Abstract
We performed a retrospective study of serum zinc levels and blood nutrient indices with malnutrition admitted to our hospital. The association between zinc levels and the onset of pressure ulcer was then investigated. The participants were 243 patients who were not administered zinc supplement as part of the nutrition support team intervention between January 2010 and March 2019. The mean zinc level was 59.7μg/dl, and 66 subjects (27.2%) had pressure ulcers. Significant positive correlations were found between serum zinc level and albumin level, and between serum zinc level and pre-albumin level. The subjects were divided into the following groups according to their serum zinc level: Normal (≥ 80μg/dl), latent zinc deficiency (60 ≤ Zn < 80μg/dl), and zinc deficiency (< 60μg/dl). The zinc deficiency group had significantly lower serum albumin levels and pre-albumin levels. The zinc deficiency group had no difference in the amount of energy intake and protein intake. This suggests that the zinc absorption control mechanism failed for some reason, which makes it difficult for the body to maintain zinc homeostasis, and that this may be related to increased excretion of zinc. Our logistic regression analysis designed to search for factors that cause pressure ulcer led to the extraction of serum zinc level and albumin level as independent factors. There is a high possibility that zinc deficiency and malnutrition are related to the onset of pressure ulcer and increased severity, respectively. We believe that future studies on pressure ulcer treatment should focus on appropriate nutrition management and zinc supplementation.
Introduction
Zinc deficiency has recently become well known in Japan; however, in clinical settings, medical professionals are relatively unfamiliar with zinc deficiency. In cases where hospitalized patients become confined to beds because of malnutrition and illness, reduction in blood nutrient indices and the development of pressure ulcers are sometimes observed. Although sufficient energy and protein supplements are considered effective treatments for pressure ulcers, there is no evidence indicating that zinc supplementation is effective [1, 2].
Zinc is an essential trace element in the body. Since it performs a wide variety of physiological actions, including nucleic acid synthesis, protein metabolism, immune functions, and blood cell differentiation, zinc deficiency causes a variety of complications. Recently, hospitalized patients tend to be increasingly advanced in age, and in cases in which appropriate nutrition management is not carried out for such patients, the resulting complications can have an effect on their vital prognosis and zinc deficiency complication can have an additional negative effect on their vital prognosis [3, 4].
At our hospital, we provide Nutrition Support Team (NST) intervention for hospitalized patients with malnutrition and for those in whom oral food intake is difficult. The NST makes bedside rounds, holds subsequent conferences, and provides feedback to the attending physician. Identifying that a hospitalized patient has zinc deficiency is important for the prevention of complications and to the improvement of the patient’s vital prognosis. At our center, once NST intervention is determined to be necessary, the patient’s serum zinc level and other blood nutrient indices are monitored. We previously reported on the relationship between nutritional indices such as serum zinc levels and pressure ulcers (grade II or higher) in 170 NST intervention, zinc-naïve patients from January 2010 to 2016, and found that factors associated with grade II or higher pressure ulcers were serum zinc levels, albumin levels, and total lymphocyte counts [5]. The results showed that the factors associated with pressure ulcers II and above were serum zinc level, albumin level, and total lymphocyte count. With the accumulation of subsequent cases, the number of cases to be examined was increased and the study was conducted again. In addition, a new item for serum zinc level in the diagnostic criteria for zinc deficiency was published in the Japanese Society of Clinical Nutrition “the Zinc Deficiency Clinical Practice Guidelines 2018” [6] and based on this, we reexamined the nutritional indices by group.
Here, we report on our retrospective study of serum zinc levels and blood tests related to nutrition performed on hospitalized patients who underwent NST intervention at our hospital, and we performed additional examination of how these values are related to pressure ulcers. In addition, we performed a survey of zinc deficiency among patients with malnutrition.
