2022 年 22 巻 2 号 p. 29-32
2022 年 22 巻 2 号 p. 29-32
Purpose: A radiopaque self-polymerizing adhesive resin was prepared by incorporating bismuth subcarbonate-poly(methyl methacrylate) prepolymerized composite (BS-PMMA) into an acrylic resin. The purpose of this study was to evaluate the radiopacity of prepared resins. Methods: As a radiopaque component, a composite containing 50% bismuth subcarbonate was used, and other metal compounds were adopted as controls. They were added to finely pulverized PMMA. Specimens were prepared from the powders, methyl methacrylate (MMA) monomer with 5% 4-methacryloyloxyethyl trimellitate anhydride (4-META) and tri-n-butylborane derivative (TBB) by mixing. Radiographs of the specimens were taken together with tooth slices and aluminum step wedges. The density of the specimens was determined with a densitometer and was expressed in terms of the equivalent thickness of aluminum per 2.0 mm unit thickness of specimen. Results: The radiopacity value of BS-PMMA-based specimen was 3.7 mm Al / 2.0 mm specimen, which was nearly the same value as enamel (3.7) and exceeded the values of dentin (2.0). Conclusion: BS-PMMA composite and bismuth compounds are useful as a radiopaque additive for the acrylic resin.
Radiopacity is one of the prerequisites for dental materials. A methyl methacrylate (MMA)-based acrylic adhesive resin (Super-Bond C&B, Sun Medical Co., Ltd., Moriyama, Japan) has been used to bond tooth structure and restorative materials in combination with various conditioning agents and primers. It has been impossible, however, for clinicians to detect the material on the radiographs because of the lack of a radiopaque element in the composition.
The bismuth compound is one of many reported in dentistry as radiopaque. Historically, Grossman [1] used bismuth subcarbonate as a radiopaque component in his original root canal sealer. Bursey and Webb [2] incorporated various metal compounds, including bismuth subcarbonate, into acrylic denture base material. Other bismuth derivatives reported for radiopaque denture materials were bismuth glass [3,4], bismuth subnitrate [5,6], bismuth tribromide, bismuth trichloride [6,7] and triphenyl bismuth [8,9]. Bismuth compounds thus appear to be more acceptable as radiopaque materials than other compounds [10,11,12,13].
However, the addition of a large amount of these compounds to acrylic resin adversely affects the handling and physical properties. This article describes the use of bismuth subcarbonate-poly(methyl methacrylate) prepolymerized composite (BS-PMMA) as a radiopaque medium for acrylic resin, and reports the radiopacity values of the prepared resins.
The original acrylic adhesive resin consisted of three components: powder, monomer liquid and initiator. The powder was finely pulverized poly(methyl methacrylate) (PMMA) having a number average molecular weight of 100,000 (Super Bond Polymer, Sun Medical Co., Ltd.). The monomer liquid included 95% methyl methacrylate (MMA) and 5% 4-methacryloyloxyethyl trimellitate anhydride (4-META). The initiator was partially oxidized tri- n -butylborane (TBB).
Radiopaque compounds were incorporated into the composition in this investigation (Table 1). Bismuth subcarbonate-poly(methyl methacrylate) prepolymerized composite (BS-PMMA, an experimental production, Sun Medical Co., Ltd.) that contained 50% bismuth subcarbonate by weight was the radiopaque medium for resin. Barium sulfate, bismuth oxide, bismuth subcarbonate without coating, and zirconium oxide were used as controls. These were added to the PMMA powder prior to curing of the resin specimens. The final concentration of the radiopaque compound in the specimens was 15.1 to 22.8% (Table 2).
