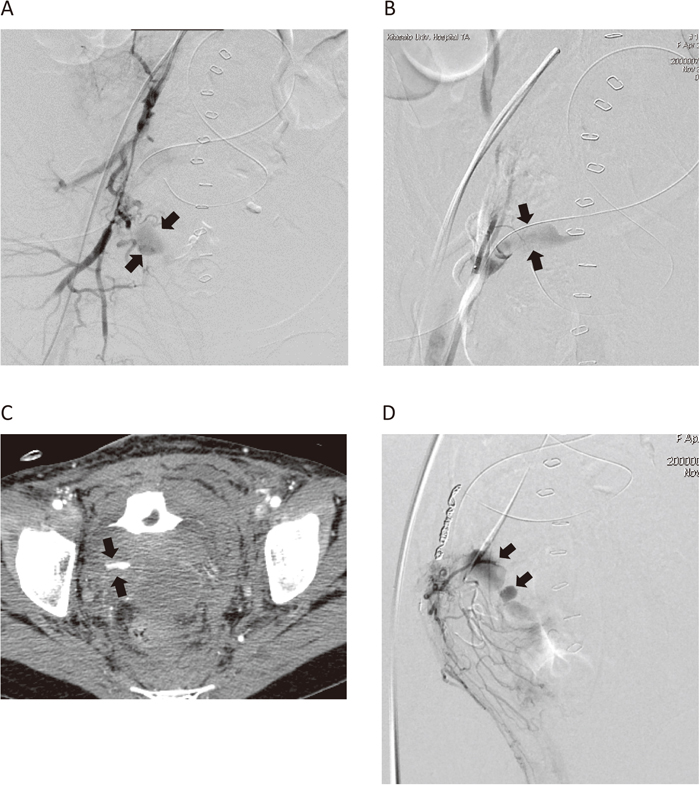
2. Trauma of the genital tractGenerally, surgical repair is indispensable for hemostasis in trauma of the genital tract. However, TAE is a helpful, and sometimes crucial, measure for hemostasis. One advantage of TAE introduced as a first-line treatment for trauma of the genital tract is that it provides a clear visual field for the obstetrician when repairing the trauma by reducing the bleeding. N-butyl 2-cyanoacrylate (NBCA) is often used for embolization in trauma cases because it makes a solid filling cast and occludes the artery as a glue (Figure 4). Contrast-enhanced CT prior to embolization may be appropriate, because information obtained from CT is useful for determining the amount and location of hematoma and detecting bleeding arteries, which in turn could help facilitate catheterization, resulting in a shorter procedure time.
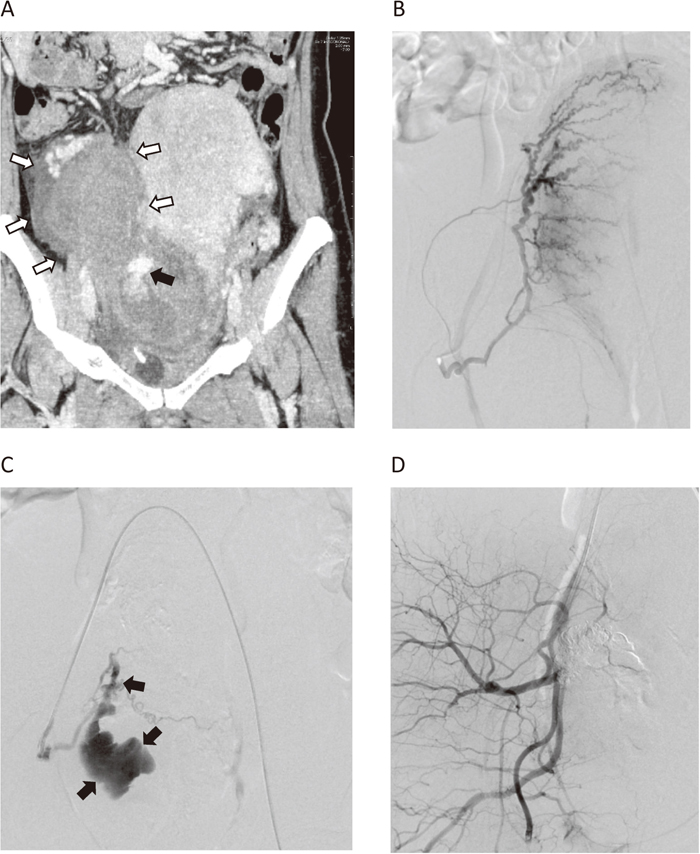
A 42-year-old woman with cervical lacerations. A mass was palpable on the left side of the cervix and uterus after vaginal delivery. Contrast-enhanced CT image revealed a huge hematoma neighboring the cervix and uterine body (A, white arrows), and extravasation from the cervix at the delayed phase (A, black arrow). An angiogram from the right uterine artery did not demonstrate extravasation (B). However, massive extravasation from the cervical branch appeared after embolization of the ascending portion of the right uterine artery using a gelatin sponge (C, arrow). The bleeding artery was occluded with NBCA administered from a microcatheter placed at the bleeding point. An angiogram after embolization showed complete hemostasis (D). She recovered without surgical repair of the torn cervix.
