2022 年 4 巻 1 号 p. 11-19
2022 年 4 巻 1 号 p. 11-19
BACKGROUND
Although outpatient cardiac rehabilitation has been shown to be effective, the participation status of older cardiac patients is unclear in real-world settings. We investigated the proportion and associated factors of outpatient cardiac rehabilitation participation among older patients with heart diseases after cardiac intervention.
METHODS
We analyzed data from medical and long-term care insurance claims data from two municipalities in Japan. The data coverage period was between April 2014 and March 2019 in City A and between April 2012 and November 2016 in City B. We identified patients aged ≥65 years with post-operative acute myocardial infarction, angina pectoris, or heart valve disease. We estimated the proportion of cardiac rehabilitation participation and conducted logistic regression to identify factors (age, sex, type of cardiac disease, open-heart surgery, Charlson comorbidity index, long-term care need level, catecholamine use, inpatient cardiac rehabilitation, and hospital volume for cardiac rehabilitation) associated with outpatient cardiac rehabilitation participation.
RESULTS
A total of 690 patients were included in this study. The proportion of patients receiving outpatient cardiac rehabilitation was 9.0% overall. Multivariable logistic regression analysis suggested that men (adjusted OR 3.98; 95% CI 1.69–9.37), acute myocardial infarction (adjusted OR 2.76; 95% CI 1.20–6.36; reference angina pectoris), inpatient cardiac rehabilitation (adjusted OR 17.01; 95% CI 5.33–54.24), and “hospital volume” for cardiac rehabilitation (adjusted OR 4.35; 95% CI 1.14–16.57 for high-volume hospitals; reference low-volume hospital) were independently associated with outpatient cardiac rehabilitation.
CONCLUSIONS
The participation rate of outpatient cardiac rehabilitation among older post-operative cardiac patients was suboptimal. Further studies are warranted to examine its generalizability and whether a targeted approach to a group of patients who are less likely to receive outpatient cardiac rehabilitation could improve the participation rate.
Cardiac rehabilitation (CR), categorized as secondary or tertiary prevention for cardiovascular diseases [1], is a multifaceted and comprehensive intervention for cardiovascular diseases. CR can be provided for patients with acute and chronic heart diseases during and after hospitalization for a period of time (e.g., five months in Japan) [2]. Outpatient CR is known to reduce rehospitalizations and cardiovascular mortality as well as improve cardiopulmonary function in patients with coronary artery disease and heart failure [3, 4].
In Japan, CR is covered by national medical insurance and is mainly for the following patients: patients with acute myocardial infarction, angina pectoris, those who have had surgery for cardiovascular disease (i.e., percutaneous coronary intervention, coronary artery bypass grafting, heart valve replacement, transcatheter aortic valve implantation), chronic heart failure, and peripheral arterial disease. In particular, post-operative patients with coronary artery disease and heart valve disease are eligible for CR and it is strongly recommended in the current guidelines of Japan, Europe, and the United States [2, 5–7].
While there has been accumulating evidence to support the benefits of CR, CR participation has been reported to be suboptimal in several countries [8–10]. Previous studies using claims data from people aged <65 years and questionnaires reported low CR participation rates of patients with heart disease in Japan [11, 12]. However, to the best of our knowledge, no studies have yet examined the CR participation status and its associated factors in older people in Japan.
Therefore, using medical and long-term care insurance receipts from two municipalities in Japan, we examined i) the state (proportion) of outpatient CR participation and ii) factors associated with outpatient CR participation, among patients receiving cardiac interventions, including percutaneous coronary intervention, coronary artery bypass grafting, heart valve replacement, or transcatheter aortic valve implantation.
