2016 Volume 4 Issue 2 Pages 68-73
2016 Volume 4 Issue 2 Pages 68-73
Aim: Rebound hypertension after termination of nicardipine intravenous (IV) infusion in cesarean section (C/S) patients with hypertensive disorders of pregnancy was investigated.
Methods: Twenty-nine patients with gestational hypertension (GH) and 37 with preeclampsia (PE) after C/S were enrolled. After termination of nicardipine IV infusion, 12 GH and 24 PE patients were treated with oral nifedipine or labetalol, while 17 GH and 13 PE patients received no antihypertensive agents. The average systolic blood pressure (SBP) was calculated for 0–24 h after IV termination, and the incidence of a rebound SBP increase (≥160 mmHg) within 8 h after IV termination was investigated.
Results: A transient rebound increase in SBP was observed in 25% of GH and 21% of PE patients with oral administration of antihypertensive agents and in 35% of GH and 15% of PE patients without oral administration of antihypertensive agents. A daily average SBP of ≥160 mmHg was observed in 17% of GH and 4% of PE patients with oral administration of antihypertensive agents and 12% of GH and 0% of PE patients without oral administration of antihypertensive agents.
Conclusions: In managing the characteristic rebound BP increase after nicardipine IV infusion, the daily average SBP could be maintained at <160 mmHg in most patients with GH and PE despite transient hypertension.
The clinical guideline for hypertensive disorders of pregnancy (HDP) by the Japan Society for the Study of Hypertension in Pregnancy (JSSHP) recommends that an intravenous infusion of antihypertensive agents (nicardipine, hydralazine or nitroglycerin) should be given instead of oral administration during and after cesarean section (C/S) and during labor, given the difficulty of maintaining blood pressure (BP) control in HDP patients, and the intravenous infusion is needed for a hypertensive emergency (systolic blood pressure [SBP] ≥180 mmHg and/or diastolic blood pressure [DBP] ≥120 mmHg).1)
The JSSHP guideline states that intravenous nicardipine infusion is commonly chosen in the management of hypertension during pregnancy and in the postpartum period. In postpartum patients, intravenous nicardipine infusion is started at 1 mg/h when an increase in SBP (≥160 mmHg) or DBP (≥110 mmHg) is noted. The infusion is usually performed using nicardipine stock solution (1 mg/ml) at 1–6 ml/h to achieve an SBP of 120–140 mmHg and DBP of 70–90 mmHg.1)
We previously reported the management of hypertension focusing on SBP, according to the procedure described in the JSSHP guideline. The subsequent administration of intravenous nicardipine infusion helped maintain SBP under 140 mmHg and achieved a stable SBP after 2 h. The infusion was administered for 2 days in most patients with severe hypertension after C/S.2)
HDP is clinically classified into gestational hypertension (GH) and preeclampsia (PE) depending on the presence of proteinuria, according to the JSSHP criteria.3) PE, which is characterized by both hypertension and proteinuria, is associated with coagulopathy, endothelial cell dysfunction, and organ disorders. PE is considered more severe than GH, as it is more difficult to control hypertension in PE than in GH with antihypertensive agents administered orally4) or intravenously.2) An increase in BP, the so-called rebound phenomenon, just after termination of antihypertensive agents is well known. An acute increase in BP, including rebound hypertension, is a risk factor for cerebral hemorrhage, which is among the severest disorders of hypertensive pregnancy.
In the present study, rebound hypertension, i.e., an increase in BP, observed after termination of intravenous nicardipine infusion was retrospectively examined in patients with PE and GH after C/S focusing on SBP, based on our previous finding5) that SBP reflects changes in BP in pregnant and postpartum women.
In this study, 29 GH and 37 PE patients were enrolled (Table 1). GH and PE were diagnosed up to 90 days postpartum according to the criteria of the JSSHP.1)
| Number | SBP (mmHg) | Stable dose (mg/h) | Total dose (mg) | Stable SBP (mmHg) | |
|---|---|---|---|---|---|
| I.GH | |||||
| With oral administration | 12 | 175±10 | 1.3±0.5 | 48±26† | 138±13‡ |
| Without oral administration | 17 | 174±13 | 1.3±0.5 | 21±15 | 134±9‡ |
| II.PE | |||||
| With oral administration | 24 | 172±18 | 2.0±0.9* | 95±62*† | 133±11‡ |
| Without oral administration | 13 | 165±15 | 1.8±0.8 | 39±25* | 132±15‡ |
Data were expressed as mean±SD.
