2023 年 5 巻 8 号 p. 331-337
2023 年 5 巻 8 号 p. 331-337
Background: Endomyocardial biopsy (EMB) is a useful modality in diagnosing the origin of cardiomyopathy and the condition of the impaired myocardium. However, the usefulness of obtaining an EMB from the right and left ventricles (RV and LV, respectively), and its associations with echocardiographic parameters, have not been explored.
Methods and Results: Ninety-five consecutive patients with non-ischemic cardiomyopathy excluding myocarditis who underwent EMB between July 2017 and May 2019 were studied. Seventy-nine RV and 93 LV biopsy specimens were pathologically analyzed. The relationships among echocardiographic data before EMB and pathologically measured cardiomyocyte diameter (CMD) and interstitial fibrosis (IF) were evaluated. CMD in both LV and RV specimens correlated with echocardiographic LV morphology, but only CMD in the LV was significantly correlated with cardiac function evaluation, including LV ejection fraction, E′ and E/E′. In contrast, there were no significant correlations between IF in either the LV or RV and any echocardiographic parameters measured. Furthermore, CMD of both ventricles was significantly correlated with B-type natriuretic peptide (BNP) concentration at EMB, whereas IF of the LV was barely related and IF of the RV was not significantly correlated with BNP concentrations.
Conclusions: Pathologically evaluated CMD of EMB specimens of the LV may be more related to functional parameters for heart failure status and LV geometry on echocardiographic examination, than IF.
Endomyocardial biopsy (EMB), a widely used examination tool, plays an important role in monitoring cardiac allograft rejection and directly diagnosing unexplained cardiomyopathy and acute myocarditis.1,2 In Japan, EMB is mostly performed to identify the cause of myocarditis or non-ischemic cardiomyopathy.3–5 Although the trajectory of treatment is determined based on left ventricular (LV) function, EMB is generally performed only in the right ventricle (RV).6 This is despite the lack of evidence that a biopsy of only the RV can be used to evaluate cardiac function. The pathological myocardial properties of the EMB assume importance in the medical treatment of heart failure (HF). Several EMB parameters, including cardiomyocyte diameter (CMD), interstitial fibrosis (IF), cardiomyocyte disorganization, nuclear deformity, myocardial disarray, and lipofuscin deposition, may be evaluated. In particular, CMD and IF can be quantified using microscopic analysis. Reports indicate an association between CMD and prognosis in patients with dilated cardiomyopathy and have compared cell diameters in patients with different cardiomyopathies.5,7 In addition, a significant difference in the CMD has been reported between patients with sick sinus syndrome and healthy controls.8 Furthermore, in a reworsening HF patient with anthracycline-induced cardiomyopathy, CMD significantly increased with decreased LV contractility after the explant of an LV assist device.9 Thus, CMD varies depending on the type of heart disease, and sensitively reflects the pathology and condition of HF.
Transthoracic echocardiography (TTE), a non-invasive modality, is used as an essential repeatable examination for each heart disease type to evaluate the quantification of cardiac chamber size, systolic and diastolic function, valve disease, and hemodynamics.10–12 Both EMB and TTE explore the etiology and myocardial properties of patients with HF and play useful roles in clinical treatment. However, little is known about the association between EMB findings and TTE. Thus, the aims of the present novel study were to investigate the relationships between the pathological findings of EMB of the LV and RV and echocardiographic parameters, as well as to evaluate the advantages and disadvantages of obtaining biopsies from the LV or RV.
This retrospective single-center study enrolled 105 patients without coronary artery disease who underwent EMB at Showa University Hospital to investigate the causes of cardiomyopathy between July 2017 and May 2019. At Showa University Hospital, EMB of the LV or both ventricles is performed, unless there is a specific reason, because EMB from both ventricles has been shown to improve the diagnostic yield of myocarditis and non-ischemic cardiomyopathy compared with sampling of the RV or LV only.13–15 The selection of study subjects is shown in Figure 1. First, 8 patients diagnosed with acute myocarditis using EMB were excluded from the study. Of the remaining 97 patients, 78 underwent EMB of both ventricles, 16 underwent EMB of the LV only, and 3 underwent EMB of the RV only. Specimens from 2 patients were excluded because the samples could not be analyzed. Therefore, 93 LV and 79 RV specimens from 95 patients were pathologically evaluated. Baseline characteristics, including demographics and laboratory data, were retrospectively collected from medical records.

