2021 年 3 巻 3 号 p. 88-95
2021 年 3 巻 3 号 p. 88-95
BACKGROUND
Primary curative treatment of resectable laryngeal cancer includes surgery and chemoradiotherapy. Other treatment options include radiotherapy, chemoradiotherapy, partial laryngectomy, and total laryngectomy. Larynx-preserving treatments (partial laryngectomy, radiotherapy, and chemoradiotherapy) are recommended in early stage cases, although total laryngectomy is needed in advanced cases. Here, we evaluated trends in treatment strategies and identified the factors that are important in decision making.
METHODS
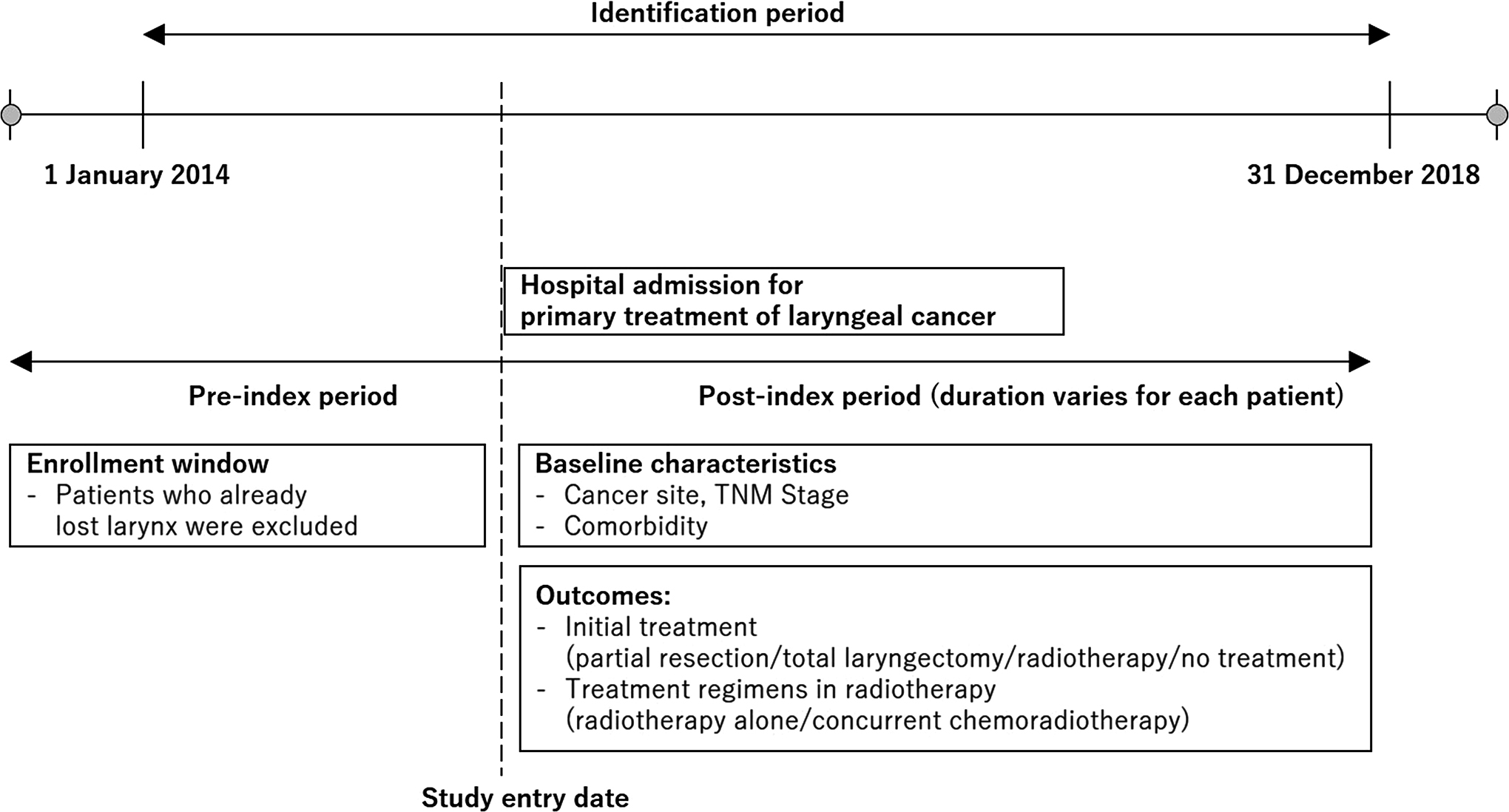
We performed a retrospective analysis of data acquired from electronic medical records in Japan. Hospitalized laryngeal cancer patients admitted between January 2014 and December 2018 were included in our analyses. The primary outcome was the initial treatment.
