2013 年 121 巻 3 号 p. 173-185
2013 年 121 巻 3 号 p. 173-185
This study provides a review of the skeletal manifestations of infantile scurvy and presents four cases observed in the Bácsalmás–Óalmás series (247 subadults and 234 adults; 126 males, 113 females, 242 unknown sex) dating from the 16–17th centuries AD. In the case of these four infants (aged 6 months–3 years) bilateral porous bone lesions were found on the external surface of the cranial bones. In three cases, these features were associated with porous new bone formations and/or abnormal blood vessel impressions in the internal surface of the skull. Moreover, porotic alterations of the long bones occurred in all cases and were mostly symmetrically developed. In order to confirm the origin of the observed features, the lesions were investigated using microscopic techniques. Analyses of the cross sections provided similar results in each case: newly built bone formations were visible on the external bone surfaces. These new bone layers are only found externally to the original bone surfaces. Thus, the original bone substance was not affected. On the basis of the characteristics of the observed lesions and their topographic distribution in the skeleton, and, additionally, by the use of microscopic analyses, we can state that the most likely diagnosis is scurvy. Furthermore, the co-occurrence of anaemia was also confirmed in one case. Up to now, there has been no archaeological evidence of scurvy in Central Europe in this time period, although on the basis of historical sources, the occurrence of this disease was expected. Additionally, besides these four cases, there are numerous other possible cases of infantile scurvy in this population, which suggests that the diet of the examined individuals was probably poor in vegetables and fruits.
The observation of scurvy in the Bácsalmás–Óalmás series is an important part of our research project dealing with the palaeopathological reconstruction of the southern Slav populations from 16–17th century AD Hungary. In the current study, numerous cases were found with similar alterations: bilateral porous lesions on the skull and the postcranial skeleton that might be caused by scurvy. The authors present four of the 47 possible cases that best fitted the macroscopic descriptions of scurvy and exhibit the best state of preservation of all potential cases. Thus, these cases were chosen for more detailed investigation and to confirm the diagnosis via microscopic examinations. The aim of this study is to provide a review and to enhance our understanding of the skeletal manifestation of scurvy at the macroscopic and microscopic levels, and also to provide insight into the nature of this disease in archaeological materials.
Scurvy is a nutritional disease caused by prolonged vitamin C (L-ascorbic acid) deficiency in the diet. During evolution, humans lost the ability to produce ascorbic acid, thus they need to obtain this vitamin from dietary sources (Chatterjee, 1973; Nishikimi and Yagi, 1996). Ascorbic acid is found in a wide range of foods, especially in fruits and vegetables. However, access to these sources usually depends on climatic, geographic, social, or occupational circumstances, e.g. fruits (and thus ascorbic acid) are easily available in tropical areas, but in regions with cooler climates these sources are limited (Aufderheide and Rodríguez-Martín, 1998; Brickley, 2000; Brickley and Ives, 2008).
Vitamin C has diverse functions in the human body, including a role in the hydroxylation of lysine and proline in protocollagen, which is necessary for the formation of the helical structure of collagen. Therefore, vitamin C deficiency leads to weak and quickly destroyable molecules, resulting in defective connective tissues (Mussini et al., 1967; Barnes and Kodicek, 1972; Barnes, 1975). The consequences are the various features of scurvy, in particular weakened walls of blood vessels, bleeding and reduced osteoblastic activity with insufficient osteoid synthesis, and skeletal growth retardation (Aufderheide and Rodríguez-Martín, 1998; Ortner, 2003; Brickley and Ives, 2006, 2008; Vigorita et al., 2008).
The skeletal manifestations of scurvy in archaeological samples are more recognizable in infants than in adults. Because of the rapid growth of bone formations in infants and young children, the symptoms of scurvy develop quickly, while in adults this process is slow (Brickley and Ives, 2006; Stuart-Macadam, 1989). Concerning these bony changes, some possible diagnostic criteria have already been established for infantile scurvy (also called Barlow’s disease) in archaeological materials. On the one hand, radiographic examination of impaired bone formation has a possible diagnostic value: infractions (partial fractures) can be observed at the long bones’ metaphyses due to the weak bone structure and thin diaphyseal cortex of the metaphyses (Resnick and Niwayama, 1988; Aufderheide and Rodríguez-Martín, 1998; Brickley, 2000; Ortner, 2003). On the other hand, bleeding due to the fragile blood vessel walls can also cause bony changes. In infants, the widening of the metaphyses at the wrists, ankles and knees can be caused by haemorrhages into the interior of the bone. Similar widening can also develop due to bleeding at the costochondral junction of ribs (Aufderheide and Rodríguez-Martín, 1998; Ortner, 2003). However, the most remarkable alterations are the signs of subperiosteal bleeding. In children, the haematoma can easily lift the loosely attached periosteum from the bone surface triggering a bony reaction. Recent palaeopathological studies have focused on the latter phenomenon as a possible criterion (e.g. Ortner and Ericksen, 1997; Ortner et al., 2001; Schultz, 2001, 2012; Brickley and Ives, 2006).
Pioneering work has been done by Ortner and his coworkers (Ortner and Ericksen, 1997; Ortner et al., 1999, 2001) in an attempt to diagnose infantile scurvy palaeopathologically. Studying archaeological materials, they suggested that abnormal porosity on the bone surface expressed by fine holes typically less than 1 mm in diameter that penetrate the compact bone surface are signs of scurvy. This porosity is suggested to appear due to chronic bleeding caused by minor mechanical stress (e.g. physiological muscle contractions) that traumatize the defective blood vessels. The extravasated blood lifts the loosely attached periosteum and may trigger chronic inflammatory changes in the underlying bone as well as the formation of additional blood vessels, resulting in holes that penetrate the cortex. In serious cases, the abnormal porosity is accompanied by hypertrophic new bone formations. The most frequently affected site of the skeleton is the skull, especially the greater wings of the sphenoid, but the orbits, the maxillae, the zygomatic bones, the hard palate and the mandible may also show abnormal porosity. On the postcranial skeleton, the scapula as well as long-bone metaphyses can be affected. These criteria have been used in numerous studies (e.g. Ortner et al., 1999, 2001; Melikan and Waldron, 2003; Brickley and Ives, 2006; Brown and Ortner, 2011; Geber and Murphy, 2012).
