2023 年 5 巻 11 号 p. 430-436
2023 年 5 巻 11 号 p. 430-436
Background: The number of octo- and nonagenarians admitted to cardiac care units (CCUs) has been increasing in the context of an aging society; however, clinical details and outcomes for these patients are scarce.
Methods and Results: Data from 2,242 consecutive patients admitted to the CCU between 2019 and 2021 (age <80 years, 1,390 [62%]; octogenarians, 655 [29%]; nonagenarians, 197 [8.7%]) were reviewed using the in-hospital database for the Tokyo CCU Network. The primary cause of admission was acute coronary syndrome in younger patients and octogenarians (58% and 49%, respectively) and acute heart failure (AHF) in nonagenarians (42%). The proportions of females, underweight, hypertension, atrial fibrillation, myocardial infarction, stroke, previous heart failure, anemia, and malnutrition were higher among octo- and nonagenarians than among younger patients. In-hospital and 1-year mortality rates were greater in octo- and nonagenarians (younger vs. octogenarian vs. nonagenarian, 2.0% vs. 3.8% vs. 5.6% and 4.1% vs. 11.9% vs. 19.0%, respectively). Multivariate analysis revealed that 1-year mortality was associated with octo-/nonagenarian status (odds ratio [OR] 2.24 and 2.64), AHF (OR 2.88), body mass index (OR per 1-kg/m2 0.91), and albumin concentration (OR per 1-g/dL 0.27).
Conclusions: Approximately 40% of patients admitted to the CCU were octo- or nonagenarians, and being an octo- or nonagenarian, having AHF, a lower body mass index, and lower albumin concentrations were associated with 1-year mortality after CCU admission.
The global population is aging. In 2023, the proportion of the Japanese population aged ≥65 years (29%) is the highest worldwide.1 Over the next 20–30 years, the proportion of the population aged ≥65 years is expected to reach approximately 20% in several regions across the globe.2 The incidence of cardiovascular diseases, including heart failure, acute coronary syndrome (ACS), and atrial fibrillation (AF), increases with age.3 In this context, more octo- and nonagenarians have been admitted to intensive care units (ICUs) and cardiac care units (CCUs).4–6 However, elderly individuals tend to have low physical reserves, poor nutritional status, and multiple comorbidities, and there is controversy regarding the efficacy and cost-effectiveness of therapeutic interventions in this group of patients.7,8 Although several minimally invasive treatments, such as intervention for structural heart disease and percutaneous ventricular assist devices, have been introduced in modern cardiology,9 cardiovascular diseases consume a large amount of medical resouces.10 Characterizing the current status and outcome of elderly patients admitted to the CCU is meaningful; however, few studies have addressed this issue. As such, the present study aimed to investigate the clinical characteristics and short- and long-term outcomes of elderly patients admitted to a contemporary CCU.
This prospective observational analysis was conducted at the Sakakibara Heart Institute (SHI; Tokyo, Japan). The SHI is a cardiovascular center affiliated with the Tokyo CCU Network, and the details of the Network have been reported previously.11,12 We analyzed patients who were transferred to the SHI CCU via the Tokyo CCU Network, with patient information extracted from a dedicated database for the Network. The SHI CCU is a 12-bed, Level 3 facility,13 and patients with prehospital cardiopulmonary arrest or non-cardiogenic shock are not accommodated. Based on Network policies, patients who were admitted electively, transferred from a general ward, or those with acute aortic syndrome were excluded from the database. For patients admitted to the CCU between 2019 and 2021, the characteristics and outcomes of octo- and nonagenarians were compared with those of younger patients (age <80 years).
The study was performed in accordance with the latest iteration of the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of SHI (Approval no: 22-042).