Enrollment of endomyocardial biopsy (EMB) specimens in this study. LV, left ventricle; RV, right ventricle.
This study was approved by the Local Ethics Committee of Showa University Hospital (No. 3268), and written informed consent was obtained from all patients according to the ethical guidelines of the Declaration of Helsinki.
Transthoracic EchocardiographyEach patient underwent resting standard TTE before undergoing EMB. LV size was evaluated by LV end-diastolic dimension (LVEDD) and LV end-systolic dimension (LVESD), whereas LV systolic and diastolic function was evaluated by LV ejection fraction (LVEF) and tissue Doppler-derived E′ and E/E′. Relative wall thickness (RWT) was calculated as (2 × posterior wall thickness) / LVEDD. RWT represents a relationship between LV wall thickness and cavity size, with an increased RWT indicating concentric LV hypertrophy. Further, an increase in RWT may underestimate the LV cavity and overestimate apparent LV contractility. The TTE findings were assessed according to the current guidelines of the American Society of Echocardiography and the European Association of Cardiovascular Imaging.10
Histological Evaluation of Biopsy SpecimensEMB specimens were obtained from the LV wall and RV septum using biopsy forceps (Argon Medical Devices, Plano, TX, USA). Between 1 and 5 specimens were collected from each location. The specimens were fixed in formalin, processed using a graded series of ethanol and xylene solutions, and embedded in paraffin. Subsequently, specimens were cut into serial 3-µm sections and stained with hematoxylin-eosin (HE) and Masson’s trichrome. CMD and IF were pathologically and quantitatively evaluated.16 Mean CMD was determined by measuring the diameter across the nucleus of a minimum of 30 randomly selected myocytes from HE-stained sections at ×400 magnification (Figure 2A). IF was evaluated in each section using ImageJ software version 1.53u (National Institutes of Health, Bethesda, MD, USA) and divided by the total myocardial area (Figure 2B). CMD and IF measurements were analyzed by 2 cardiac pathologists (E.T., T.M.) who were blinded to the clinical data.