However, Melikan and Waldron (2003) stated that the distribution and appearance of lesions in the clinical cases of scurvy they examined was completely different from any of the archaeological series where the diagnosis of scurvy was based on Ortner’s criteria. In the clinical cases, they observed large areas of new bone depositions on the frontal, parietal, and occipital bone, as well as on the roof of the orbits and the greater wings of the sphenoid bone. On the basis of their observations, Melikan and Waldron considered the criteria developed by Ortner et al. (Ortner and Ericksen, 1997; Ortner et al., 1999, 2001) ambiguous. They also point out that the cases reported by Ortner and co-workers were not clinically documented, and palaeopathological diagnostic criteria can only be derived from cases with known history (Melikan and Waldron, 2003). However, Brickley and Ives (2006), as well as Mays (2008), drew attention to a problem: the clinically documented cases are usually more severe cases of scurvy with well-developed bone lesions, while the less severe cases probably will not be present in such collections. In their interpretation, the contradiction between Ortner’s criteria and the results of Melikan and Waldron can be resolved by considering Ortner’s criteria as being indicative of early-stage scurvy, while more recent clinical cases (e.g. the samples of Melikan and Waldron) represent an advanced stage of the disease.
Schultz in his study dealing with histological methods in palaeopathology stated that the most characteristic scurvy lesions are due to subperiosteal bleeding, and these alterations are proliferative reactions that represent organized and then secondarily mineralized subperiosteal haematomas (Schultz, 2001). These changes are usually flat, porous lesions, but these proliferative reactions may reach enormous sizes in serious cases. They might appear bilaterally and are frequently found in the skull, particularly on the ectocranial surfaces, but sometimes also on the endocranial surface as well as in the area of the jaw. The shafts of the long bones are also often affected. The distribution of the lesions more or less corresponds to the opinion of Ortner and his coworkers, who, however, had not taken endocranial alterations into consideration. The latter location was also mentioned by Lewis (2004) and Carli-Thiele (1996).
The main feature of these lesions is that the proliferation of new bone formation is found only externally to the original bone surface which is not affected by the pathological process (except for the endocranial surface, where pressure atrophy may affect the internal lamina). This feature had been already described in an experimental study in an animal model by Murray and Kodicek (1949). However, these characteristics are only visible using light microscopy and thin ground sections (Murray and Kodicek, 1949; Carli-Thiele, 1996; Schultz, 1990, 2001, 2012).
This study was performed on the skeletal series of Bácsalmás–Óalmás from Hungary. The village of Bácsalmás is located in the southern part of the Danube–Tisza interfluve. There is a sandmine near the village in an area called Óalmás, where a 16–17th AD century graveyard was excavated. The excavation was carried out in three phases: the first phase was led by Erika Wicker in 1993, the second phase by Zoltán Polgár and László Pintér in 1995–1996, and the third phase by Erika Wicker in 2001–2003 (Wicker, 2008). During the three periods of excavation, 481 skeletons were unearthed, which are now stored and curated at the Department of Biological Anthropology, University of Szeged, Hungary.
On the basis of the archaeological findings, this population is supposed to have immigrated from the southern part of Serbia or Montenegro during the Turkish occupation of Hungary between 1526 and 1686 AD (Kovács and Tomka, 2003; Laszlovszky, 2003; Vaday, 2003; Wicker, 2008). The data show that the population of the cemetery subsisted on agriculture and animal husbandry. According to old Turkish defters (tax registries of the Ottoman Empire), these people raised mainly sheep and pigs, and grew cereals and very small amounts of vegetables (Başbakanlık Osmanlı Arşivi, Tapu defteri 554, 175 and 570, 135 in Wicker, 2008). These sources also suggest that this population was a poor and socially, economically, and geographically isolated group. Because of the sandy soil of the excavation site, most of the skeletons are in very good state of preservation, except the youngest (neonate and infant I) age groups (Wicker, 2008).
General osteological and palaeopathological analyses of the cemetery inhabitants was performed previously in the Department of Biological Anthropology, University of Szeged. The Bácsalmás–Óalmás series has been the subject of numerous publications dealing with general palaeopathological investigation (Lovász et al., 2005; Lovász, 2008), various palaeopathological cases (Horváth et al., 1994; Pálfi et al., 1996; Lovász et al., 2009), tuberculosis (Molnár and Pálfi, 1994; Pálfi et al., 1997; Pálfi and Ardagna, 2002; Maczel, 2003; Molnár et al., 2005; Marcsik et al., 2006; Pálfi and Molnár, 2009; Bereczki et al., 2009), as well as palaeomicrobiology (Haas et al., 1999, 2000; Zink et al., 2007; Neparáczki et al., 2011; Pósa et al., 2013).