Methods
Although there were 284 patients at our hospital who underwent NST intervention during the 9-year and 3-month study period from January 2010 to March 2019, the subjects of this study were the 243 patients who were not administered the following drugs that can affect serum zinc levels: Polaprezinc® (promac granules or promac OD tablets: Zeria Pharmaceutical Co., Ltd. Tokyo, Japan) and Nobelzin® (Nobelpharma Co., Ltd. Tokuyo, Japan). Blood samples were taken at bedside (early morning, fasting) and the following were investigated: Serum zinc (Zn) level (measured using ACCURAS AUTO Zn: Shino-Test Corporation. Tokyo, Japan), serum albumin (Alb) level, serum pre-albumin (Pre-Alb) level, and total lymphocyte count (TLC). The following data was also obtained: Age, sex, amount of energy intake, amount of protein intake, and pressure ulcers (yes vs. no). Laboratory data were measured before the NST intervention during hospitalization. The actual energy intake and protein intake were consisted of eating meal volume (nurse visually confirmed the eating ratio), enteral nutritional supplement and infusion at the time of NST intervention. Basal energy expenditure was calculated by the Harris-Benedict estimation formula [7] (male: 66.47 + 13.75 × body weight(kg) + 5.0 × height(cm)-6.76 × age(years), female: 655.1 + 9.56 × body weight(kg) + 1.85 × height(cm) - 4.68 × age(years)). Theoretical requirement of energy was calculated by the Long formula [8] (Theoretical requirement of energy = Basal energy expenditure × activity factor × injury factor). The ratio of energy intake to theoretical requirement was defined as energy sufficiency rate. Theoretical requirement of protein was calculated by multiplying the underlying disease, coefficient according to the degree of stress and the ideal body weight based on the enteral nutrition guideline 3rd edition (edited by the Japanese Society for Parenteral and Enteral Nutrition) [9]. The ratio of protein intake to theoretical requirement was defined as protein sufficiency rate. Zinc sufficiency rate was not included in this study because it was difficult to retrospectively estimate the zinc intake in the diet. Statistical analyses were performed as follows: Two-group analysis was done using the student’s t-test and the correlation between serum zinc level and each variable was investigated using Pearson’s product moment correlation coefficient. Three-group analysis was done using One-way ANOVA and chi-square test. If a significant difference was observed after performing One-way ANOVA, the Tukey-Kramer method was performed. Logistic regression analysis was performed in order to identify factors related to pressure ulcers, with the stepwise method used to select the variables. Statistical processing was performed using SPSS Version 22.0 (IBM, Chicago, IL, USA) and Excel Statistics 2015 (SSRI, Tokyo, Japan). Significance was set at p < 0.05.
This study was approved by the Ethics Committee of Saiseikai Wakayama Hospital (No.132,2021). Patients’ consent was obtained using the opt-out method.
Results
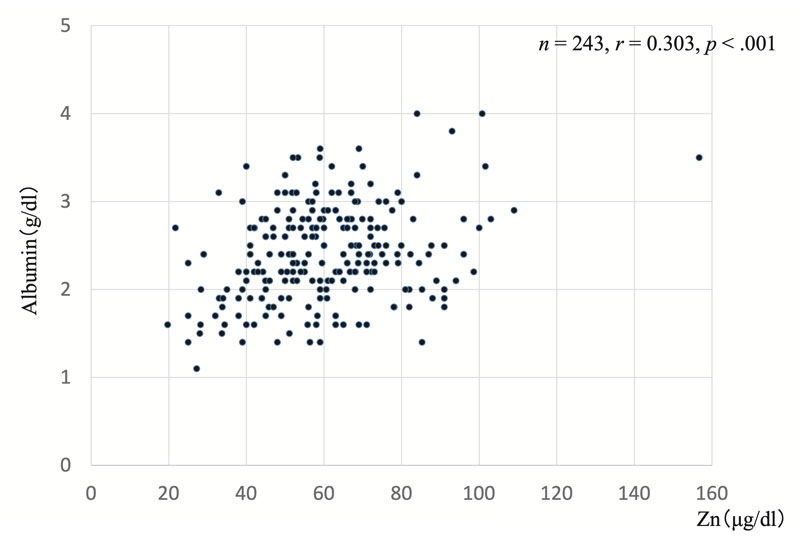
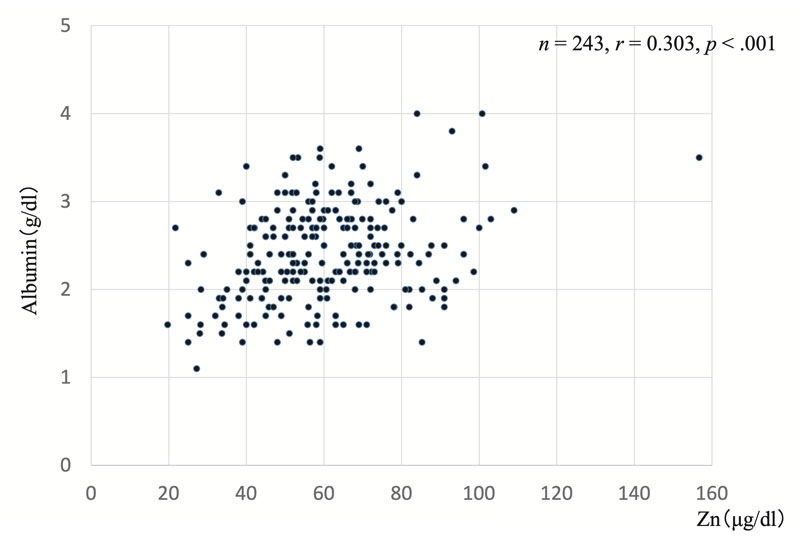