*; P<0.05 vs. GH, †; P<0.05 vs. without oral administration, ‡; P<0.05 vs. SBP.
GH, gestational hypertension; PE, preeclampsia; SBP, sysytolic blood pressure; DBP, diastolic blood pressure.
In GH and PE patients after C/S, 1 to 6 mg/h of nicardipine was administered by intravenous drip infusion with a syringe pump when SBP and DBP increased to ≥160 mmHg and ≥110 mmHg, respectively, for almost 2 days until the target SBP and DBP (120–140 mmHg and 70–90 mmHg, respectively) were achieved1) (Figure 1). After intravenous nicardipine infusion, 12 GH and 24 PE patients received oral nifedipine (20–40 mg of long-acting nifedipine/day) or labetalol (300–400 mg/day), while 17 GH and 13 PE patients received no oral antihypertensive agents. Changes in SBP after drip infusion were analyzed in four groups, GH and PE with or without oral administration of antihypertensive agents. The average SBP was calculated for 0–24 h and 24–48 h with and without oral antihypertensive agents. Furthermore, the incidence of a transient increase in SBP (≥160 mmHg) was evaluated at 8 h and 8–16 h after termination of intravenous nicardipine infusion.

The procedure for intravenous nicardipine drip infusion according to the clinical guideline for HDP by the JSSHP.1)
This study was approved by the local ethics committee.
Statistical analysisData are expressed as mean±SD. Statistical analysis was performed using Excel Toukei 2012 (SSRI Co., Ltd., Tokyo, Japan). The unpaired t-test and chi-squared test were used to compare PE and GH patients. The level of significance was set at P<0.05.
Intravenous nicardipine infusion caused a decrease in SBP and achieved an appropriate and stable BP (120<SBP<160 mmHg) in both GH and PE patients. The stable dose of intravenous nicardipine was higher in PE (2.0±0.9 mg/h) than in GH (1.3±0.5 mg/h) patients with oral administration of antihypertensive agents, while the doses were similar (1.8±0.8 mg/h in PE vs. 1.3±0.5 mg/h in GH) in patients without oral administration of antihypertensive agents (Table 1).
In most cases, intravenous nicardipine was administered for at least 24 h, with a mean duration of 37±19 h in GH and 47±22 h in PE patients with oral administration of antihypertensive agents, and 19±10 h in GH and 29±19 h in PE patients without oral administration of antihypertensive agents. Oral administration of antihypertensive agents was started approximately 48 h after C/S.
The total dose of intravenous nicardipine was greater in patients with oral administration of antihypertensive agents (48±26 mg in GH and 95±62 mg in PE) than in patients without oral administration of antihypertensive agents (21±15 mg in GH and 39±25 mg in PE) (Table 1).
Rebound BP increase after termination of intravenous nicardipine infusionIn most patients, a rebound BP increase was observed within 24 h after termination of intravenous nicardipine infusion. In GH patients, a transient SBP increase (≥160 mmHg) was observed in 3 of 12 (25%) patients, including one with an SBP ≥180 mmHg, with oral administration of antihypertensive agents, and 6 of 17 (35%) patients without oral administration of antihypertensive agents within 8 h after termination of intravenous nicardipine infusion (Figure 2A and Table 2). In PE patients, a transient SBP increase was observed in 5 of 24 (21%) patients, including two with an SBP≥180 mmHg, with oral administration of antihypertensive agents, and 2 of 13 (15%) patients without oral administration of antihypertensive agents within 8 h after termination of intravenous nicardipine infusion (Figure 2B and Table 2). The incidence of transient rebound BP increase was reduced by about half after 8–16 h in both GH and PE patients (Table 2).