In the course of the palaeodemographic analysis, data of former studies have been revised and the series re-evaluated. This work yielded 234 adults and 247 subadults in Bácsalmás–Óalmás; thus the subadult : adult ratio is 51.4% : 48.6% (Table 1). Infant mortality accounted for 43.5% of all deaths, with the highest mortality rate during the first stage of infancy (infant I) (26.6%). Only 12.3% of the individuals died during infant II stage and 4.2% as neonates. 7.9% of the individuals died during the juvenile stage. Adults represent nearly the half of the dead population with similar percentage in each age classes except the senile stage which shows a somewhat smaller percentage. The male : female ratio is 52.3% : 47.7%.
| Age class | Age cohort | Male | Female | Unknown | Total | ||
|---|---|---|---|---|---|---|---|
| n | % | ||||||
| Subadults, n = 247 (51.40%) | Neonatus | 20 | 20 | 4.2 | |||
| Infant I | 0–6 years | 128 | 128 | 26.6 | |||
| Infant II | 7–13 years | 59 | 59 | 12.3 | |||
| Infant ? | 0–13 years | 2 | 2 | 0.4 | |||
| Juvenile | 14–22 years | 11 | 8 | 19 | 38 | 7.9 | |
| Adults, n = 234 (48.60%) | Adult | 23–40 years | 33 | 51 | 1 | 85 | 17.7 |
| Mature | 41–60 years | 43 | 30 | 73 | 15.2 | ||
| Senile | + 61 years | 33 | 16 | 1 | 50 | 10.4 | |
| Unknown | 6 | 8 | 12 | 26 | 5.4 | ||
| Total | 126 | 113 | 242 | 481 | 100 | ||
The results of the palaeopathological investigation showed that pathological alterations occurred with high frequency. The abundance of minor developmental defects can refer to endogamy, which may indicate that this immigrated population probably did not have contact with the autochthonous Hungarian population (Merbs, 2004; Barnes, 2008; Kiss, 2008). The low number and the distribution of traumatic lesions show that this population presumably belonged to an agropastoralist group. In addition, the frequency of non-specific stress indicators (e.g. porotic hyperostosis, periostitis) and specific infections such as tuberculosis, were also high, which might indicate a poor state of health in the examined population (Lovász et al., 2005; Lovász, 2008).
The examinations concerning the detection of scurvy in the Bácsalmás–Óalmás series were carried out using macromorphological methods based on the observations of Schultz (2001) and also considering other papers, including Ortner and Ericksen (1997), Ortner et al. (1999, 2001), Brickley (2000), Ortner (2003), Melikan and Waldron (2003), Lewis (2004), and Brickley and Ives (2006, 2008). Therefore, we searched for bilateral porous lesions on the skeletons of infants. In order to confirm the aetiology, microscopic examinations were carried out in the four most probable cases. Samples were taken from bones showing suspicious alterations which are characteristic of scurvy. The undecalcified samples were embedded in special epoxy resin (von Hagens, 1979) and ground down to 50 and 70 μm thin sections (Schultz, 1988, 2001). The thin ground sections were analysed with plain and polarized transmission light using hilfsobject red first order (quartz) as compensator (Schultz, 1988, 2001).
The individual was identified as an infant aged 1.5–2 years. In the almost complete skeleton, extreme pathological alterations were discovered bilaterally on the skull and on the postcranial bones.
The external surface of the skull shows flat, porous, and also thick new bone formations in several areas. The alteration is most remarkable on the glabella (Figure 1A). Furthermore, the orbital regions of the frontal, the sphenoid and the maxillae all show bilateral and symmetrical fine porotic new bone formations. Similar alterations are seen on all surfaces of the zygomatic bones. Porous lesions are also apparent on the anterior surfaces of the maxillae surrounding the infraorbital foramina and below the anterior nasal spine (Figure 1B). The palatal surfaces of the maxillae also exhibit dense porous changes. In addition, both the external and the internal surfaces of the coronoid processes of the mandible display flat porous lesions which extend posteriorly into the mandibular notch and then to the base of the mandibular foramen. Fine porotic new bone formations are visible at various locations on the mandibular body and the mental eminences.

Pathological alterations in the individual from grave no. 381 (1.5–2 year old infant). (A) Ectocranial view of the frontal bone displaying porous new bone layers in the glabellar region. (B) Anterior surface of the maxillae showing porous lesions surrounding the infraorbial foramina and below the anterior nasal spine. (C) Endocranial view of the left parietal bone displaying newly built bone formations associated with abnormal blood vessel impressions. (D) Medial surface of the shaft of the left tibia showing dense porosity and post mortem damage.
Moreover, bilateral dense porous lesions can be seen on the temporal surfaces of the greater wings of the sphenoid, which continues on the temporal bones’ zygomatic processes and the adjacent region of the squamous part. The petrous parts of the temporal bones are also affected. Small areas of thin porotic new bone layers can be seen on the parietal bones surrounding all sutures and on the occipital bone most pronounced at the superior and inferior nuchal lines. There is no evidence of expanded diploë.
The internal surface of the skull also reveals severe lesions. Porous new bone forming a thick layer on top of the original bone surface can be detected over almost the entire endocranial surface of the frontal bone. Moreover, the temporal, parietal, and occipital bones show large areas of fine porous new bone plaques. On the upper parts of the parietal bones, the newly built bone formations are associated with abnormal, branching vessel impressions (Figure 1C). In addition, fine porotic lesions can be observed on the lesser wings of the sphenoid bone too.
The postcranial skeleton is also affected. Except both radii, each preserved long bone exhibits fine porous lesions. On the upper limb, the sternal ends and the anterior part of the shafts of the claviculae, the distal shafts of both humeri above the olecranon fossa, and the proximal ends of both ulnae below the radial notch are affected. Irregular porosity can also be detected in the supraspinous fossae of both scapulae. In addition, at the sternal ends of the ribs both the external and the visceral surfaces show porous new bone formation and widening.
On the lower limb, the dorsal and the medial surfaces of the shafts and the anterior surface of the distal metaphyses of both femora and the right shaft of the fibula (the left fibula is missing post mortem) display porous new bone. The porous lesions reach enormous size on the medial surfaces of the shaft of both tibia (Figure 1D). Widened metaphyses of the femora and tibiae are also observed.
