2021 Volume 9 Issue 2 Pages 40-45
2021 Volume 9 Issue 2 Pages 40-45
Few reports have described the impact of chemical pregnancy on a viable fetus in heterotopic cervical pregnancy. A 38-year-old primigravida was transferred to our hospital with severe abdominal pain at 32 weeks of gestation. She was tentatively diagnosed with placental abruption with intrauterine fetal death (IUFD), and a stillborn fetus was delivered vaginally. Massive vaginal bleeding continued during labor and was uncontrolled after delivery, requiring a hysterectomy. Macroscopic examination revealed a solid nodule in the uterine cervix. Histologically, the nodule consisted of villous tissue. Fluorescent in situ hybridization revealed two placental tissues derived from different embryos, indicating heterotopic cervical pregnancy. Although pregnancy was achieved after double embryo transfer, no early ultrasound findings suggested cervical pregnancy. This is the first report of heterotopic cervical pregnancy in which retained products after a chemical pregnancy caused sudden massive hemorrhage and IUFD in the third trimester.
Heterotopic pregnancy can result in massive hemorrhage from the site of ectopic pregnancy and is potentially life-threatening. In cases of heterotopic cervical pregnancy, a coexisting ectopic implantation in the uterine cervix is generally detected early by routine transvaginal ultrasound, and is treated surgically or medically to preserve intrauterine pregnancy. Here we report a case of heterotopic cervical pregnancy in which retained products after a chemical pregnancy caused sudden massive bleeding and fetal death at 32 weeks of gestation, along with a review of relevant literature.
A 38-year-old primigravida became pregnant after in vitro fertilization and embryo transfer. Although she underwent double embryo transfer, a singleton pregnancy was confirmed by her previous doctor. Her pregnancy course was uneventful. At 32 weeks and 5 days of gestation, she suddenly complained of severe lower abdominal pain and was transferred to our hospital. On admission, her vital signs were as follows: blood pressure 108/75 mmHg, heart rate 85, and SpO2 100% at room air. Uterine tone was extremely firm and board-like, but no vaginal bleeding was observed. Transabdominal ultrasound revealed intrauterine fetal death (IUFD), and transvaginal ultrasound revealed a hematoma-like high echoic lesion and a low echoic mass of unknown origin near the internal os of the uterine cervix (Figure 1A). Based on these findings, a diagnosis of placental abruption with IUFD was made.
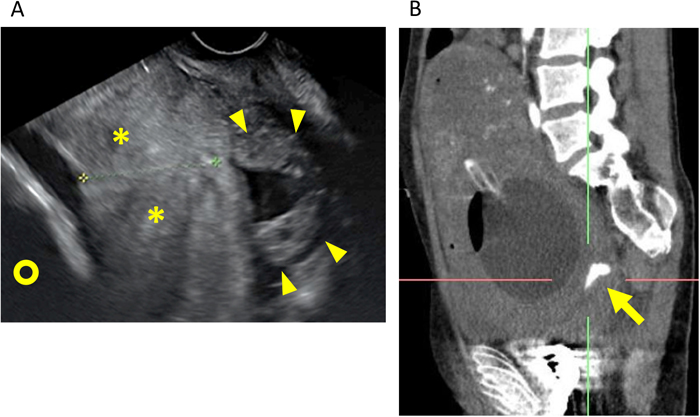
Imaging findings. (A) Transvaginal ultrasound image on admission. A hematoma-like high echoic lesion (*) was observed between the fetal head (circle) and uterine cervix. A low echoic mass of unknown origin (arrowhead) was detected near the internal os of the uterine cervix. (B) Sagittal contrast-enhanced computed tomography image. A bleeding point (arrow) was detected on the lower posterior wall of the uterus.
Mechanical cervical dilation and amniotomy were performed, and blood was allowed to flow out. Labor was induced using oxytocin, but the patient could not achieve effective labor, taking 14 hours to deliver a stillborn male infant and placenta. During labor, massive vaginal hemorrhage continued and worsened after delivery. Contrast-enhanced computed tomography (CT) revealed a bleeding point on the lower posterior wall of the uterus (Figure 1B). Balloon tamponade and uterine artery embolization were attempted but unsuccessful. Eventually, total abdominal hysterectomy was performed. Total blood loss was 29,000 ml, and 108 units of red blood cells, 106 units of fresh frozen plasma, and 125 units of platelet concentrate were transfused. The patient was discharged on postoperative day 10 without sequelae.
