Abstract
Background:
The relationship between body posture and lung fluid level has not been quantified thus far. Remote dielectric sensing (ReDSTM) is a recently introduced non-invasive electromagnetic-based technology to quantify lung fluid percentage.
Methods and Results:
ReDS values were measured at different body postures (i.e., sitting, supine, and supine with legs elevated) in a healthy volunteer cohort (n=16; median age 39 years, 69% men, median [interquartile range {IQR}] body mass index 23.3 kg/m2
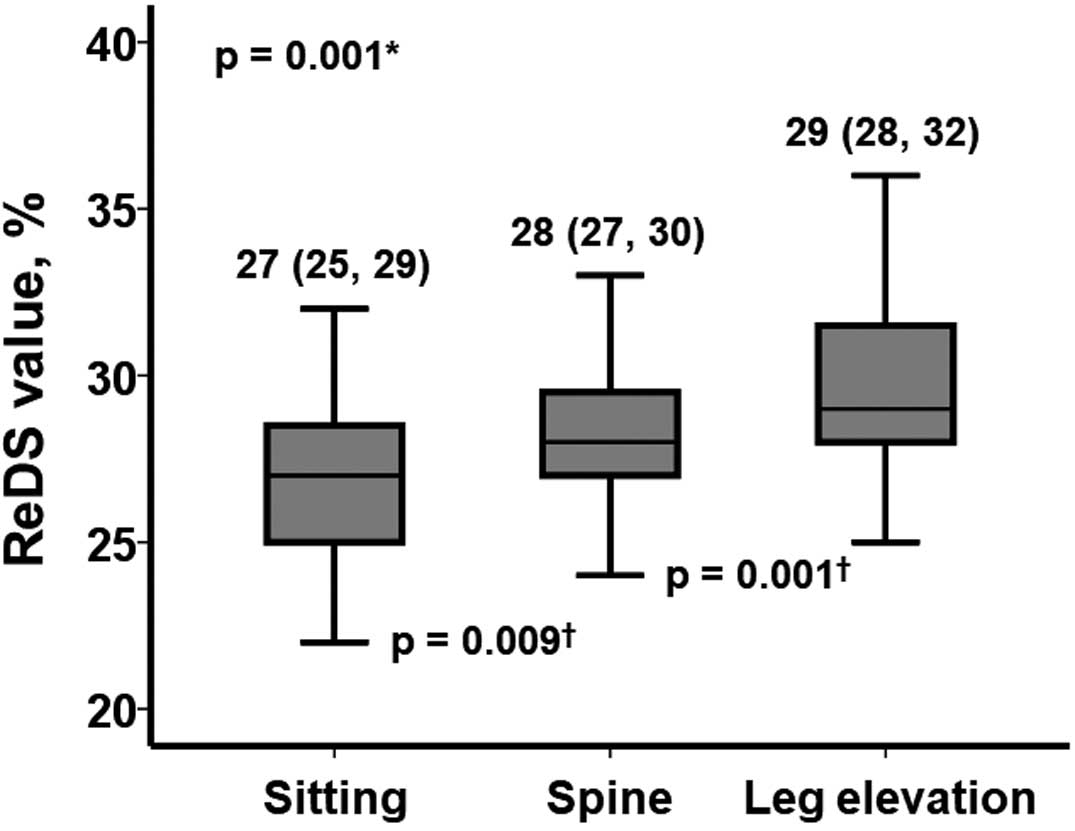
[21.0–26.2 kg/m2]). In the sitting position, the median ReDS value was 27% (IQR 25–29%). The ReDS value increased significantly in the supine position (median 28%; IQR 27–30%; P=0.009), and increased further upon leg elevation (median 29%; IQR 28–32%; P=0.001).
Conclusions:
In this proof-of-concept study, the relationship between body posture and lung fluid level was quantitatively validated in a healthy cohort.
The prevalence of heart failure is increasing, and optimal physical and medical prophylactic and therapeutic strategies are still to be determined.1–3
Of note, the management of pulmonary congestion is important to improve mortality and morbidity, as well as patients’ quality of life.4
In addition to appropriate diuretic therapy, appropriate body posture helps prevent worsening heart failure.5
Orthopnea is a well-known classical sign of pulmonary congestion in patients with decompensated heart failure.6
Theoretically, a sitting position may reduce venous return and ameliorate pulmonary congestion, relieving congestive symptoms. However, the relationship between body posture and the degree of pulmonary congestion has not been quantitatively validated in detail given the lack of a gold standard to accurately measure the fluid volume level.