We analyzed data from a retrospective cohort study using medical and long-term care insurance claims data between April 2014 and March 2019 in City A and between April 2012 and November 2016 in City B. These medical claims data include data on people with citizens’ health insurance for municipalities and unions and late elders’ health insurance, but data of other people for other types of health insurance (e.g., insurance for company employees) are not included [13]. Long-term care insurance claims data include information on long-term care need levels (support 1–2 and care 1–5) and services used for all residents who receive long-term care insurance certification [14]. Medical and long-term care insurance claims data were linked by an ID assigned to individuals for the purpose of research. The population of City A and City B were approximately 220,000 and 55,000, with approximately 40,000 (18.2%) and 16,000 (28.9%) people aged ≥65 years, respectively, in 2014.
STUDY POPULATIONWe identified patients aged ≥65 years who had at least one medical insurance claim record between April 2014 and March 2019 in City A and between April 2012 and November 2016 in City B. Patients aged ≥65 years were considered eligible for CR if they met the following criteria: had information on at least one experience of percutaneous coronary intervention or coronary artery bypass grafting for acute myocardial infarction or angina pectoris, heart valve replacement, or transcatheter aortic valve implantation for heart valve disease between October 2014 and October 2018 in City A, and between October 2012 and May 2016 in City B. We defined each disease using the International Classification of Disease, Tenth Revision codes (acute myocardial infarction: I21x; angina pectoris: I20x; heart valve disease: I340, I350, and I352). We defined each operation using the relevant Japanese original procedure codes (percutaneous coronary intervention: K546, K547, K548, K549, K550, and K550-2; coronary artery bypass grafting: K552 and K552; heart valve replacement: K555; transcatheter aortic valve implantation: K555-2). If there were more than two operations at different months, the earliest operation was considered the index event and thus included in the analysis.
The exclusion criteria were i) death during admission, ii) discharge to nursing facilities, and iii) incidence of stroke after operation during the same hospitalization. We identified people who satisfied the aforementioned conditions in each city separately, but conducted analyses using a pooled population of the two cities.
CR PARTICIPATION STATUSWe identified outpatient and inpatient CR participation using medical insurance claims data. Outpatient CR participation was defined as having treatment codes for CR (H000) within five months of the qualifying event date and post-discharge because the current Japanese insurance system allows reimbursement for outpatient CR participation for five months after discharge. Inpatient CR participation was defined as having treatment codes for CR during hospitalization. Outpatient CR participation was the outcome of interest in the current study, while inpatient CR participation was regarded as one of the exposures (covariates).
FACTORS ASSOCIATED WITH OUTPATIENT CRFor each patient, factors associated with outpatient CR were collected as follows: age, sex, type of heart disease (acute myocardial infarction, angina pectoris, or heart valve disease), Charlson comorbidity index (CCI), long-term care need level, open-heart surgery, catecholamine use during hospitalization, inpatient CR participation, and “hospital volume” for CR. CCI was initially developed as a disease-weighted score for the prediction of mortality, but it is also known to represent the burden of multimorbidity status [15–17]. We used the 2011 updated and reweighted version of the original CCI scores, which was validated in a Japanese national administrative dataset [18]. CCI scores were calculated based on the following diseases: congestive heart failure, dementia, chronic pulmonary disease, rheumatological disease, mild liver disease, diabetes mellitus, hemiplegia and paraplegia, renal disease, malignancy, moderate/severe liver disease, metastatic solid tumor, and HIV/acquired immunodeficiency syndrome. We identified these diseases from medical insurance claims data during the three months before the qualifying event date. Long-term care need level is a nationally standardized certification that is judged based on the consideration of an individual’s physical and cognitive function [19]. Long-term care need levels were classified into three groups (none, support levels 1–2, and care levels 1–5). We used the long-term care need level on the most recent certification date before the qualifying event date. Whether open-heart surgery was performed was determined by the type of surgery; coronary artery bypass grafting and heart valve replacement were identified as open-heart surgery. We used the presence or absence of the catecholamine injection during hospitalization as a proxy variable for disease severity of cardiac diseases. To account for the capacity to conduct CRs in each hospital, we defined “hospital volume” for CR by counting the average annual number (for which a CR order for a patient in a day was counted as one) of CRs (regardless of inpatient or outpatient) in each hospital, and categorized hospitals into three groups (low, middle, and high-volume hospitals) for the study participants to be roughly tertile.