The patients’ background factors are shown in Table 1. There were 243 patients who were not administered either Polaprezinc® or Nobelzin® at the time of NST introduction. Overall, 145 patients were male and 98 were female. The mean age was 79.3 ± 9.6 years; BMI was 18.9 ± 3.8 kg; the energy sufficiency rate was 73.9 ± 0.3%; and protein sufficiency rate was 76.1 ± 0.3%, indicating obvious insufficiency. Pressure ulcers were observed in 66 patients (27.2%). The mean serum zinc level was 59.7 ± 18.3 μg/dl, indicating a low level. Mean serum albumin level was low, at 2.4 ± 0.5 g/dl, and mean serum pre-albumin level (rapid turnover protein) was low, at 12.2 ± 10.6 g/dl. TLC, which is a nutrient indicator that shows a decline in immune function, was 1310 ± 798/mm3. Investigation of the correlation between serum zinc level and age, BMI, serum albumin level, serum pre-albumin level, and TLC showed that there was a significant positive correlation between serum zinc level and serum albumin level (Figure 1; n = 243, p < .001, r = 0.303) and that there was a significant positive correlation between serum zinc level and serum pre-albumin level (Figure 2; n = 243, p < .001, r = 0.318), which suggests that serum zinc level is related to nutritional status and early protein synthesis capacity.
Table 1.
Background factors.
Values are expressed as the mean ± standard deviation. Energy/protein sufficiency rate; the ratio of energy/protein intake to theoretical requirement*. Abbreviations; TLC, total lymphocyte count.
| Number of cases |
243 |
| Age (years old) |
79.3 ± 9.6 |
| Male/Female |
145/98 |
| Body mass index (kg/m2) |
18.9 ± 3.8 |
| Energy intake (kcal/day) |
1093 ± 448 |
| Energy sufficiency rate (%)* |
73.9 ± 0.3 |
| Protein intake (g/day) |
42.5 ± 17.4 |
| Protein sufficiency rate (%)* |
76.1±0.3 |
| Pressure ulcer yes/no (%) |
66/177 (27.2) |
| Zn (μg/dl) |
59.7±18.3 |
| Albumin (g/dl) |
2.4 ± 0.5 |
| Pre-Albumin (g/dl) |
12.2 ± 10.6 |
| TLC (/mm3) |
1310 ± 798 |
Therefore, based on the serum zinc levels indicating zinc deficiency in the zinc deficiency diagnostic guidelines listed in the Zinc Deficiency Clinical Practice Guidelines 2018 [6], published by the Japanese Society of Clinical Nutrition, we divided the patients into the following groups: Normal group (Group A; at least 80 μg/dl: 30 subjects), latent zinc deficiency group (Group B; at least 60 μg/dl but under 80 μg/dl: 81 subjects), and zinc deficiency group (Group C; under 60 μg/dl: 132 subjects). We then examined the relationship between serum zinc level and serum albumin level, serum pre-albumin level, and TLC. As shown in Figure 3, There was a significant difference between serum zinc level and serum albumin level by one-way ANOVA (F (2, 238) = 4.15, p = .0169). The results indicated that compared to Groups B, Group C had significantly lower serum zinc level by Tukey-Kramer method (p = .0456). There was a significant difference between serum zinc level and pre-albumin level by one-way ANOVA (F (2, 239) = 8.04, p < .001). The results indicated that compared to Groups A, Group B and C had significantly lower serum zinc level by Tukey-Kramer method (p = .0475, p < .001, respectively). No significant differences were found between the three groups in terms of age, gender, body mass index, energy intake amount, energy sufficiency rate, protein intake amount, protein sufficiency rate or pressure ulcer yes/no by One-way ANOVA and chi-square test (Table 2). And no significant differences were found between the groups in terms of TLC.
