2020 Volume 20 Issue 1 Pages 1-11
2020 Volume 20 Issue 1 Pages 1-11
This study aimed to clarify the contribution of the dorsal interosseus (DI) muscles to proximal interphalangeal (PIP) joint extension function. Six healthy males were included in the study. PIP joint extension angle and torque were measured upon electrical stimulation of the 2nd and 3rd DI muscles; furthermore, an electromyogram of both muscles during active maximum PIP joint extension was obtained. Six positions were measured between metacarpophalangeal (MP) joint flexion of 80° and hyperextension (MPH) of 20° (MP80, MP60, MP40, MP20, MP0, and MPH20).
The average PIP joint extension angle upon electrical stimulation of the 2nd DI muscle was almost constant within −60° to −70° regardless of MP joint position. Although it was 0° for MP40 and MP20 upon stimulation of the 3rd DI muscle, it was around −30° and −50° for MPH20 and MP80, respectively (p < 0.01). PIP joint extension torque was measured at MP40 and MP20, where full extension was possible, and 0.03 Nm at MP40 and 0.05 Nm at MP20. Muscular activity during finger extension motion by the maximum effort was approximately 30% of the maximum activity at MP40 and approximately 70% at MP80 and MPH20 as a peak value for both muscles (p < 0.01).
This study revealed that the 3rd DI muscle governs PIP joint extension function; its degree of effect is influenced by MP joint position. Moreover, muscular activity in PIP joint extension motion fluctuates with MP joint position, and the muscles are activated at positions where PIP joint extension is not efficiently obtained. This increased activity is caused by suppression of MP joint extension, which increases the PIP joint extension function via the extensor digitorum muscles.
Extension motions of the fingers are performed smoothly by cooperative activity of the finger extension mechanism formed of the extensor digitorum (ED) muscle, interosseous muscles, and lumbrical muscles. Above all, the interosseous and lumbrical muscles, the main components of the intrinsic muscles, extend the proximal interphalangeal (PIP) joints and suppress hyperextension of the metacarpophalangeal (MP) joints of the ED muscle, increasing PIP joint extension function. Since the interosseous muscles have greater physiological cross-sections than those of the lumbrical muscles in particular [1], their role is greater than that of the lumbrical muscles; the authors presume that they are important muscles for the finger extension motion.
The interosseous muscles, consisting of four dorsal interosseous (DI) muscles and three palmar interosseous muscles, insert at the lateral band, interosseous hood, and proximal phalanx base, while the ratios of the insertion sections differ among them. For example, the main fiber of DI muscles involved in the middle finger inserts at the proximal phalanx base for the 2nd DI muscle and the lateral band for the 3rd DI muscle, while the PIP joint extension function of the 2nd DI, which is mainly attached to the proximal phalanx base, is low [2]. However, since an anatomical study revealed the presence of fibers inserted at the lateral band in the 2nd DI muscle [3], it may be involved in the PIP joint extension function to some extent. Nevertheless, few studies have investigated the extension function of each DI muscle; therefore, their details have not been elucidated.
Studies that investigated the PIP joint extension function of the interosseous muscles include an anatomical study using cadavers [4], a study on motion electromyography (EMG) [5], and a study using electrical stimulation [6]. However, in the above anatomical study, joint motion was artificially caused by pulling of the muscle tendon; therefore, the actual motion generated by muscle contraction in vivo was not reproduced. Moreover, in the motion EMG study, the volume of muscular activity did not necessarily reflect range of motion.
In the study of electrical stimulation, the original function of the interosseous muscle can be investigated by independent contracting of the interosseous muscle in vivo. However, muscle contraction by electrical stimulation is caused by constant stimulation of the peripheral nerves and does not necessarily reflect the function in vivo because it does not reflect the descending output from the central nervous system. Therefore, to investigate the DI muscle's PIP joint extension function, it is necessary to confirm the original PIP joint extension function by electrical stimulation of the DI muscle and actually confirm the muscle activity using voluntary movements. In addition, few studies using electrical stimulation have focused on the PIP joint extension force and extension angles due to differences in MP joint position [6].
In this study, we hypothesized that there is a difference in the PIP joint extension function between the 2nd and 3rd DI muscles due to differences in the structures of the insertions; and these polyarticular muscles affected the PIP joint extension function according to the MP joint position. Therefore, the PIP joint extension function of the middle finger was investigated at different MP joint positions by contracting the 2nd and 3rd DI muscles using electrical stimulation. In addition, to confirm the PIP joint extension function of DI muscles in vivo, a motion electromyographic study was also performed.
