2022 Volume 22 Issue 1 Pages 41-50
2022 Volume 22 Issue 1 Pages 41-50
This study examined the usefulness of the lasso procedure, a reconstructive operation that uses the flexor digitorum superficialis muscle (FDS) as the donor muscle, for treating the claw hand deformation caused by paralysis of the intrinsic muscles. The subjects were 10 healthy adults, electromyograms for which were derived using wire electrodes attached to the FDS, with the ulnar flexor digitorum profundus (FDP), 4th dorsal interosseous muscle, and 2nd palmar interosseous muscle used as comparisons. For the exercise tasks used to derive the electromyography (EMG), the subjects completed a metacarpophalangeal (MP) joint exercise task with the proximal interphalangeal (PIP) joint held in the extended position and two gripping tasks. The FDS showed high activity during MP joint flexion and adduction (p < 0.001). In the cylindrical grasp task, the FDP was active and the intrinsic muscle was dominant. In the intrinsic muscle grasp task, the FDS showed high activity and the interosseous muscle was active. Considering that the lasso procedure can reconstruct the intrinsic muscle, the FDS is active in synchronization with the intrinsic muscles, especially the palmar interosseous muscle. Therefore, the lasso procedure using the FDS requires less training for postoperative functional transformation and is a valid reconstruction method for treating the claw hand deformation.
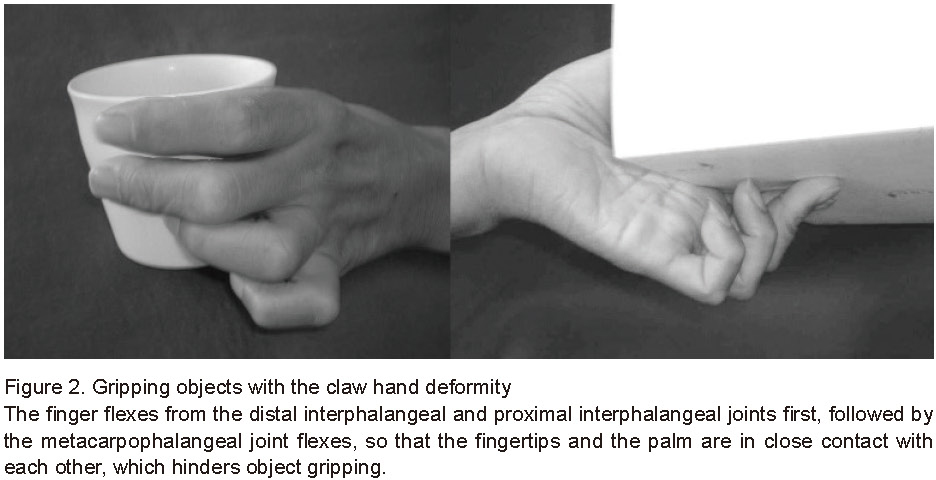
Movement disorders due to ulnar nerve palsy include flaccid paralysis and muscular atrophy of the controlling muscles such as the interosseous and lumbrical muscles (Figure 1). The resulting deformity is called the claw hand deformity or intrinsic muscle minus hand. In this deformity, the metacarpophalangeal (MP) joint is in the hyperextended position when the finger is extended, while the distal interphalangeal (DIP) joint and the proximal interphalangeal (PIP) joint cannot be extended in the flexed position [1]. In addition, when the patient flexes the finger, it flexes first from the DIP and PIP joints and then from the MP joint, so the fingertips and the palm are in close contact with each other, preventing the grasping of a large object [2]. Specifically, it is difficult for an affected individual to grip an object using an intrinsic muscle-dominant gripping form such as holding a cup (Figure 2). Therefore, in addition to the shaping problem, this deformity complicates many delicate movements used to manipulate objects and perform other activities of daily living.