Since the onset of pressure ulcers is problematic for hospitalized patients with malnutrition, we investigated the relationship between serum zinc level and pressure ulcer (yes vs. no). As a result, we found that the non-pressure ulcer group had a serum zinc level of 61.8 ± 18.3 μg/dl and the pressure ulcer group had a serum zinc level of 54.3 ± 17.4 μg/dl, indicating that the pressure ulcer group had significantly lower zinc levels (Figure 4; (t (241) = 2.88, p = .0043). We also performed logistic regression analysis with pressure ulcer (yes vs. no) as the dependent factor and age, sex, serum zinc level, serum albumin level, serum pre-albumin level, and TLC as independent factors in order to identify those factors that can cause pressure ulcers. The results were as follows: Univariate analysis indicated a significant relationship between serum zinc level (hazard ratio 0.98, 95% CI: 0.958-0.992; p = .005) and serum albumin level (hazard ratio 0.45, 95% CI: 0.256-0.799; p = .006) and multivariate analysis that extracted serum zinc level (hazard ratio 0.98, 95% CI: 0.962-0.998; p = .031) and serum albumin level (hazard ratio 0.54, 95% CI: 0.300-0.987; p = .045), indicated that serum zinc level and serum albumin level are independent factors related to the formation of pressure ulcers (Table 3).


Table 2.
Background factors by serum zinc level at the time of NST introduction.
Three-group analysis was done using One-way ANOVA* and chi-square test
†. Values are expressed as the mean ± standard deviation. Energy/protein sufficiency rate, the ratio of energy/protein intake to theoretical requirement. Abbreviations; NST, nutrition support team; BMI, body mass index
|
Group A
Zn ≥ 80 |
Group B
60 ≤ Zn <80 |
Group C
Zn < 60 (μg/dl) |
p value |
| Number of cases |
30 |
81 |
132 |
|
| Age |
75.9 ± 10.1 |
79.8 ± 7.7 |
79.9 ± 10.3 |
p = .1023* |
| Male/Female |
20/10 |
55/26 |
70/62 |
p = .0703† |
| BMI (kg/m2) |
19.1 ± 3.4 |
19.3 ± 3.6 |
18.7 ± 4.0 |
p = .5128* |
| Energy intake (kcal/day) |
1104 ± 392 |
1082 ± 437 |
1084 ± 472 |
p = .9651* |
| Energy sufficiency rate (%) |
73.5 ± 24.7 |
72.3 ± 28.2 |
74.9 ± 32.0 |
p = .8234* |
| Protein intake (g/day) |
39.8 ± 12.8 |
42.3 ± 16.7 |
43.3 ± 18.8 |
p = .6249* |
| Protein sufficiency rate (%) |
67.9 ± 21.2 |
71.3 ± 28.3 |
80.8 ± 39.1 |
p = .0605* |
| Pressure ulcer yes/no (%) |
3/27 (10.0) |
23/58 (23.4) |
40/92 (30.3) |
p = .0748† |

Table 3.