RESULTS
A total of 363 patients (mean age 71.8 ± 9.5, male/female = 333/30) met the inclusion criteria. Of these, 10.1% of the patients were treated with total laryngectomy, while 17.9% underwent partial resection, 65.8% received radiotherapy (chemoradiotherapy), and 6.1% had no treatment. Larynx-preserving treatment was used in most T1–2 cases (96.9%), and 40% of the patients with T3 cancer underwent total laryngectomy (adjusted odds ratio 26.7 [95% CI, 9.29-91.6]). Of the T3 cancers that were treated, total laryngectomy was performed in only 26.7% of patients aged ≤65 years, but in more than 50% of those aged >65 years.
CONCLUSIONS
This retrospective study showed that larynx-preserving treatments were used in most T1–2 cases, and suggested that T stage is the most important factor affecting decision making in the treatment of laryngeal cancer. Older patients with T3 disease tended to undergo total laryngectomy, and age is an important factor in the decision-making process for cases of T3 laryngeal cancer.
The larynx is responsible for several essential functions, including sound production and swallowing. Problems in the larynx can lead to significant impairment in quality of life. Hence, preserving the function and quality of the larynx is of high importance when treating patients with laryngeal cancer [1, 2]. In the 1990s, concurrent chemoradiotherapy (CCRT) was introduced as an alternative to total laryngectomy, but the overall survival rate in patients with CCRT was lower than in those with total laryngectomy [3]. With advances in chemotherapy and radiotherapy of recent years, CCRT has become as efficient as total laryngectomy in patients with locally advanced disease. Although patients with T4 tumors are treated with total laryngectomy, radiotherapy and CCRT are the standard of care for patients with laryngeal cancer [4, 5].
The Japanese Society for Head and Neck Cancer first published their clinical practice guideline (CPG) in 2009, which was revised in 2013 and 2018 [5, 6]. According to the CPG, larynx-preserving strategies and radiation therapy are recommended for patients with early-stage (T1-2N0) laryngeal cancer [5]. Moreover, according to CPG, CCRT is recommended prior to radiotherapy for patients with resectable locally advanced laryngeal cancer. Currently, available treatment options for patients with resectable locally advanced laryngeal cancer include radiotherapy, CCRT, partial laryngectomy, and total laryngectomy. However, to date, there is no information guiding the decision making for patients with resectable locally advanced laryngeal cancer in Japan. In this study, we assessed the treatment options for patients with laryngeal cancer and identified clinical factors that should be considered when choosing the appropriate therapeutic approach.
This cohort study was performed using routinely collected patient data, which were reported according to the RECORD reporting guidelines [7]. We retrospectively analyzed data from patients with T1-3N0-2M0 laryngeal cancer. We used the commercially available Real World Data (RWD) database provided by the Health, Clinic, and Education Information Evaluation Institute (HCEI) [8]. The RWD database contains electronic medical records (EMR) from multiple hospitals nationwide; it includes data from approximately 19 million inpatients and outpatients, covering 1.6% of the total population of Japan. Data from patients who had a history of laryngeal cancer according to the ICD-10 (international classification of diseases, codes; C320, C321, C322, C329) were obtained from the RWD database in September 2019; the HCEI provided this dataset to the authors.
DATA SOURCEThe RWD database contains EMR, claims, and Diagnosis Procedure Combination (DPC) data. The database contains patient baseline characteristics, including year of birth, date of death, and sex (from EMR), information on procedures, including surgeries (from claims data), laboratory test results (from EMR), and discharge abstract data. Information on diseases (i.e., ICD-10 codes) were obtained from both claims data and EMR. Drug data were labeled based on the Japanese receipt code and YJ code. Laboratory test results were standardized and labeled according to the Japanese Laboratory Code version 10.
