2023 年 5 巻 8 号 p. 317-322
2023 年 5 巻 8 号 p. 317-322
Background: This single-center retrospective analysis investigated the number of days required for postoperative 6-minute walk distance (6MWD) to recover to preoperative values after coronary artery bypass grafting (CABG) and the factors influencing this recovery.
Methods and Results: The 6MWD was measured in 101 patients (median age 69 years; 18 women) before and every day after CABG. Univariate and multivariate analyses were performed to identify factors affecting 6MWD recovery to preoperative values after CABG. The median number of days required for recovery of 6MWD after CABG was 9 (interquartile range 7–11 days). Patients were divided into 2 groups based on the median number of days required for recovery of 6MWD; there were 60 patients in the early recovery group (<9 days) and 41 in the “non-early” recovery group (38 who recovered after the median 9 days, and 3 who did not recover during hospitalization). Using univariate logistic regression analysis, diabetes (P=0.01), stroke (P=0.26), left ventricular ejection fraction (P=0.27), and grip strength (P=0.13) were selected for multivariate analysis. Multivariate logistic regression analysis revealed that diabetes (odds ratio 2.955; 95% confidence interval 1.208–7.229; P=0.02) was the only independent predictor of 6MWD recovery.
Conclusions: Diabetes was the single factor influencing the recovery of postoperative 6MWD in patients undergoing CABG.
Cardiac rehabilitation (CR) after coronary artery bypass grafting (CABG) has several beneficial outcomes, such as increasing exercise tolerance (ET), cardiac and peripheral function, and quality of life, as well as reducing rehospitalization rates.1 Therefore, CR generally starts soon after CABG. It is recommended that ET is appropriately evaluated when performing CR,1 and physical exercise programs should be established according to individual ET.2
There are various methods of measuring ET, including the cardiopulmonary exercise test (CPX) and the 6-minute walk test (6MWT).3 CPX involves using a breathalyzer to directly measure maximum oxygen uptake (V̇O2peak), which is the most objective indicator of ET. Therefore, CPX is the most reliable method for measuring ET, but it requires expensive specialized equipment.4 Furthermore, CPX cannot be performed in patients who have difficulty pedaling an aerobic bicycle. In contrast, the 6MWT is a simple way to measure ET because the 6MWT does not require specialized equipment. In addition, it is convenient, inexpensive, and easy to complete.2,5 The 6MWT is reflective of activities of daily living and may be performed by the elderly, severely limited patients, and cardiac patients after recent major surgery2,5 who cannot undertake symptom-limited exercise tests. Hence, the 6MWT is a reliable measure of ET and is widely used to assess ET after CABG.6–8
In previous studies, the timing of the 6MWT measurement was limited to the preoperative, discharge, and long-term periods.6–8 However, there has been no survey of daily 6MWT performed in the early postoperative period. Therefore, the number of days required for ET recovery following CABG remains unknown. Furthermore, factors influencing ET recovery after CABG have not been elucidated.
This study had 2 aims; the first was to determine the number of days after CABG for the 6-minute walk distance (6MWD) to recover to preoperative values and the second was to identify preoperative factors that influenced ET recovery.
This was a single-center retrospective observational study. The study participants were patients who underwent isolated CABG at Kumamoto University Hospital between April 2019 and May 2022. Of the 145 patients who underwent isolated CABG, 101 (median age 69 years; 18 women) were included in the study. The reasons for excluding the remaining 44 patients were an inability to walk 100 m independently preoperatively (n=5), walking limitations due to musculoskeletal disorders (n=7), receiving maintenance hemodialysis preoperatively (n=30), and being unable to participate in gait training because of postoperative cerebral infarction (n=2).
This study was approved by the Kumamoto University Research Ethics Committee (Approval no. 2213). The Institutional Review Board approved this retrospective study and waived the requirement for written consent. We affirm that this study adhered to the ethical principles outlined in the Declaration of Helsinki and its later amendments, including obtaining informed consent from participants, maintaining participant confidentiality, and conducting the research with integrity and respect for the rights of individuals involved.
