2021 年 3 巻 10 号 p. 569-577
2021 年 3 巻 10 号 p. 569-577
Background: Despite the prognostic effectiveness of cardiac rehabilitation (CR) in patients with cardiovascular disease (CVD), it has been underutilized. Understanding the trend of dissemination of CR over the years would help provide a perspective of CR in Japan.
Methods and Results: A retrospective epidemiological survey between fiscal years 2010 and 2017 was conducted using the diagnosis procedure combination database (a Japanese administrative database). Data on 2,046,302 patients with CVD from 1,632 hospitals were extracted. The proportion of CR-certified hospitals among hospitals treating patients with CVD increased from 31.6% in 2010 to 56.6% in 2017. Over the same period, the participation rate in inpatient CR (ICR) increased from 18.3% to 39.0%, but the participation rate in outpatient CR (OCR) remained low (from 1.4% to 2.5%). The CR participation rates varied widely according to the main disease group. Approximately 95% of ICR participants did not continue CR after discharge.
Conclusions: The number of CR-certified hospitals increased from 2010 to 2017, leading to increased ICR participation across patients with CVD; however, OCR has remained extremely underutilized. Immediate action is urgently required to increase the use of OCR.
Cardiac rehabilitation (CR) has been demonstrated to have prognostic effectiveness in patients with heart failure (HF), ischemic heart disease, and other cardiovascular diseases (CVD),1–4 leading to higher recommendation levels in clinical practice guidelines worldwide.5–8 However, the underutilization of CR has been flagged in many countries.9–13 In Japan, a 2007 nationwide questionnaire-based survey revealed that the rate of participation in outpatient CR (OCR) was extremely low.14 Since then, the trend in CR dissemination over the years has remained unknown.
With advancing emergency care systems and growing numbers of hospitals for emergency revascularization, the survival rates of patients with CVD have improved significantly.15,16 In addition, the amelioration of drug-eluting stents has reduced the risk of target region revascularization. However, it has been reported that 18.3% of patients with post-myocardial infarction in European countries experienced some cardiovascular events within 1 year,17 and 23.0% of patients undergoing drug-eluting stent implantation in Japan experienced non-target lesion revascularization within 5 years.18 Therefore, CR, including disease management and behavioral changes for a healthier lifestyle, is highly recommended.5 In addition, due to increases in the aging population and technological advances in medicine and surgery, the number of elderly patients undergoing cardiovascular (CV) surgery is gradually increasing. However, the long-term post-surgery prognosis is not better than expected,19 suggesting the importance of secondary preventive care in elderly post-CV surgery (PCS) patients. Despite robust evidence indicating the need for improving patients’ long-term prognoses, as well as the recommendation for CR in several clinical guidelines,5–8 data demonstrating the dissemination of CR are lacking, making it difficult to set policies in real-world settings.
Therefore, in this study we investigated the status of CR participation in patients with CVD in Japan from fiscal year 2010 to 2017 using nationwide administrative data and explored the factors related to CR participation.
We conducted a retrospective epidemiological survey on data registered between April 2010 and March 2018 (fiscal years 2010 and 2017, respectively) in the Diagnosis Procedure Combination (DPC) database. The DPC is a casemix classification applied in a payment system that has been introduced in more than 1,500 acute-care hospitals in Japan. As of 2014, approximately 75% of all DPC-associated hospitals had contributed to the DPC database.20 The DPC database originally contained discharge abstracts and administrative claims for inpatient care; since fiscal year 2012, it also provides information on outpatient claims.21 The database includes the following data for inpatients: dates of admission and discharge, age, sex, disease, diagnoses and outcomes, comorbidities at admission, procedures, medications, devices, and rehabilitation. Diagnoses are recorded using the International Classification of Diseases, 10th Revision (ICD-10) codes. The outpatient data include data on procedures, medications, and rehabilitation in outpatient settings. In the present study, these data were collected and, for every fiscal year, arranged from the April of that year to March of the following year. Due to the secondary use of anonymous data, written informed consent from the patients was not required. This study was approved by the Institutional Review Board of the Tokyo Medical and Dental University (M2000-788).