For microscopic examinations, six samples were taken from the following bones: second left rib, mandible (right deciduous molar region), left orbit and right greater wing of the sphenoid bone. Samples from the rib exhibit vestiges of thin but well-organized new bone layers. Moreover, a slip-like newly built bone layer is visible on the orbital roof. On the sample of the sphenoid bone, short trabeculae are visible with extensive bridging (Figure 2A). Similar lesions are visible on each samples of the mandible; however, multiple layers are also observed (Figure 2B). The original surfaces are not affected in any examined bones.

Microscopic images of the pathological alterations in the individual from grave no. 381 (1.5–2 year old infant). (A) Transverse section through the right greater wing of the sphenoid bone: (a) reorganized new bone layer; (b) original external lamina. Magnification × 100. (B) Frontal section through an alveolus of the mandible (right 4th tooth): (a) secondary built woven bone; (b) original surface of the alveolus. Magnification × 16. Thin ground sections viewed in polarized transmission light using a hilfsobject red 1st order (quartz) as compensator.
On the well-preserved skeleton (identified as an infant aged 6 months) both the skull and the postcranial elements show porous lesions. There is a sharply demarcated porous new bone formation on the frontal bone at the glabellar region (Figure 3A). The orbits are also severely affected: the orbital surfaces of the frontal and the sphenoid bones, the right maxilla and the right zygomatic bone show dense porous lesions (the left maxilla and zygomatic bone are missing post mortem). Moreover, the temporal and the palatal surfaces of the right maxilla display flat porous alterations. On the internal and external surfaces of the coronoid processes of the mandible fine porotic new bone formations are visible, which externally continue to the mandibular notch and the posterior edges of the rami (Figure 3B). Small areas of flat porous lesions are seen on the external surface of the mandibular body, especially on the mental eminences.

Pathological alterations in the individual from grave no. 436 (6 month old infant). (A) Distinctly demarcated porous new bone formation on the frontal bone in the glabellar region. (B) Medial surface of the right coronoid process of the mandible exhibiting fine porotic new bone continuing to the mandibular notch and the posterior edge of the ramus. (C) Extreme porous lesions on the temporal surface of the right greater wing of the sphenoid. (D) Dense porous new bone on the dorsomedial face of the shaft of the right humerus.
Extreme porous lesions can be observed on the temporal surfaces of the greater wings of the sphenoid bone (Figure 3C). These lesions spread over the external surfaces of the temporal bones’ entire squamous and petrous parts as well as the zygomatic processes. The porous alteration extends also to the parietal bones covering approximately one-third of the surface of the bones around the squamous and lambdoid suture and also to the squamous part of the occipital bone. In addition, the bregmatic region of the parietal bones also exhibits porous lesions.
Endocranial lesions were also revealed in this case. Small areas of thin porous new bone apposition were found all over the endocranial surface of the frontal bone and lesser wings of the sphenoid. Similar lesions were found on both parietal bones, mostly located along the sagittal suture. Small plaques of new bone are also apparent on the internal surface of the occipital bone, although post mortem damage limits the observability of pathological processes. It is worth mentioning that the endocranial alterations in this case are less pronounced than in the previous one.
Regarding the postcranial skeleton of this individual, alterations were recognized on several bones. All preserved long bones (both humeri, left radius and ulna, right femur, both tibiae) show pathological lesions. In the case of the upper limb, the dorsomedial parts of the humeral shafts (Figure 3D), the anteromedial parts of the diaphysis of the left radius, and the anterolateral part of the shaft of the left ulna display dense porous lesions. Flat porous alterations are also seen in the supraspinous fossae of both scapulae. Moreover, on the external surfaces of the ribs, porous lesions were observed mostly at the angular parts and the sternal ends. Widened sternal ends of the ribs were also discernible. The lower limbs are also affected: the dorsal part of the diaphysis of the right femur and the dorsomedial parts of the shafts of the tibiae display flat porous lesions.
Samples for microscopic analyses were taken from the occipital, frontal, and left temporal bones. Ribs, the left scapula, the right clavicle, and the mandible were also sampled. The examinations revealed a thin slip-like layer of new bone on the internal surface of the frontal bone, the external surface of the occipital and temporal bones, the mandible and also the dorsal surface of the scapula (Figure 4A). Short, bridged trabeculae of newly built bone were found on the external surface of the frontal (Figure 4B) and the internal surface of the occipital bones and the ribs. Thick, well-organized bone formations were observed in the sample of the clavicle. There is also no evidence of pathological alterations on the original surfaces of the examined bones.