Recently, a remote dielectric sensing (ReDSTM; Sensible Medical Innovations, Netanya, Israel) system, which is a non-invasive electromagnetic-based technology to quantify lung fluid level as a percentage, has been developed and is clinically available abroad.7
Several studies have demonstrated a correlation between ReDS values and lung fluid levels,8,9
as well as the clinical implications of ReDS-guided heart failure management.10,11
The Second Department of Internal Medicine, Toyama University received permission to use the device for the first time in Japan before commercial marketing. The device itself will soon be clinically available in Japan.
In the present proof-of-concept study, we investigated the relationship between body posture and ReDS values in healthy volunteers to clarify the physiological proof of fluid shift depending on different body postures.
Methods
Participant Selection
Healthy volunteers aged >20 years without any past medical history were prospectively included in this single-center proof-of-concept study between August and September 2021. This study was approved by the Clinical Research Review Board, University of Toyama (IRB no. MTK2020007), and written informed consent was obtained from all participants.
ReDS System
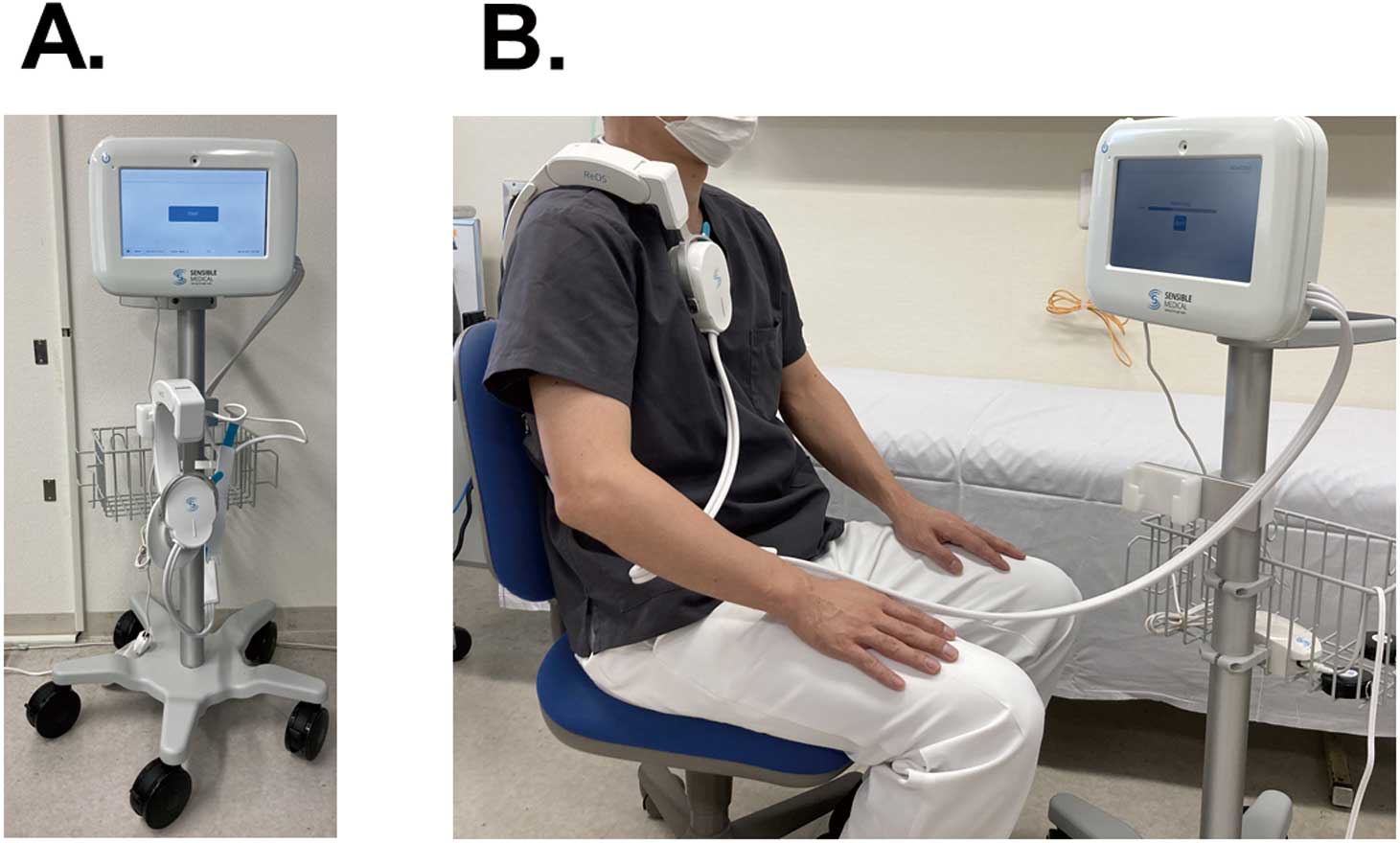
The ReDS technology has been detailed previously.7
Briefly, ReDS estimates the percentage lung fluid level and quantifies the pulmonary congestion status. ReDS uses low-power electromagnetic signals emitted between 2 sensors (one each on the anterior and posterior body surfaces) embedded in a wearable device (Figure 1). The signal analyzed reflects the dielectric properties of the lung portion between the sensors. The dielectric coefficient of a material is represented by a frequency-dependent complex number describing its interaction with electromagnetic energy, including the degree of absorption, reflection, and transmission of the energy. Because water has a very high dielectric coefficient and air has a very low dielectric constant, the dielectric coefficient of tissue is determined predominantly by its fluid content.