Clinical Characteristics, Surgery, and Postoperative CoursePreoperative cognitive and physical functions were examined by a physical therapist on the day before CABG. Grip strength was measured in seated patients with the elbow joint flexed 90°. Maximum grip strength was measured using a Grip-D T.K.K. 5401 digital grip strength meter (Takei Kiki Kogyo, Kitanagoya, Japan). In addition, the physical performance of patients was evaluated using the Short Physical Performance Battery, which consists of 3 items: a standing balance test, a 4-m walk test, and rising from a chair. A total score was obtained by summing the scores for each the 3 items.
The 6MWT was performed according to the American Thoracic Society guidelines.3 All patients were fitted with electrocardiogram (ECG) monitors. The 6MWT was performed on a flat, 50-m straight course with no inclination in a hospital corridor, with the help of a physician and a nurse. The 6MWD was measured preoperatively and on consecutive days postoperatively (starting on the day of independent walking up until the day before discharge). For patients transferred to other hospitals because of medical or social conditions, measurements were taken until the day before transfer. The start date of independent walking was defined as the day on which the patient could walk 100 m independently.
Our strategy for isolated CABG was directed at achieving complete myocardial revascularization whenever feasible using an off-pump CABG technique, as described previously.9,10 We bypassed all substantially diseased coronary arteries (stenosis ≥50%) that were >1 mm in diameter. Cardiopulmonary bypass with or without cardiac arrest was performed in patients unsuitable for the off-pump technique, including those with intramyocardial coronary arteries or severely impaired left ventricular function.
CR ProgramThe CR program was based on the Japanese Circulation Society’s early postoperative CR guidelines1 as follows. First, the rehabilitation program was generally started the morning after CABG. Once it was confirmed that the patients’ respiratory and circulatory conditions were stable, they took part in 1–2 CR sessions per day, 6–7 times per week, until discharge. Second, the CR program was performed under the supervision of a physical therapist. Third, passive and active limb exercises, respiratory physical therapy, and early mobilization (sitting on the edge of a bed, standing, walking, and exercise training) were performed. Once a patient could walk independently, rehabilitation, including the 6MWT, was conducted in the ward on weekday mornings and holidays (20 min per session). In addition, aerobic exercise, exercise for activities of daily living, and resistance exercises were performed in the rehabilitation room on weekday afternoons (20–40 min per session). Exercise intensity was determined based on the Borg Rating of Perceived Exertion scale with a target range of 12–13.
ET was assessed using the 6MWT in a hospital corridor to evaluate independent preoperative and postoperative walking up until discharge. Patients were instructed to walk as far as possible within 6 min without running or jogging, and the total 6MWD was measured in meters.3,11
Statistical AnalysesThis study determined the median number of days required for postoperative recovery of 6MWD. Patients were divided into 2 groups: the early recovery group (patients who recovered before the median) and the “non-early” recovery group (patients who recovered after the median and those who did not recover to preoperative 6MWD). Continuous variables are reported as the median and interquartile range (IQR). Nominal variables are expressed as numbers and percentages. Statistical significance was set at P<0.05; all tests were 2-tailed. Differences between groups were assessed using the Mann-Whitney U test or the χ2 test, as appropriate. Univariate logistic regression was initially performed to identify factors influencing recovery of 6MWD. Predictors with P<0.30 in the univariate analysis were incorporated into the multivariate logistic regression analysis. All statistical analyses were performed using IBM SPSS Statistics v.25 (IBM Corp., Armonk, NY, USA).
The median preoperative 6MWD was 430 m (IQR 355–470 m). In this study, all participants underwent CR after CABG. The mean and median postoperative 6MWD decreased in the early postoperative period; however, the 6MWD recovered with time postoperatively (Figure 1). No adverse events were observed during the 6MWT in any of the patients.