Table 1 Radiopaque compounds incorporated into the acrylic resin
| Compound | Component | Lot number | Manufacturer |
|---|---|---|---|
| Barium sulfate | BaSO4 | SAQ 3715 | Wako Pure Chemical, Osaka, Japan |
| Bismuth (III) Oxide | Bi2O3 | ECN 6705 | Wako Pure Chemical |
| Bismuth subcarbonate | (BiO)2CO3 | SAL 3103 | Wako Pure Chemical |
| BS-PMMA composite | 50 BS / 50 PMMA | BSC 9303 | Sun Medical Co, Ltd., Moriyama, Japan |
Table 2 Composition of prepared resins
| Group | Liquid (g) | Total powder | PMMA | Radiopaque powder | Setting time* | |||
|---|---|---|---|---|---|---|---|---|
| (g) | (g) | (g) | (g) | (wt%) | (vol%) | (min) | ||
| BiO-40V | 0.188 | 0.247 | 0.148 | Bi2O3 | 0.099 | 22.8 | 40 | |
| BiO-15W | 0.188 | 0.190 | 0.133 | Bi2O3 | 0.057 | 15.1 | ||
| BiC-40V | 0.188 | 0.183 | 0.110 | (BiO)2CO3 | 0.073 | 19.7 | 40 | |
| BiC-15W | 0.188 | 0.190 | 0.133 | (BiO)2CO3 | 0.057 | 15.1 | 35 | |
| BiP-15W | 0.188 | 0.190 | 0.076 | BS-PMMA | 0.114 | 15.1 | 14 | |
| BaS-40V | 0.188 | 0.168 | 0.101 | BaSO4 | 0.067 | 18.8 | 40 | |
| BaS-15W | 0.188 | 0.190 | 0.133 | BaSO4 | 0.057 | 15.1 | ||
| UFR-0 | 0.188 | 0.150 | 0.150 | 0 | 0 | 9.5 | ||
*ISO 9917-2: 2017 (MOD), load 300 g
Table 3 Radiopacity values of acrylic resins
| Group-40V | Radiopacity value* | Category** | Group-15W | Radiopacity value* | Category** | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| BiO-40V | 6.9 | 0.1 | BiO-15W | 4.2 | 0.2 | a | ||
| BiC-40V | 5.4 | 0.2 | BiC-15W | 3.8 | 0.5 | a, b | ||
| BiP-15W | 3.7 | 0.2 | b | |||||
| Enamel | 3.5 | 0.1 | Enamel | 3.5 | 0.1 | b | ||
| Dentin | 2.0 | 0.2 | Dentin | 2 | 0.2 | |||
| BaS-40V | 1.6 | 0.1 | BS-15W | 1.1 | 0.1 | |||
| UFR-0 | less than 1.0 | UFR-0 | less than 1.0 | |||||
*mm Al / 2.0 mm specimen
**Identical letter indicate that they are not statistically different ( P > 0.05).
Monomer liquid, initiator and powder of the TBB-initiated resins were mixed in the ratio shown in Table 2, poured into Teflon molds (10.0 mm in diameter by 2.2 mm height) and polymerized between two pieces of glass plate at 25˚C. After 24 h, the specimens were sanded with #600 silicon-carbide paper to obtain 2.0-mm-thick specimens. In addition to these specimens, pure aluminum step wedges consisting of 1.0 to 24.0-mm-thicksteps were prepared using 99.99% aluminum metal. Each resin specimen was placed together with aluminum step wedges on an occlusal radiographic film (DF-49, Eastman Kodak Co., Rochester, NY, USA). Radiographs were taken with a dental x-ray source (DFW-20, Asahi Roentgen, Kyoto, Japan) using exposure factors of 0.6 s at 60 kVp, 15 mA with a target-film distance of 35 cm. The total filtration on the X-ray beam was 2.0 mm aluminum. The films were developed at 20˚C for 4 min. The radiographic density of the films was measured with a densitometer (PDA-15, Konica Medical, Tokyo, Japan) [14]. The radiopacity values of the specimens were expressed in terms of the equivalent thickness of aluminum per 2.0 mm unit thickness of material. For each condition, the mean value and standard deviation of six replications were calculated. The values of human enamel and dentin were quoted from the previous report [14], in which methodology and sample size were the same as the current experimental setting. The radiopacity values, except for unfilled resin specimen, were compared by analysis of variance and Tukey's multiple comparison intervals with the value of statistical significance set at the P < 0.05 level. The morphological structure of radiopaque compounds was observed by means of a scanning electron microscope (S-520, Hitachi-Hightechnologies, Tokyo, Japan). In addition, setting time of selected specimens was determined according to the method described in the ISO 9917-2: 2017 (MOD).
