2021 Volume 7 Issue 1 Pages 67-72
2021 Volume 7 Issue 1 Pages 67-72
Abstract
Background: The myocardial perfusion stress conducted by physicians and nurses requires two imaging sessions, one during stress and the other during rest. Echocardiography is sometimes performed before delayed imaging, and medical laboratory technicians (MLTs) have similar exposure in such cases. This study was designed to investigate the radiation exposure of physicians, nurses, radiologists, and MLTs involved in thallium-201 chloride (201TlCl) stress myocardial perfusion imaging and echocardiography, the details of which have not been reported to date.
Methods: The dose rate at thallium-201 (201Tl) was examined using a cylindrical phantom. The exposure of physicians, nurses, and radiologists involved in the 201TlCl stress myocardial perfusion imaging was measured using pocket dosimeters, and that of the MLTs in charge of echocardiography were measured using glass-batch dosimeters.
Results: The attenuation of radiation exposure from the phantom with distance was 95% at 50 cm from the center of the phantom, demonstrated that the attenuation of the exposure dose increased with distance. The exposure dose for physicians, nurses, and radiological technologists that participated in 201TlCl stress myocardial perfusion imaging was 0.20–0.23 µSv per exam, whereas it was 6.67–10.00 µSv per exam for MLTs.
Conclusion: This study measured the dose received by physicians, nurses, and radiological technologists during stress MPI and the dose received by MLTs during echocardiography. The results provided advanced knowledge for the management of dose received by medical personnel.
Stress myocardial perfusion imaging (MPI) by single-photon emission computed tomography (SPECT) is currently performed in Japan with either thallium-201 chloride (201TlCl) or technetium-99 (99mTc) sestamibi or with 99mTc-tetrofosmin (99mTc myocardial perfusion agents: 99mTc-agents), both of which are labeled 99mTc. The imaging procedures for 201TlCl and 99mTc-agents are different; however, stress-early and rest-delayed imaging protocols are required for both preparations. Two types of myocardial stress methods have been used; exercise using an ergometer, and a treadmill and pharmacological stress using adenosine triphosphate, both methods involving the participation of physicians and nurses. Past presentations at conferences have reported that the exposure of medical staff to radiation in the stress MPI is between 0.2 µ5Sv and 3 µSv (1–4).
In some cases, echocardiography is performed on the same day as the procedure to make the best use of waiting time between examinations because the waiting time between stress and rest is 3 to 4 hours for 201TlCl, and 2 to 4 hours for 99mTc- agents. Recently, the medical laboratory technicians (MLTs) exposure to echocardiography performed on the same day for patients who underwent stressed MPI SPECT has become the MLTs exposure problem, and some facilities do not perform echocardiography on the same day as stress MPI SPECT. At our hospital, we perform the 201TlCl stress MPI SPECT, and in some cases, the echocardiography is requested and performed during the free time before redistribution imaging. MLTs who perform the echocardiography stay close to the patients, and it is presumed that they are exposed to a considerable amount of radiation.
We measured the dose of radiation received by physicians, nurses, and radiological technologists (medical staff) involved in 201TlCl stress MPI SPECT and MLTs dose when the echocardiographic examinations are held on the same day.
Methods
Measurement of dose rate by distance using a cylindrical phantom
First, the rate of attenuation of radiation with distance was measured using a phantom during 201TlCl. The cross-calibration (Figure 1) measurements for PET were conducted using a cylindrical phantom (21 cm in diameter×23 cm in length, 6.9 l in volume) that contained 111 MBq (16 kBq/ml) of 201TlCl. The gamma camera system E. CAM (Canon Medical Systems, Ltd, Tokyo, Japan) was installed on a hospital bed, and the air dose rate at each point was measured using a scintillation survey meter TCS-GD-130 (Hitachi Aloka Medical, Ltd, Tokyo, Japan; Figure 2). The measurement range was 20 points up to 200 cm horizontally at 10 cm intervals from the phantom centers, as shown in Figure 1. The measurement results were subtracted from the BG dose rate, and the attenuation of radioactivity was corrected for the measurement at the verification time. Similar measurements were also conducted for 99mTcO4-. The results are shown in the supplemental file.


Measurement of medical staff’s exposure during 201TlCl stress MPI SPECT
We assessed the radiation exposure of medical staff involved in 201TlCl stress MPI SPECT. The subjects were a cardiologist, a nurse, and a radiological technologist. The nurses assisted in the injection and observed the patients during the stress test, whereas the radiological technologist did not participate in the stress examination. We used the radionuclide 201TlCl 111MBq, which was administered at the time of overload. Stress MPI was performed 5 to 10 minutes after administering 201TlCl, and rest-delayed MPI was conducted 3.5 hours after the administration according to the imaging protocol.