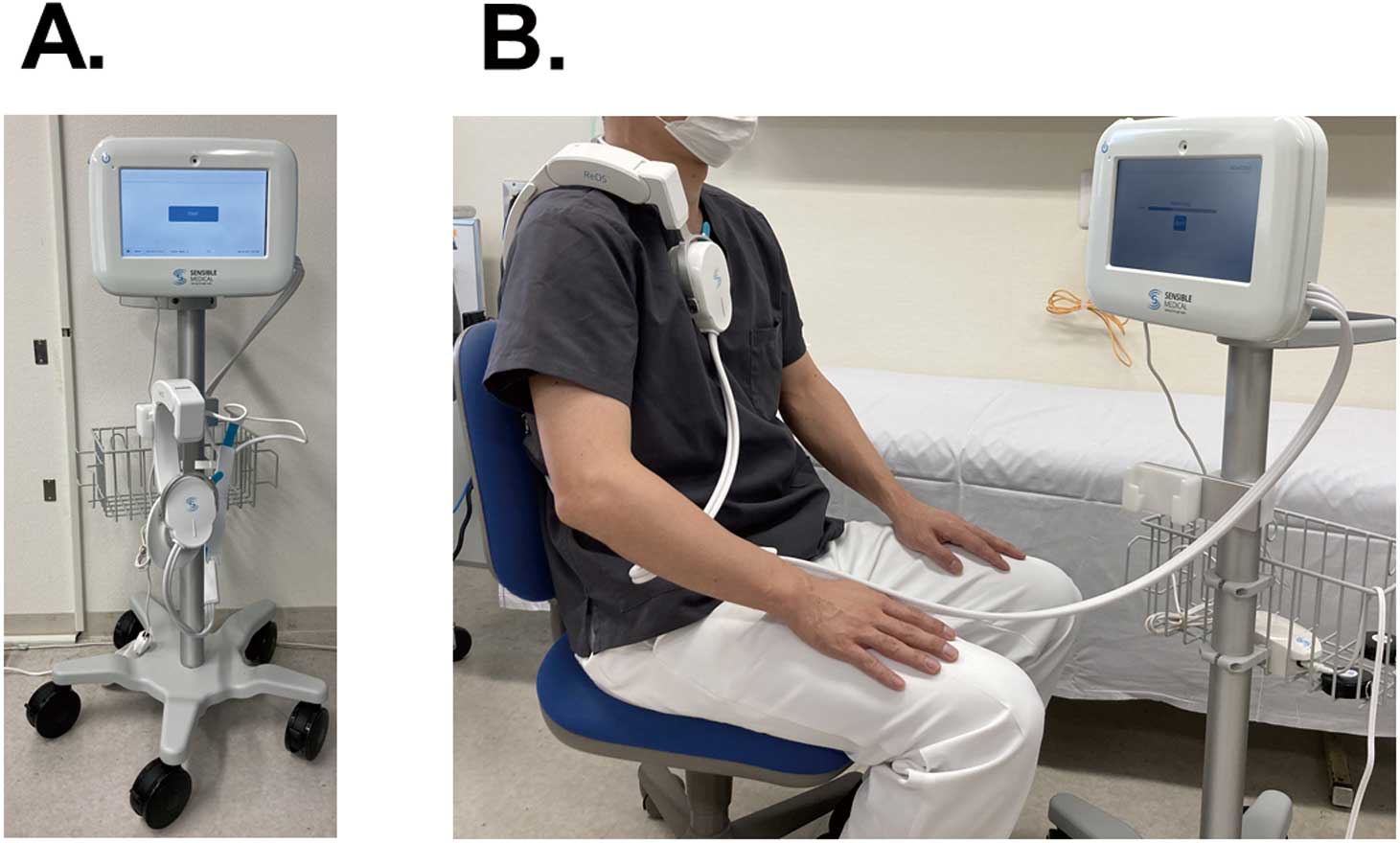
The ReDS measurement takes 45 s. From our initial experience, the overall procedure to complete the ReDS measurement can be completed within 5 min. ReDS data can be obtained by simply imputing patient information and pushing the start button. The manufacturer-proposed normal range for ReDS values is 20–35%.