The lasso procedure is a surgical procedure used to correct and functionally reconstruct this deformity reported by Zancolli [3]. This is a muscle-tendon transfer surgery that uses the flexor digitorum superficialis muscle (FDS) as the donor muscle. The procedure involves dissecting the FDS at the stop, folding the distal end of the FDS tendon at the distal end of the A1 ligamentous tendon sheath, and re-sewing it onto the palmar area of the ligamentous tendon sheath. The kinematic mechanism of deformation correction by this method is that the muscle tension of the FDS suppresses hyperextension of the MP joint and keeps it in the flexion position; thus, the PIP and DIP joints are extended only by the muscle contraction force of the extensor digitorum muscle. This mechanism was accepted by many clinicians. Omer proposed an evolution of the procedure in which the FDS was sewn onto the A2 ligamentous tendon sheath to effectively flex the MP joint [4]. Muzykewicz et al. conducted a kinematic comparative study on the gripping characteristics of two reconstructive surgical methods for intrinsic muscle paralysis using a cadaver hand and reported that the lasso procedure results in IP joint followed by MP joint flexion, while the House method results in MP joint followed by IP joint flexion [5]. However, regardless of which procedure is performed, the key to improving performance is not the dynamic tenodesis effect, but rather the voluntary contraction of the transferred FDS when extending the finger or grasping the object. However, most reports on the treatment using the lasso method have been limited to postoperative evaluation of motor functions, such as joint range of motion, grip strength, pinch strength, etc., and have not described the role of the donor muscle and FDS in these results.
Since the lasso procedure is a method that flexes the MP joint using the muscle tone of the FDS and reconstructs extension of the PIP and DIP joints, it can be said to reconstruct the interosseous muscle. The FDS is originally the flexor muscle of the PIP joint, but if it is modified to contract in synchronization with the interosseous muscle, the PIP and DIP joints can easily be extended. However, it has not been clarified to date to what extent FDS is active in MP joint flexion with PIP joint extension, that is, movements in which the interosseous muscle is active.
Therefore, to examine the usefulness of the lasso procedure, this study aimed to electromyographically clarify the activity characteristics of the FDS during MP joint exercises while maintaining the PIP joint extension position. In addition to the interosseous muscle, which is expected to be related as a synergistic muscle, the flexor digitorum profundus (FDP), the same finger flexor muscle as the FDS, was investigated for muscle activity and its relationship with the FDS.

1. Subjects
The subjects were 10 healthy adults with no history of neuromuscular disease or orthopedic disease. The subjects were all right-handed men with an average age of 35.9 ± 9.4 years. This study was approved by the Institutional Review Board of Niigata University of Health and Welfare (approval number 18301-191119). The study purpose and method were explained to the subjects in advance, and each provided informed consent.
2. Exercise tasks
Two types of exercise tasks were performed: MP joint movement of the ring finger (Task A) and a gripping task (Task B). Both tasks were performed with the subjects sitting in a chair with the shoulder joint abducted 10°, the elbow joint flexed at 90°, and the forearm in the middle position. Task A consisted of four movements of isometric maximum automatic flexion, extension, adduction, and abduction of the MP joint. All subjects were instructed to continue for 5 s while maintaining the automatic extension position of the PIP and DIP joints (Figure 3). Regarding MP joint limb position, the flexion movement was set to 40° with reference to the resting limb position after the lasso procedure described by Muzykewicz et al. [5]. The wrist joint was fixed in the middle position by a splint. In Task B, a cylinder with a 6-cm diameter was gripped in two ways and the gripping force was set as a linear ramp load task from 0 to the maximum. There are two types of gripping patterns: a cylindrical grasp (grasping that starts movement from DIP and PIP joint flexion) and an intrinsic muscle grasp (grasping performed by flexing the MP joint in the DIP and PIP joint automatic extension position) (Figure 4). In the linear ramp load task, the subject was instructed to exert the maximum gripping force in 5 s while following the tension straight line written on the monitor. Finally, we added the maximum voluntary contraction task for each muscle to show the relative percentage of maximum muscle activity. All exercise tasks were performed 3 times each, with a 2-min rest between exercise to avoid the effects of muscle fatigue and the orders randomized.