The choice of management of placenta previa accreta depends on the severity of clinical symptoms and the desire of the patient for further pregnancies. Bleeding from placenta accreta could be potentially life threatening and thus requires a multidisciplinary approach to management. Hysterectomy is often performed to achieve hemostasis. However, continuous and massive bleeding from the surface of the placenta may disrupt the visual field and operative maneuver, resulting in a delay in hemostasis or damage to the surrounding tissue and organs, and causing additional bleeding from the surface of the adhesion. Continuous bleeding may develop into coagulopathy, causing uncontrolled bleeding in a worst-case scenario. Before it turns into a serious condition, infrarenal IABO should be introduced. One problem expected here is that placement of a sheath introducer may be intractable due to vasoconstriction and the lack of pulsation at the groin during vital shock (Figure 5). Surgical cut-down of the femoral artery may be considered if puncturing the femoral artery is unsuccessful. Embolization may then be performed if the patient desires to preserve fertility. If hysterectomy is performed, infrarenal IABO should be retained, with intermittent deflation of the balloon occlusion every 20–30 min, although there is no consensus regarding ‘safe’ occlusion time.
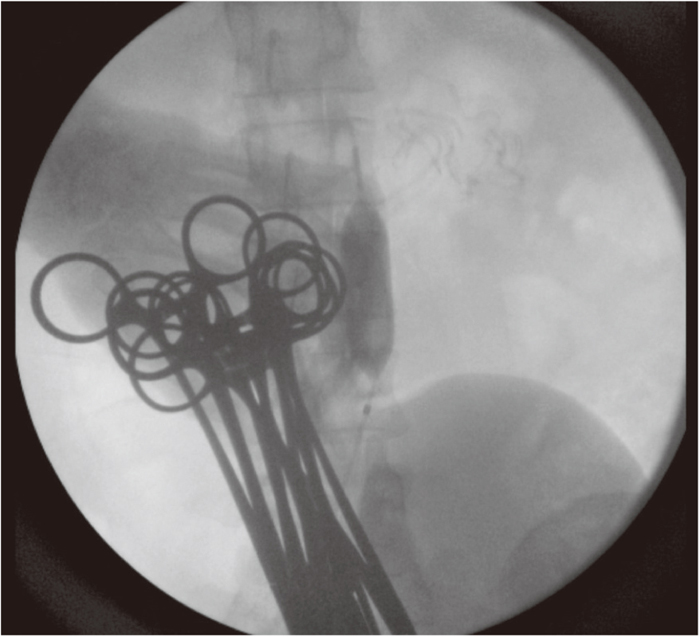
A 30-year-old woman with placenta increta. She had sudden massive bleeding during Cesarean delivery and her blood pressure had fallen below 60 mmHg. The interventional radiologist (IRist) rapidly placed a sheath introducer from the right groin and inflated an aortic balloon catheter in the abdominal aorta under the renal artery. The blood pressure recovered soon after inflation of the aortic balloon. A hysterectomy was performed under inflation of the aortic balloon catheter, which was shifted to occlude the bilateral common iliac artery. The balloon was deflated for 1–2 min every 30 min with careful observation of vital signs and Doppler auscultation of the dorsal artery of the foot.