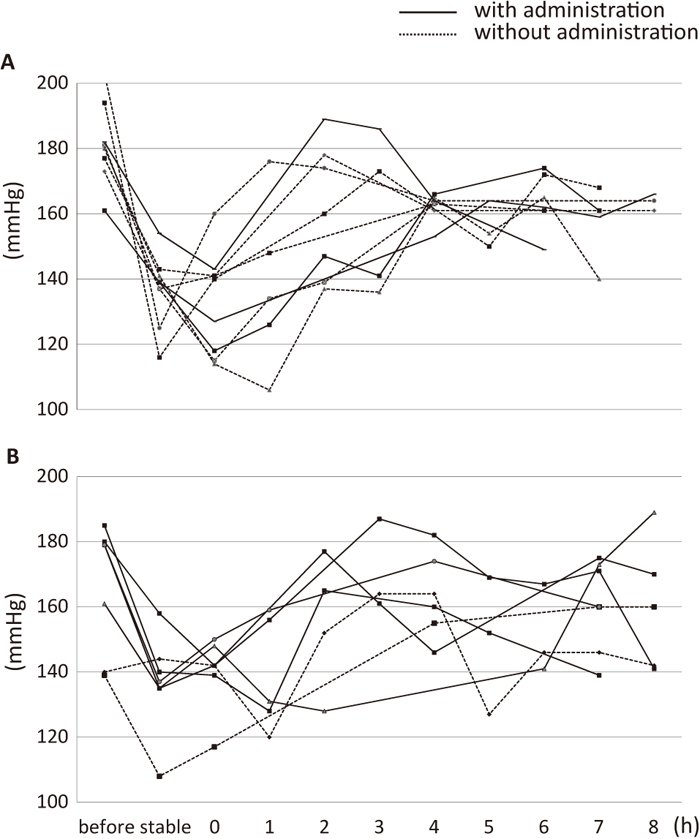
Transient SBP increase after termination of intravenous nicardipine infusion.
(A) In GH patients, a transient SBP increase (≥160 mmHg) was observed in 3 with and 6 without oral administration of antihypertensive agents within 8 h after termination of intravenous nicardipine infusion.
(B) In PE patients, a transient SBP increase (≥160 mmHg) was observed in 5 with and 2 without oral administration of antihypertensive agents within 8 h after termination of intravenous nicardipine infusion.
| Number | Transient SBP ≥160 mmHg in 0–8 h (%) | Transient SBP ≥160 mmHg in 8–16 h(%) | |
|---|---|---|---|
| I.GH | |||
| With oral administration | 12 | 3 (25) | 1 (8) |
| Without oral administration | 17 | 6 (35) | 2 (12) |
| II.PE | |||
| With oral administration | 24 | 5 (21) | 3 (13) |
| Without oral administration | 13 | 2 (15) | 0 (0) |
SBP; systolic blood pressure.
SBP was higher at 0–24 h after termination of intravenous nicardipine infusion compared to just before termination (GH: 144±13 mmHg vs. 136±13 mmHg with oral antihypertensive agents; 143±14 mmHg vs. 128±15 mmHg without oral antihypertensive agents, PE: 145±11 mmHg vs. 136±9 mmHg with oral antihypertensive agents; 140±11 mmHg vs. 125±15 mmHg without oral antihypertensive agents). In PE patients, SBP was higher just before termination of intravenous nicardipine infusion with oral antihypertensive agents than without. However, there was no difference in SBP after termination of intravenous nicardipine infusion with or without oral administration of antihypertensive agents between GH and PE patients. Furthermore, an average SBP of ≥160 mmHg at 0–24 h was observed in 4% of PE and 17% of GH patients with oral administration of antihypertensive agents, as compared to 0% of PE and 12% of GH patients without oral administration of antihypertensive agents (Table 3). The average SBP and transient increase over 24–48 h were similar to those over 0–24 h (Table 3).
| Number | SBP just before termination of nicardipine | In 0–24 h | In 24–48 h | |||||
|---|---|---|---|---|---|---|---|---|
| Average of SBP | Change of rate | Average of SBP≥160 mmHg | Average of SBP | Change of rate | Average of SBP≥160 mmHg | |||
| (mmHg) | (mmHg) | (%) | (%) | (mmHg) | (%) | (%) | ||
| I.GH | ||||||||
| With oral administration | 12 | 136±13 | 144±13* | 4±8 | 2 (17) | 139±12 | 0±9 | 1 (8) |
| Without oral administration | 17 | 128±15 | 143±14* | 5±10 | 2 (12) | 144±14 | 6±12 | 2 (12) |
| II.PE | ||||||||
| With oral administration | 24 | 136±9† | 145±11* | 6±8 | 1 (4) | 139±13* | 1±13 | 1 (4) |
| Without oral administration | 13 | 125±15 | 140±11* | 6±12 | 0 (0) | 142±8 | 8±10 | 0 (0) |
Data were expressed as mean±SD.