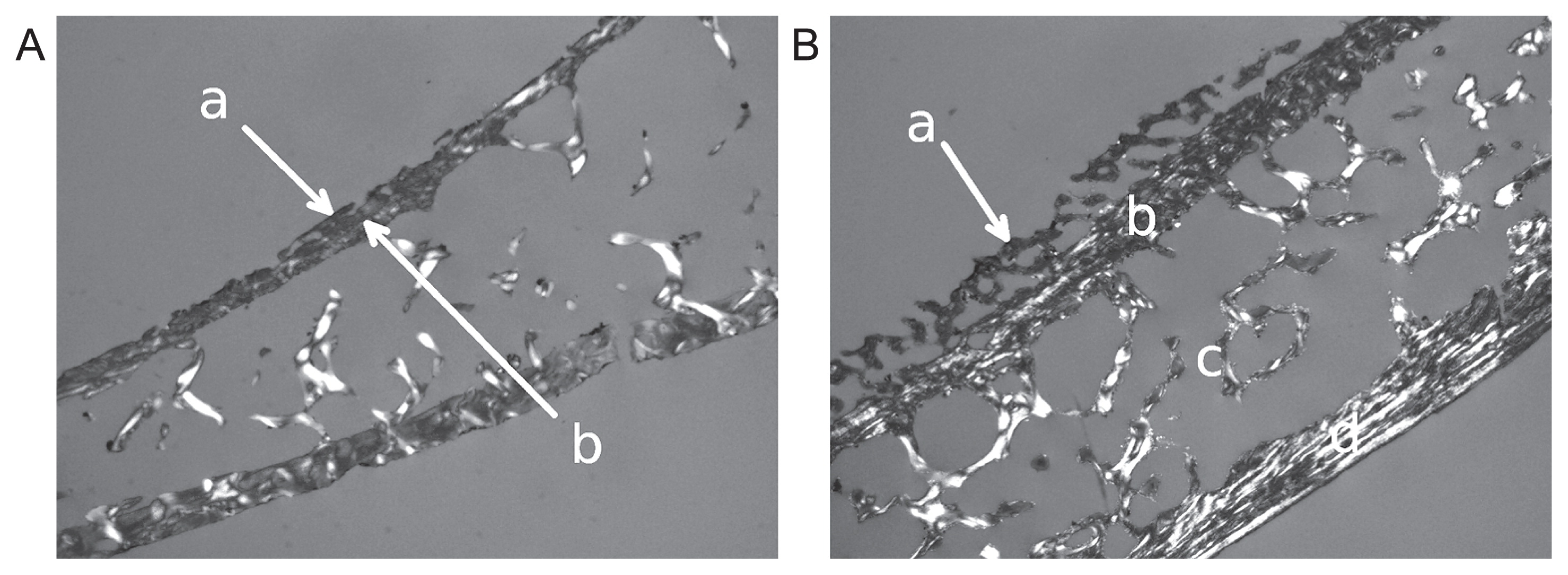
Microscopic images of the pathological alterations in the individual from grave no. 436 (6 month old infant). (A) Sagittal section through the left scapula: (a) slip-like layer of new bone on the dorsal surface; (b) original bone surface. Magnification × 16. (B) Sagittal section through frontal bone: (a) new bone formation on the external surface; (b) external lamina; (c) diploë; (d) internal lamina. Magnification × 16. Thin ground sections viewed in polarized transmission light using a hilfsobject red 1st order (quartz) as compensator.
The poorly preserved skeleton of an infant aged 1–1.5 years also displays porous alterations on the skull and the postcranial bones. Only a few parts of the skull are preserved: the glabellar region and small pieces of the orbital surfaces of the frontal bone, a few parts of the left parietal bone, the base and the left lateral part of the occipital bone, and the mandibular body. The pieces of the left parietal bone and the lateral part of the occipital bone show slight, flat porous lesions on their external surfaces. The mandibular body also displays flat porosity on the mental eminences. No pathological alterations of the glabella and the orbital parts of the frontal bone were found. Endocranial lesions were not observed on the preserved bones.
Besides the lesions of the skull, fine porotic alterations on the surfaces of each preserved long bone and some other postcranial elements were detected. On the upper limb, the lesions are located on the anterior surface of the sternal end of the left clavicle, the dorsal shafts of the left humerus (Figure 5A), and both radii (the right clavicle, the right humerus and both ulnae are missing post mortem). On the ribs, flat porous lesions were found on the external surfaces of the angular parts (Figure 5B). Widened sternal ends with increased porosity were observed as well (Figure 5C). In addition, slight porous lesions are visible on the supraspinous area of the right scapula (the left is missing post mortem).

Pathological alterations in the individual from grave no. 439 (1–1.5 year old infant). (A) Fine porotic alteration on the dorsal face of the shaft of the left humerus. (B) Flat porous lesions on the external surface of the angular part of the 9th right rib. (C) Widened sternal end with increased porosity of the 9th right rib; external view. (D) Flat porous lesions on the dorsal face of the shaft of the right femur.
On the lower limb, all surfaces of the femoral shafts (Figure 5D), medial surfaces of the tibial shafts and lateral surfaces of the fibular shafts show slight, flat porosity. Moreover, the distal metaphyses of the femora and the proximal metaphyses of the tibiae are widened.
Microscopic analyses were carried out on the samples of the left humerus, the right ulna, and the left tibia. Each sample showed similar results: short bone trabeculae with extensive bridging (Figure 6A, B). In the case of tibia and ulna, several layers of newly built bone were revealed. The original bone substance was not affected in any of the samples.

Microscopic images of the pathological alterations in the individual from grave no. 439 (1–1.5 year old infant). (A) Cross section through the right ulna: (a) newly built bone layers; (b) original cortical bone. Magnification × 16. (B) Cross section through the left tibia: (a) newly built bone layers; (b) original compact bone. Magnification × 25. Thin ground sections viewed in polarized transmission light using a hilfsobject red 1st order (quartz) as compensator.
The skeleton of an infant aged 2.5–3 years is almost complete and shows multiple symmetric areas of porous lesions on the skull and the postcranial bones.
Abnormal flat porous lesions can be detected on the glabella. Moreover, both orbits are severely affected: the orbital roofs display dense, porous, abnormal bone growth with associated vessel impressions (Figure 7A). This bony overgrowth is approximately 1.5 mm at the thickest point. The orbital surfaces of the sphenoid bone and both maxillae also show flat porous lesions. Besides these alterations, the palatal, temporal, and anterior surfaces around the infraorbital foramina of both maxillae also show porosity. Slight porous lesions are also visible on the anterior surfaces of the zygomatic bones. Moreover, the internal surfaces of the coronoid processes of the mandible also display fine porotic lesions that extend to the bases of the mandibular foramina. On the mandible, the oblique lines are covered with small patches of porous new bone.