3. EMG derivation
In addition to the FDS of the right ring finger and the ulnar FDP, the 4th dorsal interosseus muscle (4th DI) and 2nd palmar interosseus muscle (2nd PI) were selected as the representative intrinsic muscle. A bipolar bonded wire electrode (non-insulated part: 1 mm; inter-electrode distance: 3 mm) made of a stainless wire (TN204-123; Unique Medical, Tokyo, Japan) with an 0.05-mm diameter coated with hard urethane was used to derive the EMG of these streaks (Figure 5). The electrode was inserted using a 60-mm-long cathelin needle (25G) as a guide and confirmed by ultrasonic images taken by an ultrasound machine (LOGIQ e, GE Healthcare, Tokyo, Japan). The unrelated electrode was inserted into the head of the elbow. After insertion, only the guide needle was removed and the electrode was placed. After the electrodes were placed in each muscle, electrical stimulation was delivered using the placed bipolar wire electrode. It was then confirmed that single flexion of the PIP joint and the FDS of the ring finger were simultaneously flexed; the MP, PIP, and DIP joints of the middle, ring, and little fingers were simultaneously flexed in the ulnar FDP; and the ring finger was abducted and adducted in the 4th DI and 2nd PI, respectively. We also confirmed a lack of cross-talk for each muscle.

4. Data analysis
The obtained EMG signals of each muscle were amplified 100 times by an amplifier (FA-DL-140, 4 Assist, Tokyo, Japan), A/D-converted at a sampling frequency of 2000 Hz through an analog output box (FA-DL-720, 4 Assist, Tokyo, Japan), and captured in a personal computer using a data recording and analyzing system (Power Lab 8/35; AD Instrument, Australia). The recorded EMG signal was processed by a 20-1000-Hz band pass filter and full-wave rectified. After that, in Task A, the integrated electromyogram (IEMG) in the 500-msec section before the point at which the maximum tension was obtained was calculated from the full-wave rectified waveform. In Task B, a linear loading task was calculated using IEMGs for 500-msec intervals at 20% intervals to examine how each muscle was activated in response to the exerted grasp force. Each calculated IEMG value was then normalized by the IEMG value for 500 msec in the maximum voluntary contraction task (normalized IEMG [NIEMG]). Next, the mean NIEMG value was calculated for each subject and the mean value and standard deviation between subjects were calculated.
5. Statistical processing
Prior to the statistical analysis, the normality of each data point was confirmed by the Shapiro-Wilk test. In Task A, repeated-measures analysis of variance (ANOVA) with MP joint motion as a factor were performed for each muscle. We also compared NIEMG between MP joint motions using Bonferroni multiple comparison as a post-test. In Task B, repeated-measures ANOVA was performed with the gripping morphology (cylindrical grasp, intrinsic muscle grasp) for each muscle and the gripping force at 20% intervals (20%, 40%, 60%, 80%, 100%) as two factors. For those who showed the main effect, Bonferroni multiple comparison was used as a post-test, and the NIEMG were compared between gripping forms. The significance level was set to less than 5%, and SPSS software (SPSS statistics version 28.0.1; SPSS Japan Inc., an IBM Company, Japan) was used for the statistical processing.
1. Task A: MP joint movement task (Figure 6)
The mean subject-to-subject NIEMG for Task A was 56.7 ± 15.8% for MP joint flexion, 2.4 ± 1.0% for extension, 36.9 ± 12.9% for adduction, and 5.8 ± 4.2% for abduction in FDS. A significant difference was observed between MP joint movements (F (3,27) = 60.965, P <0.001, ηp2 = 0.871), and flexion and adduction movements were significantly higher than extension and abduction movements (flexion: P < 0.001, P < 0.001; adduction: P < 0.001, P < 0.001). In FDP, all exercises were less than about 10%; however, a significant difference was observed between MP joint movements (F (3,27) = 8.149, P < 0.001, ηp2 = 0.475), while adduction movement was significantly higher than extension movement (P < 0.05). In 4th DI, a significant difference was observed between MP joint movements (F (3,27) = 40.398, P < 0.001, ηp2 = 0.818), and abduction movements were significantly higher than extension, adduction, and flexion movements, while flexion movements were significantly higher than extension and adduction movements (abduction: P < 0.001, P < 0.001, P < 0.01; flexion: P < 0.05, P < 0.05). A significant difference was also observed between MP joint movements in the 2nd PI (F (3,27) = 14.153, P < 0.001, ηp2 = 0.611), and both adduction and flexion movements were significantly higher than extension and abduction movements (adduction: P < 0.01, P < 0.05; flexion: P < 0.05, P < 0.05).