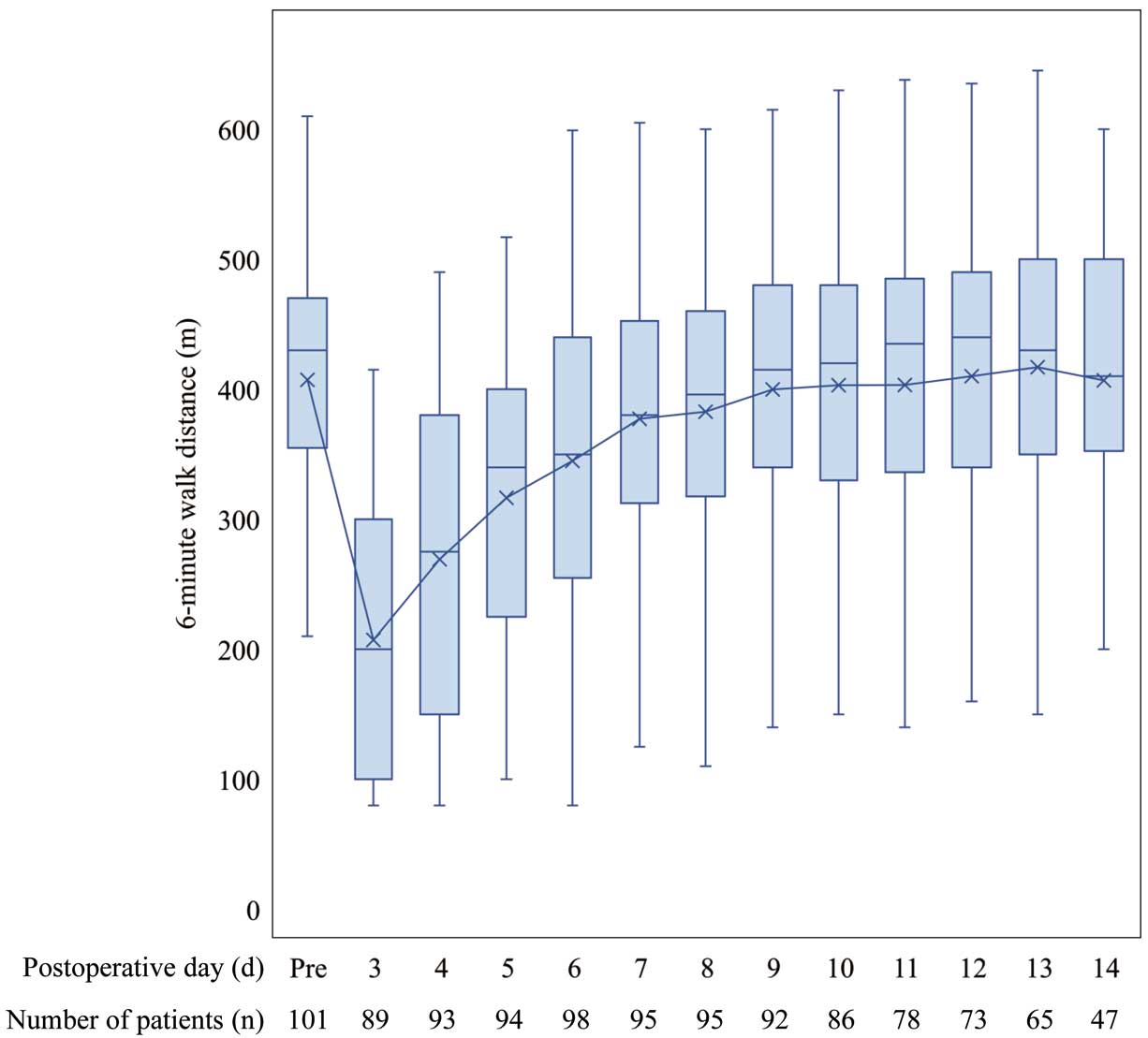
Preoperative (Pre) and postoperative 6-minute walk distance (6MWD). The boxes show the interquartile range (IQR), with the median value indicated by the horizontal line; whiskers show the range and “X” indicates the mean value. The median preoperative 6MWD was 430 m (IQR 355–470 m). The mean and median 6MWD decreased in the early postoperative period, but the 6MWD recovered with time after coronary artery bypass grafting.
Figure 2 shows the days required for postoperative 6MWD to recover to preoperative values. The median number of days required for 6MWD recovery after CABG was 9 (IQR 7–11 days).