Pathological alterations in the individual from grave no. 451 (2.5–3 year old infant). (A) Ectocranial view of the right orbital roof displaying dense, porous, abnormal bone growth with associated blood vessel impressions. (B) External surface of the right greater wing of the sphenoid exhibiting abnormal porous lesions. (C) Endocranial view of the right parietal bone showing well pronounced branching blood vessel impressions. (D) Fine porous lesions and slight and short blood vessel impressions on the dorsal face of the shaft of the right ulna.
Bilateral abnormal porous lesions can be observed on the external surface of the greater wing of the sphenoid (Figure 7B). These alterations also continue on the temporal bones’ zygomatic processes and on the whole squamous part. Abnormal porosity can be found on the surrounding area of the lambdoid suture on both parietals and the occipital.
Endocranial alterations are also discernible in this case. Fine porotic new bone formations are visible on the upper part of the frontal bone, accompanied by slight vascular impressions. Moreover, highly pronounced branching blood vessel impressions are apparent on the upper part of both parietal bones (Figure 7C). Thickening of the affected regions is also observable. Fine porosity can be seen in the sinus of the sagittal suture as well.
The postcranial skeleton of this individual also displays porous alterations. The upper limb bones show slight, fine porous changes on the anterior surfaces of the sternal ends of clavicles, lateral parts of the humeral shafts, the dorsal surfaces of the shafts of both ulnae (Figure 7D), and lateral surfaces of the shafts of both radii. Moreover, flat porous lesions can be detected on the supraspinous areas of both scapulae. Extended porosity and widening of the sternal ends of the ribs were observed as well. On the lower limb, the anterior and posterior surfaces of both femoral shafts, the medial and lateral surfaces of both tibial shafts, and the lateral surfaces of the shafts of both fibulae are covered with fine porotic lesions. However, the changes in the tibiae and fibulae can are barely visible to the naked eye. In addition, the distal ends of the femora as well as the proximal ends of the tibiae are widened.
Microscopic examinations were carried out on samples taken from the left orbit, the left parietal bone, and the right tibia. The sections through the parietal bone including the external and the internal lamina as well as the diploë and the cross section of the tibia show remains of thick, well-organized new bone formation (Figure 8A). There are no pathological changes in the original substance of the bones. On the external surface of the sample taken from the roof of the left orbit, very fine and thin layers of newly built woven bone and the onset of the orbital lamina’s reduction are visible (Figure 8B). Furthermore, there are abnormal trabecular formations in some regions of the orbital lamina and the external lamina of the left parietal where the original lamina is slightly reduced, though only in some parts. Such changes are sometimes found in the case of chronic anaemia. In the left orbital roof, a relatively pronounced change of the diploic trabeculae is observable which is characterized by a parallel packing of the trabeculae (Figure 8B, c). This morphological change of the diploë comes along with the formation of some small blood vessel canals which are radially oriented to the internal lamina and open out into the orbit, perforating the flat bone apposition on the orbital surface (Figure 8B, d). All these changes concede the case that we might have here an organized haemorrhagic process in a relatively advanced stage of healing. The locality inside the diploë is seemingly unusual and difficult to explain. Such changes on external bone surfaces are characteristic of chronic vitamin-C-deficiency in infants and young children.
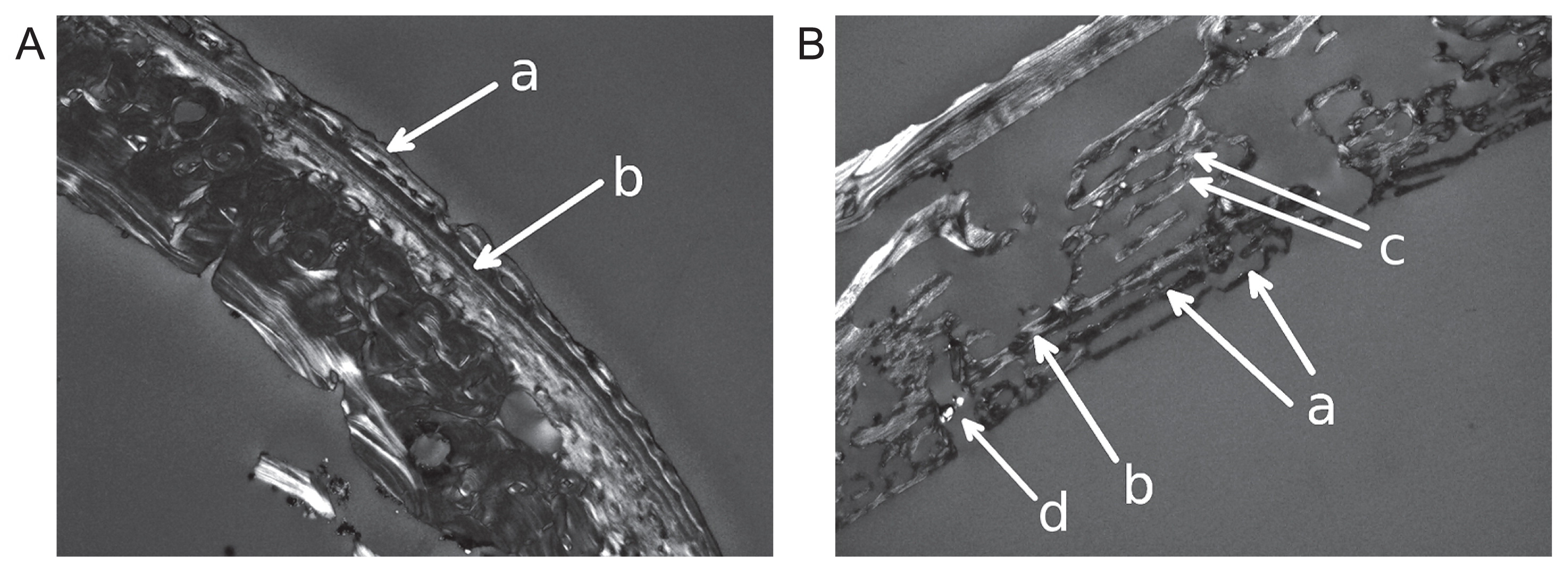
Microscopic images of the pathological alterations in the individual from grave no. 451 (2.5–3 year old infant). (A) Cross section through the right tibia: (a) well-organized new bone formation; (b) original compact bone. Magnification × 25. (B) Sagittal section through the left orbital roof: (a) secondary bone layers; (b) original lamella of the orbital roof; (c) parallel diploic woven bone trabeculae which are tangentially oriented to the external and internal laminae; (d) small blood vessel canal which perforates the original orbital lamina and has its opening in the newly built bone formation. Magnification × 16. Thin ground sections viewed in polarized transmission light using a hilfsobject red 1st order (quartz) as compensator.