Details of CCU ManagementThe CCU is a semiclosed care unit that requires mandatory consultation with cardiac intensivists. The general rules of CCU admission include ACS requiring emergency or urgent coronary revascularization, acute heart failure (AHF) with an inotrope, invasive or non-invasive positive pressure ventilation (IPPV/NPPV) or mechanical circulatory support, fatal arrhythmia requiring an emergency procedure (e.g., temporary pacemaker, intravenous antiarrhythmic drug or electrical defibrillation), and massive or submassive pulmonary thromboembolism. Patients with acute myocarditis or Takotsubo cardiomyopathy are generally admitted to the CCU for close monitoring. Following intensive interventions and stabilization of the systemic condition, patients were transferred to a high care unit or general ward.
EndpointsPrimary endpoints included in-hospital (or 30-day) and 1-year all-cause mortality rates. Patient survival was confirmed using electronic medical charts.
Statistical AnalysisCategorical variables are expressed as numbers with percentages, whereas continuous variables are expressed as the mean±SD. Group comparisons were performed using the Chi-squared test for categorical variables and analysis of variance for continuous variables. The association between the respective variables and 1-year mortality was analyzed using logistic regression. Variables with P<0.05 in the univariate analysis were entered into multivariate analysis considering plausibility, multicollinearity, and overfitting. Statistical analyses were performed using JMP ver. 16.0.0. (SAS Institute Inc., Cary, NC, USA), and two-tailed P<0.05 was considered to be statistically significant.
In total, 2,242 patients were admitted to the CCU through the Tokyo CCU network between 2019 and 2021. Of these patients, 1,390 (62%) were <80 years old, 655 (29%) were octogenarians, and 197 (8.7%) were nonagenarians (Figure 1). The primary causes of admission in younger patients and octogenarians were ACS followed by AHF, and vice versa in nonagenarians (Table 1; Figure 2). The octo- and nonagenarian groups had a higher proportion of females, underweight, hypertension, AF, myocardial infarction, stroke, previous heart failure, anemia, and malnutrition than the younger patients (Table 1). Oxygen saturation at contact with the ambulance crew was lower, and IPPV/NPPV was highly used in octo- and nonagenarian patients, although mechanical circulatory support was less frequently used in these groups.

Patients included in the present study (n=2,242). Approximately 40% of patients admitted to the cardiac care unit (CCU) between 2019 and 2021 were octo- and nonagenarians. In-hospital (or 30-day) mortality was confirmed in all patients, and 1-year mortality was evaluated in 57% of patients.
Patient Details
| Age <80 years (n=1,390) |
Octogenarians (n=655) |
Nonagenarians (n=197) |
P value | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age (years) | 64.6±12.9 | 84.3±2.8 | 92.5±2.5 | <0.0001* |
| Reasons for CCU admission | <0.0001* | |||
| Acute coronary syndrome | 807 (58) | 323 (49) | 69 (35) | |
| AHF | 236 (17) | 186 (28) | 83 (42) | |
| Arrhythmia | 177 (13) | 90 (14) | 21 (11) | |
| Pulmonary thromboembolism | 22 (1.6) | 2 (0.3) | 0 (0) | |
| Takotsubo cardiomyopathy | 17 (1.2) | 9 (1.4) | 4 (2.0) | |