1. Subject
Six normal adults without a medical history of neuromuscular or orthopedic diseases were included in this study. All were male; mean participant age was 31 years (SD 5.9). All were right-handed. The study was approved by the Ethics Committee of Niigata University of Health and Welfare (Approval No: 17341-120816). The subjects received a written explanation about the study's purpose and method, and each provided written consent prior to participating.
2. Measurement of PIP joint extension angle and torque when the DI muscle is electrically stimulated
1) Electrical stimulation
PIP joint extension angle and torque were measured under the condition of electrical stimulation of the 2nd and 3rd DI muscles of the subjects' right hands. Since the DI muscle can provide more stable electrical stimulation than the palmar interosseous muscle by surface stimulation, the 2nd DI and 3rd DI muscles that constitute the middle finger extension mechanism were used as the target muscles. An electrostimulator (MEB-5500, Neuro Pack Σ; Nihon Kohden, Japan) provided the electrical stimulation using 10-mm plate electrodes (EP-20; Unique Medical, Japan). The electrodes were placed 2 cm apart at the dorsal part of the DI muscles, which most strongly induce the flexion movement of the MP joint of the middle finger and the extension movement of the PIP joint by electrical stimulation. To avoid the influence of the stimulus site differences among MP joint positions, electrode positions were adjusted so that the maximum MP joint flexion force was exerted for each MP joint position. In addition, during electrical stimulation of the DI muscles, palpation and visual examination confirmed that the non-stimulated DI muscles did not contract. The stimulation pulse width of the electrical stimulation, stimulation frequency, and stimulation time were 200 µsec, 20 Hz, and 3 sec, respectively, and the stimulus intensity was set to the supramaximal stimulus. The supramaximal stimulus was 1.1 times the strength at which the maximum MP joint flexion was exerted for each MP joint position. The maximum flexion force was confirmed using the digital force gauge (RZ-100; Aikoh Engineering, Japan). Electrical stimulation was provided five times under each condition for the separate measurements of PIP joint extension angle and torque. Before electrical stimulation, the patient was placed in a relaxed resting position immediately after active flexion, and the values of the electric goniometer and digital force gauge confirmed that no voluntary movement had occurred. The stimulation was delivered in a random order for each condition, and the subjects were given a 1-min break after each electrical stimulation to avoid fatigue. An immobilizing brace made of plastic was used to maintain MP joint and wrist positions during the electrical stimulation (Figure 1).

PIP joint extension angle (a) and extension torque (b) when the 2nd and 3rd DI muscles were electrically stimulated. An electric goniometer for fingers was used to measure PIP joint extension angle, while a digital transducer was used to measure extension torque. The sensor of the digital transducer was set vertically on the dorsal part of the middle phalanx 2.5 cm away from the PIP joint. DI, dorsal interosseous; PIP, proximal interphalangeal.
2) Measurement of PIP joint extension angle
Electrical stimulation was provided separately for the 2nd and 3rd DI muscles during the measurement of PIP joint extension angle. PIP joint extension angle caused by the contraction of each muscle was measured by the electric goniometer for fingers (R-360-C finger; Tiger Medical Instruments, Japan). The measurements were performed in the forearm pronation position and wrist joint intermediary position. Flexed positions of 80°, 60°, 40°, 20°, and 0° and hyperextended positions of 20° at 0° of adduction and abduction were used; thus, a total of six positions were employed for MP joint. Electric goniometer signals were A/D-converted at a sampling frequency of 1 kHz and recorded on a personal computer; these signals were processed with a band-pass filter at 20–500 Hz.
3) Measurement of PIP joint extension torque
PIP joint extension force was measured with the forearm and wrist in the pronation and intermediary positions the same as the PIP joint extension angle. In the MP joint position, the extension force cannot be measured in a position in which the PIP joint cannot be fully extended. Therefore, MP20 and MP40 were employed, in which full PIP joint extension was possible by electrical stimulation of the 3rd DI muscle. The PIP joint was flexed at 10°. Electrical stimulation was provided to the 2nd and 3rd DI muscles simultaneously to balance MP joint adduction and abduction. For measurement of extension force, the digital force gauge mentioned before was set vertically on the dorsal part of the middle phalanx 2.5 cm away from the PIP joint. The acquired extension force signals were A/D-converted at a sampling frequency of 1 kHz and recorded on a personal computer; these signals were processed with a band-pass filter at 20–500 Hz. After that, extension torque was obtained by multiplying it by 0.025 as an external moment arm.