On the basis of the macromorphological characteristics of the observed lesions, in all of the four cases the most likely diagnosis was scurvy. In the cases of grave no. 381, 436 and 451, advanced stages of scurvy were presumed because of the abundance of porous lesions. In the case of grave no. 439, the lesions are only slightly visible in the macroscopic assessment. Thus, an early stage of this disease was supposed. In the case of grave no. 451, the thickening of the parietal bones at the site of the endocranial lesions and the slightly visible porosity of the long bones indicate a possible healing process. In the latter case, the co-occurrence of an advanced stage of anaemia was also assumed because of severe porotic hyperostosis in the orbits.
However, several other diseases must be taken into consideration, since similar periosteal reactions can be caused by inflammatory processes of various origin (e.g. infectious conditions, such as sinusitis frontalis, non-specific periostitis and osteomyelitis or TB), rickets, anaemia, hypertrophic osteoarthropathy, or child abuse (Aufderheide and Rodríguez-Martín, 1998; Schultz, 2001, 2012; Ortner, 2003; Lewis, 2004; Wapler et al., 2004; Brickley and Ives, 2006). To exclude these aetiologies, we have to consider not only the macroscopic appearance of the lesions but also the distribution and the microscopic features of the alterations (Table 2).
| Cases | Macroscopic features | Microscopic features | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Porous lesions | Widening | Original bone substance | ||||||||||||
| Orbital roof | External surface of the skull vault | Endocranial surface | Ribs | Long-bone diaphyses | Long-bone metaphyses | Sternal end of the ribs | Affected | Not affected | ||||||
| Unilateral | Bilateral | Unilateral | Bilateral | Visceral surface | External surface | Unilateral | Bilateral | |||||||
| Grave no. 381 | − | + | − | + | + | + | + | − | + | + | + | − | + | |
| Grave no. 436 | − | + | − | + | + | − | + | +* | + | − | + | − | + | |
| Grave no. 439 | − | − | +* | −* | − | − | + | +* | + | + | + | − | + | |
| Grave no. 451 | − | + | − | + | + | − | + | − | + | + | + | + | + | |
| Possible aetiologies | ||||||||||||||
| Scurvy | − | + | − | + | + | +/− | + | − | + | + | + | +/− (only endocranial lesions) | + | |
| Inflammatory processes | sinusitis frontalis | +/− | + | − | − | + | − | − | − | − | − | − | + | − |
| non-specific osteomyelitis, osteitis | + | + | + | + | − | − | − | + | + | + | − | + | − | |
| non-specific periostitis | + | + | + | + | − | + | + | + | + | − | − | + | − | |
| non-specific meningitis | − | − | − | − | + | − | − | − | − | − | − | + | − | |
| TB | − | − | − | − | + | + | − | − | + | − | − | + | − | |
| Rickets | − | + | − | + | + | − | + | − | + | + | + | + | − | |
| Anaemia | + | + | + | + | − | − | − | − | − | − | − | + | − | |
| Hypertrophic osteoarthropathy | − | − | − | − | − | − | − | − | + | − | − | − | + | |
| Child abuse | + | + | + | +/− | + | − | − | + | +/− | − | − | +/− (only endocranial lesions) | + | |
Key: + characteristic for the condition; +/− not typical for the condition, but possible; − not characteristic for the condition;
The analyses of the cross sections yielded similar results in each case: newly built bone formations and/or remodelled new bone was/were visible on the bone surfaces. These new bone layers are only found externally to the original bone surfaces, and the original bone substance was not affected except for the sample of the left orbit of the case from grave no. 451. In this case we have also morphological changes which, apparently, were caused by anaemia. All these alterations are characteristics of subperiosteal haematomas (Schultz, 2001, 2012).
In the cases of grave no. 381 and 436, the microscopic images of the lesions revealed different morphological conditions of the haemorrhages: newly built bone layers and well-organized, remodelled bone tissue were detected in the same section showing different stages of a healing process. This was found in various elements of the skeleton of those two individuals. In the cases of grave no. 381 and 439, some samples displayed multiple layers of newly built bone which refer to recidivation (Schultz, 2001). Even though the individual from grave no. 439 seemed to represent a case of an early stage of scurvy on the basis of the macroscopic analysis, the microscopic examination revealed a far more severe stage. In the case of grave no. 451, each sample of the microscopic analysis showed only remodelled bone appositions, confirming our presumption of a healing process (Schultz, 2001).