Study PopulationWe extracted data of patients aged ≥18 years who were admitted with acute myocardial infarction (AMI), angina pectoris (AP), HF, or peripheral artery disease (PAD) as the main disease or who underwent CV surgery between April 2010 and October 2017. However, because CR was covered by insurance for up to 150 days, we evaluated CR implementation for 150 days from the date of CR initiation. The ICD-10 codes were I21, I22, and I23 for AMI; I20 for AP; I110, I130, I132, and I50 for HF; and I702 and I743 for PAD. CV surgeries included coronary artery bypass grafting, valve surgery, and aortic surgery. Patients who died during hospitalization, had a hospital stay of <2 days, or had a hospital stay of >60 days were excluded from the study.
Cardiac RehabilitationWe evaluated the participation status for inpatient CR (ICR) and OCR by using the inpatient and outpatient claims data, respectively. We referred to inpatient records and considered a patient to be an ICR participant if they had participated in the CR program at least once during their hospitalization. We also referred to outpatient records and considered a patient to be an OCR participant if they had participated in the CR program at least once within 30 days of discharge. Considering data availability, the OCR survey period was limited to fiscal year 2012 and later. For ICR participants, the number of ICR sessions and their total time were evaluated by counting the number of CR claims. In Japan, every 20 min of CR time is converted to 1 “unit”. The number of units corresponding to each rehabilitation session provided to the patients is recorded on the claims. Therefore, the total time can be calculated by multiplying the number of units by 20. For OCR participants, the number of sessions and the duration of OCR were evaluated.
In Japan, hospitals that can provide CR programs under the national insurance system need to meet certain criteria, including in terms of staff, structure, and equipment. In the present study, we defined hospitals certified for CR (i.e., “CR hospitals”) as hospitals that provided at least 1 session of CR during the fiscal year. Therefore, the CR implementation rate indicated the proportion of CR hospitals among hospitals treating patients with CVD.
The participation and implementation rates of ICR and OCR for each fiscal year were evaluated as the main outcomes of this study. Participation rates were also calculated according to main disease, sex, and age group. In addition, the OCR transition rate (i.e., the proportion of ICR participants who moved from ICR to OCR) was calculated to assess whether patients continued with CR after discharge.
Other VariablesWe evaluated the major disease for which patients were admitted based on the ICD-10 codes. Patient characteristics including age at admission, sex, smoking history, body mass index, comorbidities (hypertension, dyslipidemia, diabetes, HF, cerebrovascular disease, PAD, renal disease, anemia, dementia, depression, and sleep apnea syndrome), hemodialysis status, Charlson comorbidity index (calculated from the comorbidity data in the DPC database), medication usage (aspirin, clopidogrel, prasugrel, β-blocker, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, nicorandil, calcium channel blocker, statin, loop diuretic, and spironolactone), and rehabilitation programs other than CR during hospitalization were evaluated. Furthermore, the annual number of patients with CVD was evaluated as a variable representing hospital size.
Statistical AnalysisPatient characteristics were evaluated for the following 3 groups: the non-CR group (comprising patients who had never participated in the CR program), the ICR group (comprising patients who had participated in the ICR program but never in the OCR program), and the OCR group (comprising patients who had participated in the OCR program, regardless of ICR participation). For group comparisons, t-tests, χ2 tests, and the Wilcoxon rank-sum test were used. Some main outcomes were summarized by the fiscal years and patient groups. To evaluate differences in the annual increase in the CR participation rates among each patient group, we performed a linear regression analysis of the participation rates and estimated the slope for each group.
All data management and statistical analyses were conducted using Stata 14.2 (Stata Corp., College Station, TX, USA). Two-sided P<0.05 was considered statistically significant.