2. Task B: Gripping task (Figure 7)
Regarding NIEMG in Task B, FDS increased significantly with increasing gripping force (F (4,36) = 66.399, P < 0.001, ηp2 = 0.881), but no significant difference was noted due to the difference in gripping morphology (F (1,9) = 0.689, P = 0.428, ηp2 = 0.071). No interaction was observed (F (4,36) = 0.037, P = 0.997, ηp2 = 0.004). In FDP, in addition to being significantly different due to the difference in gripping force (F (4,36) = 60.263, P < 0.001, ηp2 = 0.870), it was significantly different due to the difference in gripping form (F (1,9) = 162.064, P < 0.001, ηp2 = 0.947), and all gripping forces were significantly higher in the cylindrical versus intrinsic muscle grasp (P < 0.001). Interactions were also observed (F (4,36) = 23.172, P < 0.001, ηp2 = 0.720). In the 4th DI, it increased significantly as gripping force increased (F (4,36) = 27.024, P < 0.001, ηp2 = 0.75). There was also a significant difference in gripping morphology (F (1,9) = 22.313, P < 0.001, ηp2 = 0.713), which was significantly higher in the intrinsic versus cylindrical grasp (40%: P < 0.05; 60%: P < 0.001; 80%: P < 0.001; 100%: P < 0.01). Interactions were also observed (F (4,36) = 725.043, P < 0.001, ηp2 = 0.545). Similarly, in the 2nd PI, it increased significantly as gripping force increased (F (4,36) = 31.231, P < 0.001, ηp2 = 0.776). There was also a significant difference in grip morphology (F (1,9) = 93.179, P < 0.001, ηp2 = 0.912), which was significantly higher in the intrinsic versus cylindrical grasp (P < 0.001). Interactions were also observed (F (4,36) = 16.841, P < 0.001, ηp2 = 0.652).

To achieve good hand function after muscle-tendon transfer surgery, it is important to select an effective donor muscle. When the synergistic muscle, that is, the muscle that works in synchronization with the reconstructing muscle, is used as the donor muscle, effective function can be restored. On the other hand, like the Boys method [6], which reconstructs finger extension, when transferring the FDS tendon, an antagonistic muscle, to the extensor digitorum superficialis, it is difficult to voluntarily contract the FDS when the finger is extended, while the function must be acquired using the dynamic tenodesis effect. Alternatively, a special muscle re-education training program is required to convert motor function postoperatively. In either case, activities of daily living that utilize the hands will be poor and difficult to improve. Considering these facts, the lasso procedure described in this study can acquire MP joint flexion function during PIP joint extension by using FDS as a donor muscle or, in other words, reconstruct the intrinsic muscle using the FDS. Therefore, it is desirable that the FDS and intrinsic muscle be synergistic. Therefore, here we examined whether the FDS and the intrinsic muscles are synergistic by using an electromyographic method. We found that the FDS tended to show 57% and 37% of its maximum activity during flexion and adduction movements of the MP joint, respectively, even when the PIP joint was voluntarily extended with high activity during movements that increased the excitability of the 2nd PI. This suggested that the FDS was a co-muscle with the palmar interosseous muscle involved in the MP joint movements. In the grasping task, the FDP was significantly higher in the cylindrical grasp, and the 2nd PI and 4th DI were significantly higher in the intrinsic muscle grasp, indicating that these activities increased linearly with the increasing grasp force. In contrast, the FDS increased linearly to approximately 60%, with the increasing grasp force in both cylindrical and intrinsic muscle grasp movements. The FDS was considered an active muscle with the FDP during the cylindrical grasp and with the 2nd PI and 4th DI during the intrinsic muscle grasp. This suggests that the FDS is active in synchrony with the interosseous muscles of the hand in daily activities, including MP flexion and adduction (Figure 8), and that the FDS is a synergistic muscle with the interosseous muscles, especially the palmar interosseous muscles. We concluded that the use of the FDS as a donor muscle in the lasso technique was highly effective.