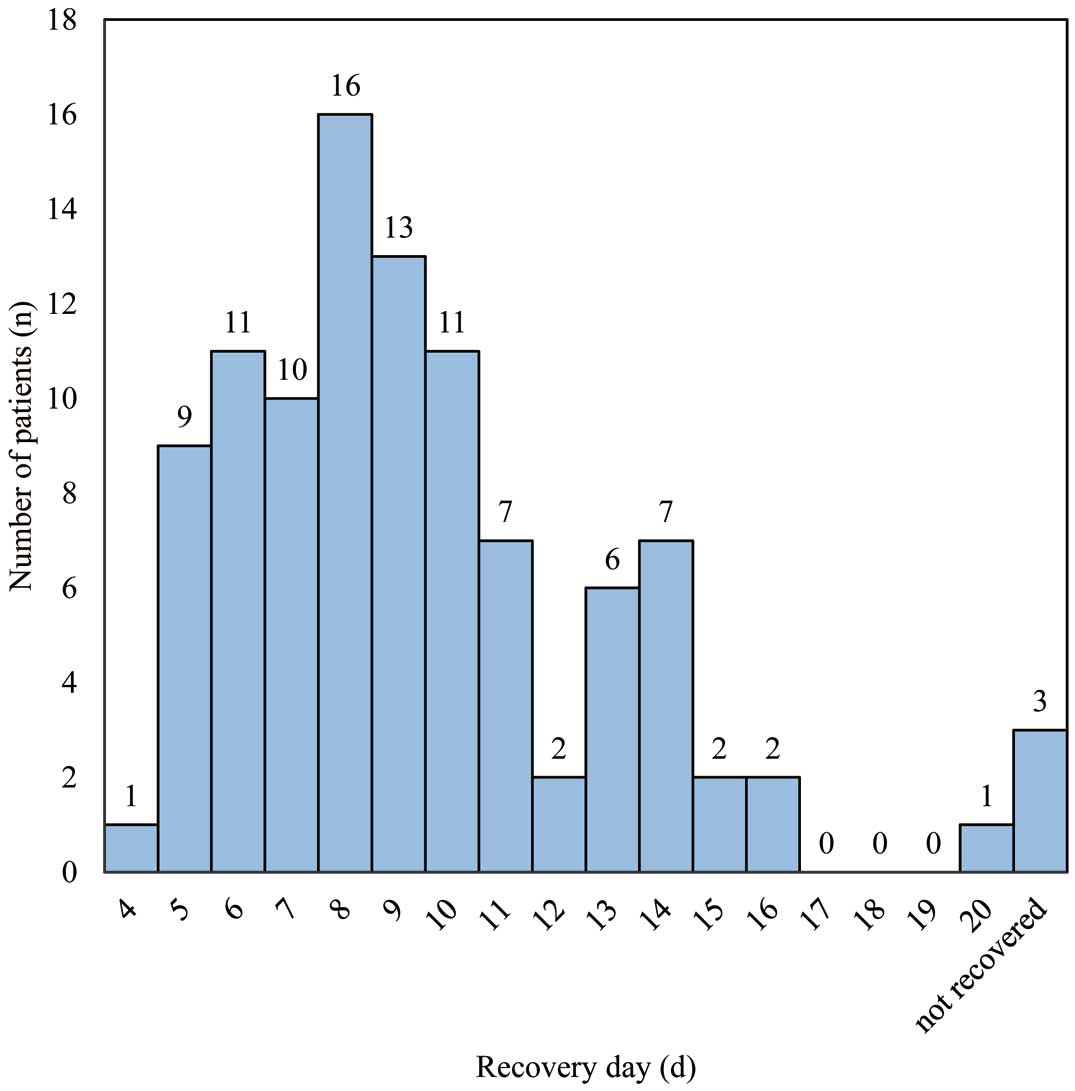
Distribution of the number of postoperative days required for 6-minute walk distance (6MWD) to recover to preoperative values. The median number of days required for recovery of 6MWD after coronary artery bypass grafting was 9 (interquartile range 7–11 days).
Preoperative 6MWD values were attained by 98 (97%) patients. The reasons why 6MWD did not recover in the remaining 3 (3%) patients included a prolonged postoperative wound pain in the leg (n=1), postoperative vasovagal reflex (n=1), and respiratory complications (n=1).
Clinical Characteristics, Surgery, and Postoperative OutcomesThere were 60 patients in the early recovery group and 41 in the non-early recovery group (38 patients in whom 6MWD recovered after the median period, and 3 patients in whom 6MWD did not recover to preoperative values during hospitalization).