3. Measurement of muscular activity at PIP joint extension movement
The EMG was derived from the 2nd and 3rd DI muscles of the right hand, with bipolar pasting wire electrodes made of stainless wire 0.05 mm in diameter coated with rigid urethane (TN204-123; Unique Medical, Tokyo, Japan). The measurements were performed with the forearm in pronation and wrist joint in the intermediary and flexed positions of 80°, 60°, 40°, 20°, and 0° and a hyperextended position of 20°; thus, a total six positions were employed for the MP joint, same as measurements of PIP joint extension angle induced by electrical stimulation. The motion task was the active maximum extension of the PIP and distal interphalangeal (DIP) joints of the middle finger. The subjects were instructed to extend only the PIP and DIP joints of their middle finger in the immobilizing brace; furthermore, they were instructed not to consciously move the MP joint and other fingers. Moreover, to normalize the EMG obtained by each motion, EMG during the active maximum flexion movement of the MP joint at 60° flexed position was also measured. The MP joint flexion angle was set at 60° since preliminary experiments confirmed that muscle activity was greatest at the MP joint flexion of 60°. The duration of muscle contraction for each motion task was approximately 3 sec; each task was performed three times. EMG signals derived from the wire electrodes were A/D-converted with the sampling frequency of 2 kHz and recorded on a personal computer. A data acquisition and analysis system (PowerLab 8/35; AD Instruments, Australia) was used for the above processing. The recorded EMG signals were processed with a band-pass filter at 20–1000 Hz.
4. Data analysis and statistics
For PIP joint extension torque and angle, average values among the subjects for every MP joint position were obtained by calculating the average values of five measurements for each subject. For the electromyography (EMG) analysis, all wave signals in 1-sec intervals from the 3-sec EMG signals were rectified and an integrated EMG (IEMG) was calculated. Data acquisition and analysis system software (LabChart 8; AD Instruments, Australia) was used for the data analysis. The calculated IEMG values were normalized with the IEMG values of active maximum flexion movement of the MP joint as a standard (normalized IEMG [NIEMG]), and the average NIEMG values of three measurements were calculated for each subject. Next, the average NIEMG values among subjects for every MP joint position were calculated.
For statistical processing, prior to the test, the Shapiro-Wilk test was used to confirm that each variable followed a normal distribution. The subjects' average PIP joint extension torque values were compared for MP joint position using the paired t-test. Moreover, regarding PIP joint extension angle and NIEMG, subjects' average values were compared with muscle and MP joint position as factors by the two-way repeated measures analysis of variance. As a retrospective test, the factors of muscle and the MP joint position were analyzed using the paired t-test and Turkey's multiple comparison test, respectively, with the significance level < 5% for both. SPSS Statistics ver. 18 (SPSS Japan Inc, an IBM company, Japan) was used for the above processing.
1. PIP joint extension angle and torque upon electrical stimulation of DI muscles
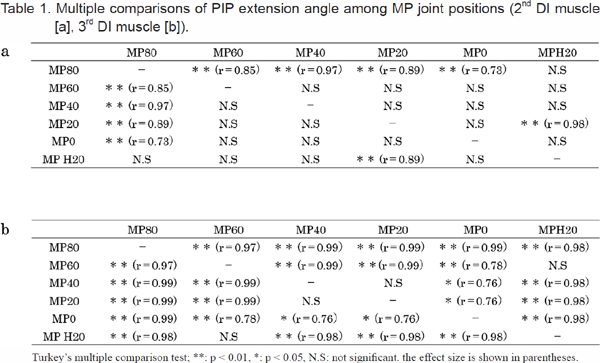
The range of the electric stimulus intensity in this study was 16.1–18.7mA (SD 0.4–0.9). The main effect of muscle and MP joint position on PIP joint extension angle of by electrical stimulation was significant (muscle: F (1,5) = 197.9, p < 0.01, η2 = 0.76; MP joint position: F (5,25) = 108.0, p < 0.01, η2 = 0.18). In addition, interaction was seen between muscle and MP joint position, while significant differences were seen in changing patterns of extension angle accompanied by differences in MP joint position between the 2nd and 3rd DI muscles (F (5,25) = 21.7, p < 0.01, η2 = 0.05). Mean PIP joint extension angle due to contraction of the 2nd DI muscle were −73.7° (SD 2.3), −61.2° (SD 4.9), −59.8° (SD 7.4), −57.2° (SD 