The radiopacity values of the 2.0-mm-thick resin specimens, enamel and dentin are presented in Table 3. Although there are differences among the weights of the powders used in group-40V, the powders were all equal in volume and each contained 40% by weight of a radiopaque compound in the powder part. Specimens of group-15W were prepared with an identical powder/liquid ratio so as to obtain a uniform final content of radiopaque component. The BS-PMMA composite consisted of an equal amount of bismuth subcarbonate and PMMA. The actual weight of radiopaque compound in BiP-15W was therefore one half of 0.114 g (0.057 g), which was the same quantity as that in other group-15W specimens.

Fig. 1 Scanning electron micrograph of bismuth (III) oxide (a), barium sulfate (b), and pulverized unfilled PMMA powder (c)
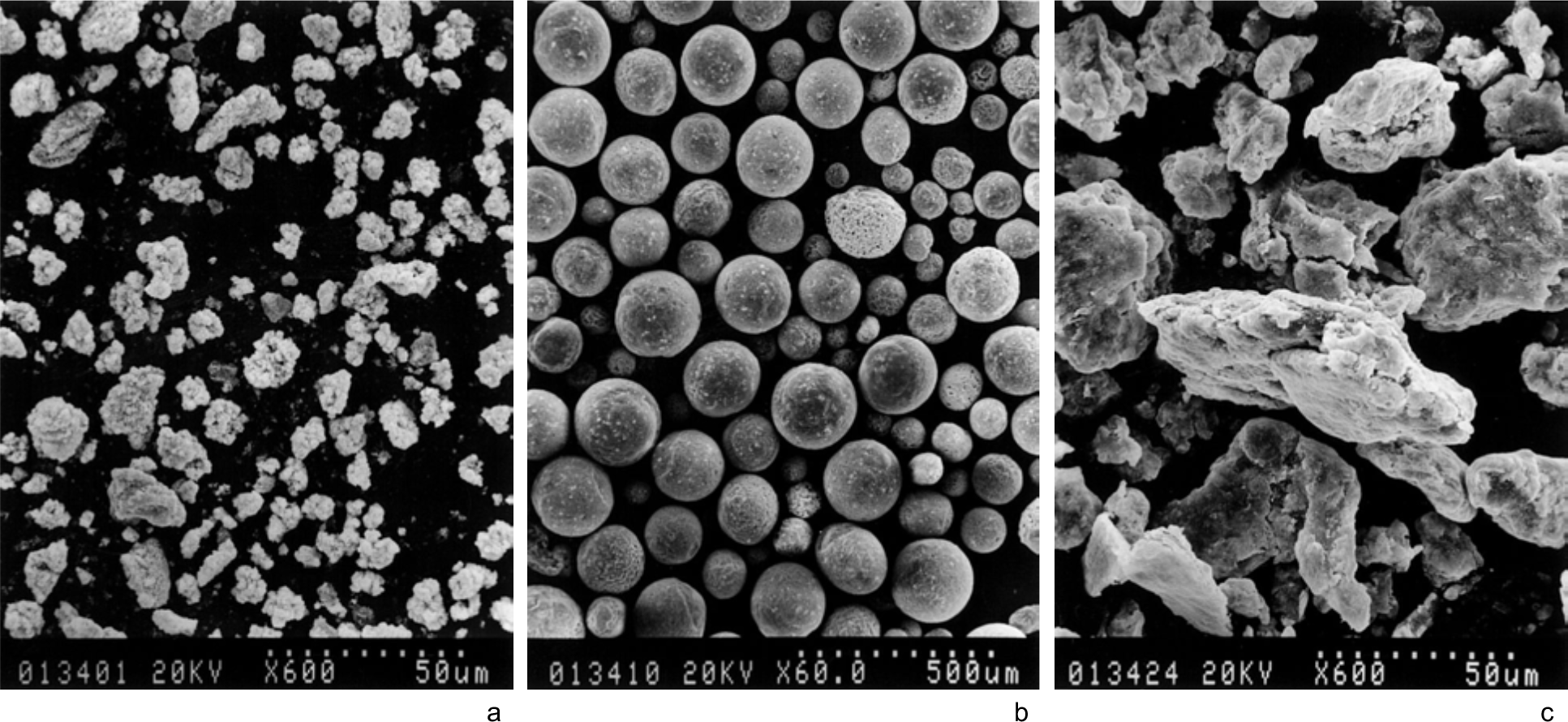
Fig. 2 Scanning electron micrograph of bismuth subcarbonate (BS) (a), BS-PMMA composite (b), and pulverized BS-PMMA (c)
In both group-40V and group-15W, the specimens containing bismuth oxide showed the highest radiopacity values, followed by bismuth subcarbonate, and barium sulfate. A radiopacity value equal to or greater than that of enamel was obtained by the incorporation of bismuth compounds in proportions greater than 15% in the composition of the acrylic resin. Specimens with 18.8% barium sulfate had a radiopacity value lower than dentin. The statistical analysis of radiopacity values for acrylic resins is summarized in Table 3. Significant difference in radiopacity value was not found between the groups BiO-15W and BiC-15W ( P > 0.05). Also, difference among the BiC-15W, BiP-15W, and enamel was not statistically significant ( P > 0.05).
Figure 1 shows scanning electron micrographs of powder component of the acrylic resin. Particle size of bismuth (III) oxide and PMMA was in the range 10-50 µm, whereas barium sulfate demonstrated fine submicron structure. Commercially available bismuth subcarbonate exhibited somewhat smaller particle size as compared with bismuth oxide (Fig. 2a). Figure 2b shows prepolymerized spherical particle consists of bismuth subcarbonate and PMMA (BS-PMMA). Fig. 2c is a micrograph of pulverized BS-PMMA incorporated into the acrylic resin. Surface structure of the bismuth particle is not distinct after pulverization of the PS-PMMA composite.