Logistic regression analysis with pressure ulcer (Yes/No ).
Univariate analysis indicated a significant relationship between serum zinc level and serum albumin level.* Multivariate analysis that extracted serum zinc level and serum albumin level.
†
Note. Logistic regression analysis was performed with the stepwise method used to select the variables. Female group was set for the baseline hazard (ratio = 1). Abbreviations; HR, hazard ratio; TLC, total lymphocyte count
|
univariate
HR(95%CI) |
p value |
multivariate
HR(95%CI) |
p value |
| Gender |
Female |
1 |
p = .149 |
|
|
| Male |
1.57 (0.853-2.838) |
| Age |
0.926 (0.972-1.032) |
p = .926 |
|
|
| Zn |
0.98 (0.958-0.992) |
p = .005 * |
0.98 (0.962-0.998) |
p = .031† |
| Albumin |
0.45 (0.256-0.799) |
p = .006 * |
0.54 (0.300-0.987) |
p = .045† |
| Pre-albumin |
0.98 (0.941-1.021) |
p = .336 |
|
|
| TLC |
1.00 (1.000-1.001) |
p = .122 |
|
|
Discussion
Zinc is an essential trace element that performs a wide variety of physiological functions including nucleic acid synthesis, protein metabolism, immune functions, and blood cell differentiation. In our hospital, NST bedside rounds and team conferences attended by the hospital’s staff are performed for hospitalized patients to provide feedback to the attending physician. Patients with malnutrition and particularly pressure sore complication have long been known to have complication of zinc deficiency. At our hospital, once the determination is made to start NST intervention, serum zinc levels are measured and the attending physicians of patients who are not administered zinc supplement are advised to administer oral zinc supplement and nutritional supplements containing zinc actively to their patients. In particular, patients with illnesses, such as malignant tumors who have undergone surgery and underwent anti-cancer drug treatment, cerebrovascular disease, cardiovascular disease, aspiration pneumonia become bedridden and suffer from complication of pressure ulcer; as a result, their treatment is delayed, and this further exacerbates their complications in a vicious cycle. Holding multidisciplinary in-hospital conferences in addition to the care provided by the attending physician is an important way to accurately identify malnutrition and zinc deficiency, and determine menus based on an appropriate nutrition management plan as soon as possible [10].
There were 284 patients at our hospital over the 9-year and 3-month study period, between January 2010 and March 2019, who underwent NST intervention. However, 243 of these patients who were not administered oral zinc supplement and whose serum zinc levels were monitored were the subjects of this study. The mean serum zinc level was low, at 59.7 ± 18.3 μg/dl, and 132 patients (more than half) had a serum zinc level below the cutoff point for zinc deficiency (under 60 μg/dl). The mean energy sufficiency rate at the time of NST intervention (actual energy intake vs. theoretical requirement of energy as calculated using the Harris-Benedict Equation) was 73.9% and the mean protein sufficiency rate (actual protein intake vs. theoretical requirement of protein) was 76.1%, indicating clear insufficiency. These data indicate that there were many cases of NST patients who had insufficient nutritional intake and complication of zinc deficiency. Investigation of the relationship between serum zinc level and various nutrient index parameters showed that there was a significant correlation with serum albumin level and serum pre-albumin level. Additionally, when the subjects were divided into three groups according to their serum zinc level, no inter-group difference was found in the background energy intake amounts or protein intake amounts, but in Group C (zinc deficiency group) serum albumin and serum pre-albumin levels were significantly lower than those of the other groups (serum albumin; group B, serum pre-albumin; group A, respectively). Bate J et al. reported that patients with severely low serum zinc levels have low serum albumin levels and low pre-albumin (a rapid turnover protein) levels, and that zinc deficiency improved rapidly upon zinc supplement administration [11]. In their investigation of the relationship between blood zinc levels and serum albumin levels in 57 patients with chronic viral hepatitis, Takamatsu et al. reported that there was a significant positive correlation between blood zinc levels and serum albumin levels, and discussed the possibility that this may be due to increased urinary excretion of zinc in patients with liver cirrhosis, not for decreased absorption rates from food [12]. About 60 to 70 percent of albumin in the blood bonds weakly with the absorbed zinc, and an increase in the urinary excretion of zinc relates hypoalbuminemia and zinc deficiency can be treated with diuretics which is unrelated to absolute insufficiency in zinc intake [13, 14]. Regarding zinc absorption, Kambe et al. reported that ZIP4 and ZIP5, which are zinc transporters in tissues that are important to the internal storage of zinc (small intestine epithelial cells) are important to zinc homeostasis and for example, in cases of insufficient zinc levels, the amount of ZIP4 that is expressed increases and decomposition is suppressed [15, 16]. If a patient develops malnutrition, the absorption regulation mechanism for ingested zinc fails to function normally, which in turn may cause disruption of the maintenance of zinc homeostasis. We look forward to future research designed to identify the actual mechanism by which clinical administration of zinc is involved in this.