Electronic pocket dosimeters, PDM-117 (Hitachi Aloka Medical, Ltd, Tokyo, Japan), were attached to nurses’ and radiological technologists’ chests for the measurements. However, the sizeable directional dependence of the pocket dosimeter might preclude accurate measurements of physicians in charge of the stress test, who do not have a frontal view of the patient. Therefore, the dosimeter was not placed on the body part, but was placed at the electrocardiogram (ECG) operation position next to the patient. The electronic pocket dosimeter was placed on a desk post at the same height as the patient, facing the patient, at the electronic medical record terminal operation position about 2 m away from the patient (Figure 3). We were used to measure the radiation dose during 61 examinations (21 exercise and 40 pharmacological stress) conducted on different days. We used these data to calculate the dose per examination.

MLTs’ exposure during echocardiography after 201TlCl stress MPI
In this study, we measured the exposure of the MLTs in the echocardiography examination before and after the control of exposure. The exposure control was carried out by registering MLTs as radiation workers under the Medical Service Act, and by conducting monthly dose measurements and health examinations for ionizing radiation.
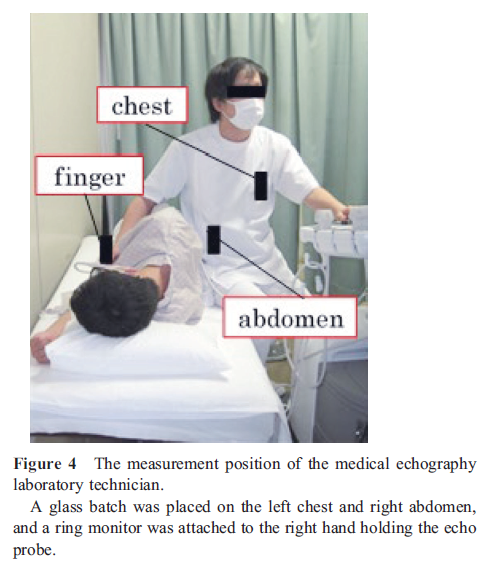
Measurements before exposure management
We conducted stress MPI on patients that requested this examination, and we measured the radiation dose of health care workers on the same day during echocardiographic examinations. Echocardiographic examinations were performed between 1 and 3 hours after stress. The examination time ranged from 10 to 15 minutes per patient. Three MLTs (one male and two females) had over ten years’ experience in echocardiography, whereas one had less than five to ten years’ experience, and another had less than five years’ experience. Glass-batch OSL dosimeters (Nagase Landauer, Ltd, Tsukuba, Japan) were placed on the left chest, and the right abdomen of MLTs’ conducting echocardiography, and a thermo luminescence dosimetry (TLD) ring monitor (Nagase Landauer, Ltd, Tsukuba, Japan) was placed on the right finger that held the echocardiographic probe (Figure 4). We examined 47 patients; 15 in the first month, 12 in the second, and 20 in the third month. The identical instruments were used in rotation by each MLT, and the integrated dose was considered as the exposure dose. In this study, echocardiography was performed between 1 and 3 hours after administering 201TlCl, since the physical half-life of 201Tl is 72.9 hours and the effective half-life, after considering the biological half-life, is 2.22 days (5). Therefore, the difference in measurement results due to radioactivity decay and excretion between 1 and 3 hours after administration was considered negligible.
Measurement after management
After the investigation described in Section 2.3.1, two male and two females MLTs in charge of echocardiography were registered as radiation workers and subjected to exposure management by wearing glass badges and ring monitors. Exposure dose were measured at the chest (abdomen for women), head, neck, and fingers. The study period was three months. Four MLTs in charge of the examination (3 MLTs described in Section 2.3.1 and one MLT with over ten years’ experience in echocardiography) were included in the study. The four MLTs performed 22, 11 and 30 examinations in the first, second and third months, respectively, for a total of 63 patients. The examinations were carried out by four MLTs in a distributed manner, and the dose were recorded for each individual.
Results
Dose rate by distance from the cylindrical phantom
The relationship between distance and dose rate of 201TlCl (111MBq) enclosed in a phantom is shown in Figure 5, and the relationship between distance and attenuation rate is shown in Figure 6. The phantom indicated that the highest dose rates after subtracting the BG dose rate (140 nSv/h) were found on the phantom’s surface at a distance of 10 cm: 201TlCl, 73.4 µSv/h. The attenuation rate was 95% at a distance of 50 cm from the phantom’s center if the phantom’s surface was considered as 1.0, which indicated that the exposure dose was significantly attenuated by distance.