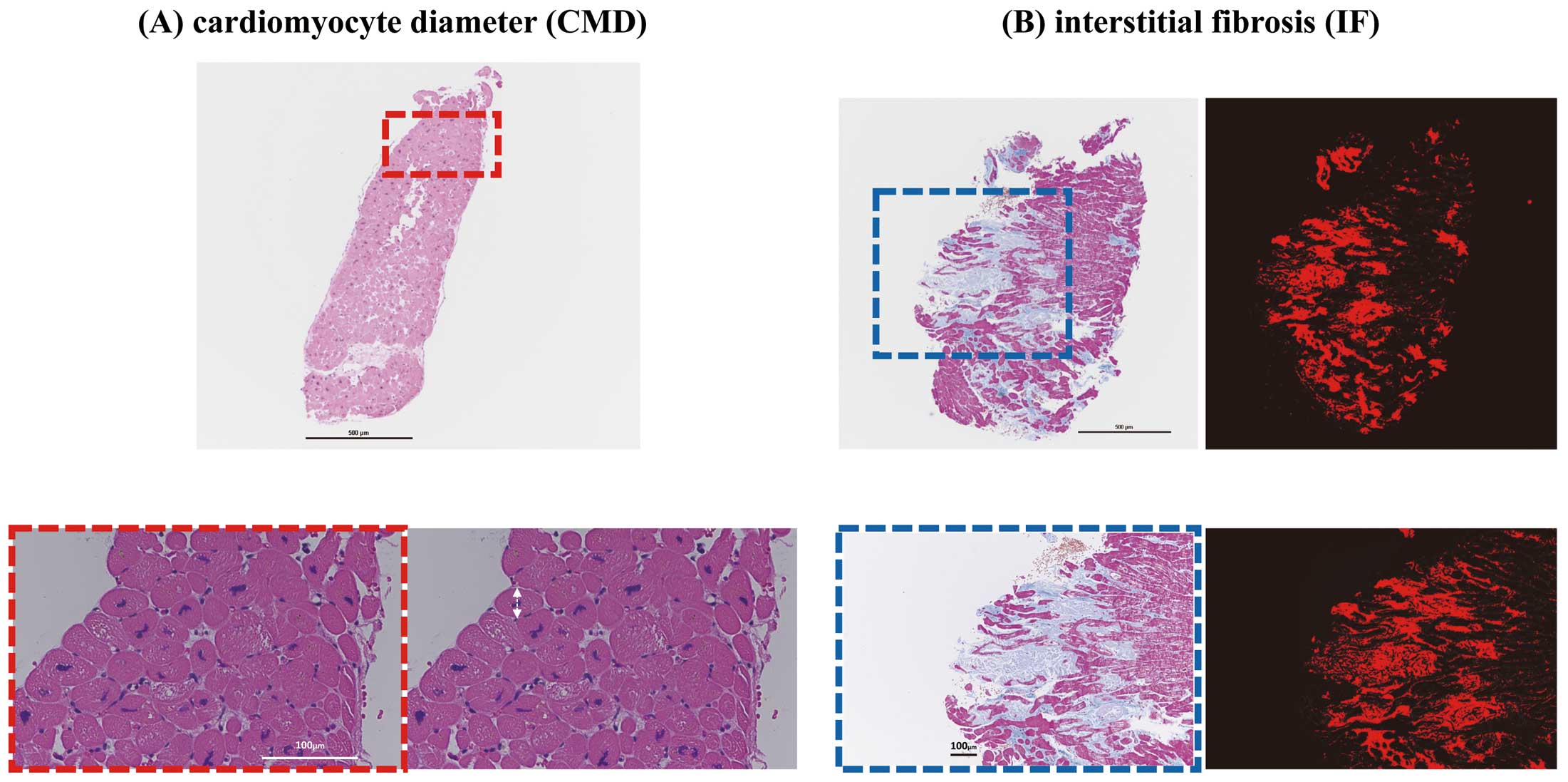
(A) Images showing measurement of cardiomyocyte diameter (CMD) in hematoxylin-eosin (HE)-stained sections. The upper sample is at low magnification (40×) and the bottom samples are highly magnified (200×). A minimum of 30 myocardial cell diameters (double-headed arrows) were measured. (B) Calculation of interstitial fibrosis (IF) from sections stained with Masson’s trichrome (Right) and HE (Left). The upper images are shown with low magnification (40×) and the bottom images with high magnification (100×). The percentage of IF was calculated in each section by dividing the fibrotic area (red in Masson’s trichrome-stained sections) by the total myocardial area in ImageJ (National Institutes of Health, Bethesda, MD, USA) software.
Normally distributed continuous variables are expressed as the mean±SD, whereas those that were not normally distributed are presented as the median with interquartile range (IQR). Categorical variables are expressed as frequencies and percentages. Correlations between echocardiographic parameters, CMD, and IF were analyzed using Spearman’s rank correlation coefficients. Generally, LV hypertrophy affects LV morphology. Hence, when LV hypertrophy is present, the relative shrinkage of the LV cavity must be considered in the echocardiographic evaluation of LV geometry. Subsequently, the relationships were adjusted for LV RWT using a partial correlation. All analyses were performed using MedCalc version 20.215 (MedCalc Software, Mariakerke, Belgium). For all analyses, two-tailed P<0.05 was considered statistically significant.