Data on 2,046,302 patients from a total of 1,632 hospitals registered between fiscal years 2010 and 2017 were extracted. The characteristics of the study participants are presented in Table 1. There were 562,208 and 33,525 patients classified into the ICR and OCR groups, respectively. Furthermore, 5,475 patients from the OCR group did not participate in ICR. The mean age of the patients increased annually, and patients with HF were the oldest. The mean duration of hospitalization reduced over time, except in patients with HF (Supplementary Table 1). Compared with the non-CR group, the ICR and OCR groups had more emergency admissions, longer hospital stays, more patients with HF complications, and a higher medication usage. Furthermore, compared with the non-CR group, the ICR and OCR groups had fewer patients with renal failure and fewer patients on hemodialysis. Compared with the other groups, the OCR group had younger patients and a higher number of men, smokers, and patients with complications such as hypertension and dyslipidemia.
| Variables | Non-CR group (n=1,450,569) |
CR group | |
|---|---|---|---|
| Inpatient (n=562,208) |
Outpatient (n=33,525) |
||
| Mean (±SD) age (years) | 72.7±11.8 | 73.8±12.4 | 66.9±11.9 |
| Male sex (%) | 67.7 | 62.1 | 74.6 |
| Main disease (%) | |||
| AMI | 7.6 | 19.1 | 36.3 |
| Angina pectoris | 34.8 | 13.2 | 19.3 |
| Other IHD | 7.8 | 2.8 | 5.4 |
| Heart failure | 34.1 | 38.0 | 25.0 |
| PAD | 9.1 | 3.3 | 2.8 |
| Procedures (%) | |||
| CABG | 1.5 | 9.4 | 7.2 |
| Valve surgery | 1.8 | 11.6 | 6.7 |
| Aortic surgery | 4.8 | 12.8 | 5.1 |
| Non-emergency PCI | 40.1 | 11.0 | 16.2 |
| Emergency PCI | 8.5 | 17.9 | 39.7 |
| Comorbidities (%) | |||
| Hypertension | 54.4 | 58.0 | 63.7 |
| Dyslipidemia | 38.4 | 35.5 | 52.8 |
| Diabetes | 31.7 | 28.6 | 30.7 |
| Heart failure | 14.8 | 21.5 | 25.3 |
| Cerebrovascular disease | 6.5 | 6.8 | 3.8 |
| PAD | 6.8 | 6.6 | 4.4 |
| Renal disease | 11.4 | 9.3 | 4.6 |
| Anemia | 3.7 | 5.1 | 2.6 |
| Dementia | 1.3 | 1.6 | 0.2 |
| Depression | 0.7 | 0.8 | 0.6 |
| SAS | 0.8 | 1.2 | 2.5 |
| Mean (±SD) CCI | 1.97±1.45 | 2.17±1.36 | 1.98±1.23 |
| Mean (±SD) BMI (kg/m2) | 23.3±3.9 | 23.1±3.9 | 24.1±3.8 |
| Smoking history (%) | 44.8 | 43.3 | 52.7 |
| Hemodialysis (%) | 7.2 | 4.4 | 1.9 |
| Mean (±SD) LOS (days) | 12.2±11.3 | 21.2±11.9 | 16.7±10.8 |
| Emergency admission (%) | 27.0 | 47.7 | 59.9 |
| Discharge (%) | |||
| Home | 92.7 | 87.0 | 99.4 |
| Other hospital | 4.7 | 9.9 | 0.4 |
| Nursing facility | 2.3 | 2.9 | 0.1 |
| Other | 0.3 | 0.2 | 0.1 |
| Other rehabilitation (%) | 11.4 | 5.0 | 2.7 |
| Medication (%) | |||
| Aspirin | 54.3 | 60.4 | 73.7 |
| β-blocker | 36.2 | 59.7 | 70.3 |
| ACEI ARB | 29.5 | 43.6 | 55.3 |
| Statin | 41.0 | 49.1 | 66.9 |
ACEI, angiotensin-converting enzyme inhibitor; AMI, acute myocardial infarction; ARB, angiotensin II receptor blocker; BMI, body mass index; CABG, coronary artery bypass grafting; CCI, Charlson comorbidity index; CR, cardiac rehabilitation; IHD, ischemic heart disease; LOS, length of stay; PAD, peripheral artery disease; PCI, percutaneous coronary intervention; SAS, sleep apnea syndrome; SD, standard deviation.
The trend of the CR implementation rate is shown in Figure 1. The proportion of hospitals implementing CR increased annually, rising from 31.6% in 2010 to 56.6% in 2017.