STATISTICAL ANALYSISWe described the patient overall and by disease outpatient CR participation status. Next, we divided eligible patients into two groups based on whether they used outpatient CR. We compared the characteristics of eligible patients between the groups using the χ2 test for binary variables and the Wilcoxon rank sum test for ordinal variables.
Next, we conducted univariable and multivariable logistic regression analyses to examine factors associated with outpatient CR participation. The outcome in the logistic regression model was outpatient CR participation and potential exposures were age, sex, type of disease, CCI, long-term care need level, open-heart surgery, catecholamine use, inpatient CR participation, and “hospital volume” for CR. In the multivariable model, due to limited number of outcomes, we included only factors significantly associated with the outcome in the univariable models. We estimated unadjusted and adjusted OR and 95% CI from these regression models.
In a sensitivity analysis, we excluded patients who were admitted in hospitals with no CR at all.
All statistical analyses were conducted using Stata version 15.0 (Stata Corp LP, College Station, TX, USA). A p-value <.05 (two sided) was considered statistically significant.
ETHICAL CONSIDERATIONSThe ethics committee of the University of Tsukuba approved this study (approval numbers: 1445 and 1447). Informed consent from individuals was waived because the claims data were anonymized before the data were made available to the researchers.
Of 66,220 people aged ≥65 years with at least one medical insurance claim record in two cities, 690 patients receiving cardiac intervention at (one of) 56 hospitals were included in the analyses. The flowchart in Fig. 1 shows the process of study population selection. Among the 690 patients, 681 patients (98.7%) had available data until 5 months after cardiac intervention, while 9 patients died within 5 months.
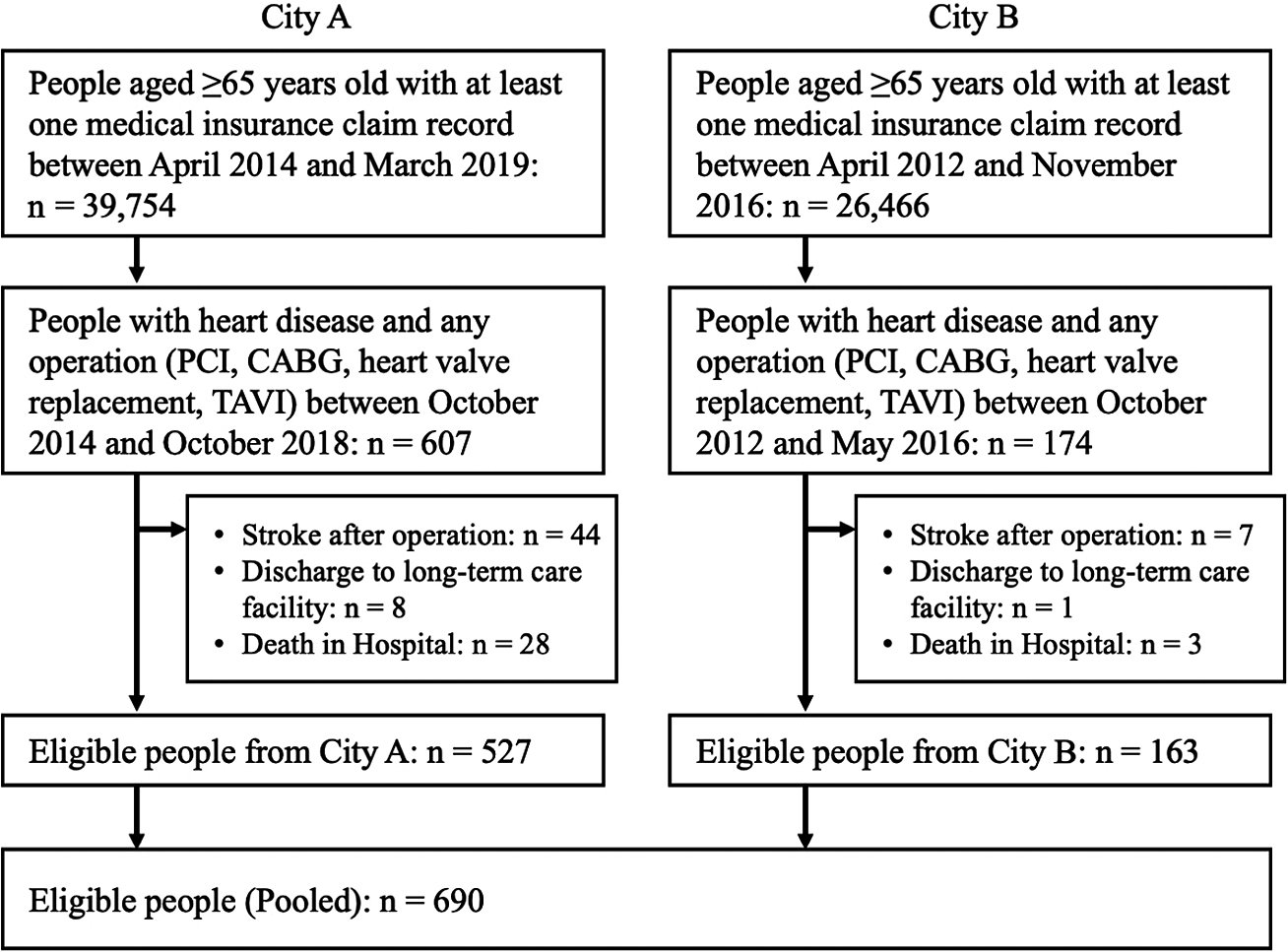
Abbreviation: PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; TAVI, transcatheter aortic valve implantation.
The proportion of patients receiving outpatient CR was 9.0% (62/690) overall, 20.1% (38/189) for acute myocardial infarction, 3.1% (13/413) for angina pectoris, and 12.5% (11/88) for heart valve disease.
