2022 年 22 巻 1 号 p. 1-4
2022 年 22 巻 1 号 p. 1-4
Purpose: The purpose of this study was to analyse the correlation between the presence of temporomandibular joint (TMJ) effusion and limitation of mouth opening after arthroscopic surgery. Methods: The authors studied 88 joints in 86 patients with TMJ disorders who underwent lysis and lavage in the superior space of the TMJ. The patients were referred for magnetic resonance (MR) imaging before and after surgery. The joints were divided into two categories based on the presence of TMJ effusion. Chi-square tests were used to evaluate differences between distributions for these two groups. The alpha level was set to 0.05. Results: The number of joints with effusion decreased after surgery. However, after surgery, there was no significant difference between the distributions of TMJ effusion for TMJs with and without limitation of mouth opening. Conclusion: The amount of joint effusion in the temporomandibular joint decreased after surgery, but the effusion did not completely disappear even after the clinical symptoms improved. It was suggested that the joint effusion naturally accumulates in a vacant space, the upper joint space located in the lateral recess.
Temporomandibular joint (TMJ) effusion appears as an accumulation of increased signal on T2-weighted magnetic resonance (MR) images [1]. This condition has been recognized as an important clinical sign of the TMJ in patients with TMJ disorders; however, the clinical significance of TMJ effusion remains unclear. Many reports, including initial studies [2,3,4], have shown that TMJ effusion is associated with pain, although several investigations have questioned this relationship [5,6,7,8].
Arthroscopic surgery on the TMJ could influence the correlation between TMJ effusion and pain [9]. However, an earlier study showed that TMJ effusion on MR imaging could not be used as a predictor of treatment outcomes after arthroscopic surgery [10]. This issue may be complicated by the lack of important clinical symptoms, such as limitation of mouth opening, when evaluating outcomes after surgery. This consideration led the authors to investigate the relationship between limitation of mouth opening and TMJ effusion after arthroscopic surgery to discover the background of TMJ effusion.
The purpose of this study was to analyse the relationship between the presence of limitation of mouth opening and TMJ effusion in patients who underwent arthroscopic surgery and were referred to us for MR imaging.
The authors studied 88 TMJs in 86 patients suffering from TMJ pain and dysfunction who were referred to us for MR imaging of the TMJ (Table 1). These 86 patients underwent double-contrast arthrography of the TMJ space and lysis and lavage of the superior joint space combination with arthrocentesis when conservative treatments proved to be unsuccessful, as evidenced by manifestations such as pain and/or limitation of mouth opening, from 1993 to 2003.
Table 1 Distribution of the patients according to gender and age
| 10-19 | 20-29 | 30-39 | 40-49 | 50- | N * | |
|---|---|---|---|---|---|---|
| Male | 1 | 0 | 2 | 2 | 2 | 7 |
| Female | 9 | 32 | 15 | 9 | 16 | 79 |
| N* | 10 (11.6) | 32 (37.2) | 17 (19.7) | 11 (12.7) | 18 (20.9) | 86 |
*Number of joint (% in parentheses)
Patients with a history of systemic inflammatory disease, mandibular growth disturbance, or TMJ tumours were excluded from this study. All subjects provided explicit consent for participation in the study in accordance with procedures approved by the Ethical Review Board at Tsurumi University (approval number 867).
MR imaging was performed before and after arthroscopic surgery using a 0.4-tesla imager (Aperto Inspire, Hitachi Medico, Tokyo, Japan). T2*-weighted sagittal images (TR: 400 ms, TE: 14 ms, matrix size: 256 × 192, field of view: 120 mm, slice thickness: 4 mm) were acquired to diagnose temporomandibular disorders, and T2-weighted sagittal images (TR: 2,800 ms, TE: 105 ms, matrix size: 256 × 192, field of view: 120 mm, slice thickness: 5 mm) were acquired to diagnose TMJ effusion with bilateral TMJ surface coils (9 cm in size). The sagittal plane was set perpendicular to the long axis of the mandibular condyle. Arthroscopic surgery was performed in accordance with previous reports [11].
Based on the MR findings, the joints were classified into two groups using the criteria for the presence of TMJ effusion described by Westesson and Brooks [3] in 1992. MR images were evaluated by two oral radiologists. Each radiologist assessed each MR image to evaluate both the status of the TMJ and the presence of TMJ effusion. When the radiologists’ assessments differed, they re-evaluated the images and arrived at a mutually satisfactory assessment. Based on clinical records prior to MR imaging, the authors divided the joints into the two categories of joints with limitation of mouth opening and joints without limitation of mouth opening. Before and after arthroscopic lysis and lavage, joints with limitation of mouth opening were evaluated as allowing for less than 40 mm of mouth opening.