Exposure of medical staff during 201TlCl stress MPI
The 201TlCl stress MPI results are shown in Table 1. The integrated dose at the physician’s ECG position were 8 µSv and 0.13 µSv per examination. Similarly, the cumulative dose for the physician at the medical record terminals’ position were 12 µSv and 0.197 µSv per examination. Moreover, the cumulative dose for nurses were 14 µSv and 0.23 µSv per examination. Additionally, the cumulative dose for radiological technologists were 12 µSv and 0.197 µSv per examination. Therefore, physicians, and radiology technologists had the same cumulative doses as physicians and radiological technologists and slightly higher for nurses. Assuming that the hourly dose from natural radiation was 0.14 µSv, the dose to the medical staff per examination was about 1 to 2 hours of natural radiation.

Post 201TlCl stress MPI exposure of MLTs
Measurements before exposure management
Table 2 shows the results of echocardiography performed on the same day as 201TlCl stress MPI. The detection limits for glass and ring batches were 100 µSv and 200 µSv, respectively. The cumulative doses at the left chest in the three MLTs were below the detection limit in all three months. Cumulative doses at the right abdomen were below the detection limit in a month (12 cases), while doses of 100 µSv were detected in the two months (35 cases). The cumulative dose at the right finger was below the detection limit in the first month (15 cases). However, in the remaining two months (32 cases), the cumulative radiation dose of the three MLTs was 200 µSv. The cumulative doses per echocardiogram for MLTs were calculated to be less than 5.0 µSv for the left chest, 5.0–6.67 µSv for the right abdomen, and 6.25–10 µSv for the right hand.

Measurements after management
The results of the measurements after exposure management are shown in Table 3. The monthly results show that the radiation exposure of all the MLTs was below the detection limit. Therefore, even if the echocardiogram was performed on the same day as the 201TlCl stress MPI, the MLT’s radiation exposure dose was at a level at which it was undetectable in the glass batch.

Discussion
The airborne dose of 201TlCl (111MBq) was measured by using a phantom. The results indicated that the rate of attenuation increased rapidly with the distance compared to the surface dose. If the surface dose was assumed to be 1, then the dose was reduced by 70% at 10 cm and by 85% at a distance of 20 cm, demonstrating that a slight increase in the distance could reduce the exposure dose.
However, the pharmacokinetics of drug accumulation and excretion are different in the actual human body, and therefore, the phantom experiment is expected to be slightly different from that in the human body.
On the other hand, Kashikura et al. reported exposure of 4.9±1.7 µSv/h at 50 cm of the site during 201TlCl stress MPI (1), which is slightly different from the present result of 3.3 µSv/h. However, if we consider that the lower limit of the Kashikura et al.’s result is 3.2 µSv/h, possibly, there was no difference between the present and Kashikura et al.’s result. The difference between the two is that the present study was conducted on a phantom and measured with a scintillation survey meter, while the former was conducted on a human body and measured with an ionization chamber survey meter. Considering these differences, it can be inferred that the dose rate in the vicinity of 50 cm is at least about 3.2 µSv/h.
Clouvas et al. measured the absorbed dose rate from 201TlCl patients at 1 m and reported that the total absorbed dose from the air for a patient at 1 m was 0.03 mSv (2). They showed hourly absorbed dose rates for the time elapsed after the administration of 129 MBq, ranging from 0.25 to 0.3 µSv/h, 25 minutes after the injection of 201TlCl. In their study, the absorbed dose rate was administered to a patient weighing 99 kg, but in our study, it was 1.1 µSv/h at a distance of 1 m, which was lower than the results of Clouvas et al. However, the results are considered reasonable considering the body weight and the dose of radioactivity administered.
Physicians and radiological technologists conducting 201TlCl stress MPI were exposed to approximately 0.2 µSv per examination, consistent with the exposure dose of radiological technologists in Yoneda et al. (3). The exposure of the medical staff depended greatly on the distance between the medical staff and the patient, and movement lines of the medical staff after administering radiopharmaceutical to the patient showed that most of them were in contact with the patient at a distance of 1 m or more. Although there is a possibility of contact with the patient within a distance of 1 m during electrocardiography, sphygmomanometer attachment/detachment, needle removal, and positioning with gamma camera equipment, but the exposure dose for these operations was low because they were conducted in a short time. The physician’s exposure dose was slightly higher at the electronic medical record terminals’ position than at the electrocardiogram’s position, but this may have been due to the difference in the way the exercise and drug loads were administered. The time from the radiopharmaceutical administration to SPECT imaging differed between exercise and pharmacological stress, and the electronic medical record terminal’s position differed between pharmacological stress and exercise conditions. The number of pharmacological stress patients in this study exceeded exercise patients. In addition, during pharmacological stress, the ECG was closer to patients than the electronic medical record terminal. Therefore, we speculated that the position of the ECG manipulation might have been slightly more prominent. However, these are positional problems that are unique to our hospital. Therefore, it can be generally considered that the exposure dose would be small if the distance to the patient is about 1 m.