| Acute myocarditis | 6 (0.4) | 0 (0) | 0 (0) | |
| OthersA | 125 (9.0) | 45 (6.9) | 20 (10) | |
| Male sex | 1,029 (80) | 346 (53) | 90 (46) | <0.0001* |
| Body mass index (kg/m2) | 24.1±4.3 | 22.4±3.8 | 21.4±3.1 | <0.0001* |
| Hypertension | 820 (59) | 467 (72) | 143 (73) | <0.0001* |
| Diabetes | 380 (28) | 199 (31) | 34 (17) | 0.0007* |
| Dyslipidemia | 762 (55) | 315 (49) | 87 (44) | 0.001* |
| Atrial fibrillation | 292 (21) | 191 (30) | 63 (32) | <0.0001 |
| Previous MI | 210 (15) | 133 (21) | 39 (20) | 0.008* |
| Previous PCI | 294 (21) | 215 (36) | 50 (25) | <0.0001* |
| Cerebrovascular accident | 112 (8.1) | 92 (14) | 26 (13) | <0.0001* |
| Peripheral artery disease | 42 (3.0) | 21 (3.2) | 7 (3.6) | 0.92 |
| Prior heart failure | 172 (12) | 119 (18) | 49 (25) | <0.0001* |
| Hemodialysis | 53 (3.8) | 24 (3.7) | 3 (1.5) | 0.19 |
| Medications | ||||
| Antiplatelet | 259 (19) | 149 (23) | 52 (27) | 0.010* |
| Oral anticoagulant | 290 (21) | 191 (30) | 44 (23) | 0.0002* |
| β-blocker | 509 (37) | 271 (42) | 71 (36) | 0.082 |
| RAASi | 523 (38) | 303 (47) | 75 (38) | 0.0006* |
| Diuretic | 313 (23) | 233 (36) | 98 (50) | <0.0001* |
| Statin | 490 (36) | 307 (48) | 63 (32) | <0.0001* |
| Vital signsB and laboratory findings | ||||
| Systolic blood pressure (mmHg) | 138±29 | 140±65 | 142±32 | 0.17 |
| Shock statusC | 56 (4.1) | 31 (4.8) | 7 (3.6) | 0.68 |
| Heart rate (beats/min) | 87±27 | 84±28 | 84±28 | 0.061 |
| Respiratory rate (/min) | 19.7±6.1 | 20.2±6.0 | 21.4±4.9 | 0.001* |
| Oxygen saturation (%) | 95.5±7.2 | 94.6±6.4 | 92.8±7.5 | <0.0001* |
| White blood cell (/μL) | 7,996±3,877 | 7,461±2,893 | 7,861±4,083 | 0.003* |
| Hemoglobin (g/dL) | 13.6±2.3 | 12.0±2.0 | 11.4±1.8 | <0.0001* |
| Creatinine (mg/dL) | 1.27±1.48 | 1.42±1.36 | 1.34±0.81 | 0.10 |
| K (mEq/L) | 4.2±0.6 | 4.4±0.6 | 4.5±0.7 | <0.0001* |
| Log NT-proBNP (pg/mL) | 2.86±0.90 | 3.26±0.75 | 3.49±0.62 | <0.0001* |
| C-reactive protein (mg/dL) | 1.4±3.6 | 1.5±3.6 | 1.6±4.0 | 0.74 |
| Glucose (mg/dL) | 148±60 | 158±65 | 149±61 | 0.006* |
| Total cholesterol (mg/dL) | 187±48 | 172±40 | 176±40 | <0.0001* |
| Triglyceride (mg/dL) | 136±116 | 109±73 | 94±65 | <0.0001* |
| HDL (mg/dL) | 50±16 | 50±15 | 53±15 | 0.11 |
| LDL (mg/dL) | 111±38 | 100±33 | 101±33 | <0.0001* |
| Albumin (g/dL) | 3.9±0.9 | 3.6±0.5 | 3.5±0.4 | <0.0001* |
| Intensive therapy | ||||
| MCSD | 180 (13) | 66 (10) | 10 (5.1) | 0.001* |
| IPPV/NPPV | 339 (24) | 196 (30) | 70 (35) | 0.0007* |
| CRRT | 65 (4.7) | 42 (6.4) | 6 (3.1) | 0.10 |
Unless indicated otherwise, data are given as the mean±SD or n (%). *P<0.05. AOther reasons for admission included other acute cardiovascular diseases or non-cardiovascular diseases. BMeasured by the ambulance crew. CSBP <90 mmHg. DIncluding intra-aortic balloon pumping, percutaneous ventricular assist device, and extracorporeal membrane oxygenation. AHF, acute heart failure; CCU, cardiac care unit; CRRT, continuous renal replacement therapy; HDL, high-density lipoprotein; IPPV, invasive positive pressure ventilation; LDL, low-density lipoprotein; MCS, mechanical circulatory support; MI, myocardial infarction; NPPV, non-invasive positive pressure ventilation; NT-proBNP, N-terminal pro B-type natriuretic peptide; PCI, percutaneous coronary intervention; RAASi, renin-angiotensin-aldosterone system inhibitor; SBP, systolic blood pressure.