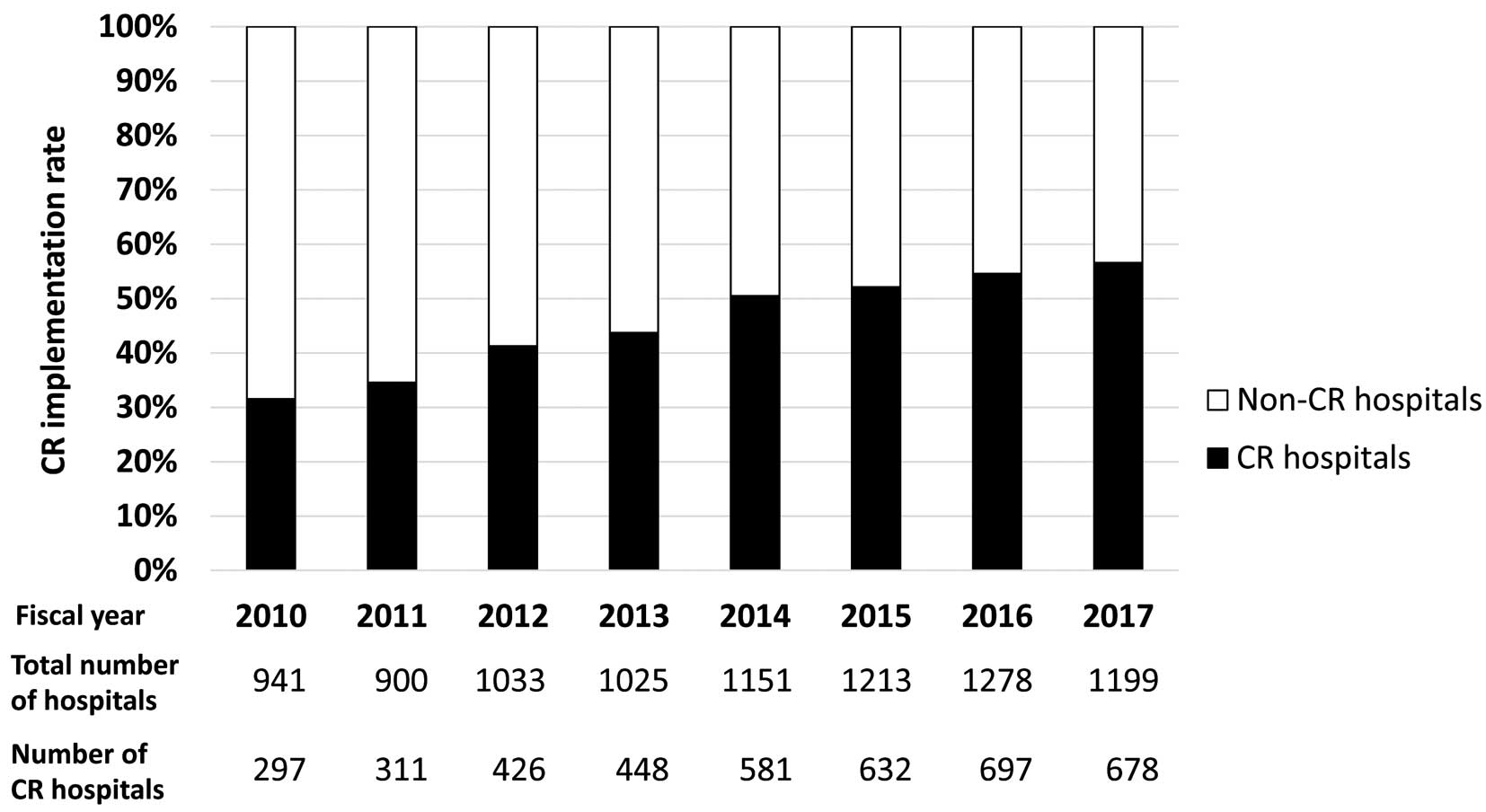
Trends in cardiac rehabilitation (CR) implementation rates from 2010 to 2017. The CR implementation rate indicates the proportion of CR hospitals that provided at least 1 session of CR during the fiscal year among all hospitals treating patients with cardiovascular disease.