The exposure dose to the surgeon during echocardiography performed on the same day as the 201TlCl stress MPI was higher in the hand, abdomen, and chest, in that order, and the exposure dose to the hand was 6.25 to 10 µSv. The reasons for this were considered to be the fact that echocardiography is a procedure in which the distance from the patient is close and the exposure time at close proximity to the patient is long, ranging from 10 to 15 minutes. If we consider the minimum value of 100 µSv to be detected in a glass batch as the standard, and if we assume that one inspection using 201TlCl takes 10 to 15 minutes, we can estimate that the glass batch will be detected after 13 to 15 inspections. In the report by Suzuki et al. (4), the right upper abdomen of an echo patient was measured with a pocket dosimeter at 3 µSv, and our value was higher than that reported by Suzuki et al. One possible reason for this is that Suzuki et al. measured doses using pocket dosimeters, and the directional dependence of the dosimeters may have caused their results to differ from ours. Therefore, MLTs performing echocardiography tended to have a higher dose during stress MPI than medical staff, but dose was reduced by exposure control. There was no difference in the measurement methods or units before and after the exposure management, but since the glass batches could not detect doses below 100 µSv, the detected values were divided by the number of inspections to calculate the dose per inspection. After exposure management, MLTs performing echocardiography were registered as radiation workers, which increased their awareness of radiation exposure. In addition, the number of MLTs in charge of echocardiography was increased and the number of examinations per person was distributed.
In the present study, the number of examinations per MLTs performing echocardiography after exposure management was not known, but dividing the number of examinations decreased the number of examinations per person, resulting in a reduction in the exposure dose to each person.
Conclusion
We assessed the radiation exposure received by physicians, nurses, and radiological technologists involved in 201TlCl stress MPI and MLTs involved in echocardiography performed on the same day as the MPI. Results indicated that the exposure dose to physicians, nurses, and radiological technologists conducting 201TlCl stress MPI ranged from 0.2 to 0.23 µSv per examination. The dose to MLTs ranged from 6.67 to 10.0 µSv per examination, but it decreased to a level detectable in the glass batch due to exposure management.
Acknowledgments
We want to thank Hiromi Tsuchiya and Takafumi Nagaya, in the Department of Clinical Laboratory Medicine, at the Gifu Prefectural Tajimi Hospital, for their cooperation in this study. We also wish to thank MLTs in the Department of Clinical Laboratory Medicine, the physicians in the Department of Cardiology, and nurses in the Nuclear Medicine Department for their cooperation in conducting the measurements. Finally, we would like to express our gratitude to Prof. Takashi Kudo of the Atomic bomb disease institute at the Nagasaki University for his cooperation in correcting the language.
Sources of funding
None.
Conflicts of interest
The authors declare that they have no conflict of interest with the findings of this study.
References
1. Kashikura K, Kanaya S, Kashikura A, Kobayashi H, Maki M, Kusakabe K.Dose to the examiner from patients in nuclear medicine examinations. Kakuigaku 1996; 33: 477–83.
2. Clouvas A, Xanthos S, Antonopoulos-Domis M. Gamma ray spectrometry for the determination of absorbed dose rate in the air following myocardial perfusion scintigraphy with 201Tl. Radiat Prot Dosimetry 1997; 74: 97–101.
3. Yoneda K, Fukuda R, Tsuchiya T, Haramiishi K, Otamaru T, Fukuchi K. Exposure dose of technician in charge of cardio-nuclear medicine examination. Kakuigaku Gijutsu (proceeding) 2019; 39: 381.
4. Suzuki Y, Kurihara M, Shimada Y. Estimating echocardiography staff exposure after cardiac nuclear medicine examination. Kakuigaku Gijutsu 2007; 27: 137.
5. Bunko H, Tonami N, Hisada K. Evaluation of scanning condition and early organ accumulation with large field of view gamma camera in 201Tl myocardial scan. Radioisotopes 1976; 25: 794–9. [Article in Japanese]