We also demonstrated that MP joint flexion and adduction is also effective for FDS muscle contraction training. However, the activity mode and amount of muscle activity change as muscle length increases [7]. The factors include changes in muscle length, joint limb position, moment arm, etc. In addition to the postoperative change in the muscle length of the FDS in the lasso technique, the FDS is an extrinsic muscle, and its activity can change depending on the wrist and forearm limb positions. However, the characteristics of the FDS to be active in synchronization with the interosseous muscles remain even after surgery on the ulnar nerve-paralyzed hand, and the FDS is sutured with increased tension during surgery. To further improve performance, we considered it necessary to acquire FDS activity regardless of the wrist or forearm position using muscle reeducation. On the other hand, the FDP, which is the same as the finger flexor muscle, was less active in both MP joint movements when the DIP and PIP joints were held in the extended position, and it was about 10% of the most active adduction movement. In the intrinsic muscle grasping task, FDP activity was extremely low compared to FDS activity. Therefore, unlike the FDS, the FDP does not work in synchronization with the interosseous muscle, an intrinsic muscle.
From a clinical point of view, the FDS has been widely used in various motor function reconstruction procedures ranging from cases of motor nerve palsy due to peripheral nerve injury to cases of subcutaneous rupture of the tendon of flexor pollicis longus and the FDP and cases of crushed muscle tendons. This is probably because the FDS has many advantages as a donor muscle during muscle-tendon transfer surgery such as contractile force, stretching distance, and independent contraction [8]. The lasso procedure is also a surgical procedure that uses the FDS as a donor muscle and a popular reconstructive operation for treating intrinsic muscle minus hand. Twenty clinical treatments using the lasso procedure corrected the deformity and improved the ball gripping form, grip force, and pinch force [9]. Inferring from the results of this study, this clinical result was contributed by the flexion force of the MP joint due to the voluntary contraction of the FDS, which is not dynamic tendon fixation. Interestingly, the postoperative hand form was immediately improved without special training [9]. This suggests that the FDS acted as an MP joint flexor muscle early in the postoperative period, indicating that the lasso procedure does not require muscle re-education training to enable functional transformation. As shown above, the results of this study, which clarified the activity characteristics of the FDS, are the basis for these excellent clinical results. In addition to the selection of the donor muscle, knowledge of the activity characteristics of the FDS may be helpful for postoperative rehabilitation in many functional reconstruction procedures using the FDS.
This study has several limitations. First, it was limited to the ring finger muscles; the FDS of the index, middle, and little fingers should be investigated in future studies. Second, the FDS is an extrinsic muscle and may be affected by the forearm and wrist positions; further studies with more patients are needed in a variety of settings to provide more reliable results. Last, clinical studies are needed to investigate FDS activity in actual patients undergoing the lasso technique; this would further support the findings.

In this study, the usefulness of the lasso procedure for reconstruction using the FDS for claw hand deformity was examined using EMG. We clarified that the FDS has the characteristics of being active during MP joint flexion and adduction movements even in the PIP joint extension position. The FDS also showed high activity in conjunction with the dominant gripping form of the intrinsic muscle in which the interosseous muscle works. Therefore, the lasso procedure for migrating the FDS, a PIP joint flexor, to the MP joint flexor effectively reconstructs the claw hand deformity. Furthermore, the need for postoperative functional transformation training is low, and the correction of deformation and improvement in object gripping force are expected at the early postoperative stage.
We thank Dr. M.Kubo and Dr. T.Nara for helpful comments on the manuscript. We would like to thank Editage (www.editage.com) for English language editing.
The study was approved by the Ethics Committee of Niigata University of Health and Welfare (approval number:18301-191119).
There are no conflicts of interest to declare.