Trends in the number of ICR and OCR participants are presented in Table 2 (also see Supplementary Figure 1). The annual number of ICR participants increased approximately 4-fold during this period. The annual number of OCR participants also increased over the years; however, this increase was much smaller than that in ICR participants. There was a large variation in ICR participation rates among the hospitals (Supplementary Figure 2); for example, the median ICR participation rate in fiscal year 2017 was 45.8% (interquartile range [IQR] 32.7–58.1%), with a minimum of 0.4% and a maximum of 100%. In the same year, the median OCR participation rate was 3.6% (IQR 1.5–7.7%), with a minimum of 0.1% and a maximum of 33.3%. The ICR and OCR participation rates by hospital size are presented in Supplementary Table 2.
| Fiscal year | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| ICR (n) | 30,996 | 46,878 | 57,736 | 63,279 | 90,713 | 105,002 | 122,913 | 124,699 |
| Overall (%) | 18.3 | 20.5 | 21.9 | 24.6 | 30.5 | 34.0 | 36.8 | 39.0 |
| Main disease (%) | ||||||||
| AMI | 36.7 | 40.5 | 42.0 | 46.6 | 54.0 | 60.2 | 63.3 | 65.6 |
| AP | 10.5 | 11.2 | 11.1 | 12.3 | 13.8 | 15.1 | 15.6 | 16.3 |
| HF | 15.2 | 17.6 | 20.3 | 24.1 | 33.7 | 38.6 | 43.0 | 46.9 |
| PAD | 8.5 | 10.2 | 10.1 | 11.0 | 13.2 | 13.4 | 14.4 | 16.1 |
| PCS | 44.5 | 49.2 | 53.4 | 55.5 | 64.0 | 69.4 | 73.0 | 76.5 |
| Sex (%) | ||||||||
| Men | 18.0 | 19.8 | 21.1 | 23.6 | 28.8 | 32.0 | 34.3 | 36.3 |
| Women | 19.1 | 21.8 | 23.6 | 26.6 | 33.9 | 37.8 | 41.5 | 44.3 |
| Age group (%) | ||||||||
| ≤49 | 23.4 | 25.2 | 26.5 | 28.2 | 33.8 | 38.2 | 39.4 | 43.3 |
| 50–59 | 19.4 | 21.1 | 23.6 | 25.2 | 29.3 | 32.4 | 34.5 | 36.5 |
| 60–69 | 17.8 | 20.0 | 20.9 | 23.4 | 27.3 | 30.7 | 32.6 | 34.5 |
| 70–79 | 18.0 | 20.3 | 21.3 | 23.7 | 28.5 | 31.7 | 34.0 | 36.0 |
| ≥80 | 18.0 | 20.3 | 22.3 | 25.9 | 34.6 | 38.2 | 42.2 | 44.8 |
| OCR (n) | – | – | 3,773 | 3,922 | 6,156 | 6,314 | 8,707 | 7,977 |
| Overall (%) | – | – | 1.4 | 1.5 | 2.1 | 2.0 | 2.6 | 2.5 |
| Main disease (%) | ||||||||
| AMI | – | – | 4.7 | 5.4 | 6.5 | 6.7 | 8.4 | 8.5 |
| AP | – | – | 1.0 | 1.1 | 1.6 | 1.4 | 1.7 | 1.5 |
| HF | – | – | 1.0 | 1.0 | 1.5 | 1.5 | 1.9 | 2.0 |
| PAD | – | – | 0.5 | 0.5 | 0.8 | 0.7 | 1.0 | 0.8 |
| PCS | – | – | 1.9 | 1.9 | 2.4 | 2.5 | 3.3 | 2.9 |
| Sex (%) | ||||||||
| Male | – | – | 1.6 | 1.7 | 2.3 | 2.3 | 2.9 | 2.8 |
| Female | – | – | 1.1 | 1.2 | 1.5 | 1.5 | 2.0 | 2.0 |
| Age group (%) | ||||||||
| ≤49 years | – | – | 3.2 | 3.6 | 4.6 | 4.9 | 5.8 | 5.8 |
| 50–59 years | – | – | 2.7 | 2.7 | 3.4 | 3.8 | 4.5 | 4.2 |
| 60–69 years | – | – | 1.9 | 2.2 | 2.8 | 2.7 | 3.5 | 3.3 |
| 70–79 years | – | – | 1.4 | 1.5 | 2.1 | 2.0 | 2.7 | 2.5 |
| ≥80 years | – | – | 0.5 | 0.5 | 0.8 | 0.8 | 1.1 | 1.1 |
AMI, acute myocardial infarction; AP, angina pectoris; HF, heart failure; ICR, inpatient cardiac rehabilitation; OCR, outpatient cardiac rehabilitation; PAD peripheral artery disease; PCS, post-cardiovascular surgery.