Setting time of selected three materials was determined and the results are shown in Table 2. Although setting time of the acrylic resin extended from 9.5 min to 35.0 min through the 15% incorporation of bismuth subcarbonate into the PMMA powder. Setting time, however, was shortened from 35 min to 14 min by incorporation of BS-PMMA composite instead of bismuth subcarbonate.
The TBB-initiated acrylic resin has displayed various functions with the use of additives. Matsumura and Nakabayashi [15] reported the use of PMMA-coated titanium dioxide for the preparation of adhesive opaque resin. The coated titanium dioxide was an excellent pigment to make the resin optically opaque. Radiopacity, however, could not be achieved by titanium dioxide because of the high radiolucency of titanium atom. In the current investigation, various radiopaque compounds were incorporated into acrylic resin and the radiopacity values were determined. The radiopacity value of the specimen containing 18.8% of the typical radiopaque reagent barium sulfate (BaS-40V) was below that of dentin and therefore insufficient.
With regard to the two bismuth compounds used, the oxide seemed to be superior to subcarbonate with respect to the radiopacity. Taking into account stability, toxicity, and color, bismuth subcarbonate was selected as a radiopaque additive for the acrylic resin. With the incorporation of 15% bismuth subcarbonate into the composition, the 4-META resin showed a radiopacity value equal to enamel. Two major problems associated with the incorporation of large amounts of bismuth subcarbonate have been the prolongation of setting time and the poor handling property. BS-PMMA prepolymerized composite was used to alleviate these disadvantages. With the use of BS-PMMA composite, clinicians will find no difference between the original and the radiopaque acrylic resin in handling, and they will be able to detect the material on the dental radiograph. In conclusion, BS-PMMA composite is applicable as a radiopaque additive for the TBB-initiated acrylic resin. Remaining concern is control of setting time.
Acknowledgments
The authors wish to thank Sun Medical Co., Ltd. for the preparation of BS-PMMA composite.
Conflicts of Interest
The authors declare no conflicts of interest.
Author contributions
NH and MS Performed experiments. Prepared the manuscript. MN Contributed to the research idea and experimental design. Proofread the manuscript.