Study Protocol
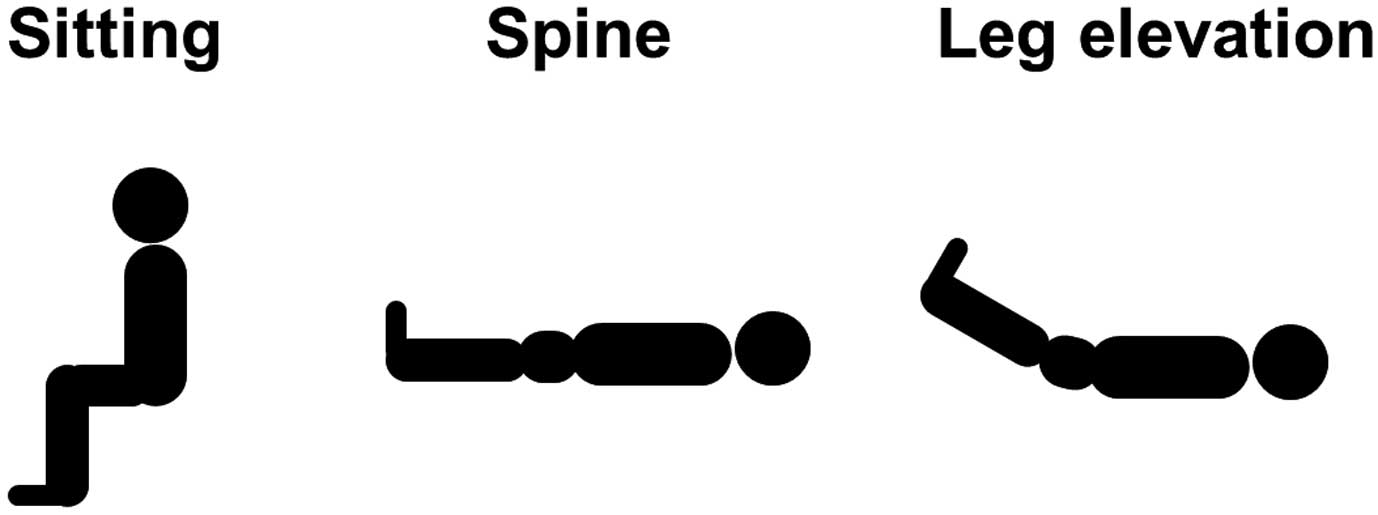
ReDS values were successively measured in participants in 3 different body positions (Figure 2). In the early morning, participants were left to sit for 5 min at rest, and the ReDS value was then measured as described above. Next, participants were asked to lie down in the spine position. After a 5-min rest, the ReDS value was measured again. Then, with participants still in the supine position, clinicians elevated participants’ legs by 30° from the horizontal and this position was maintained for 5 min before the ReDS value was measured again. All measurements were repeated twice and averaged.
Statistical Analysis
Continuous variables are presented as the median and interquartile range (IQR). Categorical variables are presented as numbers and percentages. ReDS values successively measured at 3 different body postures were compared by the Friedman test to determine trends, and with a post hoc Wilcoxon signed-rank test. All analyses were performed using SPSS Statistics 23.0 (IBM Corp., Armonk, NY, USA) and 2-sided P<0.05 was considered significant.
Results
Baseline Characteristics
Sixteen healthy volunteers participated in this proof-of-concept study (Table). The median age was 39 years (IQR 33–77 years), 69% were men, and the median body mass index was 23.3 kg/m2
(IQR 21.0–26.2 kg/m2). No participants had any major medical history or comorbidities. None of the participants were taking any medications.