The trends in ICR and OCR participation rates for the entire study population are shown in Figure 2, and the corresponding specific values are presented in Table 2. The overall ICR participation rate increased annually, from 18.3% in 2010 to 39.0% in 2017, whereas the OCR participation rate remained at 2.5% in 2017. Participation rates varied according to the main disease group; in 2017, patients with PCS had the highest ICR participation rate (76.5%), followed by patients with AMI (65.6%). Conversely, patients with AP and PAD had the lowest participation rates (16.3% and 16.1%, respectively). In the same year, patients with AMI had the highest OCR participation rate (8.5%), whereas the participation rates for the other disease groups were <3%. The annual increase in ICR and OCR participation rates for each disease group was estimated using linear regression analysis (Supplementary Table 3). The increase in ICR participation rates differed significantly according to the main disease groups; the annual increase was approximately 5 points in patients with AMI, HF, and PCS and approximately 1 point among those with AP and PAD. Conversely, the annual increase in the OCR participation rate was convergent, and all increases among the different disease groups were <1 point.

Trends in (A) inpatient and (B) outpatient cardiac rehabilitation (CR) participation rates by disease group. The inpatient CR participation rate is the proportion of patients who participated in at least 1 session of an inpatient CR program during their hospitalization. The outpatient CR participation rate is the proportion of patients who participated in an outpatient CR program after discharge. AMI, acute myocardial infarction; AP, angina pectoris; HF, heart failure; PAD, peripheral artery disease; PCS, post-cardiovascular surgery.
Changes in the relationships between CR participation rates and age groups in each fiscal year are shown in Figure 3. In the case of the ICR participation rate, an inverse relationship was observed across all age groups before 2011: the older the age group, the lower the participation rate. However, during subsequent years (especially since 2014), the curve became U-shaped, as the participation rate increased again for those aged ≥60 years. Conversely, in the case of the OCR participation rate, the relationship remained an inverse one (Figure 3).

Changes in the relationship between (A) inpatient and (B) outpatient cardiac rehabilitation (CR) participation rates and age in each fiscal year.
The OCR transition rate remained low (Figure 4), because approximately 95% of ICR participants discontinued CR at discharge and never participated in the OCR program at that hospital.

Trends in the outpatient cardiac rehabilitation (CR) transition rate (i.e., the proportion of inpatient CR participants who moved to outpatient CR) by main disease group. AMI, acute myocardial infarction; AP, angina pectoris; HF, heart failure; PAD, peripheral artery disease; PCS, post-cardiovascular surgery.
The participation status for ICR and OCR for each disease group is presented in Table 3. The number of ICR sessions according to disease group was associated with the length of hospital stay (for the length of hospital stay, see Supplementary Table 1). Under Japanese health insurance, the OCR program is standardized to be performed 3 times a week and is covered for up to 150 days after CR initiation. Therefore, excluding the hospitalization period, patients can participate in the OCR program for at least 18 weeks, or approximately 54 sessions. However, only a median of 6–8 sessions was conducted, which was extremely low.