Table 1 shows the differences between the characteristics of patients who used outpatient CR and those who did not use outpatient CR. Patients who used outpatient CR tended to be men, had a higher percentage of acute myocardial infarction and catecholamine use, had a lower percentage of angina pectoris, underwent open-heart surgery, participated in inpatient CR, and were admitted in hospitals with a larger “hospital volume” for CR.
| Overall n = 690, n (%) |
Patients with outpatient cardiac rehabilitation n = 62, n (%) |
Patients without outpatient cardiac rehabilitation n = 628, n (%) |
P value | |
|---|---|---|---|---|
| Sex (men) | 516 (74.8) | 55 (88.7) | 461 (73.4) | .008 |
| Age category (years) | .403 | |||
| 65–69 | 167 (24.2) | 18 (29.0) | 149 (23.7) | |
| 70–74 | 169 (24.5) | 17 (27.4) | 152 (24.2) | |
| 75–80 | 173 (25.1) | 17 (27.4) | 156 (24.8) | |
| 80–84 | 110 (15.9) | 5 (8.1) | 105 (16.7) | |
| ≥85 | 71 (10.3) | 5 (8.1) | 66 (10.5) | |
| Type of disease | <.001 | |||
| Angina pectoris | 413 (59.9) | 13 (21.0) | 400 (63.7) | |
| Acute myocardial infarction | 189 (27.4) | 38 (61.3) | 151 (24.0) | |
| Heart valve disease | 88 (12.6) | 11 (17.7) | 77 (12.3) | |
| Open-heart surgery | 98 (14.2) | 16 (25.8) | 82 (13.1) | .006 |
| Charlson comorbidity index | .468 | |||
| 0 | 152 (22.0) | 16 (25.8) | 136 (21.7) | |
| 1 | 129 (18.7) | 15 (24.2) | 114 (18.2) | |
| 2 | 122 (17.7) | 9 (14.5) | 113 (18.0) | |
| ≥3 | 287 (41.6) | 22 (35.5) | 265 (42.2) | |
| Long-term care need level | .245 | |||
| None | 600 (87.0) | 57 (91.9) | 543 (86.5) | |
| Support need level 1–2 | 28 (4.1) | 3 (4.8) | 25 (4.0) | |
| Care need level 1–5 | 62 (9.0) | 2 (3.2) | 60 (9.6) | |
| Catecholamine use | 465 (67.4) | 55 (88.7) | 410 (65.3) | <.001 |
| Inpatient cardiac rehabilitation | 270 (39.1) | 58 (93.5) | 212 (33.8) | <.001 |
| “Hospital volume” for cardiac rehabilitation* | <.001 | |||
| Low | 188 (27.2) | 3 (4.8) | 185 (29.5) | |
| Middle | 170 (24.6) | 14 (22.6) | 156 (24.8) | |
| High | 332 (48.1) | 45 (72.6) | 287 (45.7) |
* We defined “hospital volume” for cardiac rehabilitation (i.e., the capacity to conduct cardiac rehabilitations in the hospital) by counting the average annual number (meaning that a cardiac rehabilitation order for a patient in a day was counted as one) of cardiac rehabilitations (regardless of inpatient or outpatient) in each hospital, and categorized hospitals into three groups for the study participants to be roughly tertile: low (0–10/year), middle (11–300/year), and high (301–1000/year)