No retroplacental hematoma was observed at the time of delivery, and there were no gross or microscopic abnormalities of the placenta and the uterine corpus. However, a solid nodule 5.8 cm in diameter was observed at the posterior wall of the uterine cervix (Figures 2A and 2B). Histologically, the nodule consisted of villous tissue. Pathologically, villous tissue was directly attached to the cervical stroma with no decidua (Figures 2C and 2D), and dilatation of vessels and prominent blood sticking were observed, which were compatible with the source of bleeding, leading to a diagnosis of cervical pregnancy. Fluorescent in situ hybridization for sex chromosome determination revealed that the placenta of the stillborn fetus was male (XY), whereas the cervical villous tissue was female (XX) (Figures 2E and 2F).

Pathological findings. (A and B) Excised uterus. A solid nodule 5.8 cm in diameter (arrowhead) was observed on the posterior wall of the uterine cervix. (C and D) Microscopic findings of the nodule. A few chorionic villi with viable trophoblasts were found in its fibrin deposition, which were directly attached to the cervical stroma with no decidua (arrows). Hematoxylin and eosin-stained sections. Bar: 1 mm in (C) and 500 μm in (D). (E and F) Fluorescent in situ hybridization of villous tissue for sex chromosome determination. The green signal indicates the X chromosome (arrow), and the red signal indicates the Y chromosome (arrowhead). (E) Both X and Y chromosomes were detected in the placenta of the stillborn fetus. (F) Only the X chromosome was detected in cervical villous tissue.
To the best of our knowledge, this is the first report of heterotopic cervical pregnancy in which a very early chemical pregnancy resulted in abrupt IUFD with massive bleeding in the third trimester. Cervical pregnancy was not diagnosed until hysterectomy and histopathological analysis were performed. Interestingly, the ectopic implantation appeared to have stopped growing, and there was no fetus. Nevertheless, the villous tissue was not only viable but also resulted in sudden massive bleeding in the third trimester, thereby inducing placental abruption-like symptoms, IUFD, and a maternal life-or-death crisis.
The precise mechanism underlying sudden bleeding and IUFD in the present case is unknown. Although cervical pregnancy appeared to have been aborted very early, a viable trophoblast was observed later in pregnancy. The pathogenesis of sudden hemorrhage in the present case might be similar to that of post-abortion hemorrhage caused by retained products of conception (RPOC).1) As for fetal death, one plausible explanation is that massive bleeding between the uterine wall and amniotic membrane without vaginal bleeding induced placental abruption-like excessive continuous uterine tone and hypoxia in the intervillous space (Figure 3).
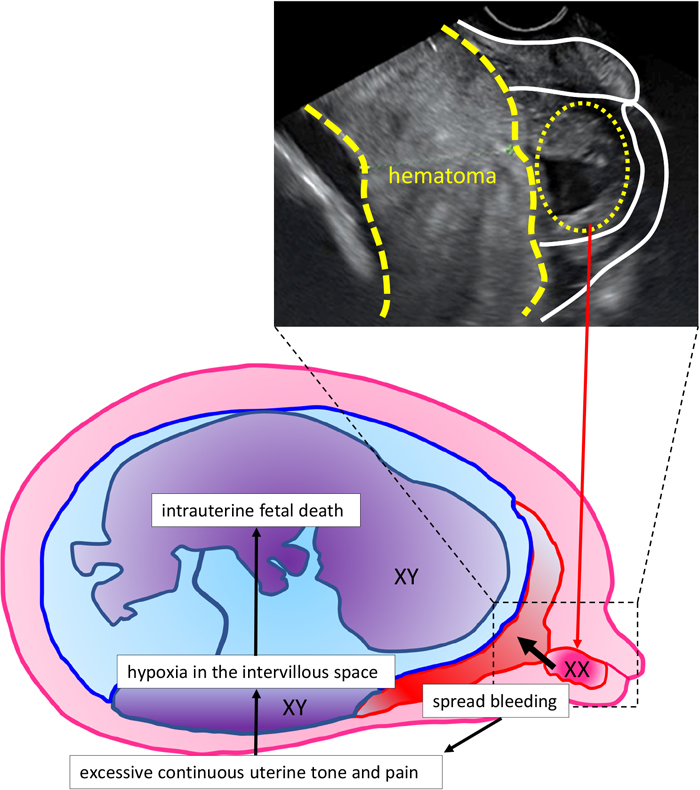
Scheme illustrating the pathogenesis in the present case. Massive bleeding between the uterine wall and amniotic membrane without vaginal bleeding induced placental abruption-like excessive continuous uterine tone and hypoxia in the intervillous space.