| ICR | OCR | |||
|---|---|---|---|---|
| No. sessions | Total time of sessions (min) |
No. sessions | Duration of participation (days) |
|
| Overall | 8 (5–13) | 260 (140–460) | 7 (3–17) | 88 (29–146) |
| AMI | 7 (4–10) | 240 (140–380) | 8 (3–16) | 90 (29–143) |
| Angina pectoris | 5 (2–10) | 180 (60–380) | 8 (3–18) | 94 (32–151) |
| Heart failure | 9 (5–14) | 280 (160–500) | 7 (3–18) | 80 (26–151) |
| PAD | 6 (2–11) | 180 (80–380) | 6 (2–16) | 70 (25–149) |
| PCS | 10 (6–15) | 340 (200–560) | 6 (2–15) | 87 (30–136) |
Data are presented as the median (interquartile range). Data related to ICR were derived from fiscal years 2010 to 2017, whereas data related to OCR were derived from fiscal years 2012 to 2017. The duration of participation in OCR is the number of days from discharge to last participation. Abbreviations as in Table 2.
This study revealed the trend in CR dissemination in Japan from 2010 to 2017 using administrative data. We found that the number of hospitals implementing CR increased from 31.6% in 2010 to 56.6% in 2017, and the overall rates of ICR participation increased from 18.3% in 2010 to 39.0% in 2017. In turn, the overall rates of OCR participation remained strikingly low, having increased a mere 1.1% between 2012 and 2017. In addition, the trends varied widely among disease and age subgroups.
To the best of our knowledge, the present study is the first in Japan to report the CR dissemination trend over time on a nationwide scale. A previous survey conducted mainly among Japanese Circulation Society (JCS)-authorized cardiology training hospitals and JCS-associated hospitals in the early 2000 s reported an OCR participation rate of 3.8–7.6%.14 Another study focusing on patients with coronary artery disease between 2006 and 2013 reported participation rates of 23.7% for ICR and 4.2% for OCR.13 Our findings provide valuable information regarding ICR and OCR in recent years. These data are fundamental to understanding the nationwide spread of CR and to help develop future strategies to improve CR delivery in Japan.
Progress of ICR and OCR Implementation and ParticipationThe CR implementation rate increased by 25% from 2010 to 2017. Thus, CR became more widespread in Japan over the past decade. This may be due to the reimbursement revisions undertaken in the 2000s, in which facility criteria related to staffing and systems were relaxed. These relaxations may have resulted in more hospitals being able to meet the criteria for CR hospitals. Still, nearly half the hospitals did not offer CR in 2017. This may be due to a lack of awareness among physicians, barriers to developing systems that meet the facility criteria, or profitability issues.
Along with the increase in CR hospitals, the number of CR participants increased every year. Notably, the ICR participation rate increased significantly from 18% in 2010 to 40% in 2017. This may indicate that an increase in facilities is an important factor for increasing ICR participation; the increased dissemination of ICR must contribute to improved quality of care for inpatients with CVD. However, it was also found that the ICR participation rate varied widely among individual hospitals and was not homogeneous. Therefore, to further improve the quality of inpatient care, efforts must be taken by individual hospitals. Interestingly, the situation of ICR participation in Japan was comparable to that of ICR participation in the US.22 Pack et al22 reported that a formal ICR program was available at 49% of eligible hospitals between 2007 and 2011, with an overall ICR utilization rate of 21.2%.
In the present study, despite the marked increase in the number of CR hospitals, the OCR participation rate remained extremely low throughout the survey period, indicating that the status of OCR participation in Japan has not improved for more than 15 years.14 This also suggests that factors other than an increased number of CR hospitals affected OCR participation. These factors could include patient clinical characteristics,9,23–25 patient perception,23,24 and physician awareness regarding the benefits of CR.9,23–25 This low rate of OCR participation was also indicated by the low rate of transition from ICR to OCR, which meant that most ICR participants quit the program after hospital discharge. This may be due to problems such as scheduling conflicts, transportation issues, and a need to resume work earlier. To promote secondary prevention care, an approach that solves these issues is required. To this end, strategies other than a hospital-based program may be necessary. For example, a home-based CR program may be one solution because it solves the problem of hospital visits and seems to be as effective as a center-based program.26 In addition, recent developments in telecommunications have enabled remote exercise monitoring and health management.27,28 These new technologies have the potential to enhance the accessibility and individuality of the program29 and are thus likely to improve OCR participation.