The clinical characteristics of the patients are presented in Table 1. The non-early recovery group had a significantly higher rate of diabetes than the early recovery group. There were no significant differences in other factors between the 2 groups.
| All patients (n=101) |
Early recovery (n=60) |
Non-early recovery (n=41) |
P value | |
|---|---|---|---|---|
| Age (years) | 69 [61–74] | 68 [59–74.8] | 70 [61–73] | 0.73 |
| Female sex | 18 (17.8) | 9 (15) | 9 (22) | 0.37 |
| BMI (kg/m2) | 23.8 (22–26) | 23.8 (21.6–25.9) | 23.5 (22.3–26.5) | 0.62 |
| Hypertension | 76 (75.2) | 47 (78.3) | 29 (70.7) | 0.39 |
| Atrial fibrillation | 7 (6.9) | 3 (5) | 4 (9.8) | 0.44 |
| Diabetes | 61 (60.4) | 30 (50) | 31 (75.6) | 0.01 |
| CKD | 27 (26.7) | 14 (23.3) | 13 (31.7) | 0.35 |
| Old MI | 30 (29.7) | 20 (33.3) | 10 (24.4) | 0.33 |
| Stroke | 26 (25.7) | 13 (21.7) | 13 (31.7) | 0.26 |
| LVEF (%) | 58.6 [52.9–63.2] | 59.9 [53.6–63.1] | 57.4 [52.3–63.8] | 0.57 |
| Albumin (g/dL) | 4.3 [4–4.5] | 4.3 [3.9–4.5] | 4.2 [4–4.4] | 0.77 |
| eGFR (mL/min/1.73 m2) | 62 [52–76.5] | 62 [53–74] | 61 [48.5–79] | 0.97 |
| BNP (pg/mL) | 29.6 [12.1–59.4] | 34.6 [18.3–69.4] | 24 [10.4–48.8] | 0.10 |
| HbA1c (%) | 6.4 [5.8–7] | 6.3 [5.7–6.9] | 6.4 [6.2–7.3] | 0.06 |
| EuroSCORE II | 1.3 [0.9–1.9] | 1.3 [0.9–1.9] | 1.3 [1–2.1] | 0.52 |
| Psoas muscle index (cm2/m2) | 6.4 [5.2–7.3] | 6.5 [5.3–7.5] | 6.4 [4.9–7.2] | 0.75 |
| MMSE (points) | 29 [27.5–30] | 29 [27–30] | 29 [28–30] | 0.41 |
| Handgrip strength (kg) | 30.6 [24.5–36] | 31.6 [25.5–37] | 29.3 [22.7–34.3] | 0.14 |
| SPPB (points) | 12 [11–12] | 12 [12–12] | 12 [11–12] | 0.48 |
| 6MWD (m) | 430 [355–470] | 431 [343.8–467.5] | 425 [357.5–477.5] | 0.67 |
| Barthel index (points) | 100 [100–100] | 100 [100–100] | 100 [100–100] | 0.83 |
Unless indicated otherwise, data are presented as the median [interquartile range] or n (%). 6MWD, 6-minute walk distance; BMI, body mass index; BNP, B-type natriuretic peptide; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; EuroSCORE, European system for cardiac operative risk evaluation; LVEF, left ventricular ejection fraction; MI, myocardial infarction; MMSE, Mini-Mental State Examination; SPPB, Short Physical Performance Battery.
Operative and postoperative outcomes are summarized in Table 2. There was no significant difference in the operative data between the 2 groups. However, the postoperative hospital stay was significantly longer in the non-early recovery group than in the early recovery group.