Table.
Baseline Characteristics (n=16)
| Age (years) |
39 [33–77] |
| Male sex |
11 (69) |
| Body height (cm) |
170 [157–175] |
| Body weight (kg) |
67 [61–73] |
| Body mass index (kg/m2) |
23.3 [21.0–26.2] |
Continuous variables are presented as median [interquartile range]; categorical variables are presented as the number and percentage.
ReDS values were measured in each participant without any complications. The median ReDS value in the sitting position was 27% (IQR 25–29%;
Figure 3). All values were within the manufacturer-recommended normal range (i.e., between 20% and 35%).
The ReDS value increased significantly in the supine position (median 28%; IQR 27–30%; P=0.009), without any congestive symptoms. The ReDS value further increased significantly after leg elevation (median 29%; IQR 28–32%; P=0.001), again without any accompanying congestive symptoms. Two participants had ReDS value of 36%, which was above the normal range.
Discussion
In this proof-of-concept study in healthy volunteers, we investigated the relationship between body posture and ReDS values (obtained using non-invasive technology to quantify lung fluid levels) to validate a physiological proof of fluid shift depending on body posture. As expected, we confirmed that ReDS values increased with the incremental height of the leg relative to the chest (i.e., sitting < supine < supine + leg elevation).
ReDS System
Accurate assessment of the severity of pulmonary congestion is essential for the management of congestive heart failure, but thus far there is no gold standard to quantify the degree of pulmonary congestion.12
Chest X-ray and computed tomography (CT) are often used to qualify pulmonary congestion, but these modalities may not necessarily be accurate and require expertise to interpret the results. Right heart catheterization and CardioMEMS are useful for quantifying the intracardiac pressure, although the CardioMEMS is not available in Japan thus far.9
The difference between volume and pressure should be noted and understood. Plasma B-type natriuretic peptide (BNP) concentrations are used in daily practice to estimate intracardiac loading, but several conditions that affect BNP values, including obesity and renal impairment, need to be taken into consideration.13
As detailed above, ReDS is a recently introduced non-invasive technology that quantifies lung fluid volume.7
In patients with and without heart failure, ReDS was statistically non-inferior in estimating lung fluid volume compared with CT using specific commercially available software.8
In another study, ReDS values were moderately correlated with pulmonary capillary wedge pressure.9
Again, it should be noted that the focus of the measurements in these 2 studies differs: one measured volume and the other measured pressure. Another 2 studies reported that ReDS-guided management that included adjusting the dose of diuretics improved clinical outcomes in patients with congestive heart failure.10,11
We used the ReDS technology for the first time, before commercial marketing, in Japan to quantify lung fluid levels. This technology will soon be available in Japan.
Body Posture and Lung Fluid Volume
Ideally, this study should have included subjects with congestive heart failure. However, we believe that such an intervention, including leg elevation, would be ethically challenging. This is why healthy volunteers were enrolled in the study.
In addition to medical therapy including diuretics, management of body posture is essential in the management of heart failure patients in acute and chronic situations.6
Heart failure patients should be educated as to the appropriate body posture to stabilize their pulmonary congestion according to validated evidence.
In this study, we confirmed a physiological fluid shift depending on body posture using a novel device in a healthy cohort. Interestingly, some healthy volunteers showed ReDS values beyond the normal range (>35%) after leg elevation, even though they were asymptomatic. In this study in healthy volunteers, the degree of increase in ReDS values after leg elevation was small. However, the effect of leg elevation would be greater and is better avoided in patients with abnormally higher baseline ReDS values, such as those with congestive heart failure. Our findings should be validated in other populations with comorbidities, including congestive heart failure, using a carefully considered protocol.
Study Limitations
This is a proof-of-concept study using the ReDS system for the first time before commercial marketing in Japan, and the study cohort was relatively small. Nevertheless, we emphasize that this study validated, for the first time, the classically hypothesized implication of body posture by quantifying fluid lung volume. We performed ReDS measurements at a single time point. Trends in ReDS values over a certain observation period should be evaluated in future studies.
This study was conducted in a healthy cohort, and it may not be possible to extrapolate the findings to subjects with comorbidities, including heart failure, or those with abnormal physics. For most participants in this study, the degree of change in ReDS values was small within the normal range. We believe that the degree of change in ReDS values would increase in patients with elevated baseline ReDS values, such as those with congestive heart failure. Other factors, such as age, obesity, and renal function, may also affect the degree of change in ReDS values.