Causes of cardiac care unit admission according to age group. The proportion of patients admitted for acute coronary syndrome (ACS) decreased, whereas that of acute heart failure (AHF) increased, with the patient age. PTE, pulmonary thromboembolism.
Primary Endpoints and Predictors of Mortality
Compared with younger patients, in-hospital or 30-day mortality was additive, and 1-year mortality synergistically increased in octo- and nonagenarian patients (in-hospital mortality 2.0% vs. 3.8% vs. 5.6% [P=0.007], respectively; 30-day mortality 4.1% vs. 12% vs. 19%, [P<0.0001], respectively; Figure 3). According to the cause of admission, 1-year mortality was highest (19%) for AHF, followed by ACS (2.2%) and arrhythmia (5.5%; P<0.0001). (Note that patients with pulmonary thromboembolism, Takotsubo cardiomyopathy, and acute myocarditis were omitted from this analysis due to the small sample size.) In multivariate analysis, being an octo- or nonagenarian was independently associated with 1-year mortality (Table 2). In addition to these variables, AHF as a cause of admission, body mass index (BMI), and albumin concentrations were independent predictors of 1-year mortality.
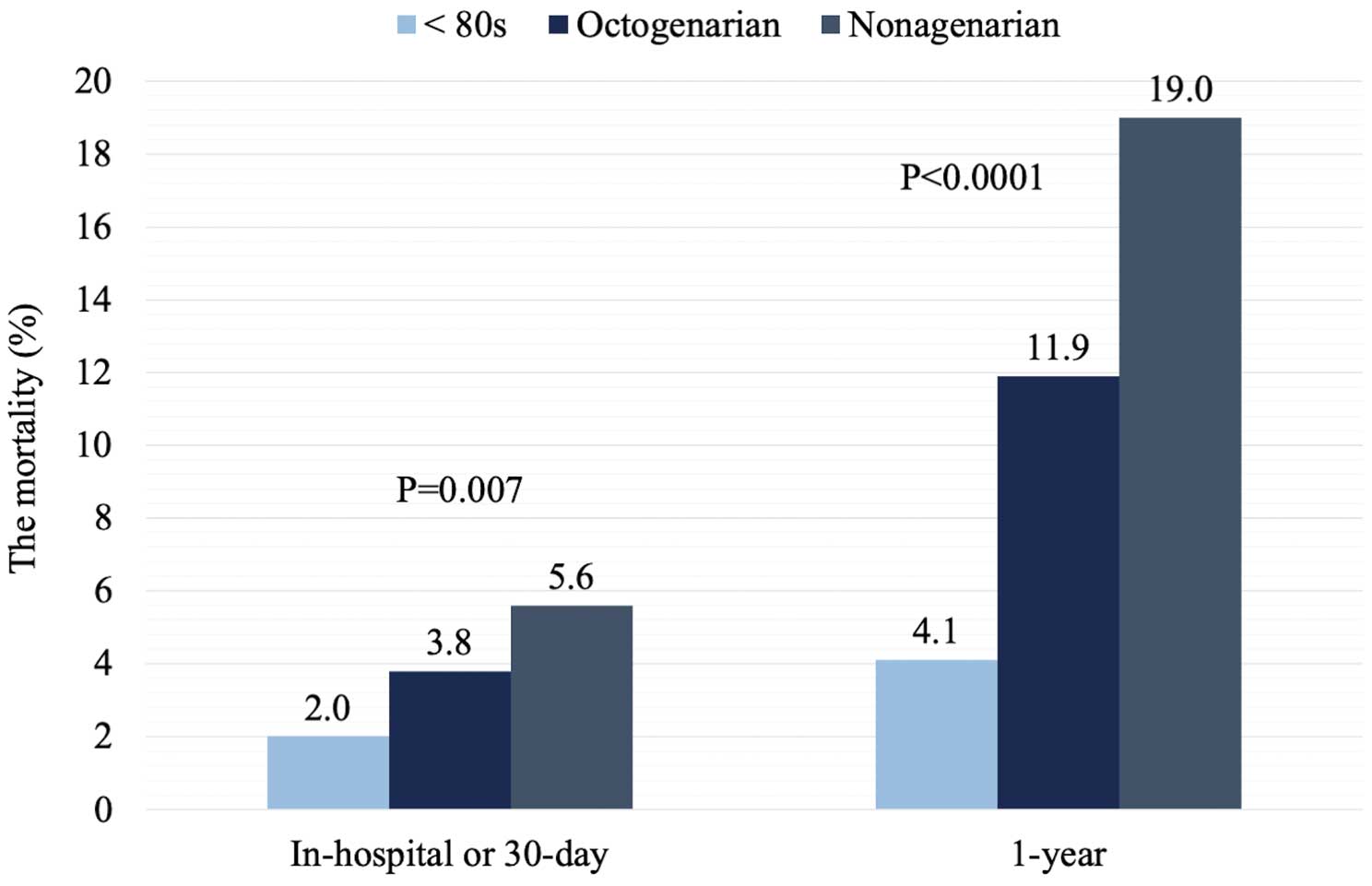
In-hospital/30-day and 1-year mortality according to age group. In-hospital or 30-day mortality was additive, and 1-year mortality synergistically increased in octo- and nonagenarians.
Predictors of 1-Year Mortality
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| ORA | 95% CI | P value | ORA | 95% CI | P value | |
| Age (years) | 1.04 | 1.02–1.05 | <0.001* | |||
| OctogenariansB | 3.15 | 2.03–4.41 | <0.0001* | 2.24 | 1.17–4.32 | 0.016* |
| NonagenariansB | 5.49 | 3.02–9.96 | <0.0001* | 2.64 | 1.09–6.38 | 0.031* |
| AHF as reason for CCU admission | 7.49 | 4.74–11.8 | <0.0001* | 2.88 | 1.50–5.50 | 0.001* |
| Male sex | 1.45 | 0.96–2.18 | 0.78 | |||
| Body mass index (kg/m2) | 0.82 | 0.77–0.88 | <0.0001* | 0.91 | 0.83–1.00 | 0.032* |
| Hypertension | 0.58 | 0.39–0.87 | 0.009* | 0.66 | 0.36–1.21 | 0.19 |
| Diabetes | 0.93 | 0.59–1.47 | 0.75 | |||
| Dyslipidemia | 0.57 | 0.38–0.85 | 0.006* | |||
| Atrial fibrillation | 3.12 | 2.08–4.70 | <0.0001* | 1.43 | 0.78–2.61 | 0.25 |
| Previous MI | 1.22 | 0.74–2.00 | 0.45 | |||
| Previous PCI | 0.96 | 0.61–1.52 | 0.87 | |||
| Cerebrovascular accident | 1.53 | 0.84–2.76 | 0.18 | |||
| Peripheral artery disease | 1.14 | 0.40–3.24 | 0.81 | |||
| Prior heart failure | 4.21 | 2.76–6.41 | <0.0001* | 1.90 | 0.99–3.65 | 0.057 |
| Hemodialysis | 1.59 | 0.61–4.11 | 0.37 | |||