Table 2 shows the results of univariable and multivariable logistic regression analyses to identify factors associated with outpatient CR participation. Multivariable logistic regression analysis suggested that men (adjusted OR 3.98; 95% CI 1.69–9.37), acute myocardial infarction (adjusted OR 2.76; 95% CI 1.20–6.36; reference angina pectoris), inpatient CR (adjusted OR 17.01; 95% CI 5.33–54.24), and “hospital volume” for CR (adjusted OR 4.35; 95% CI 1.14–16.57 for high-volume hospital; reference low-volume hospital) were independently associated with outpatient CR. In a sensitivity analysis excluding 37 patients admitted in hospitals with no CR at all, the results were similar to those in the main analysis (Supplementary Appendix).
| Univariable (n = 690) | Multivariable* (n = 690) | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P Value | Odds ratio | 95% CI | P Value | |
| Sex, men | 2.84 | 1.27–6.37 | .011 | 3.98 | 1.69–9.37 | .002 |
| Age category, y | ||||||
| 65–69 | Reference | |||||
| 70–74 | 0.93 | 0.46–1.86 | .829 | |||
| 75–80 | 0.90 | 0.45–1.82 | .773 | |||
| 80–84 | 0.39 | 0.14–1.10 | .074 | |||
| ≥85 | 0.63 | 0.22–1.76 | .376 | |||
| Type of disease | ||||||
| Angina pectoris | Reference | Reference | ||||
| Acute Myocardial infarction | 7.74 | 4.01–14.94 | <.001 | 2.76 | 1.20–6.36 | .017 |
| Heart valve disease | 4.40 | 1.90–10.17 | .001 | 1.07 | 0.39–2.92 | .896 |
| Open heart surgery | 2.32 | 1.25–4.28 | .007 | 1.47 | 0.57–3.79 | .427 |
| Charlson comorbidity index | ||||||
| 0 | Reference | |||||
| 1 | 1.12 | 0.53–2.36 | .769 | |||
| 2 | 0.68 | 0.29–1.59 | .371 | |||
| ≥3 | 0.71 | 0.36–1.39 | .312 | |||
| Long-term care need level | ||||||
| None | Reference | |||||
| Support need level 1–2 | 1.14 | 0.33–3.90 | .831 | |||
| Care need level 1–5 | 0.32 | 0.08–1.33 | .117 | |||
| Catecholamine use | 4.18 | 1.87–9.33 | <.001 | 1.20 | 0.43–3.36 | .729 |
| Inpatient cardiac rehabilitation | 28.45 | 10.19–79.43 | <.001 | 17.01 | 5.33–54.24 | <.001 |
| “Hospital volume” for cardiac rehabilitation | ||||||
| Low | Reference | Reference | ||||
| Middle | 5.53 | 1.56–19.61 | .008 | 2.34 | 0.61–9.05 | .217 |
| High | 9.67 | 2.96–31.57 | <.001 | 4.35 | 1.14–16.57 | .031 |
CI, confidence interval
* Due to limited number of outcomes, we included only factors significantly associated with the outcome in the univariable models.