6.2), −59.8° (SD 8.1), and −67.0° (SD 7.7) for MP80, MP60, MP40, MP20, MP0, and MPH20, respectively. Multiple comparisons of MP joint positions revealed no differences among MP0, MP20, MP40, and MP60; full extension was impossible at any position. The extension angles of MPH20 and MP80 presented more significant decreases than those of other positions, while extension motion rarely occurred at MP80 in particular (p < 0.01) (Figure 2, Table 1a). Mean PIP joint extension angles due to contraction of the 3rd DI muscle were −47.5° (SD 7.2), −19.8° (SD 3.1), 0° (SD 0), 0° (SD 0), −8.7° (SD 8.1), and −27.5° (SD 6.5) for MP80, MP60, MP40, MP20, MP0, and MPH20, respectively. Comparison with the 2nd DI muscle revealed a significantly higher PIP joint extension angle in the 3rd DI muscle for either position (p < 0.01) (Figure 2, Table 2). Multiple comparisons among MP joint positions presented full extension at MP20 and MP40; on the other hand, it presented significantly greater decreases for MPH20 and MP80 than those for other positions (p < 0.01) (Figure 2, Table 1b). Figure 3 shows PIP joint extension under electrical stimulation of the DI muscles of the representative subject. PIP joint extension torque with electrical stimulation to the 2nd and 3rd DI muscles was 0.05 Nm and 0.03 Nm for MP20 and MP40, respectively. Extension torque presented significantly greater values for MP20 (t (5) = 7.74, p < 0.01, r = 0.96) (Figure 4).



Upon electrical stimulation of the 2nd DI muscle, full extension of the PIP joint was not seen at either MP joint position (upper). Upon electrical stimulation of the 3rd DI muscle, full extension was seen at MP40 but not at MP80 or MP20 (lower). In this representative example, the electric goniometer and force gauge were removed to increase visibility. 2nd DI muscle, second dorsal interosseous muscle; 3rd DI muscle, third dorsal interosseous muscle; MP80, MP joint at 80° flexed position; MP40, MP joint at 40° flexed position; MPH20, MP joint at 20° hyperextended position; PIP, proximal interphalangeal.

2. Muscular activity of PIP joint extension motion
NIEMG during the maximal extension movement of the PIP and DIP joints had no main effect on the muscles but a significant main effect on MP joint position (muscle: F (1,5) = 0.85, p = 0.85, η2 = 0.76; MP joint position: F (5,25) = 75.8, p < 0.01, η2 = 0.92). In addition, no interaction was seen between muscle and MP joint position, and changing patterns of NIEMG accompanied by changes in MP joint position were similar in the 2nd and 3rd DI muscles (F (5,25) = 0.18, p = 0.97). Average NIEMG values of the 2nd DI muscle were 68.4% (SD 13.0), 44.7% (SD 16.0), 27.1% (SD 5.3), 38.3% (SD 13.7), 54.2% (SD 12.3), and 65.9% (SD 10.7) for MP80, MP60, MP40, MP20, MP0, and MPH20, respectively. Mean NIEMG values of the 3rd DI muscle were 70.3% (SD 8.8), 48.2% (SD 5.3), 30.4% (SD 10.5), 44.2% (SD 7.0), 58.3% (SD 5.1), and 71.4% (SD 4.5), respectively. Multiple comparisons of NIEMG among MP joint positions revealed that it was approximately 70%, the highest, at MPH20 and MP80 for both muscles and approximately 30%, the minimum, at MP40 (p < 0.01) (Figure 5, Table 3).


1. PIP joint extension angle and torque under electrical stimulation of DI muscles
In this study, the authors investigated the influence of MP joint position on PIP joint extension function of the DI muscles. As a result, the PIP joint minimally extended when the 2nd DI muscle was stimulated, but the PIP joint could completely extend when the 3rd DI muscle was stimulated. However, the extension function was greatly affected by MP joint position, and the function decreased when the MP joint was hyperextended and in the strong flexed position.
Although the presence of lateral band fibers involved in the extension function of the PIP joint was anatomically confirmed in the 2nd DI muscle, only a slight extension movement occurred during the maximum electrical stimulation in this study. These results suggested the presence of only a few transition fibers or that their structures were weak and they were not capable of transmitting power that could sufficiently extend the PIP joint.