One of the limitations of the ReDS system is that this device cannot distinguish pulmonary congestion from other lung diseases that occupy the lung field, including lung cancer and pneumonia. This technology should soon be commercially available in Japan. Future studies should evaluate the clinical implications of ReDS-guided management in Japanese patients with congestive heart failure.
Conclusions
In this proof-of-concept study, the relationship between body posture and lung fluid level was quantitatively validated. The clinical implications of our findings in patients with congestive heart failure remain to be determined.
Sources of Funding
This study did not receive any specific funding.
Disclosures
T.I. receives grant support from JSPS KAKENHI (JP20K17143). The remaining authors have no conflicts of interest to report. K.K. is an Editorial Board member of
Circulation Reports.
IRB Information
This study was approved by the Clinical Research Review Board, University of Toyama (IRB no. MTK2020007).
References
- 1.
Farmakis D, Mehra MR, Parissis J, Filippatos G. Heart failure in the course of a pandemic. Eur J Heart Fail 2020; 22: 1755–1758.
- 2.
Kitaoka H, Tsutsui H, Kubo T, Ide T, Chikamori T, Fukuda K, et al; on behalf of the Japanese Circulation Society Joint Working Group. JCS/JHFS 2018 guideline on the diagnosis and treatment of cardiomyopathies. Circ J 2021; 85: 1590–1689.
- 3.
Tsutsui H, Ide T, Ito H, Kihara Y, Kinugawa K, Kinugawa S, et al; on behalf of the Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group. JCS/JHFS 2021 guideline focused update on diagnosis and treatment of acute and chronic heart failure. Circ J 2021; 85: 2252–2291.
- 4.
Rivas-Lasarte M, Maestro A, Fernandez-Martinez J, Lopez-Lopez L, Sole-Gonzalez E, Vives-Borras M, et al. Prevalence and prognostic impact of subclinical pulmonary congestion at discharge in patients with acute heart failure. ESC Heart Fail 2020; 7: 2621–2628.
- 5.
Thibodeau JT, Turer AT, Gualano SK, Ayers CR, Velez-Martinez M, Mishkin JD, et al. Characterization of a novel symptom of advanced heart failure: Bendopnea. JACC Heart Fail 2014; 2: 24–31.
- 6.
Beck da Silva L, Mielniczuk L, Laberge M, Anselm A, Fraser M, Williams K, et al. Persistent orthopnea and the prognosis of patients in the heart failure clinic. Congest Heart Fail 2004; 10: 177–180.
- 7.
Amir O, Rappaport D, Zafrir B, Abraham WT. A novel approach to monitoring pulmonary congestion in heart failure: Initial animal and clinical experiences using remote dielectric sensing technology. Congest Heart Fail 2013; 19: 149–155.
- 8.
Amir O, Azzam ZS, Gaspar T, Faranesh-Abboud S, Andria N, Burkhoff D, et al. Validation of remote dielectric sensing (ReDS) technology for quantification of lung fluid status: Comparison to high resolution chest computed tomography in patients with and without acute heart failure. Int J Cardiol 2016; 221: 841–846.
- 9.
Uriel N, Sayer G, Imamura T, Rodgers D, Kim G, Raikhelkar J, et al. Relationship between noninvasive assessment of lung fluid volume and invasively measured cardiac hemodynamics. J Am Heart Assoc 2018; 7: e009175.
- 10.
Lala A, Barghash MH, Giustino G, Alvarez-Garcia J, Konje S, Parikh A, et al. Early use of remote dielectric sensing after hospitalization to reduce heart failure readmissions. ESC Heart Fail 2021; 8: 1047–1054.
- 11.
Amir O, Ben-Gal T, Weinstein JM, Schliamser J, Burkhoff D, Abbo A, et al. Evaluation of remote dielectric sensing (ReDS) technology-guided therapy for decreasing heart failure re-hospitalizations. Int J Cardiol 2017; 240: 279–284.
- 12.
Pirrotta F, Mazza B, Gennari L, Palazzuoli A. Pulmonary congestion assessment in heart failure: Traditional and new tools. Diagnostics (Basel) 2021; 11: 1306.
- 13.
Madamanchi C, Alhosaini H, Sumida A, Runge MS. Obesity and natriuretic peptides, BNP and NT-proBNP: Mechanisms and diagnostic implications for heart failure. Int J Cardiol 2014; 176: 611–617.