In contrast to haemorrhagic processes, inflammatory processes always affect the original bone surface, and frequently also the deeper structures. Rickets also causes changes in the original bone substance, usually changing its microstructure completely (Schultz, 2001, 2012). Therefore, on the basis of the results of the microscopic examination, we can eliminate in these four cases the possibility of an occurrence of inflammatory processes of infectious origin or caused by rickets.
Microscopic images of porotic hyperostosis in chronic anaemia display a reduction of the external lamina of the skull vault and the orbital roof and/or radial orientation of the diploic trabeculae (Schultz, 1986, 2001, 2012; Wapler et al., 2004). Thus, anaemia can also be excluded in three cases (grave no. 381, 438 and 439). In the case of grave no. 451, the onset of the external lamina’s destruction in the orbital roof as well as the abnormal structure of the newly built bone formation are indicative of the coexistence of chronic anaemia and scurvy (Stuart-Macadam, 1989; Schultz, 2001, 2012; Wapler et al., 2004). Interestingly, the macroscopic observations suggested advanced stage of anaemia, since the outer morphology of the multiple layers of new bone mimics well-pronounced expanded diploë.
The microscopic images of the remaining possible aetiologies such as hypertrophic osteoarthropathy or child abuse are similar or the same, since subperiosteal bleedings are characteristic for all of these possibilities (Schultz, 2001, 2012). Therefore we have to consider the distribution pattern of the lesions.
In each of the presented cases, the skull and the postcranial skeleton (usually each long bone of the limbs and the ribs) were bilaterally affected. In the case of hypertrophic osteoarthropathy (caused by, for example, chronic pulmonary or heart disease), diffuse, bilaterally symmetrical, subperiosteal bone deposition on the bone shafts usually occurs. As a rule, these lesions affect the forearms and the lower legs, while involvement of the skull is not characteristic. Therefore, on the basis of the localization of the observed lesions, this diagnosis is unlikely (Aufderheide and Rodríguez-Martín, 1998; Ortner, 2003). Child abuse, such as “shaken baby syndrome” or other forms of abuse, might cause bleeding all over the body, including subperiosteal haemorrhages. However, bilaterally symmetrical appearance of the alterations is uncommon, and therefore the possibility of this aetiology is very low (Caffey, 1974; Kempe, 1985).
Considering the macromorphological and microscopic features of the lesions, the distribution pattern of the changes and their comparison with the features of the other possible aetiologies, we can establish the diagnosis of scurvy in each examined case. Moreover, the co-occurrence of anaemia was only confirmed in one case.
Besides these four cases, there are 43 other possible cases of infantile scurvy in the Bácsalmás–Óalmás series. However, we have to take into consideration that among these possible cases the macromorphological characteristics and the pattern of the lesions do not exclude the possibility of other aetiologies. The uncertainty of the diagnosis is also increased by the poor state of preservation in most of these cases. Thus, in the evaluation of the palaeoepidemiological data of scurvy we have to be very cautious. The four proved and 43 potential cases of scurvy suggest a remarkable 19% frequency among subadults. Among these cases 44.7% were younger than 1 year old, 31.9% were 1–2 years of age, and 23.4% were older than 2 years. These data correspond to the pathological literature that scurvy commonly occurs in infants between the ages 5 and 24 months and reaches its maximum prevalence between 8 and 10 months (Stuart-Macadam, 1989; Ortner, 2003; Brickley and Ives, 2006). Considering the age distribution of the affected children in this population, the possibility of false nutrition during or after weaning should be taken into account.
According to the Turkish tax registries (defters) the diet of this population was poor in vegetables and fruits (Wicker, 2008). Therefore the population of Bácsalmás–Óalmás had insufficient access to natural vitamin C resources which increased the risk of scurvy.
Chronic vitamin C deficiency could occur alongside other diseases, such as infections, which are also frequent in this population—many of these infectious cases might be due to TB infection. The large number of pathological alterations (including non-specific stress indicators such as porotic hyperostosis and periostitis) might refer to the poor state of health in this population. The very high infant mortality compared to neighbouring series also supports this finding (e.g. the palaeodemographical data of the Zombor–Repülőtér series, the closest known cemetery from the same archaeological period and same ethnic group, where the ratio of subadults : adults is 33.7% : 66.3% (Lovász, 2009a, b)). In the background to this phenomenon there might be several possible factors. This population immigrated most probably from the southern region of Serbia or Montenegro (Wicker, 2008), and had to adapt to a new environment which definitely induced stress phenomena. This stress might have been increased by the social, economical, and geographical isolation of this population. In addition, just like in the rest of Europe, the climate of the Carpathian Basin in the 16–17th centuries became extremely cold (the so-called “Little Ice Age”). In this period, the average temperature was significantly lower than in the years before or even today, and the winters were often quite hard and long. This climate provided adverse conditions for agriculture. Therefore hunger was frequent in this period (Glaser et al., 1999; Rácz, 2001). The political and military crisis during the Turkish occupation must have also contributed to frequent starvation of the people in this region. All these conditions might have affected this population too, causing decreased resistance to disease.
Up to now, no archaeological evidence of scurvy in Central Europe in this time has existed, although on the basis of historical sources, occurrence of the disease was expected (Réthly, 1962 in Rácz, 2001). Additionally, the scurvy cases described above give insights into the nature of this disease in archaeological materials, since not only the macroscopic, but also the microscopic features of the lesions were also presented. Our study provides an excellent example of the complementarity of macromorphological and micromorphological observations in palaeopathological practice and how microscopic techniques can reorient a diagnostic process in a case otherwise seemingly simple and easy to diagnose.
The study was supported by the Hungarian Scientific Research Fund, OTKA no. 78555 and 78696. Special thanks are due to the staff of the Department of Biological Anthropology, University of Szeged for their continuous help and support during the course of the study.