| All patients (n=101) |
Early recovery (n=60) |
Non-early recovery (n=41) |
P value | |
|---|---|---|---|---|
| Operative time (min) | 238 [213.5–264] | 236 [207–262] | 247 [218.5–276] | 0.24 |
| Off-pump procedure | 98 (97) | 59 (98.3) | 39 (95.1) | 0.57 |
| No. grafts per patient | 4 [3–5] | 4 [3–5] | 4 [3.5–5] | 0.45 |
| Use of BITA | 87 (86.1) | 52 (86.7) | 35 (85.4) | 0.85 |
| Use of SVG | 99 (98) | 58 (96.7) | 41 (100) | 0.35 |
| Blood transfusion | 42 (41.6) | 22 (36.7) | 20 (48.8) | 0.23 |
| Duration of intubation (h) | 6.5 [5.4–15.7] | 6.2 [5.4–15.6] | 6.9 [5.4–16.4] | 0.61 |
| Re-exploration for bleeding | 1 (1) | 1 (1.7) | 0 (0) | 0.59 |
| POAF | 19 (18.8) | 13 (21.7) | 6 (14.6) | 0.37 |
| Heart failure | 0 (0) | 0 (0) | 0 (0) | |
| Standing at the bedside (days) | 1 [1–1] | 1 [1–1] | 1 [1–1] | 0.82 |
| Walking around the bed (days) | 2 [2–2] | 2 [2–2] | 2 [2–2] | 0.45 |
| 100 m independent walking (days) | 2 [2–3] | 2 [2–2] | 2 [2–3] | 0.45 |
| Postoperative LOS (days) | 15 [13–16] | 14 [11–15] | 16 [14–17.5] | <0.001 |
Unless indicated otherwise, data are presented as the median [interquartile range] or n (%). BITA, bilateral internal thoracic artery; LOS, length of stay; POAF, postoperative atrial fibrillation; SVG, saphenous vein graft.
Using univariate logistic regression analysis, diabetes (P=0.01), stroke (P=0.26), left ventricular ejection fraction (P=0.27), and grip strength (P=0.13) were selected for multivariate analysis (Table 3).
| Independent variables |
Univariate model | Multivariate model | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age | 1.009 | 0.967–1.054 | 0.67 | |||
| Female sex | 1.594 | 0.572–4.438 | 0.37 | |||
| BMI | 1.042 | 0.922–1.178 | 0.51 | |||
| Hypertension | 0.668 | 0.269–1.662 | 0.39 | |||
| Atrial fibrillation | 2.054 | 0.435–9.708 | 0.36 | |||
| Diabetes | 3.100 | 1.293–7.430 | 0.01 | 2.955 | 1.208–7.229 | 0.02 |
| CKD | 1.526 | 0.627–3.712 | 0.35 | |||
| Old MI | 0.645 | 0.264–1.575 | 0.34 | |||
| Stroke | 1.679 | 0.682–4.128 | 0.26 | 1.423 | 0.553–3.657 | 0.46 |
| LVEF | 0.977 | 0.937–1.019 | 0.27 | 0.975 | 0.933–1.020 | 0.27 |
| Albumin | 0.773 | 0.268–2.230 | 0.63 | |||
| eGFR | 1.001 | 0.979–1.024 | 0.93 | |||
| BNP | 1.001 | 0.997–1.005 | 0.70 | |||
| HbA1c | 1.289 | 0.868–1.914 | 0.21 | |||
| Psoas muscle index | 0.975 | 0.752–1.265 | 0.85 | |||
| MMSE | 1.108 | 0.842–1.458 | 0.46 | |||
| Handgrip strength | 0.962 | 0.914–1.012 | 0.13 | 0.958 | 0.908–1.011 | 0.12 |
| SPPB | 1.069 | 0.806–1.417 | 0.64 | |||
| 6MWD | 1.002 | 0.997–1.006 | 0.43 | |||
CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.
Multivariate logistic regression analysis revealed that diabetes (odds ratio 2.955; 95% confidence interval 1.208–7.229; P=0.02) was the only independent predictor affecting the recovery of 6MWD.
The first main finding of this study was that the median time to recovery of 6MWD, which was measured every day postoperatively in patients who underwent CABG, to preoperative values was 9 days.
The present study revealed an early postoperative recovery of 6MWD compared with a previous study that measured 6MWD preoperatively and postoperatively in patients who underwent CABG.12 In that study, 6MWD was measured in CABG patients preoperatively, 7–10 days postoperatively (at the beginning of CR), and 4 weeks postoperatively (at the end of CR).12 The study indicated that 6MWD 7–10 days after CABG had not recovered to preoperative values (mean [±SD] 459.8±110.1 vs. 344.8±105.6 m, respectively).12 One explanation for the early recovery of 6MWD in our patients may be measuring 6MWD every day after CABG as part of the CR program. Another reason is the use of cardiopulmonary bypass in this study, which is known to affect the recovery of postoperative 6MWD. Arefizadeh et al13 compared ET before and after surgery in patients who underwent off-pump and on-pump CABG, reporting that patients who underwent off-pump CABG showed a significant improvement in ET after CR than those who underwent on-pump CABG. Reports indicate that off-pump CABG confers better postoperative renal function, a lower incidence of metabolic acidosis and oxidative stress, reduced myocardial injury, and lower activation of inflammatory mediators than on-pump CABG.13,14 Moreover, off-pump CABG leads to fewer metabolic disturbances than on-pump CABG.14 In the present study, 97% of patients underwent off-pump CABG, which may have favored the recovery of ET after CABG. However, the present study did not compare patients who underwent off-pump CABG to those who underwent on-pump CABG. Therefore, this requires further investigation.