Regarding the result that PIP joint extension function of the 3rd DI muscle differed among MP joint positions, the cause differed between MP joint hyperextension and a strong flexed position. Factors related to MP joint hyperextension included an increased resistance due to tension of the palmar tissue such as the finger flexor muscles against extension force of the 3rd DI muscle for the PIP joint [4] or limited muscle contraction amplitude beyond a certain DI muscle by fixing of the MP joint in the hyperextended position; we suppose that the latter is the major cause. For the latter cause, we presume that fibers causing strong flexion action of the MP joint run on the palmar side of the axis of flexion-extension of the MP joint on the 3rd DI muscle and inserts in the proximal phalanx base; most of the tension from the 3rd DI muscle was conveyed by these fibers, which limited the muscle contraction amplitude at the hyperextension position and, therefore, limited the tension transmitted to the fibers shifting to the lateral band. Conventionally, it was believed that the PIP joint extension function would increase as a result of DI muscle extension for the MP joint extension position [4,6]. However, this theory is denied by the above theory. With increased MP joint flexion, a shortened 3rd DI muscle length and decreased tension with an increased MP joint flexion angle were considered factors contributing to the decreased extension function. Other factors included the assumption that, with an increased MP joint flexion angle, the traction force caused by contraction of 3rd DI was transmitted only to the MP joint flexion and little tension was transmitted to the lateral band fibers [4].
Full PIP joint extension was achieved at MP20 and MP40; its factors included the fact that the contractive force was effectively transmitted to the lateral band directionally without contraction of the 3rd DI muscle being blocked at these positions, while the optimal length of the 3rd DI muscle was maintained. Moreover, judging from the result of this study that PIP extension torque increased more at MP20 than at MP40, since the extension moment arm of a PIP joint was not varied by MP joint position, MP20 is a position that allows more effective transmission of contractive force of the 3rd DI muscle to the lateral band and maintains the optimal length of the 3rd DI muscle.
2. Muscular activity of PIP joint extension motion
High activity was seen for both the 2nd and 3rd DI muscles during MP joint hyperextension and high flexion; the lowest activity was seen at MP40. This result opposes PIP joint extension function with electrically stimulated 3rd DI muscle, indicating that DI muscles are active when PIP joint extension is insufficient. We presume that this activity increases PIP joint extension function via the ED muscle. In other words, when the 3rd DI muscle was electrically stimulated, full PIP joint extension could not be achieved in the more flexed and hyperextended MP joint positions; therefore, PIP joint extension at these positions may be performed mainly by the ED. Therefore, DI muscles prevent MP joint extension caused by ED and increases the PIP joint extension function.
3. Clinical application of study results
The data presented in this study can be referenced in cases in which reconstruction of the central slip or resection of lateral band cannot be avoided. It is recommended that the 3rd DI muscle, which has a strong PIP joint extension force, be selected for reconstruction of the central slip [7,8] versus the 2nd DI muscle for resection of the lateral band. Moreover, for postoperative therapy in cases of proximal phalanx fracture or extensor tendon injury of the proximal phalanx, PIP joint extension at MP40 is recommended to improve gliding performance to prevent adhesion of the lateral band and training at MP20, at which the extension force is further increased, for improving gliding performance in cases of adhesion of the lateral band.
4. Study limitations
This study has several limitations. First, the lumbrical muscle on the palmar side of the 2nd DI muscle or the adjacent interosseous muscles might have been inadvertently stimulated. However, since PIP joint extension motion was stimulated only a little under the electrical stimulation of the 2nd DI muscle, we presume that its influence was not significant. Thus, it will be necessary to stimulate it with wire electrodes or needle electrodes in the future. Moreover, although we investigated the extension function of the middle finger in this study, there exist individual differences in the insertion of the 2nd DI muscle [2,3]; as other fingers have interosseous muscles, the presents result may not be applicable to all fingers. To further investigate the function of the interosseous muscles on PIP joint extension, it will be necessary to increase the number of subjects and investigate the functions of other interosseous muscles.
This study investigated the PIP joint extension function of the 2nd and 3rd DI muscles for the purpose of clarifying the kinematic characteristics of DI muscles. As a result, we confirmed that the 2nd DI muscle does not have a PIP joint extension function, whereas the 3rd DI muscle does. Moreover, the PIP joint extension function of the 3rd DI muscle was influenced by MP joint position. DI muscle activity during PIP joint extension varied among MP joint positions for both muscles and was high at those positions at which PIP joint extension was not efficiently achieved. The authors considered that this increased activity suppresses MP joint extension and that the ED muscle increases PIP joint extension function.
We thank Dr. T. Nara and Dr. T. Soma for helpful comments on the manuscript. This work was supported by a Grant-in-Aid for Scientific Research of Graduate Students of Niigata University of Health and Welfare, Grant Number H24F05. We would like to thank Editage (www.editage.com) for English language editing.