In this population-based study using combined medical and long-term care claims data, the proportion of outpatient CR participation of post-operative heart disease patients aged ≥65 was 9.0%. Of the heart diseases included in this study, acute myocardial infarction was the most common disease, for which outpatient CR was performed. Men, having acute myocardial infarction, inpatient CR participation, and higher “hospital volume” for CR were independently associated with outpatient CR participation. Although the results were from two cities, to the best of our knowledge, this study is the first population-based study of outpatient CR participation and associated factors in Japanese older people. The population-based study can collect information on outpatient CR more comprehensively than hospital-based studies. The findings of our study can be basic data to suggest who should be targeted when promoting outpatient CR participation.
This study showed a low proportion of post-operative CR among patients with heart diseases aged ≥65 years in two municipalities. The proportion of outpatient CR participation in this study was somewhat higher than results from a previous study of patients aged <65 years using claims data (approximately 5%) [11]. Compared to previous studies in the United States (24.4% overall, 34.5% for acute myocardial infarction with any procedure, 37.2% for heart valve procedure), the proportion of outpatient CR participation was lower both overall and by disease [9].
In addition, the proportion of outpatient CR participation was also low, at 9.0% in total and 21.5% (58/270) in patients who used inpatient CR. The results suggest that seamless interventions from inpatient to outpatient CR have not been sufficiently implemented. CR is not only recommended in the acute phase, but also in the sub-acute phase after discharge from the hospital in many guidelines, including the Japanese version [2, 20]. Therefore, the proportion of outpatient CR participation in older patients derived from this study is still suboptimal. The Million Hearts Cardiac Rehabilitation Collaborative set a goal in 2016 to increase CR participation in the United States from 20% to 70% by 2022 [21]. In Japan, goals like those in the United States have not yet been decided. Thus, Japan may also need to set a specific goal to improve the proportion of outpatient CR participation.
The multivariable logistic regression analysis showed that being a man, having myocardial infarction, inpatient CR participation, and higher “hospital volume” for CR were associated with outpatient CR participation. In particular, inpatient CR participation was strongly associated with outpatient CR participation. However, inpatient CR participation was also suboptimal, at 39.1% in the current study. The reasons why more than 60% of study participants did not undergo inpatient CR may include the short length of stay after surgery, the hospital where patients were admitted not being a hospital that could provide CR, or the physician’s insufficient understanding of the need for CR [22–24]. As the number of hospitals that could provide CR has increased in recent years [25], it is necessary to promote inpatient CR participation. In addition, referring patients who did not undergo inpatient CR to outpatient CR programs needs to be increased. Currently in Japan, it is not common to refer a patient to an outpatient CR program at another facility from a hospital where patients were admitted. Therefore, referring patients who were not able to use inpatient CR to outpatient CR programs may need to be considered.