PATIENT SELECTIONFor our analyses, we included patients with resectable laryngeal cancer aged 20 years or more who were admitted within the 5-year study period (January 2014 to December 2018). Patients with ICD-10 C320, C321, C322, and C329 on DPC data were potentially eligible for this study. The hospital admission date was used as the study entry date (index date). For our analyses, we included patients who were admitted for laryngeal cancer treatment (Fig. 1). T4, N3, or M1 cases, as well as patients with unclear T stage, were excluded. Patients who had surgeries with Japanese procedure codes C112 (tracheostomy), K394-2 (laryngectomy), K395 (pharyngolaryngectomy), K403-2-4 (laryngotracheal separation), or K403-2-3 (total laryngectomy for aspiration) before the index date were also excluded.
As primary outcomes of the initial treatment of patients, we included “total laryngectomy”, “partial resection (cordectomy or partial laryngectomy)”, “radiotherapy (CCRT)”, and “no treatment”. Total laryngectomy and partial resection included postoperative radiotherapy or CCRT. As “no treatment”, we also considered cases treated with non-radical chemotherapy, because chemotherapy alone does not provide a cure for laryngeal cancer. As secondary outcomes, we considered the regimens of radiotherapy and chemotherapy.
STATISTICAL ANALYSISFor the primary outcome, we calculated the proportion of initial treatment for each T stage and age. Multivariate regression analysis was performed to assess the relationships between patient characteristics and treatment strategy. First, we performed univariate analysis using Fisher’s exact test (for T stage, N stage, sex, dementia-related daily life activities, number of hospital beds, case volume, hypertension, diabetes mellitus, and renal dysfunction), or Student’s t-test (for age). Factors for which P < 0.2 in univariate analysis were included in multivariate regression analysis. For the univariate and multivariate analyses, we included patients who had a total laryngectomy, partial resection (cordectomy or partial laryngectomy), or radiotherapy (CCRT). Cancer site was unclear in about 10% of patients, so was not included in the univariate or multivariate analysis. Patients who had undergone total laryngectomy were classified as “larynx-lost”, while patients who had undergone partial resection (cordectomy or partial laryngectomy) and radiotherapy (CCRT) were classified as “larynx-preserving”.
For the secondary outcomes, we calculated the relative proportions of radiotherapy regimens in each cancer stage and age. We also assessed the variation between hospitals. We classified hospitals as higher case volume hospitals (≥30 cases during the study period) or lower case volume hospitals (<30 cases), and then compared the relative proportions of radiotherapy regimens between the two groups.
The institutional review board of Kurashiki Central Hospital approved this study, which was registered at the UMIN Clinical Trial Registry (No UMIN000041785).
For our analyses, a total of 363 patients (mean age, 71.8 ± 9.5; male to female ratio, 333/30) from 23 hospitals were included. Five of the 23 hospitals had at least a total of 30 cases (five cases per year), while ten hospitals had less than nine cases. Ten of the twenty-three hospitals had 500 or more hospital beds, while nine had 300–499 hospital beds, and four had fewer than 300 hospital beds. The baseline characteristics of the patients are shown in Table 1.
| Variables | Laryngeal Cancer (n = 363) |
|---|---|
| Characteristics | |
| Age (year) | 71.8 ± 9.5 |
| Gender (male/female) | 333/30 |
| Cancer site | |
| Upper | 92 (25.3%) |
| Vocal cord | 228 (62.8%) |
| Lower | 10 (2.8%) |
| Unclear | 33 (9.1%) |
| T Stage classification (UICC 7th Edition) | |
| T1 | 173 (47.7%) |
| T2 | 120 (33.1%) |
| T3 | 70 (19.3%) |
| Smoke index | |
| 1200 or more | 101 (27.8%) |
| 601–1200 | 118 (32.5%) |
| 51–600 | 68 (18.7%) |
| –50 | 76 (20.9%) |
| Concurrent medical disease | |
| Hypertension | 144 (39.7%) |
| Diabetes mellitus | 93 (25.6%) |
| Renal dysfunction (serum creatinine >1.5 mg/dl) | 15 (4.1%) |
| Dementia related activity daily life | |
| Normal* | 345 (95.0%) |
| I–II | 14 (3.9%) |
| III–IV | 4 (1.1%) |
| Hospital beds | |
| 500 or more | 10 (43.5%) |
| 300–499 | 9 (39.1%) |
| 100–299 | 4 (17.4%) |
| Case-volume of hospitals | |
| 30 or more (5 cases per year) | 5 (21.7%) |
| 10–29 | 8 (34.8%) |
| –9 | 10 (43.5%) |
The proportions of initial treatment in each T stage and age are summarized in Fig. 2. In general, T1–T2 patients underwent larynx-preserving treatments, regardless of age. In contrast, the treatment of patients with T3 stage varied immensely. In univariate analyses, the T stage, N stage, number of hospital beds, and age had P-values <0.2. Therefore, these factors were included in the multivariate logistic regression analysis. T stage was significantly correlated with larynx-lost (Table 2). Although the correlation was not significant, older patients were more likely to undergo total laryngectomy (larynx-lost).

