2020 年 2 巻 11 号 p. 701-702
2020 年 2 巻 11 号 p. 701-702
An 88-year-old man had severe aortic valve stenosis. Preprocedural contrast-enhanced computed tomography showed diffuse atheroma in the aorta (Figure A–C). The patient underwent transcatheter aortic valve replacement (TAVR) via the right femoral artery using a balloon-expandable valve. The next day, he complained of numbness and a slight color change in his left foot. Two days later, he complained of sharp pain in his feet and in the tip of the penis. The area around the external urethral orifice had turned purple. Necrosis of the feet (Figure D–F) and at the tip of the penis (Figure G) worsened. Amputation of the penis was warranted because of voiding difficulty. Pathological evaluation of the penis revealed needle-shaped clefts (Figure H, arrow), thus confirming cholesterol crystal embolization (CCE).
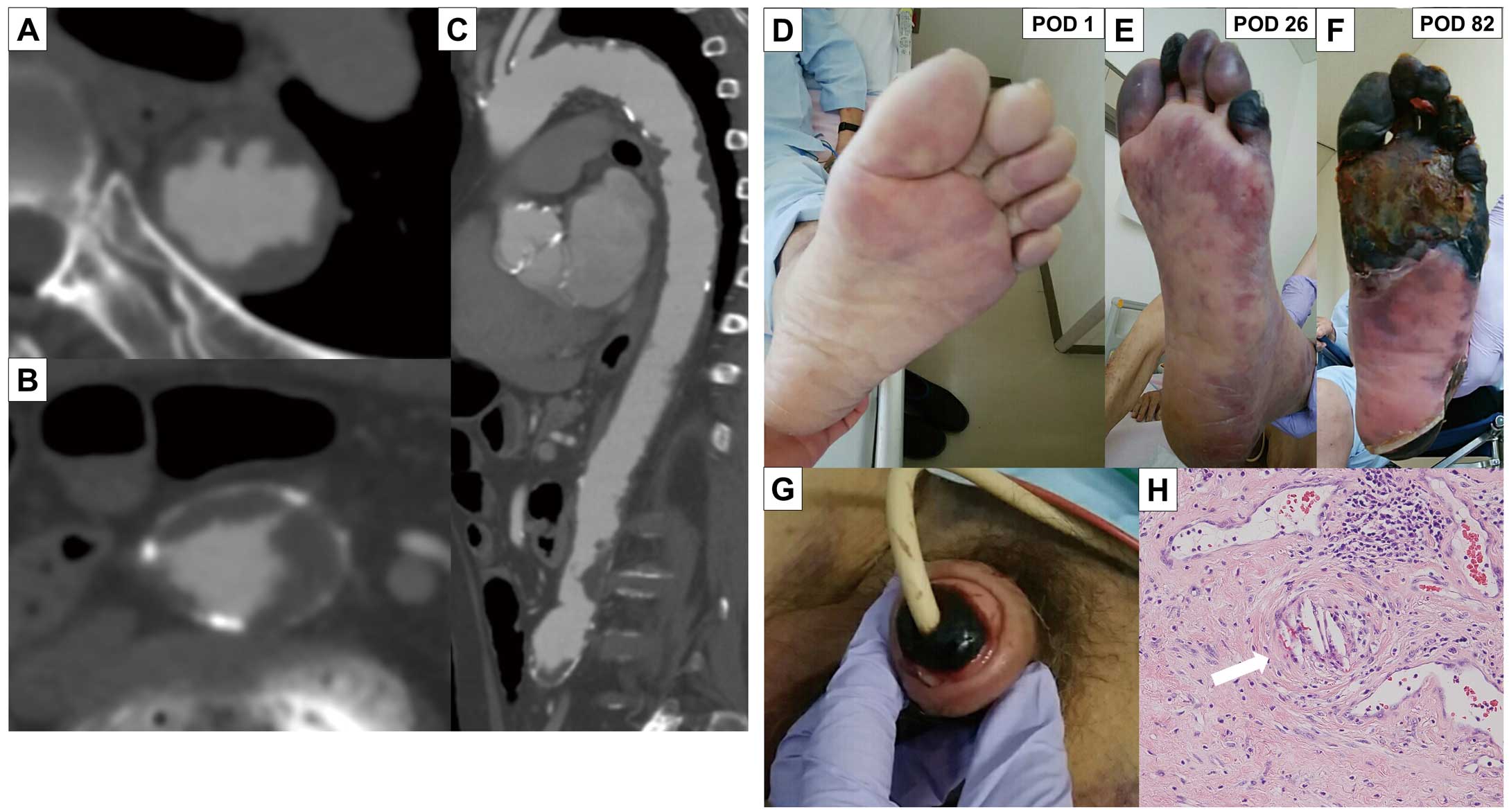
(A–C) Preprocedural contrast-enhanced computed tomography. (A,B) Axial plane; (C) long axis view. (D–G) Deterioration of the color of the feet on postoperative days (POD) 1 (D), 26 (E), and 82 (F) and the penis on POD 5 (G). (H) Pathology of the penis. Hematoxylin-eosin staining revealed cholesterol crystals (arrow).
The patient was administered statins and steroids and underwent renal replacement therapy. He refused amputation of the foot and ultimately died of sepsis from foot necrosis 9 months after TAVR.
CCE is a dreaded complication of endovascular intervention in patients with atherothrombotic plaques in the access vessels.1 In such cases, it is important to choose alternative access, such as transaxillary, transaortic, or transapical.
T.M. is a member of Circulation Reports ’ Editorial Team.
This study was approved by Nagoya University Hospital Institutional Review Board (2019-0179) and was performed in accordance with the Declaration of Helsinki.