Patients with myocardial infarction were more likely to participate in outpatient CR compared with those with angina pectoris. This finding is consistent with the results of a Japanese study of outpatient CR in patients with coronary artery disease and younger than 65 years of age [11]. The guidelines strongly recommend comprehensive outpatient CR for patients undergoing percutaneous coronary intervention or coronary artery bypass grafting [2, 26]. Increased promotion of outpatient CR for patients with angina pectoris may be needed.
The lower proportion of outpatient CR participation among women compared to men is consistent with some previous studies [27]. One previous study showed that patient-level CR barriers of women included transportation, high burden of family responsibilities, lack of CR awareness, experience of exercise as tiring or painful, and comorbidities [28]. Although it is unclear whether these factors may be directly applicable to women in our study, it is possible that being a woman may have affected CR participation. Outpatient CR programs for women have also been studied, but the optimal method has not yet been established [29, 30]. Further studies are needed to develop appropriate support for women or gender-specific CR programs.
Several methods have been proposed to improve inpatient CR participation, low rates of women participating in outpatient CR, and referrals to outpatient CR. A systematic approach to CR referral, including automatic referral and assisted enrollment, was reported to be helpful in promoting CR participation [31, 32]. This type of approach may also be useful in promoting inpatient and outpatient CR. In recent years, while the method of CR after discharge in Japan has mainly been based on outpatient CR, home-based and remote CR have also been attempted [33–35]. Using these interventions in combination with conventional CR may improve CR participation after discharge. Implementation of home-based and remote CR is expected to increase in Japan in the future. Then, systems that can monitor CR participation that include these CR methods are also needed to properly evaluate CR participation.
This study has several limitations. First, we could not obtain information other than that contained in the claims data, such as clinical, geographic, and socioeconomic status. Among these unmeasured factors, there may be factors related to CR participation. For example, some physicians may decide to prescribe outpatient CR based on the disease severity of the patient. In addition, we could not use CR certification information of hospitals for providing CR because this information was not available in the claims data. However, as a hospital-level factor, we defined and adjusted for “hospital volume” for CR in the current study, in addition to our sensitivity analysis excluding patients admitted in hospitals with no CR at all. Second, the study population was limited to patients who should be indicated for outpatient CR in the relevant clinical practice guidelines [2, 5, 6, 36], but the inclusion and exclusion criteria may not have sufficiently identified the population who should definitely conduct outpatient OR. For example, some patients may be too severe and contraindicated for outpatient CR. Third, the number of patients who used outpatient CR was small, and we did not have sufficient statistical power. Therefore, we needed to select the minimum number of factors associated with outpatient CR. Finally, we used only information of patients from two municipalities, and thus, the generalizability of this study is limited. In addition, in this study, we limited the study population to patients with cardiac interventions, mainly because (i) the current guidelines in the United States strongly recommend outpatient CR for these patients, while it is not necessarily indicated for all medically-treated heart failure patients [26], and (ii) it is practically difficult to identify medically-treated heart failure, including mild and moderate heart failure from the medical claims data alone. Thus, the generalizability of our findings to medically-treated heart failure is unknown, although we speculate that the rate of outpatient CR in this population would be lower than that in our current study population.
We showed that the proportion of outpatient CR participation of post-operative heart disease patients was low in older people living in two cities. Men, those having myocardial infarction, those who had undergone inpatient CR participation, and those admitted in a hospital with a higher “hospital volume” for CR were more likely to receive outpatient CR participation. There is a need to promote CR from admission to the hospital, and a system of CR referral for patients who cannot receive inpatient CR should also be developed. Appropriate support is also needed to encourage older Japanese women to participate in CR. Further studies will need to be conducted on a national database in Japan.
There are no conflicts of interest to declare.
This work was supported by a grant-in-aid from the Ministry of Health, Labour and Welfare Policy Research Grants, Japan (grant number: 21AA2007). The funder did not play any role in the conception, design, conduct, or reporting of this study. We would like to thank Editage (www.editage.com) for English language editing.