The clinical and ultrasound characteristics of the 95 patients are summarized in Table 1. The mean age of the patients in this study was 59±15 years, and 65% were men. Based on the combination of clinical course, other imaging, and pathological findings, concluded that 32 (34%) patients were classified as having dilated cardiomyopathy (DCM), 9 (9%) were classified as having tachycardia-induced cardiomyopathy, 9 (9%) were classified as having hypertrophic cardiomyopathy, 23 (24%) were classified as having hypertensive heart disease, 4 (4%) were classified as having sarcoidosis, and 18 (19%) were classified as having some other clinical diagnosis (Table 1). The median B-type natriuretic peptide (BNP) concentration was elevated to 445.9 pg/mL (IQR 136.3–1,070.1 pg/mL). The mean LVEF was 40.3±14.1% and 22 (23%) patients had RWT >0.42, which was defined as LV concentric remodeling. Only one cardiac tamponade, a major complication of EMB of the LV, was observed among the 95 patients (1.1%) and was surgically treated.
| Clinical data | |
| Age (years) | 59±15 |
| Male sex | 62 (65) |
| Height (cm) | 164±9.1 |
| Weight (kg) | 65.8±16.3 |
| BMI (kg/m2) | 24.3±4.9 |
| Atrial fibrillation | 18 (19) |
| T2D | 18 (19) |
| Hypertension | 54 (57) |
| Dyslipidemia | 50 (53) |
| Follow-up time (years) | 2.1±1.1 |
| Clinical diagnosis | |
| DCM | 32 (34) |
| TIC | 9 (9) |
| HCM | 9 (9) |
| HHD | 23 (24) |
| Sarcoidosis | 4 (4) |
| Other* | 18 (19) |
| Blood examination | |
| Hemoglobin (mg/dL) | 13.4±2.3 |
| BUN (mg/dL) | 21.2±12.7 |
| Creatine (mg/dL) | 1.2±1.1 |
| Albumin (g/dL) | 3.7±0.6 |
| HbA1c (%) | 6.1±1.0 |
| LDL (mg/dL) | 111.4±37.5 |
| HDL (mg/dL) | 50.2±15.8 |
| TG (mg/dL) | 111.3±74.1 |
| BNP on admission (pg/mL) | 445.9 [136.3–1,070.1] |
| Echocardiography | |
| LVEDD (mm) | 55.6±8.3 |
| LVESD (mm) | 44.5±10.5 |
| IVS (mm) | 9.4±2.3 |
| PWT (mm) | 9.7±2.0 |
| LVEF (%) | 40.3±14.1 |
| LAD (mm) | 43.1±8.1 |
| E (cm/s) | 77.4±28.1 |
| E′ (cm/s) | 7.6±3.1 |
| E/E′ | 11.9±5.9 |
| TRPG (mmHg) | 23.9±9.3 |
| RWT | 0.36±0.1 |
| RWT >0.42 | 22 (23) |
| Histological morphometry | |
| CMD (μm) | |
| LV | 22.1±4.5 |
| RV | 16.9±3.0 |
| IF (%) | |
| LV | 12.5±11.5 |
| RV | 8.3±5.1 |
Data are given as the mean±SD, median [interquartile range], or n (%). *Other clinical diagnoses include undiagnosed cardiomyopathies, such as chronic inflammatory cardiomyopathy except sarcoidosis, connective tissue disease and cancer-related chemoradiation therapy. BMI, body mass index; BNP, B-type natriuretic peptide; BUN, blood urea nitrogen; CMD, cardiomyocyte diameter; DCM, dilated cardiomyopathy; HCM, hypertrophic cardiomyopathy; HDL, high-density lipoprotein; HHD, hypertensive heart disease; IF, interstitial fibrosis; IVS, interventricular septum; LAD, left atrial dimension; LDL, low-density lipoprotein; LV, left ventricle; LVEDD, left ventricular end-diastolic dimension; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic dimension; PWT, posterior left ventricle wall thickness; RV, right ventricle; RWT, relative wall thickness; T2D, Type 2 diabetes; TIC, tachycardia-induced cardiomyopathy; TRPG, tricuspid regurgitant pressure gradient.