Initial treatment was classified as total laryngectomy (+ postoperative radiotherapy [CCRT]), partial resection, radiotherapy (CCRT) or no treatment.
| Larynx-preservation (n = 304) | Larynx-lost (n = 37) | Adjusted odds ratio (95% CI) | p-value | |
|---|---|---|---|---|
| T stage | ||||
| T1 | 163 | 5 | 1 (ref) | <0.01 |
| T2 | 110 | 4 | 1.04 (0.24–4.14) | |
| T3 | 21 | 28 | 26.7 (9.29–91.6) | |
| N stage | ||||
| N0 | 271 | 31 | 1 (ref) | 0.220 |
| N1–2 | 33 | 6 | 0.26 (0.07–0.85) | |
| Hospital beds | ||||
| 500 or more | 212 | 33 | 1 (ref) | 0.547 |
| <500 | 92 | 4 | 1.62 (0.48–6.57) | |
| Age | ||||
| –65 | 78 | 6 | 1 (ref) | 0.205 |
| 66–75 | 125 | 16 | 2.53 (0.80–8.97) | |
| 76– | 101 | 15 | 2.51 (0.79–8.87) | |
Larynx-preservation include radiotherapy (chemoradiotherapy) and partial resection. Larynx-lost include total laryngectomy.
Of the patients with T3 cancer who underwent treatment, total laryngectomy was performed in only 26.7% of those aged 65 years or younger, but in more than 50% of those older than 65 years (Fig. 3). Total laryngectomy was performed in 52.2% of patients aged 66–75 years and in 57.1% of those–76 years or older.

Initial treatment was classified as total laryngectomy (+postoperative radiotherapy [CCRT]) or radiotherapy (CCRT). Patients who were not treated were excluded. No T3 disease patients elected to undergo partial resection.
The variations in proportion of radiotherapy according to age and stage (I–II versus III–IV) are summarized in Fig. 4. The majority of patients who had radiotherapy alone had stage I–II cancer, while approximately 50% of the patients with stage III–IV disease received CCRT. None of the patients aged 81 years or older underwent CCRT. The results of the stratified analysis by case volume in each hospital are summarized in Fig. 5. Compared with higher case volume hospitals (≥30 cases during the study period), CCRT was more frequent in stage I–II patients in lower volume hospitals (<30 cases). The mean was 72.3 and 70.8 years in the higher and lower case volume hospitals, respectively. The proportions of cases with hypertension, diabetes mellitus, and renal dysfunction were 42.1%, 24.8%, and 2.5% in higher case volume hospitals and 44.6%, 36.9%, and 7.7% in lower case volume hospitals, respectively. Intravenous drug dose data, in claims and RWD databases, are not accurate in Japan, so we did not analyze the chemotherapy doses in this study.

The chemotherapy regimens contained cisplatin, cetuximab, and TS-1 (tegafur/gimeracil/oteracil).

Hospitals were classified as high case volume hospitals (≥30 or more cases of laryngeal cancer during the study period [≥5 cases annually]) or low case volume hospitals (<30 cases).