Even if hemorrhage is controlled and hysterectomy is avoided with TAE, the retained product may cause late-phase bleeding and infection. It should be noted that the retained placenta can be associated with prevention of adequate contraction, which can cause atonic bleeding. If the risk of placenta accreta is expected, because of placenta previa before delivery, placement of a sheath introducer and balloon catheter prior to Cesarean delivery (“prophylactic IR”) may serve as an immediate measure against massive bleeding. In fact, many doctors in clinical practice realize the effect of balloon occulucsion in reducing the bleeding speed and amount in a case of placenta accreta during Cesarean delivery. However, evidence for the feasibility and safety of prophylactic IR in the current literature is scarce and controversial, with some reports demonstrating no effect of reducing bleeding or the amount of blood transfusion.24,25) There are several presumed reasons for unfavorable results, including lack of technical sophistication, cohort bias, and various technical issues regarding the balloon positioning, the occlusion timing, and the adjunctive use of TAE. Also, complications arising from temporary balloon occlusion, including thromboembolism and lower limb ischemia, have been described in several reports.25,26,27,28) The most important factor when performing prophylactic IR is to minimize vascular complications by careful application of the technique and vascular surveillance.
4. Iatrogenic bleeding after obstetric surgeryIR is a minimally invasive, feasible, and effective approach for bleeding after obstetric laparotomy because the maneuver is not disrupted by hemorrhage, organs, or adhesion. Angiography in postoperative bleeding will demonstrate extravasation or pseudoaneurysm in most cases.29,30) Pseudoaneurysms arise frequently from the internal pudendal artery, the cervical branches of the uterine artery, and the vaginal artery after a vaginal birth. Contrast-enhanced CT is recommended prior to IR to detect bleeding arteries, given that there are several possibilities for bleeding arteries (Figure 6). The disadvantages of extra use of contrast material and radiation exposure with CT will be counterbalanced by shortened bleeding artery seeking time, resulting in a reduced radiation dose and more efficient and faster hemostasis at angiography. Super-selective catheterization into the bleeding point is ideal, as in many cases bleeding occurs due to relatively large tears in arteries; tears can be occluded effectively by introducing embolic material to the bleeding point.
A 34-year-old woman who had a hysterectomy due to uterine bleeding after Cesarean delivery. An angiography demonstrated extravasation from the branches of the anterior division of the internal iliac artery (A, arrow). After embolization of the anterior division of the internal iliac artery, massive bleeding from the epigastric artery due to drain placement was found (B, arrow), and was embolized using a metallic coil and NBCA. On the following day, contrast-enhanced CT was performed because unstable vital signs revealed an extravasation in the right pelvis (C, arrow). An angiogram demonstrated re-bleeding through the anastomosis from the inferior mesenteric artery to the branch of the internal iliac artery (D, arrow). Embolization from the inferior mesenteric artery stopped the bleeding successfully.
Arterial ligation used to be performed frequently for PPH, but the outcomes vary.14,15,31,32) Thus, this technique has been performed at a decreasing frequency and is limited to situations where TAE is not readily available. The causes of re-bleeding after ligation include incomplete ligation and complete ligation.33) The proximal ligation of a bleeding artery may cause continued bleeding from an anastomotic arterial root. TAE for re-bleeding after complete ligation could be refractory, because there are various collateral vessels that could be causing the bleeding. Anastomotic roots are often too narrow and tortuous for catheterization. Reflux and migration of embolic material must be considered when the depth of catheterization is insufficient. Performing CT with contrast material is recommended in order to locate bleeding vessels prior to TAE.
6. Recurrence of bleeding after TAERecurrence of bleeding after TAE is observed in 5–10% of cases.3,4,34) The angiographic causes of re-bleeding after TAE include recanalization of the embolized artery due to coagulopathy, bleeding from collaterals due to proximal embolization, overlooking the bleeding artery during the first IR, release of arterial spasm, and remaining causative factors, such as the retained placenta and trauma to the genital tract. Etiologies of failed TAE have been reported, including severe DIC, massive blood transfusion, massive blood loss, invasive placenta, and embolization with gelatin sponges. Angiography from the point above the renal artery, or a contrast-enhanced CT scan before re-intervention, is recommended to determine the cause of re-bleeding for efficient re-embolization (Figure 7).