Pathological findings showed that the mean CMD in the LV and RV was 22.1±4.5 and 16.9±3.0 μm, respectively, with a corresponding IF of 12.5±11.5% and 8.3±5.1%. There were no sex differences in either CMD or IF. This study included 54 (57%) patients with hypertension and 18 (19%) with diabetes. Comparing patients with and without hypertension, CMD (23.5±4.2 vs. 20.4±4.1 μm; P=0.0007) and IF (14.5±13.6% vs. 9.8±6.3%; P=0.049) of the LV were significantly greater in the group with hypertension, whereas there were no differences in CMD and IF of the RV between the 2 groups. Moreover, CMD and IF of the LV and CMD in the RV did not differ between those with and without diabetes, although IF of the RV was significantly higher in those with than without diabetes (8.8±5.3% vs. 5.9±3.6%; P=0.049).
Comparison of Pathological Findings and Differences Between the LV and RVThere was a weak correlation between CMD in the LV and RV (r=0.31, P=0.008), but there was no correlation between IF in the LV and RV (r=0.22, P=0.053). Furthermore, there was no significant correlation between CMD and IF in the LV (r=0.01, P=0.36), but there was a weak positive correlation between CMD and IF in the RV (r=0.31, P=0.006).
Correlation Between EMB and TTE FindingsCorrelations between echocardiographic parameters and quantified EMB findings, namely CMD and IF, in the LV and RV are presented in Table 2A. Because LV concentric hypertrophy may affect the relationship between pathological evaluations and LV morphology and function, the association of EMB with TTE was re-evaluated after adjusting for RWT (Table 2B). As indicated in Table 2A, the correlation between CMD and TTE findings was stronger in specimens obtained from the LV than RV, based on parameters that indicate LV morphology. Conversely, little correlation was found between quantified IF from EMB and echocardiographic findings, regardless of whether samples came from the LV or RV. Table 2B presents results corrected by RWT as an indicator of LV concentric remodeling. Considering the degree of LV wall thickening, the relationships among CMD, LVEDD, and LVESD were stronger in the LV than RV. Although a weak correlation was observed between CMD in the RV and echocardiographic findings, it did not change after adjustment for RWT.
| (A) | CMD | IF | ||||||
|---|---|---|---|---|---|---|---|---|
| LV | RV | LV | RV | |||||
| r | P value | r | P value | r | P value | r | P value | |
| LVEDD | 0.37 | <0.001 | 0.23 | 0.039 | −0.007 | 0.950 | −0.01 | 0.906 |
| LVESD | 0.35 | <0.001 | 0.25 | 0.028 | 0.02 | 0.818 | 0.01 | 0.917 |
| E′ | −0.25 | 0.021 | −0.11 | 0.340 | −0.17 | 0.122 | −0.27 | 0.016 |
| E/E′ | 0.28 | 0.001 | 0.26 | 0.027 | 0.01 | 0.373 | 0.13 | 0.273 |
| LVEF | −0.26 | 0.001 | −0.16 | 0.142 | −0.06 | 0.599 | −0.08 | 0.492 |
| (B) | ||||||||
| LVEDD | 0.48 | <0.001 | 0.24 | 0.036 | 0.03 | 0.764 | −0.05 | 0.629 |
| LVESD | 0.44 | <0.001 | 0.26 | 0.024 | 0.07 | 0.517 | −0.02 | 0.835 |
| E′ | −0.24 | 0.023 | −0.14 | 0.25 | −0.16 | 0.137 | −0.29 | 0.011 |
| E/E′ | 0.27 | 0.011 | 0.27 | 0.025 | 0.09 | 0.387 | 0.13 | 0.267 |
| LVEF | −0.30 | 0.004 | −0.16 | 0.18 | −0.08 | 0.422 | −0.06 | 0.594 |
Abbreviations as in Table 1.
An additional analysis was performed with 76 patients for whom EMB samples were obtained from both ventricles. As shown in Supplementary Table A,B, there was a weak correlation found between CMD and IF of both ventricles and echocardiographic findings, similar to the findings presented in Table 2A,B.
Relationship Between HF Status and Pathological Evaluation of EMBCMD in the LV was correlated with LV morphology, contractility, and diastolic function on TTE. Thus, we examined the correlation between CMD and IF in both ventricles and logarithmically transformed BNP concentrations in EMB samples. CMD in both the LV and RV was significantly correlated with BNP concentrations (r=0.28 [P=0.007] and r=0.31 [P=0.007], respectively), whereas IF exhibited a very weak correlation with BNP only in the LV (r=0.21, P=0.044) and not the RV (r=0.11, P=0.331).
