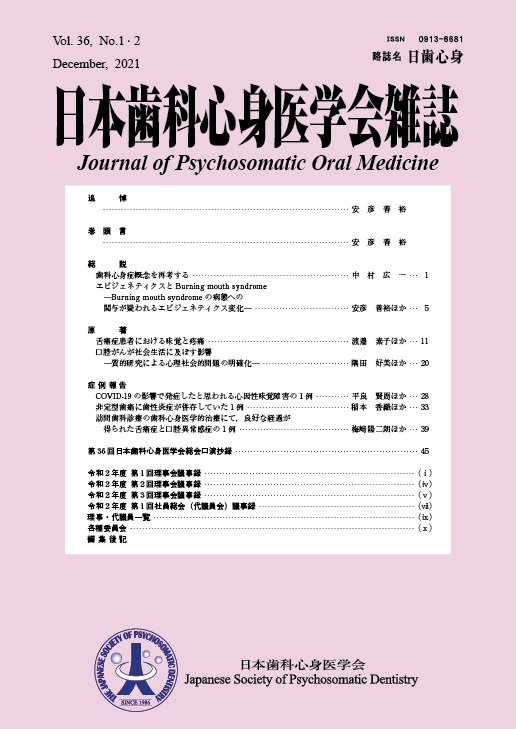
Volume 36, Issue 1-2
Displaying 1-7 of 7 articles from this issue
- |<
- <
- 1
- >
- >|
Review Articles
-
2022 Volume 36 Issue 1-2 Pages 1-4
Published: 2022
Released on J-STAGE: February 03, 2022
Download PDF (231K) -
2022 Volume 36 Issue 1-2 Pages 5-
Published: 2022
Released on J-STAGE: February 03, 2022
Download PDF (237K)
Original Articles
-
2022 Volume 36 Issue 1-2 Pages 11-
Published: 2022
Released on J-STAGE: February 03, 2022
Download PDF (896K) -
2022 Volume 36 Issue 1-2 Pages 20-
Published: 2022
Released on J-STAGE: February 03, 2022
Download PDF (643K)
Case Reports
-
2022 Volume 36 Issue 1-2 Pages 28-
Published: 2022
Released on J-STAGE: February 03, 2022
Download PDF (419K) -
2022 Volume 36 Issue 1-2 Pages 33-
Published: 2022
Released on J-STAGE: February 03, 2022
Download PDF (846K) -
2022 Volume 36 Issue 1-2 Pages 39-
Published: 2022
Released on J-STAGE: February 03, 2022
Download PDF (396K)
- |<
- <
- 1
- >
- >|