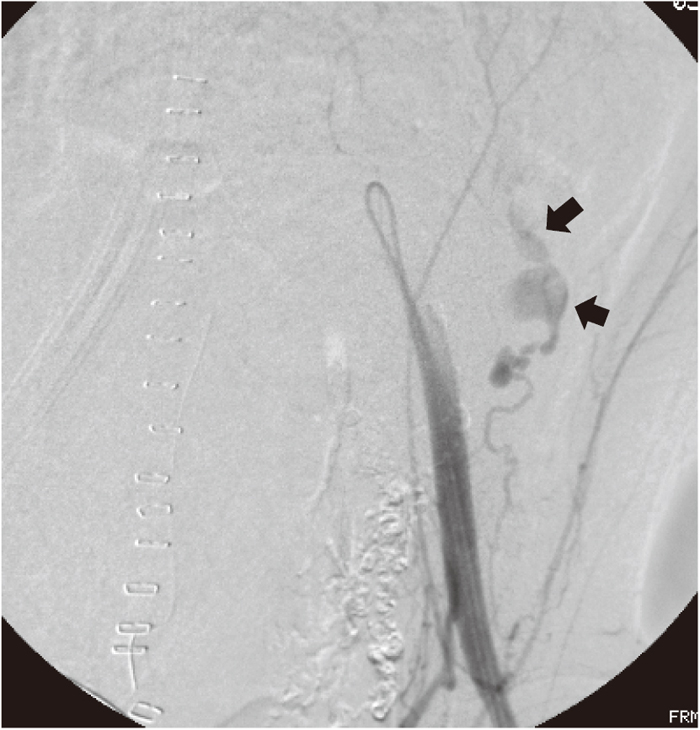
A 34-year-old woman who had a supracervical hysterectomy because of massive bleeding from the placenta percreta. Transcatheter arterial embolization (TAE) for the bilateral uterine artery using NBCA under infrarenal intraaortic balloon occlusion (IABO) was performed for continuous bleeding from the remaining placenta. However, she needed to undergo re-embolization because of hemodynamic instability on the following day. An angiogram from the external iliac artery revealed extravasation from the deep iliac circumflex artery (arrow), which was considered to be due to the operative trauma. Embolization using NBCA stopped the bleeding successfully.
Complications of IR include vascular injury from catheterization and ischemic events associated with embolization. With adequate expertise and skill, however, the complication rate can be lowered to less than 1.6%.35) Hematomas and arteriovenous fistulas at the puncture point, arterial dissection, and thrombus formation have been reported as complications of catheterization.36,37) Migration of embolic material into untargeted arteries, usually the posterior division of the internal iliac artery or, rarely, a lower limb artery, can cause buttock claudication, skin ischemia, bladder necrosis, nerve ischemia, and limb ischemia.38,39) However, not all patients who undergo aggressive bilateral embolization with large quantities of embolic material from the main trunk of the internal iliac artery develop pelvic complications. Young women can usually tolerate pelvic embolization well because of rich collateral vessels (if there is no underlying vessel disease). Arterial spasm from vital shock, acute anemia, hypovolemic shock, the use of vasoconstrictive drugs, prolonged immobility after a procedure, and other individual factors may contribute to the occurrence of ischemic complications.
The possibility of Asherman’s syndrome, also known as intrauterine adhesions, due to uterine ischemia and following inflammation has been suggested after embolization.40) Subsequent complaints of amenorrhea or decreased menstrual flow may adversely affect fertility. Some previous reports have suggested a relationship between menstrual disorder and ovarian dysfunction due to ischemia of the ovary caused by migration of embolic material though utero-ovarian anastomosis.40,41,42)
Uterine necrosis following the isolated use of small polyvinyl alcohol particles and gelatin sponge, or the combined use of gelatin sponge and polyvinyl alcohol particles, has been reported previously.36) The penetration of small particles into the peripheral zone of the uterine artery may be a causative factor in ischemic complications. Instead of case series reporting on these complications, most previous reports suggest that embolization for PPH does not compromise a woman’s subsequent fertility or obstetric outcomes. Preparation of a gelatin sponge by the cutting method may reduce the possibility of ischemic complications, because the particles will be relatively more uniform in size compared to those prepared by a pumping method.
Obstetricians and other medical staff who are engaged in the treatment of PPH need to recognize the utility of IR; any of these personnel may suggest consulting an interventional radiologist before it is too late or, even better, immediately after recognizing abnormal bleeding. Close, precise, and efficient communication and teamwork among the obstetrician, anesthesiologist, and interventional radiologist is essential for achieving effective, successful, and minimally invasive hemostasis in primary PPH.
None.