Pressure ulcer onset is an important complication experienced by hospitalized patients with malnutrition. In particular, in cases in which deep ulcers that form pockets occur, it is difficult to elevate serum albumin levels due to the outflow of exudates, which in turn makes it difficult to improve the patient’s nutritional status. In many cases, this becomes the cause of additional ulcer infection. In our investigation of pressure ulcers and zinc, we performed logistic regression analysis in order to identify the factors that cause pressure ulcers. The results showed that serum zinc level and serum albumin level were both independent factors. However, although it is generally considered that protein intake and zinc intake decrease due to a decrease in food intake, it is considered that each deficiency may accelerate the other deficiency. This time, we have not examined the amount of zinc in the meal, and it is not clear, but it is a future examination issue.
Kurasawa et al. reported that even if the elevation of serum albumin level is insufficient, zinc supplement therapy improves pressures ulcers if serum zinc concentration is increased [17]. Furthermore, in the present study we also found that pressure ulcers and zinc deficiency were independently related [5]. Nishida et al. verified that the zinc transporter ZnT2 is the gene responsible for zinc accumulation in the secretion granules of mast cells and that the zinc secreted by mast cells is related to skin wound healing [18]. It has also been shown that the zinc released by mast cells is related to the production of IL-6 during the inflammatory phase of skin ulcer healing [18]. In their study using Zip13 knockout mice, Fukada et al. verified that in skin and other connective tissues Zip13 is the regulatory molecule for the BMP/TGF-β signal pathway [19, 20]. In this way, zinc is thought to play an important role in the healing process of the skin. Hence, we believe that it is important to provide zinc supplements in addition to appropriate nutritional management as part of the treatment of pressure ulcers.
Conclusion
Zinc is an essential trace element in the body. Although clinical physicians have an academic understanding of its importance, in actual clinical practice, appropriate zinc supplement administration is not done, as zinc deficiency is not suspected. In this study, we investigated the relationship of serum zinc level with nutrient index parameters and pressure ulcers in patients who qualify for NST intervention. In spite of the fact that the in-hospital physicians are aware of the existence of NST, few of them administer zinc supplement to their patients. A variety of previous studies reported the possibility that zinc administration to patients with zinc deficiency might improve their nutritional status [21]. Hence, it is necessary to check serum zinc concentration first when examining patients with malnutrition. We look forward to more vigorous activities that will raise awareness regarding zinc in the future. As additional important knowledge regarding zinc and its role in the body is being accumulated, we look forward to an increase in the understanding of zinc deficiency.
Acknowledgments
The authors would like to thank the NST staff at Saiseikai Wakayama Hospital and other hospital staff who provided valuable assistance.
Statements about COI
The authors declare no conflict of interest associated with this manuscript.
References
- [1]
Haesler
E
:
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers:
Quick Reference Guide.
Cambridge Media,
Perth, Australia,
2014.
- [2]
Posthauer
ME
,
Banks
M
,
Dorner
B
,
Schols
JM
:
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. The Role of Nutrition for Pressure Ulcer.
Adv Skin Wound Care,
28:
175-
188,
2015.
- [3]
Miyata
M
:
Clinical zinc deficiency.
Kinpodo,
2009.