Factors Affecting the Recovery of Postoperative 6MWDThe second main finding of this study was that diabetes is a factor that influences the recovery of postoperative 6MWD.
Diabetes in the present study was defined according to the diagnostic flowchart of the 2019 Japanese clinical practice guidelines for diabetes.15 Diabetes is an independent predictor of morbidity and mortality in patients undergoing various surgical procedures,16 and several studies have demonstrated that diabetes increases short-term morbidity and mortality.17
In a previous study concerning the impact of diabetes on the improvement of ET after CR, Savage et al18 reported that 21% of patients, with a majority having diabetes and undergoing cardiac surgery, had less improvement in ET after 3 months of CR. Vergès et al19 reported that after CR, individuals with and without diabetes exhibited a significant increase in V̇O2peak. However, this increase in V̇O2peak in the diabetes group was less than half the improvement in V̇O2peak in the non-diabetes group (mean [±SD] 13±24% vs. 30±25%, respectively; P=0.002).19 Although the duration and content of exercise therapy in that study differed from those in the present study, certain results were similar in that patients with diabetes were less likely to regain ET.
Previous studies have reported lower ET in patients with than without diabetes.20,21 Similarly, in CABG patients, Nishitani et al22 reported that V̇O2peak was significantly lower in those with than without diabetes (mean [±SD] 12.5±3.7 vs. 13.7±4 mL/min/kg; P=0.01). The impaired recovery of ET after CABG in patients with diabetes is due to lower ET than that in patients without diabetes. This was attributed to a reduced circulatory response to exercise, decreased cardiac reserve, and decreased peripheral vasodilatory capacity.20,21 In addition, impaired functional capacity of the mitochondria in skeletal muscle has been observed in diabetes.23 Although we did not investigate physiological function or measure V̇O2peak or other factors, similar predispositions may be affected by CABG. Furthermore, they play a role in impeding the early recovery of postoperative 6MWD. This study did not evaluate the presence of complications, such as neuropathy and retinopathy. Hence, future studies should evaluate these factors to study the severity of diabetes in this patient population.
Study LimitationsThis study has several limitations. First, it is essential to note that this was a retrospective, observational study. Second, we could not compare patients undergoing CABG with and without a cardiopulmonary bypass. In future studies, we plan to perform a comparison of patients undergoing CABG with and without cardiopulmonary bypass. Third, the study only included Japanese patients; therefore, the generalizability of the findings to other populations may be limited. Fourth, the 6MWD has a few limitations. The outcome of this test may be influenced by an individual’s motivation, effort, and willingness to perform the test, which may not be uniform across individuals or different testing sessions. Finally, our sample size was small, which could have affected the statistical power of the study and the precision of the results.
Our study highlights the potential influence of diabetes on the response to CR following cardiac surgery. In this study, 6MWD after CABG was measured daily, and the median time required to recover to the preoperative value was 9 days. In this study, diabetes influenced the recovery of postoperative 6MWD. Although CR can lead to significant improvements in aerobic capacity, the impact on ET may be less pronounced in patients with diabetes. Our findings underscore the importance of personalized approaches and targeted interventions to optimize the outcomes of CR in this patient population and indicate CR after CABG for improved outcomes.
The authors thank Wiley Editing Services (www.wileyeditingservices.com) for help with English language editing.
This study did not receive any specific funding.
The authors declare that there are no conflicts of interest.
This study was approved by the Kumamoto University Research Ethics Committee (Approval no. 2213). The requirement for obtaining informed consent was waived due to the retrospective nature of this study.
The data supporting the findings of this study are available from the corresponding author upon reasonable request.