The treatment patterns in laryngeal cancer in have been explored in various countries [9]. The Japan Society for Head and Neck Cancer launched the Head and Neck Cancer Registry [10] and reported an association between T classification and treatment type. However, a previous study using the registry did not report treatments according to patient age. In addition, that study classified the treatments as surgery, radiotherapy, or chemotherapy, and did not distinguish partial resection (larynx-preserving) from total laryngectomy (larynx-lost). This multi-institutional database study revealed that the treatment of patients with resectable laryngeal cancer in Japan varies significantly. Several guidelines recommend that larynx-preserving therapeutic approaches should be used in patients with early-stage cancer (clinical stage I-II, T1-2N0) [5, 11, 12]; larynx-preserving strategies were widely used in the patients included in our analyses. These guidelines also advise laryngectomy for T4 cases, although the appropriate treatment for T3N0 and T1-3N1 has not been established. This study also revealed variations in the initial treatment and radiotherapy (CCRT) depending on the disease stage and age.
CCRT is one of the larynx-preserving strategies offered to patients with advanced cancer [13, 14]. However, its efficacy is limited, especially in older patients and patients with impaired health status [14]. In addition, treatment with high doses of cisplatin (≥200 mg/m2) is recommended in CCRT [15, 16]; however, these doses are toxic, especially in older patients. Randomized controlled trials assessing the efficacy of CCRT involve younger patients than those included in our study [14, 17]. In cases where patients cannot tolerate chemotherapy, CCRT provides poor survival rates compared with total laryngectomy. A population study assessing the relationship between age and treatment (total laryngectomy or CCRT) in patients with advanced laryngeal cancer in the USA [18]. The proportion of patients undergoing total laryngectomy was 42.5% in the 66–74 years age group (early elderly) and 44.7% in those 75 years or older age group (late elderly) [18]. However, there have been no studies on the association between age and treatment among elderly and non-elderly patients. Our results indicated that ,medical decision making in cases of advanced laryngeal cancer is similar between early and late elderly patients (Fig. 3), and that elderly patients with T3 stage cancer undergo total laryngectomy at a higher rate compared with non-elderly patients. The results also indicated that radiotherapy combined with cisplatin was largely avoided in older patients.
Analysis stratified according to case volume in each hospital suggested that lower case volume hospitals tended to treat cases of stage I–II cancer with CCRT, although the baseline characteristics of patients did not tend to vary by case volume. CCRT was not recommended in stage I cancer patients [6]; it is important to confirm whether this trend applies throughout Japan.
This study assessed the variation in treatment of laryngeal cancer patients using large-scale real-world data. However, the study had some limitations. First, the database included potential misclassification of patients’ disease, drug exposure, and outcome. Compared with other diseases, malignancy has high sensitivity and positive predictive value [19, 20]. In an effort to improve the accuracy of the disease, we used the DPC disease code [19]. Second, for this study, we used real-world data; however, it is very likely that the population included in our analyses does not represent the whole Japanese population. A nationwide survey estimated 5,000 new cases of laryngeal cancer annually [21]. This study included approximately 0.7% of the laryngeal cancer cases; our cohort was similar in both sex and age to those of the survey [21]. We, therefore, assumed that the population included in this study reflected the total laryngeal cases of Japan. Third, considered the first admission date as the index date, but it was unclear whether the index date was truly the date of first diagnosis. The time between diagnosis and admission may have introduced bias. The TNM stages in this study were those on admission rather than those on first diagnosis. Our analysis showed that all T1–2 patients aged 86 years or older received treatment, although about 10% of the T1–2 patients aged 81–85 years did not receive any treatment. Our analyses included patients who were admitted for laryngeal cancer, and excluded those who were not hospitalized. Thus, patients with T1–2 laryngeal cancer who refused to undergo treatment, as well as patients admitted later because of airway obstruction (T3 stage), were considered as T3 cases. Finally, the clinical outcomes, including survival rate, complications, and quality of life (QOL), are important factors for decision making in the treatment of laryngeal cancer patients [22]. However, these outcomes were not analyzed in this study. These outcomes should be analyzed in future large-cohort studies.
In this retrospective study from data acquired from a medical database in Japan, T1-2 laryngeal cancer patients were commonly treated with larynx-preservation strategies; however, total laryngectomy was performed in 40% of T3 laryngeal cancer cases. T factor was associated with the treatment- decision making for patients with resectable locally advanced laryngeal cancer, and age would be an important factor in T3 laryngeal cancer cases.
This research was supported by the Kurashiki Clinical Research Institute.
All authors have no potential conflict of interest in this study from third parties (e.g. research grand, honoraria for speaking at symposia, financial support, employment/consultation, support from project sponsor, or position on advisory board)