| Medications | ||||||
| Antiplatelet | 1.05 | 0.65–1.70 | 0.85 | |||
| Oral anticoagulant | 2.87 | 1.90–4.33 | <0.0001* | |||
| β-blocker | 2.92 | 1.90–4.48 | <0.0001* | |||
| RAASi | 0.97 | 0.64–1.46 | 0.88 | |||
| Diuretic | 4.19 | 2.75–6.38 | <0.0001* | |||
| Statin | 0.85 | 0.56–1.29 | 0.44 | |||
| SBP (mmHg) | 0.98 | 0.98–0.99 | <0.0001* | |||
| Shock statusC | 3.46 | 1.73–6.91 | 0.002* | 1.34 | 0.43–4.20 | 0.61 |
| Heart rate (beats/min) | 1.01 | 1.00–1.02 | 0.007* | |||
| Respiratory rate (/min) | 1.03 | 1.01–1.06 | 0.008* | |||
| Oxygen saturation (%) | 0.98 | 0.96–1.00 | 0.058 | |||
| White blood cell (/μL) | 1.00 | 1.00–1.00 | 0.25 | |||
| Hemoglobin (g/dL) | 0.69 | 0.63–0.76 | <0.0001* | 1.01 | 0.86–1.16 | 0.99 |
| Creatinine (mg/dL) | 1.13 | 1.02–1.25 | 0.35 | |||
| K (mEq/L) | 1.64 | 1.23–2.20 | 0.001* | |||
| Log NT-proBNP (pg/mL) | 4.67 | 3.30–6.61 | <0.0001* | |||
| C-reactive protein (mg/dL) | 1.08 | 1.04–1.12 | <0.0001* | |||
| Glucose (mg/dL) | 1.00 | 1.00–1.00 | 0.31 | |||
| Total cholesterol (mg/dL) | 0.99 | 0.98–0.99 | <0.0001* | |||
| Triglyceride (mg/dL) | 0.99 | 0.99–1.00 | <0.0001* | |||
| HLD (mg/dL) | 0.95 | 0.93–0.96 | <0.0001* | |||
| LDL (mg/dL) | 0.99 | 0.98–0.99 | 0.0002* | |||
| Albumin (g/dL) | 0.17 | 0.12–0.25 | <0.0001* | 0.27 | 0.16–0.49 | <0.0001* |
| MCSD | 0.82 | 0.42–1.61 | 0.56 | |||
| IPPV/NPPV | 2.62 | 1.75–3.91 | <0.0001* | |||
| CRRT | 2.24 | 1.07–4.69 | 0.048* | 1.92 | 0.68–5.48 | 0.22 |
*P<0.05. AOdds ratio (OR) per unit of the continuous variable. BCompared with the <80-year-old age group. CSBP <90 mmHg. DIntra-aortic balloon pumping, percutaneous ventricular assist device, and extracorporeal membrane oxygenation. CI, confidence interval. Other abbreviations as in Table 1.
The major findings of the present study are as follows: (1) approximately 40% of patients admitted to the SHI CCU between 2019 and 2021 were octo- or nonagenarian, with this group having a higher proportion of patients with AHF as the cause of CCU admission and many more comorbidities than younger patients; and (2) the short- and long-term mortality were substantially higher rates among octo- and nonagenarians than among younger patients. Being an octo- or nonagenarian, AHF, lower BMI, and low albumin values independently predicted mortality.