In addition, the association between pathological evaluation of EMB samples and LV reverse remodeling after optimal medical treatment for HF was investigated. In this study, a ≥15% reduction in LV end-systolic volume was used as a definition of a responder to optimal medical therapy HF.17,18 Of 69 patients with echocardiographic follow-up, 42 had baseline LVEF <40%. Among these 42 patients, 36 (86%) were considered responders to optimal medical therapy for a mean of 9±6 months. There were no significant differences in CMD and IF of both ventricles between responders and non-responders.
Reproducibility of Microscopic QuantificationThe respectively intra- and interobserver variabilities, as assessed based on intraclass correlation coefficients (ICCs), were 0.872 (95% confidence interval [CI] 0.676–0.949) and 0.783 (95% CI 0.452–0.914) for CMD in the LV and 0.973 (95% CI 0.932–0.989) and 0.970 (95% CI 0.924–0.988) for CMD in the RV. Similarly, the intra- and interobserver variabilities (ICCs) for IF were 0.971 (95% CI 0.928–0.989) and 0.964 (95% CI 0.909–0.986), respectively, in the LV and 0.915 (95% CI 0.785–0.966) and 0.916 (95% CI 0.789–0.967), respectively, in the RV.
This is the first study to highlight the differences in pathological findings between RV and LV EMBs and their association with echocardiographic findings. The 2 new findings of this study are that: (1) CMD obtained from EMB of the LV, but not from the RV, was strongly related to LV morphological and functional indices on echocardiography and this association tended to be stronger after adjusting for RWT as an index of LV concentric remodeling; and (2) IF in either the LV and RV had few significant correlations with most echocardiographic parameters.
Diagnostic Value of LV vs. RV EMBNot only is EMB an important examination for monitoring cardiac allograft rejection for heart implantation and determining the cause of myocarditis and cardiomyopathy, but it is also valuable for assessing the clinical outcome of patients with LV dysfunction.19–21 EMB is performed primarily in the RV and is a relatively safe procedure, except in rare cases of cardiac tamponade.1,22 Conversely, TTE is an indispensable non-invasive examination for assessing heart size, contractility, diastolic function, and valvular disease. Notably, TTE evaluation of systolic and diastolic function in patients with HF primarily used the LV. This clinical discrepancy in assessing different ventricles is expected because EMB is primarily performed on the RV, and echocardiography primarily evaluates the LV. Several studies have shown that obtaining specimens from both the LV and RV increases the diagnostic yield of myocarditis and cardiomyopathy compared with sampling the RV or LV alone.13–15 In contrast, several relatively small studies have reported no significant difference in the degree of IF and electron microscopy findings between LV and RV specimens in patients with HF.16,23 The present study examined whether LV morphology and cardiac function on TTE were consistent with the pathological evaluation of LV or RV EMB. CMD, a microscopic indicator of dysfunctional myocardium in LV specimens, was strongly associated with echocardiographic indices. Consequently, the novel of this study is that CMD of the LV correlates more strongly with LV morphology and cardiac function than CMD of the RV. EMB in HF with LV dysfunction should be evaluated on the basis of specimens obtained in the LV.