Heterotopic cervical pregnancy was not suspected by the referring obstetrician, and it was difficult to identify the cause of massive hemorrhage before delivery. The use of contrast-enhanced CT might have helped determine the exact cause of bleeding during labor attempts. In the case of placental abruption with IUFD, the dead fetus is generally delivered in approximately 5 hours2) with no heavy external bleeding, unlike the present case. Since our patient presented with symptoms resembling placental abruption, vaginal delivery was attempted, but sufficient uterine contraction was not achieved, and massive vaginal bleeding persisted despite adequate doses of uterine contraction agents; these are striking differences from usual placental abruption cases with IUFD. Revision of the management strategy in a timely and appropriate manner may have reduced the amount of bleeding in the present case.
A literature review using PubMed with search terms “heterotopic pregnancy” AND “cervical pregnancy” (October 1, 2020) retrieved 44 cases of heterotopic cervical pregnancy. Of these, only 3 cases had severe bleeding (defined as bleeding that required a transfusion) despite successful treatment of cervical lesions during early pregnancy (Table 1). Gyamfi et al. reported a case of heterotopic pregnancy successfully treated with KCl injection at 6 weeks of gestation, which resulted in emergent cesarean section with a live birth and subsequent hysterectomy due to acute bleeding at 31 weeks of gestation.3) The authors described a brown-green necrotic mass 5 cm in diameter with degenerating chorionic villi, which were retained in the uterine cervix similar to our case. However, vaginal hemorrhage from the outset did not increase intrauterine pressure, and the child therefore survived. In another two cases, heterotopic cervical pregnancies were also successfully treated with KCl injection in the first trimester,4,5) but severe hemorrhage from the cervix ensued after cesarean section. In both cases, bleeding was not observed before cesarean section, and the definitive cause of hemorrhage was unclear. Presumably, however, the 4 cases, including the present case, have the same background, and massive bleeding in the third trimester was attributable to RPOC.
| Authors | Age | Method of conception | Gestational age at diagnosis | Cervical pregnancy | Delivery | Fetal outcome | Circumstances of hemorrhage |
|---|---|---|---|---|---|---|---|
| Gyamfi et al.3) | 34 | IVF-ET | 6 weeks | Local injection of KCl and aspiration | CS due to acute hemorrhage from cervical lesion at 31 weeks | Alive | Acute hemorrhage (3,000 ml) from the cervical region, requiring hysterectomy and 8 units of RBC transfusion. |
| Kumar et al.4) | 32 | Spontaneous | 7 weeks | Local injection of KCl | CS due to impending eclampsia at 35 weeks | Alive | At CS, severe hemorrhage from the cervical canal ensued. Ligation of the anterior division of both internal iliac arteries was performed. |
| Olah et al.5) | 34 | IVF-ET | 12 weeks | Local injection of KCl | CS due to uterine bleeding and non-reassuring fetal heart rate at 36 weeks | Alive | Sudden bleeding occurred when forewaters were ruptured. Hemorrhage occurred from the site of cervical pregnancy and continued after CS, requiring hysterectomy and 24 units of blood transfusion. |
| Present case | 38 | IVF-ET | After delivery | Chemical pregnancy | VD | Dead | The patient presented with severe abdominal pain and IUFD, and labor was induced. Massive vaginal bleeding (29,000 ml) from the cervical mass continued during labor and after delivery, requiring hysterectomy and massive blood transfusion. |
IVF-ET, in vitro fertilization and embryo transfer; KCl, potassium chloride; CS, cesarean section; VD, vaginal delivery; RBC, red blood cell; IUFD, intrauterine fetal death.
In summary, we experienced a case of aborted heterotopic cervical pregnancy that resulted in sudden IUFD due to massive bleeding from the ectopic site at 32 weeks of gestation. Catastrophic massive hemorrhage from the uterine cervix can occur in cases of heterotopic cervical pregnancy, even if the ectopic pregnancy is aborted spontaneously or treated successfully during the first trimester.
This case report received no financial support.
None.
All procedures were performed in accordance with the ethical standards of the responsible committees on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments. Written informed consent was obtained from the patient for publication of this case report and accompanying images. This article does not contain any studies with human subjects performed by any of the authors.