Chi-square tests were used to evaluate differences between distributions for the two relevant groups. The alpha level was set to 0.05 for this study.
The period between the first MR examination and arthroscopic examination ranged from 2 to 387 days, with a median of 34 days, and the period between arthroscopic examination and the follow-up MR examination ranged from 42 to 2875 days, with a median of 225 days.

Fig. 1 A corrected sagittal T2*-weighted image shows a TMJ from a 25-year-old female with limitation of mouth opening after arthroscopic surgery. She still has pain in the TMJ, and her maximal inter-incisal distance is 30 mm. The disc is located anterior to the condyle (white arrow). TMJ effusion is evident in the upper joint space (arrow heads); this phenomenon was also observed prior to arthroscopic surgery.
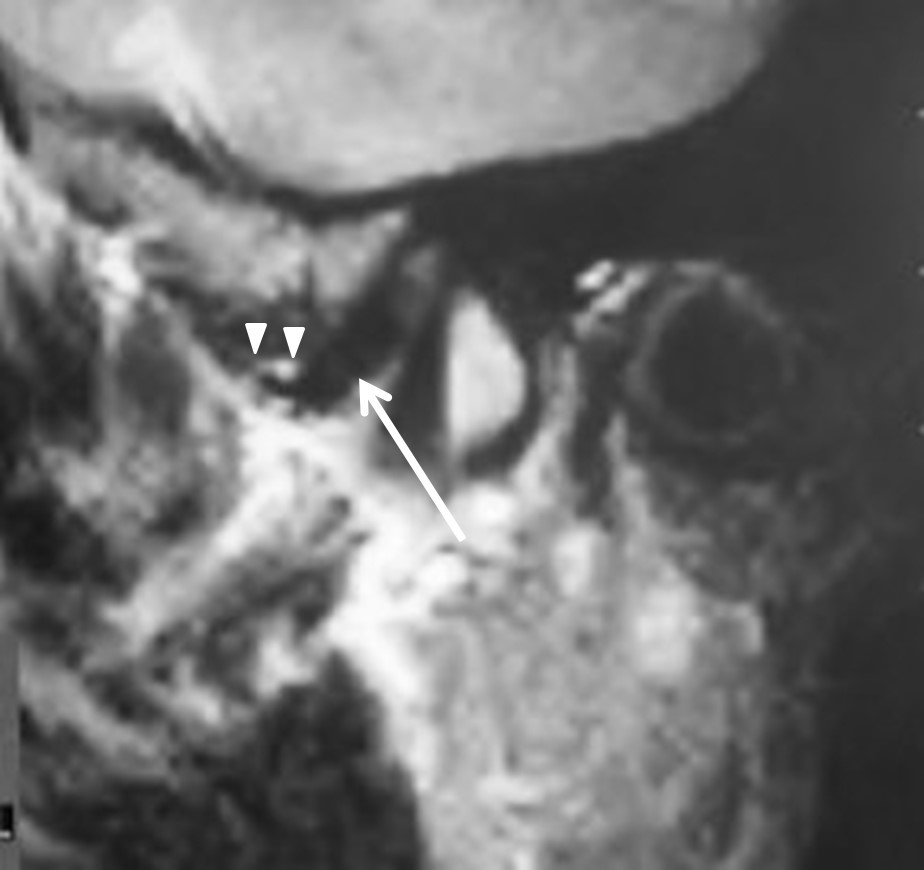
Fig. 2 A corrected sagittal T2*-weighted image shows a TMJ from a 32-year-old female without limitation of mouth opening after arthroscopic surgery. She has pain in the TMJ; however, her maximal inter-incisal distance is 50 mm. The disc is located anterior to the condyle (white arrow). TMJ effusion is evident in the upper joint space (arrow heads); this phenomenon was also observed prior to arthroscopic surgery.

Fig. 3 Changes in joints with effusion before and after arthroscopic surgery
Table 2 Prevalence of joints with limitation of mouth opening before and after surgery
| Before | After | |
|---|---|---|
| Limitation of mouth opening | 77 (87.5) | 17 (19.3) |
| Non-limitation of mouth opening | 11 (12.5) | 71 (80.7) |
| Average mouth opening distance (mm) | 29.7 ± 7.9 | 43.0 ± 6.3 |
| Median mouth opening distance (mm) | 28 | 43.5 |
Number of joint (% in parentheses)
Significant difference between the distributions before and after surgery based on a chi-square test (P < 0.05).
Table 3 Prevalence of joints with effusion before and after surgery
| Before | After | |
|---|---|---|
| Effusion | 31 (35.2) | 15 (17.0) |
| Non-effusion | 57 (64.8) | 73 (83.0) |
Number of joint (% in parentheses)
Significant difference between the distributions before and after surgery based on a chi-square test (P < 0.05).