Differences in CR Participation Between Specific GroupsThe relationship between CR participation and age differed between the ICR and OCR programs. In line with the results of previous studies,9–11,23,24 the OCR participation rates in the present study consistently declined with age. Conversely, the ICR participation rate showed a U-shaped relationship with age, especially after 2014, as it increased among those aged ≥60 years. This likely reflects the special needs for rehabilitation among elderly patients, such as early mobilization to prevent complications due to physical inactivity during hospitalization. Therefore, in addition to a secondary prevention program, the ICR program may be required for an early and safe return to social activities.
The CR participation rates varied widely according to the main disease group. ICR and OCR participation rates were highest in patients with PCS and AMI and lowest in patients with PAD and AP, with a greater than 4-fold difference between them. The rates in patients with HF were also comparably low. Similar results have been reported in other studies: participation rates were higher in patients who had undergone cardiac surgery or had AMI and were lower in patients with medically managed HF or stable AP.11,22 Furthermore, the present study showed that the annual increases in the ICR participation rates were significantly lower in patients with AP and PAD than in patients with AMI, PCS, and HF. Rehabilitation for postoperative patients is likely to be included as part of the postoperative care, which aims for functional recovery and the prevention of complications. Conversely, for patients who are medically managed, referral to CR may be largely dependent on the judgment of the attending physician. The underuse of exercise therapy in patients with PAD has been reported previously.30 Given the potential benefits of exercise therapy in patients with HF,31,32 AP,33 and PAD,34–36 there may be a need to establish a system to evaluate and provide CR appropriately.
A recent report showed that the OCR participation rate among patients with HF was 7%,37 which is higher than that in the present study. This difference may be due to differences in the subjects and methods between the 2 studies; the previous study was a questionnaire survey of cardiologists who are members of the Japanese Heart Failure Society and belong to medical institutions affiliated with the Japanese Heart Failure Society, and the survey covered 270 institutions.37 However, the present study was based on insurance claims data from more than 1,200 hospitals. Thus, the data included many hospitals not as specialized in HF care, which may have contributed to the difference between the 2 studies. Furthermore, the present study may provide a more realistic representation of clinical practice in Japan.
Study LimitationsWe used a nationwide administrative claims database in this study. Although using the database has several advantages, including the ability to conduct large-scale surveys, to include patients and institutions with various characteristics, and to objectively assess whether a practice has been implemented, there are some limitations due to the nature of the data. First, we could not evaluate the contents of the CR program, such as exercise intensity and exercise components. Therefore, the quality of the CR program could not be evaluated. Second, because the DPC database comprised facility-based data, OCR attendance in hospitals other than those included in the analysis remains unknown. Third, because we evaluated only medical care covered by health insurance, CR programs not covered by health insurance reimbursements were not included in the study. Furthermore, hospitals that provide CR without health insurance coverage were not included as CR hospitals. Thus, we could not assess whether performing CR under health insurance coverage influenced CR participation. Finally, the data analyzed in this study were representative of a part of the target population and did not comprise data from all hospitals treating patients with CVD in Japan. Nevertheless, the analyzed data from approximately 1,200 hospitals across Japan are sufficient to generalize the findings of our study. A future periodical survey using national data will be necessary to assess and support the precise policymaking for CR in Japan.
This study revealed the progress of CR dissemination from 2010 to 2017 in Japan. Throughout the survey period, ICR had gradually become widespread and the number of CR hospitals increased, whereas OCR remained underutilized. To promote secondary prevention care in patients with CVD, a creative strategy, along with an understanding of the factors that facilitate ICR and OCR participation, is of extreme importance. The findings of this study may provide fundamental resources for overcoming these challenges.
The authors thank all the hospitals that joined the DPC research group, as well as the DPC Research Institute for the collection and contribution of their electronic healthcare records.
This study was supported by JSPS KAKENHI Grant Number JP20K19441.
The authors declare that there are no conflicts of interest.
This study was approved by the Institutional Review Board of the Tokyo Medical and Dental University (M2000-788).
The deidentified patient data are available upon reasonable request from the corresponding author (K.F.; kfushimi.hci@tmd.ac.jp). Reuse of the data subset is permitted only for the revalidation of the results of this study.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circrep.CR-21-0018