- [4]
Pepersack
T
,
Rotsaert
P
,
Benoit
F
,
Willems
D
,
Fuss
M
,
Bourdoux
P
,
Duchateau
J
, et al
:
Prevalence of zinc deficiency and its clinical relevance among hospitalised elderly.
Archger
33:
243-
253,
2001.
- [5]
Kawaguchi
M
,
Yamahara
K
,
Hanabusa
T
, et al
:
Serum zinc levels are relevant to some of nutritional markers and the aggravations of pressure ulcers in patients who had been treated by a nutrition support team.
J Zinc Nutr Therapy
2:
73-
80,
2016.
- [6]
Kodama
H
:
Zinc Deficiency Clinical Practice Guidelines 2018.
Japanese Society of Clinical Nutrition
1-
46,
2018.
- [7]
Harris
JA
,
Benedict
FG
:
A biometric study of human basal metabolism.
Proc Natl Acad Sci USA
4(
12):
370-
373,
1918.
- [8]
Long
CL
,
Schaffel
N
,
Geiger
JW
, et al
:
Metabolic response to injury and illness: estimation of energy and protein needs from indirect calorimetry and nitrogen balance.
JPEN
1979(
3):
452-
456,
1979.
- [9]
Inoue
Y
:
The enteral nutrition guideline 3rd edition (edited by the Japanese Society for Parenteral and Enteral Nutrition).
Shorinsha,
Tokyo,
2013.
- [10]
Higashiguchi
T
:
The usefulness of zinc in nutrition management. Treatmentsupplement: Exploring the usefulness of zinc
18-
24,
2009.
- [11]
Bates
J
,
McClain
CJ
:
The effect of severe zinc deficiency on serum levels of albumin, transferrin, and pre-albumin in man.
Am J Clin Nutri
34:
1655-
1660,
1981.
- [12]
Takamatsu
S
,
Shigemitsu
K
,
Takeda
O
, et al
:
Chronic liver disease and zinc in the elderly.
J Geriatric Gastroenterol
19:
85-
89,
2007.
- [13]
Chiba
M
,
Katayama
K
,
Takeda
R
, et al
:
Diuretics aggravate zinc deficiency in patients with liver cirrhosis by increasing zinc excretion in urine.
Hepatology Research
43(
4):
365-
373,
2012.
- [14]
Katayama
K
:
Zinc metabolism in liver cirrhosis: Diuretics aggravate zinc deficiency.
JJPH
21:
110-
112,
2015.
- [15]
Kambe
T
,
Tsuji
T
,
Hashimoto
A
, et al
:
The physiological, biochemical, and molecular roles of zinc transporters in zinc homeostasis and metabolism.
Physiol Rev
95:
749-
784,
2015.
- [16]
Hashimoto
A
,
Arimoto
S
,
Kambe
T
:
Reciprocal expression regulation of ZIP4 and ZIP5 in intestinal epithelial cells.
Trace Nutrients Research
33:
122-
127,
2016.
- [17]
Kurasawa
R
:
Zinc deficiency: Back ground, clinical features, and treatment:
J Zinc Nutr Therapy
4(
1):
4-
16,
2013.
- [18]
Nishida
K
,
Hasegawa
A
,
Yamasaki
S
, et al
:
Mast cells play role in wound healing through the ZnT2/GPR39/IL-6 axis:
Scientific Reports
9(
1),
2019.
- [19]
Fukada
T
,
Civic
N
,
Furuichi
T
, et al
:
The Zinc Transporter SLC39A13/Zip is required for Connective Tissue Development; Its Involvement in BMP/TGF-β Signaling Pathways.
Plos One
3:
e3642,
2008.
- [20]
Hara
T
,
Takeda
T
,
Takagishi
T
, et al
:
Physiological roles of zinc transport: molecular and genetic importance in zinc homeostasias.
J Physiol Sci (
67):
283-
301,
2017.
- [21]
Kikunaga
S
,
Kosaka
K
:
A variety of previous studies reported the possibility that zinc administration to patients with zinc deficiency might improve their nutritional status.
Trace Nutrients Research
30:
101-
109,
2013.