Table 4 Prevalence of effusion after surgery for joints with and without limitation of mouth opening
| Limitation of mouth opening | Non-limitation of mouth opening | |
|---|---|---|
| Effusion | 3 (17.6) | 12 (16.9) |
| Non-effusion | 14 (82.4) | 59 (83.1) |
| Total | 17 | 71 |
Number of joint (% in parentheses)
No significant difference between the distributions for joints with and without limitation of mouth opening
The average mouth opening was 29.7 mm (S.D. 7.9 mm, median 28.0 mm) before surgery and 43.0 mm (S.D. 6.3 mm, median 43.5 mm) after surgery. The number of joints with limitation of mouth opening was significantly decreased after surgery (Table 2). There were significantly fewer joints with effusion after surgery than before surgery (Table 3). A comparison of TMJ effusion before and after surgery indicated that after surgery, effusion disappeared in 20 joints, appeared in 4 joints, and remained unchanged in 11 joints (Figs. 1-3). However, the prevalence of effusion in TMJs with limitation of mouth opening and TMJs without limitation of mouth opening were nearly identical (Table 4).
TMJ effusion is generally defined as the pathological collection of TMJ fluid in the joint spaces. This condition manifests as increased signal on T2-weighted MR images. To determine the significance of TMJ effusion, previous articles have focused on the correlation between joint effusion and clinical symptoms [2,3,4,5,6,7,8,12,13,14,15,16]. For the knee joint, MR imaging can be used to distinguish effusion from synovitis [17]. Westesson and Brooks [3] regarded images as showing joint effusion if more than one line of high signal was present in the upper or lower joint spaces on T2-weighted images. They found the frequency of joint effusion on MR images for various TMJ states, such as normal disc position, internal derangement and osteoarthritis.
Although Westesson and Brooks [3] and Murakami et al. [5] regarded more than one line of high signal as indicative of joint effusion, high signals are also visible on T2-weighted images of asymptomatic volunteers. The association between joint effusion and pain has been investigated several times and remains controversial [2,3,4,5,6,7,8,14,15,16]. In 1992, Westesson and Brooks [3] showed that the frequency of joint effusion is higher in more painful joints than in less painful joints and concluded that TMJ effusion was strongly associated with joint pain. However, Murakami et al. [5] showed that there was no significant statistical correlation between pain level and the presence of high signal on T2-weighted images and argued that joint effusion was somewhat inappropriate as a screening parameter for a painful TMJ. Sato et al. [10], Haley et al. [7], Larheim et al. [4], Rudisch et al. [8], and Yamamoto et al. [18] also reported the existence of a significant relationship between joint effusion and TMJ pain. In a longitudinal MR imaging study, TMJ pain was alleviated or resolved in all joints in which the quantity of fluid decreased [19]. Emshoff et al. also stated that the presence or absence of effusion may prove to be an important diagnostic determinant of successful arthrocentesis. However, the same authors [8] previously suggested that pain was not reliable for predicting the presence of effusion in a consecutive series of patients with TMJ pain.
On the other hand, marked improvements in arthroscopic findings and MR imaging over time must also be noted. An important milestone in the development of treatments for TMJ pain and dysfunction is the use of arthroscopic surgery [20] for the TMJ, which allows joint pain related to pathological conditions, such as adhesion in the joint space, to be decreased. In a prior study, a comparison of MR imaging before and after TMJ arthroscopic lysis and lavage indicated that changes in the level of joint effusion were not related to patients’ clinical conditions [10].
One study has concluded that TMJ effusion may be predictive of the clinical outcomes of TMJ irrigation in chronic closed lock patients [10]. Given the aforementioned background, TMJ effusion may become a predictor of outcomes after arthroscopic surgery. This present study does not describe any evidence of joint effusion in MR imaging as a predictor for evaluating joints in patients with limitation of mouth opening after arthroscopic surgery. However, in this study, there were significantly fewer joints with effusion after arthroscopic surgery than before surgery. It has been suggested to be effects of the arthroscopic surgery and arthrocentesis. However, the limitation of mouth opening improved, but TMJ effusion remained. It has been suggested that TMJ effusion is a pooling of synovial fluid with no direct relation to inflammation [21]. The authors speculate that joint fluid naturally accumulates in a vacant space, the upper joint space located in the lateral recess, when anterior disc displacement occurs. However, it has been reported [22] that asymptomatic joints in which effusion has been detected should be followed up, bearing in mind that they may be candidates for intracapsular disorders, so the authors considered necessary to perform MR studies in the follow-up after treatment. To further clarify these issues, it is necessary to focus on detailed observations, including observations of clinical symptoms, when performing a longer-term investigation of TMJ effusion.
Conflict of Interest
The authors have no conflicts of interest directly relevant to the content of this article.