Increases in Elderly Patients Admitted to the CCU and Their CharacteristicsThe number of patients admitted to ICUs and CCUs has been increasing due to global trends in aging. In a single-center analysis from Israel, the number of nonagenarians admitted to the CCU increased from 4.0% in 2019 to 5.3% in 2022.6 In the CCU of Barcelona University, the number of elderly individuals aged >75 years has increased from 10% to 27% over the past 2 decades.5 In the present study, approximately 40% of patients were octo- or nonagenarians. Possible explanations for this high proportion of octo/nonagenarians are the high aging rate and longer life expectancy in Japan, in addition to differences in study periods, insurance systems, and cultural backgrounds. The aging rate in Japan is projected to reach 38% in 2060,14 and is 41% in South Korea, 36% in Italy, 31% in Germany, 30% in China, and 29% in France.14 Although issues regarding elderly patients in the ICU/CCU are universal, there are few studies to date that have directly addressed octo- and nonagenarians in the CCU.6,15,16 As such, details, outcomes, predictors, and the cost-effectiveness of treating elderly patients in the CCU require further investigation. Bruoha et al. reported that, among nonagenarians, there was a higher proportion of females and patients with hypertension, cerebrovascular accident, congestive heart failure, AF, and anemia, and lower BMI and albumin values,6 which is consistent with our findings. Females have longer lifespans than males, and aging is a risk factor for hypertension, congestive heart failure, and AF. Lower BMI and albumin concentrations reflect low physical reserve, malnutrition, and frailty among nonagenarians.7,17 The main reasons for CCU admission among nonagenarians have been reported to be AHF16 and ACS.6 In contrast to effective interventions, including intensive lipid-lowering therapy and smoking cessation for ACS, the heart failure pandemic has increased the proportion of patients with AHF as a cause of CCU admission.18
Outcomes of Elderly Patients Admitted to the CCU and Future DirectionsPrevious studies6,16 have reported in-hospital mortality rates for nonagenarians admitted to the CCU of 5.6% and 15%, with 1-year mortality rates of 30% and 47%; in the present study, these percentages were 5.6% and 19%, respectively. The independent predictors of long-term outcomes among nonagenarians have been reported to be pulmonary hypertension, diabetes, Elder Risk Assessment score, the Acute Physiology, Age, and Chronic Health Evaluation (APACHE) III score, diastolic blood pressure, blood urea nitrogen, inotrope use, and a recent emergency department visit.6,16 In the present study, octo-/nonagenarian status, AHF, lower BMI, and lower albumin concentrations were negatively correlated with 1-year mortality.