*; P<0.05 vs. SBP just before termination of intravenous nicardipine infusion, †; P<0.05 vs. without oral administration.
GH, gestational hypertension; PE, preeclampsia.
Nicardipine blocks the inflow of Ca2+ through L-type channels and decreases the concentration of Ca2+ in vascular smooth muscle cells. An intravenous infusion of nicardipine acts within 10 min, has a half-life of 2 to 5 min, and usually decreases BP within 20 min.6) Thus, intravenous nicardipine infusion has a high potency to control maternal BP and is equal to labetalol, a commonly used α/ß blocker.6) However, labetalol is not available for intravenous use in Japan. Seki et al. reported that intravenous nicardipine infusion could be effective for managing BP in HDP patients, in a comparison of short-term (≤7 days), medium-term (8–28 days), and long-term (≥29 days) treatments.7)
The clinical guideline for HDP set forth by the JSSHP recommends that intravenous infusion of nicardipine, hydralazine or nitroglycerin should be given instead of oral administration during and after C/S and during labor, given the difficulty of maintaining BP control in HDP patients. Furthermore, it is also needed for a hypertensive emergency (SBP≥180 mmHg and/or DBP≥120 mmHg).1)
In the JSSHP criteria, HDP is classified mainly into GH for hypertension alone and PE with hypertension and proteinuria.3) The pathogenesis of GH and PE differs, with PE thought to be more severe than GH, since PE can develop into eclampsia. In a previous study, we found that the higher the BP (SBP ≥180 mmHg), the higher the dose of nicardipine required for GH. For PE, even though most patients had moderate hypertension (180>SBP≥160 mmHg), the required dose of nicardipine was even higher.2) Furthermore, we present the first evidence that nicardipine is useful in the management of BP according to the clinical guideline of HDP by the JSSHP.
In the present study, the dose of intravenous nicardipine required to achieve target BP levels was higher in PE patients than in GH patients, which was consistent with our previous results.2) The NICE guidelines also recommend different management strategies for PE and GH.8)
In the present retrospective study, a transient rebound increase in BP was observed when oral administration of antihypertensive agents was stopped in patients with HDP managed according to the JSSHP guideline, in both PE and GH patients with or without oral administration. Within 8 h after termination of intravenous nicardipine infusion, a transient increase in SBP (≥160 mmHg) was noted in 35% and 25% patients with and without oral administration of antihypertensive agents, respectively, in GH patients, as compared to 21% and 25% of patients with and without oral administration of antihypertensive agents, respectively, in PE patients. The average SBP at 0–24 h after termination of intravenous nicardipine infusion was similar (about 140 mmHg) in all groups, although a significantly higher average SBP was obtained just before termination. An average SBP of ≥160 mmHg was observed in less than 20% of GH patients and less than 10% of PE patients with or without oral administration of antihypertensive agents.
From these results, the management protocol of hypertension was thought to be almost proper because average SBP after termination of infusion was about 140 mmHg and cases beyond 160 mmHg of SBP were few. Importantly, a transient rebound increase was noted in roughly 30% of GH and 20% of PE patients.
An elevated BP more than 48 h after C/S might be less important in the management of both GH and PE, because probably it caused the critical disorders, such as eclampsia within 48 h in our previous reports.9) The patient with a SBP of >160 mmHg and DBP of >110 mmHg after termination of intravenous nicardipine infusion was administered an additional nicardipine infusion according to the criteria. However, the management of rebound hypertension in BP has not been established.
Oral administration after termination of intravenous infusion is controversial with respect to its effectiveness in preventing a rebound BP increase. In PE, but not GH, SBP just before termination of infusion was significantly higher with oral administration than without oral administration. Whether or not patients should receive oral administration of antihypertensive agents was determined at the discretion of the individual clinician due to the retrospective study design. Therefore, it is possible that antihypertensive agents were administered preferentially to patients with more severe hypertension. Accordingly, the time course as well as selection criteria of oral antihypertensive agents could not be clarified. Furthermore, whether there was a difference in the incidence of a transient BP increase between labetalol and slow-release nifedipine administration remains unclear. A further study will be needed to address these limitations associated with the retrospective design.
In conclusion, with respect to the characteristic rebound BP increase after termination of intravenous nicardipine infusion in PE and GH patients, the average SBP could be maintained at ≤160 mmHg in most patients despite transient hypertension with or without oral administration of antihypertensive agents.
This work was partly supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (26462496).
None.