Microscopic Quantitative Evaluation of EMB Samples and Its Relationship With Cardiac FunctionPathological evaluation of EMB samples includes not only CMD and IF, but also cardiomyocyte disorganization, nuclear deformity, myocardial disarray, and semiquantitative deposition of lipofuscin for comprehensive evaluation of myocardial deformity.16 Differentiating the 3 major patterns of IF progression in EMBs is useful for classifying myocardial diseases; however, these patterns do not indicate fibrosis of the entire heart.16,24 Hence, IF does not necessarily correlate with the amount of late gadolinium enhancement (LGE) on cardiac magnetic resonance imaging (MRI), which indicates fibrosis of the entire LV, nor does it predict the prognosis of patients with DCM.25,26 In contrast, CMD is not only associated with pressure load for the ventricle but also with HF status and cardiomyopathies such as hypertrophic cardiomyopathy.16 This explains the correlation between CMD, but not IF, and echocardiographic parameters of the whole heart, such as LV morphology, contractility, and diastolic function in this study. The diastolic tissue Doppler velocity (E′) in TTE indicates active LV myocardial relaxation and E/E′ calculated as the early mitral inflow velocity (E wave) divided by E' reflects LV filling pressure.27 BNP, a peptide released by the ventricle as myocytes stretch, is correlated with LV filling pressure and other cardiac morphological abnormalities.28 Although neither BNP nor E/E' are clinical parameters that can completely estimate LV filling pressures, they are simple and useful for understanding the status of HF.29,30 This study included a large number of patients hospitalized for congestive HF and LV dysfunction, so that elevated BNP concentrations can be a compensatory response to LV overload. Hence, the results of the present study show a correlation between these indices and CMD, and may indirectly explain the usefulness of CMD in EMB. However, the correlation is not strong enough to directly link increased CMD to worsening cardiac function.
Clinical Implications of EMB in HF Patients With CardiomyopathyThe association between the pathological findings of EMB and HF prognosis remains unclear. Vigliano et al reported that EMB findings, such as CMD and autophagic vacuolization, may predict mortality in idiopathic DCM.7 Conversely, other studies have reported that EMB findings are not associated with prognosis.31,32 Although the association between EMB findings and prognosis was not evaluated in the present study, CMD in the LV was related to LVEF, E′, and E/E′, which, in turn, are associated with the prognosis of HF.33,34 CMD is related to genetic factors and the heart under pressure overload does not necessarily enlarge.35 Several studies have demonstrated that genetic mutations affect cardiovascular events and prognosis.36,37 Furthermore, LGE on cardiac MRI is a predictor of the combined endpoints of all-cause mortality and cardiovascular hospitalization in patients with DCM.38 Therefore, the combination of CMD findings in EMBs with others parameters, such as genetic factors and MRI findings, may be a powerful prognostic indicator. This retrospective study was too small to show an association between response to optimal medical therapy for HF and pathological findings on EMB. A prospective observational study is needed to reveal the relationship between the response to medical therapy and EMB findings.
Study LimitationsThe present study has some limitations. First, this was a relatively small retrospective study at a single institution. Therefore, the cases in which EMB could not be performed from both ventricles may contain examiner intent or bias based on individual clinical reasons. Second, EMB has the inevitable problem of sampling error. Hence, the EMB findings may not reflect the findings of the whole heart. In addition, the present study did not adequately analyze the response to optimal medical treatment for HF. A study to determine whether pathological findings can stratify the response to medical therapy for HF is one of the next topics to be investigated. Furthermore, the present retrospective study lacks information focusing on the RV, so the association between biventricular EMB and echocardiographic evaluation of the RV could not be investigated. Finally, our study included patients with various cardiomyopathies; if each disease was assessed separately, the results may vary.
Among the pathologically evaluated EMBs, specimens obtained from the LV had a closer association with functional indices as well as LV geometry on echocardiography than those from the RV, and more so than IF from both ventricles. In addition to diagnosing myocarditis and cardiomyopathies, the pathological evaluation of EMB samples may indicate the stage of cardiomyopathy and HF status, which would be useful in HF management.
The authors are grateful for the support of all the staff in the Ultrasound Examination Center and Pathology Department in Showa University Hospital. The authors also thank Editage (www.editage.com) for English language editing.
This study did not receive any specific funding.
All authors declare that there are no potential conflicts of interest.
This study was approved by the Local Ethics Committee of Showa University Hospital (No. 3268).
The individual deidentified participant data, demographics, laboratory, echocardiography, and pathology findings, will be shared. The research proposal (in Japanese) will also be available. The the data will become available immediately following publication, ending 5 years after publication. Data will be shared with anyone wishing to access the data and will be shared as Excel files via email.
Please find supplementary file(s);
https://doi.org/10.1253/circrep.CR-23-0062