Aging is an established risk factor for AHF and ACS (e.g., GRACE risk score),19 which were the primary causes of CCU admission. In elderly patients with heart failure, the outcomes of nonagenarians were inferior to those of septua- and octogenarians.20 The obesity paradox, which suggests poorer outcomes in patients with a low BMI, has been repeatedly reported for both AHF and AMI.21,22 The cardioprotective effect of adipose tissue, systemic disease or inflammation associated with low BMI, intolerance to the catabolism of AHF, concomitant frailty, and poor nutritional status could be the cause of this relationship. Low albumin concentrations are also negative predictors of AHF and AMI.23,24 Hypoalbuminemia is a marker of comorbidity burden, inflammatory state, and malnutrition, and has adverse pleiotropic effects on prognosis.23 The effectiveness of exercise, dietary support, and anti-inflammatory therapy in patients with hypoalbuminemia remains unclear. Shock status, which means systolic blood pressure <90 mmHg in the present study, was not associated with 1-year mortality in the multivariate analysis. One explanation for this is the definition of shock status adopted. Another explanation is that non-disease-specific parameters highly influenced the 1-year outcome in the survivors from 30 days after CCU admission (i.e., age, BMI, and albumin value), indicating the effects of patients’ physical and nutritional reserve, as well as comorbidities, on prognosis.
Study LimitationsThe present study had some limitations, the first of which was its single-center design; as such, the results should be interpreted with caution. Follow-up relied on confirmation from electronic medical charts, and the follow-up rate was not sufficient. However, the number of octo- and nonagenarians in this study was greater than in previous studies, and the predictors detected were validated for AHF and ACS. Second, our database lacked severity scores, including the APACHE or Sequential Organ Failure Assessment score. However, the applicability of these scores in the CCU has not yet been fully examined. Third, there was no dedicated scale for assessing frailty in the database. However, we collected BMI and albumin data, which are objective and quantitative indices relevant to frailty. Fourth, the only long-term outcome in this study was mortality, and symptom status and quality of life were not assessed. A cost-effectiveness analysis requires this information.
Approximately 40% of patients admitted to the SHI CCU between 2019 and 2021 were octo- or nonagenarians. AHF as a cause of CCU admission and comorbidities were more frequently recognized in octo- and nonagenarians. The mortality rate of these elderly patients was notably higher than that of the younger population (i.e., those aged <80 years). Octo-/nonagenarian status, AHF, lower BMI, and lower albumin concentrations were associated with 1-year mortality in patients admitted to the CCU. These findings should aid in resource utilization, prognostication, and shared decision making in elderly patients admitted to the CCU.
The authors greatly appreciate the members of the CCU.
This study did not receive any specific funding.
The authors declare no potential conflicts of interest relevant to this article.
This study was approved by the Institutional Review Board of Sakakibara Heart Institute (22-042).
The deidentified participant data will not be shared.